Abstract
Although Romania has a long-lasting tradition in organized medical healthcare, in the last two decades the Romanian healthcare system has been undergoing a perpetual transition with negative effects on all parties involved. The lack of long-term strategic vision, the implementation of initiatives without any impact studies, hence the constant short-term approach from the policy makers, combined with the “inherited” low allocation from GDP to the healthcare system have contributed significantly to its current evolution. Currently, most measures taken are of the “fire-fighting” type, rather than looking to the broader, long time perspective. There should be no wonder then, that predictive and preventive services do not get the proper attention and support. Patient and physicians should step in and take action in regulating a system that was originally designed for them. But until this happens, the organizations with leadership skills and vision need to take action—and this has already started.
Keywords: Healthcare system, Predictive diagnostics Prevention, Personalized medicine, Brain aging, Public health
Historical context
Romania has a long-lasting tradition in organized medical healthcare. The first legal provisions for social solidarity were enforced in 1895 (Mining Act), further developed in the 1902 Labor Act. The first compulsory insurances for accidents, diseases and retirement were enacted as early as 1915—being deemed at that time as one of the most modern laws in Europe in this field.
The initial healthcare system was first established between the two world wars (1933) and originated in the social security system initially designed by 2nd Reich Chancellor Otto von Bismarck in 1881. Industrial workers, traders, their employees and families as well as independent contractors were the first insured Romanians (not exceeding 5% of overall population, however). The contributions were proportional with the incomes gained and were equally supported by employers and employees.
The 1949 Health Act enacted the initial transition towards a Semashko health insurance system. This model involved publicly funded, centralized and integrated health systems with universal or close to universal entitlement to free healthcare. The Semashko model placed an emphasis on in-patient and specialist care and on wide-scale public health interventions. The burden of financing the health system was evenly distributed across the population, there were few financial barriers to accessing services and geographical coverage was excellent. From 1950 to 1970 Romania experienced a dramatic fall in early mortality and enjoyed better health outcomes than other countries with a similar level of average income. Major achievements included successes in controlling vaccine-preventable diseases, tuberculosis, leprosy and schistosomiasis, and the eradication of malaria.
However, the management of the healthcare system was strictly centralized and rigid. The Government held complete monopoly over all healthcare services; no private medical care was allowed (the private-owned medical facilities were all abolished) and all health professionals were state-employed public servants.
Although several amendments were brought to the initial law, a new Health Act was passed only in 1978. Further on, in 1983 was legislated that certain service costs had to be supported by patients; however all medical care was still provided in state-owned medical facilities. The lack of any competition and/or private initiative resulted in poor-quality medical care services.
By December 1989 (that is, at the end of Romanian communist regime) the public health system was unsatisfactory, underfinanced, inefficient, inflexible, outdated and unresponsive to patients’ demands and needs. Investment decisions were politicized and often inefficient, leading, for instance, to an over-reliance on curative, in-patient and specialist care at the expense of health promotion, disease prevention and primary care [1]. Such flaws limited the system’s ability to deal with an aging population and changing disease patterns, and the 1980’s saw a decline in some of the major health indicators.
Some negative aspects derived from that system still bear a negative burden upon the current health insurance system:
A relatively low share of the GDP is still granted for healthcare services (for 2009 only a 3.2% of the GDP was assigned for healthcare);
The system is dysfunctional due to inequitable and centralized allocation of resources;
Specific local requirements are not met;
The former centralization of medical and healthcare policies had already lead to hospital managers incapable of operating funds, resources and supplies.
In the first years after the fall of the communist regime (1990–1998) a dual financing system was implemented; namely, funds originated from state budget as well as from additional sources (i.e. a special public health fund, World Bank funding, Phare funds and donations). During that period the patient was for the first time allowed to freely choose which physician he/she should address, and it was about that time when the first family practitioners emerged.
The Social Health Insurance Act was first passed in 1997 but was still tributary to the Bismarck model. Health insurance contributions were compulsory, thus enforcing social solidarity in a newly emerging decentralized system. Following a 1-year transition, the NHIH started administering health funds (1999); the NHIH was an autonomous public institution led by representatives of the insured population (employees) and employers organized in administration boards.
The 2002 Social Health Insurance Act brought further improvements: entire population had to be covered in a consolidated national social protection system; this Act legislated for the first time that each citizen was free to address any medical facility (i.e. physician office, hospital) of his/her choice. This Act also featured the first predefined package of medical services (as set forth in the healthcare framework contract).
Further reforms were brought by the 2006 Act, which actually reunites some of the beneficial features of the inter-war healthcare insurance system with the routine and bureaucracy of communist social and healthcare administration.
Primary healthcare services are still of a relatively poor quality; high bureaucracy as well as incoherent investigation and drug prescription limitations, all of these targeting especially the family physicians resulted in an ineffective management of referrals to in-hospital care and in overrated in-hospital services (albeit diagnostic or curative). Furthermore, high-end equipment and medication supplies are occasionally scarce, especially in disadvantaged geographic enclosures. Hospital care is currently characterized by discrepancies between the number of hospital beds and the staff assigned to provide in-hospital healthcare services; occasionally hospital capacity gets exceeded by patient inflow.
Current challenges
Amongst the negative aspects in this newly emerging hybrid healthcare system we noted that it still bears the main stigmata of Bismarck-derived health systems: healthcare professionals have no power in influencing (that is, fine-tuning) the system. For instance, the RCoP only plays a consultant role in the yearly negotiations of the healthcare framework contract, the leading players remaining the MoH and the NHIH.
The latest shifts in MoH policies aim at giving up the centralized MoH management of hospitals in favor of local administration. However, the leaders of the RCoP officials criticize the decentralization process, since it seems to target mainly dysfunctional hospitals (understaffed, underequipped, with huge debts and heavily relying on public funds). Even if this decision would bring such hospitals closer to the communities they serve, making them perhaps more receptive to specific community needs and requirements, the Chairman of the RCoP fears the worst, given the ongoing financial crisis. Moreover, his criticisms also target the politicization of the healthcare system.
Another critical challenge resides in the fact that throughout Romania the healthcare facilities use local initiatives and voluntary quality assurance mechanisms instead of national quality or safety legislation. Such legislation is much needed in order to address the “side effects” of the previous healthcare system.
Although clinical practice guidelines are commonly regarded as an accessible tool for improving quality, reducing disparities in clinical practice and improving patient safety and in spite of aggressively emerging malpractice legislation, Romania is just beginning to introduce practice guidelines. Thus, the MoH website presented only 12 clinical practice guidelines, dedicated to stroke, angina pectoris, acute coronary syndromes, myocardial infarction, hypertension, chronic lung disease, chronic obstructive pulmonary disease, cervical cancer, breast cancer, prostate cancer, colorectal carcinoma and diabetes care. No currently MoH-approved guidelines address primary, preventive or family care.
Healthcare personnel issues
The inadequately low payment levels in the healthcare system resulted in a decreased motivation of the medical professionals and have led to: proliferation of informal payments, dual working and a brain drain to other professions, other countries or the private sector. Average yearly wages for young specialists-in-training range from 2,040 to 4,080 EUR, while the average yearly wages for a specialist is around 4,500 EUR (mass media estimates). According to the official labor cost survey, the average monthly gross earnings for health and social care reached about 380 EUR [2].
Given the accession of Romania to the European Union (2007) and therefore the mandatory alignment of Romanian legislation to EU practices, the Romanian healthcare system currently faces a never-before encountered challenge: the migration of healthcare professionals towards more financially secure locations in the EU. According to a recent mass-media statement of the Chairman of the RCoP (Dr. Vasile Astarastoaie), Romania should probably declare a red alert code due to medical staff migration. According to the data presented in this interview, about 10% of Romanian medical staff decided to work abroad, mainly due to severe underfunding of medical facilities (especially hospitals). Mass media estimates point to an alarmingly high 5,500 physicians leaving to work abroad (1,500 in 2007, 2,100 in 2008 and 1,900 in 2009).
In consequence, the vacancies rate in the first quarter of 2010 (mid-quarter) was 0.70% [higher than in the fourth quarter of 2009 (0.50%) but lower than in the first quarter of 2009 (1.27%)]. The highest vacancy rates among all the economic sectors, in the first quarter of 2010 were registered in social insurance of public sector (1.94%) and in health and social care (1.39%) [2].
Unofficially, mass media currently claims that one of the leading motivations for following a medical career and/or training as a doctor resides in the hope of being able to either migrate abroad or work as a medical representative for international pharmaceutical companies (Table 1).
Table 1.
An overview of medical coverage in Romania (end-year number of items) [2]
| 1999 | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | |
|---|---|---|---|---|---|---|---|---|---|
| OP | 22,458,022 | 22,435,205 | 22,408,393 | 21,680,974* | 21,733,556 | 21,673,328 | 21,623,849 | 21,584,365 | 21,537,563 |
| Physicians | 46,238 | 45,786 | 46,773 | 45,805 | 46,919 | 48,150 | 47,388 | 46,936 | 48,199 |
| P/P | 486 | 490 | 479 | 476 | 463 | 450 | 456 | 460 | 447 |
| Dentists | 7,708 | 8,307 | 8,694 | 8,830 | 9,447 | 9,907 | 10,249 | 10,620 | 11,651 |
| Pharmacists | 6,610 | 7,189 | 7,298 | 7,328 | 7,793 | 8,763 | 9,283 | 9,932 | 11,108 |
| AMS | 118,875 | 119,446 | 120,433 | 123,836 | 120,740 | 121,683 | 123,455 | 126,613 | 136,353 |
| H beds | 164,215 | 166,858 | 167,943 | 162,675 | 142,739 | 142,573 | 143,027 | 142,034 | 138,025 |
| GPO | n/a | 4,698 | 5,220 | 5,758 | 2,483 | 1,021 | 906 | 1,007 | 1,036 |
| FPO | n/a | 9,026 | 8,937 | 8,803 | 9,278 | 10,924 | 10,939 | 10,969 | 11,048 |
| NCI-FP | 14,051,000 | 13,610,000 | 15,713,000 | 15,791,000 | 15,439,000 | 16,205,000 | 16,159,000 | 15,324,000 | 14,848,000 |
* official population census
OP overall population, P/P population per physician, AMS ancillary medical staff, H hospital, NCI-FP new cases of illnesses, as reported by family physicians, GPO general practitioner offices, FPO family practitioner offices
Public health funding
The operational character of a health system ultimately and crucially depends on its funding and organization (including herein the policies for collecting and managing funds). The public health system funding has been one of the most controversial issues undergoing debates throughout the past 20 years.
Given previous misconceptions deeming the public health sector as a non-productive sector of the economy, the public health expenditures have always been low in Romania, lesser than in western countries and even lesser than in other former communist countries.
Lower public health expenditures could only be provided by (1) decreased healthcare staffs (hence, the understaffing noted above) and by (2) having the medical personnel constrained to scarcely using the (already) scarce resources available.
Lesser healthcare staff was in the past a state policy; lesser healthcare staffing was deemed as financially profitable, since lesser staff meant (a) lesser staff employment expenditures and (b) lesser recommendations for public health expenditures (i.e. healthcare, drugs, procedures etc.). The public health expenditure has therefore traditionally held only a minor share of the GDP.
After the fall of the communism, the average public health expenditure ranged between 3 and 4% of the GDP [3]; the WHO health statistics for 2010 however noted an estimated 4.7% of the GDP for 2007 [4].
The sources of public health funding are currently based on the state budget, on a unified national fund for social health insurance—FNUASS, on local administration budgets, on individual incomes, on foreign loans (including herein non-refundable loans), on donations and sponsorships. The FNUASS held in 2007 a 75% share in the public health funds, based on mandatory contributions collected from employees (5.5% of income) and employers (5.5% of wage funds) [3] (Fig. 1).
Fig. 1.
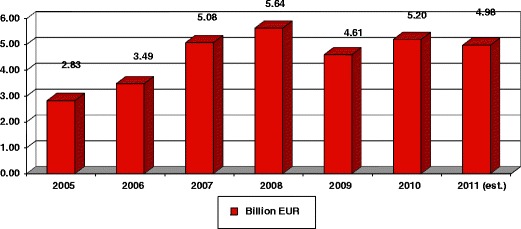
Evolution of funds allocated for health throughout the past years in billion EUR [5]
However, given an overall population aging as well as due to unemployment and financial instability, the public health funding has decreased (4 million social health insurance contributors currently strive to cover the needs of the entire Romanian population, estimated to roughly 22 million).
Unfortunately, there were no transparent, evidence-based guidelines issued by the government for allocating funds [3] and therefore public health expenditures are, to a large extent, managed on a preferential basis (i.e. personal or political affiliations, etc.). Therefore, there have been many situations covered by media regarding acquisitions of high-end expensive medical equipment, which was later on left unused (sometimes for hilarious reasons, i.e. the lack of trained personnel capable of using such equipment or due to insufficient funding for installing/operating/servicing them).
Recent financial media reports [5–7] announce a new draft health law being under work, derived from the 2008 report of the Presidential Health Committee [3], expected to be inspired from the legislation in force in the Netherlands. This draft, initially expected to be released in October 2011, allegedly creates the premises for private funding of the national health system (functional private health insurances, competing with the state health system), since the current health system is based on the monopoly of the NHIH. Breaking state monopoly and the long-expected emergence of private competitors on the healthcare insurance market is expected to boost financial performance (as in, service value per price) for the benefit of both health care providers (healthcare organizations or professionals) and patients, by creating premises for better planning and management of health-related expenditures.
The initial position, which claimed that the mandatory contribution of employees for the national, social health insurance fund would be expected to increase by at least 2.6% [6], has been eliminated in the more recent statements. It is now said that the sources of extra money shall be, on one hand the inclusion of the currently several contribution-exempted categories of population (by increasing the collecting base) and on the other hand from the optional insurances (for people who want more than the basic package of medical services covered by the mandatory contribution/insurance). These two measures should bring additional 1,5 billion EURO in the system [7].
Public health system management
Although efforts are made to decentralize the healthcare system by transferring hospitals to local administration, the Romanian healthcare system is still built around the central administration; hence, its feedback mechanisms depend mainly on medical staff and administration.
However, RCoP was assigned with a consultative role when it comes to the negotiation of the framework contract for providing healthcare, according to the current Health Act in force. This eloquent phrasing actually translates into an absolute lack of power to interfere with the decision-making process, since the College is in fact only being notified on decisions, albeit in their draft, while the actual decision-makers most often ignore the suggestions made by the RCoP. Moreover, patients and their organizations/representatives lack possibilities to interfere in terms of regulation with a system funded mainly based on their own contributions.
The NHIH is still tributary to the Ministry of Health and to the Ministry of Public Finances in terms of decision-making processes.
There is an increased need for focusing healthcare policies on patient-targeted issues, i.e. on quality of medical services and patient safety.
The lack of responsibility in allotting resources and the lack of previous, sound feasibility studies before making costly decisions quite often lead to acquisitions of high-end medical equipment later left unused (sometimes even unwrapped) due to the lack of highly-trained personnel capable of handling such equipment (as revealed in local mass-media throughout the past year or so). However, plenty of the mass media stories were inaccurate: journalists are sometimes keen to judge and denigrate physicians, in spite of their insufficient medical background, and therefore many of the shortcomings due to a malfunctioning, transitional healthcare system are attributed in the overall public eye to the medical staff. It is therefore understandable why the medical staff, underpaid and unjustly blamed, chooses to relocate in other EU countries.
Patient needs and population health status
A first step towards analyzing patient needs and an overall assessment of population healthcare was performed as part of a national program for the assessment of health in overall population (known as “PNESS”). PNESS was run between July 1st 2007 and December 31st, 2008 with costs summing up to 631,604,957 RON (equiv. to ~158.5 million EUR). Although it initially reported a reasonable coverage in terms of overall population (55%), a press release of the MoH [8] identified that it was too costly, that the data collected was inaccurate/incomplete for 1.2 million patients and that 450,000 people were double-reported. The same report also identified that, for those patients that were in fact insured, the tests paid for within the PNESS could have also been covered by their social health insurance, thus decreasing program expenditures.
As far as the PNESS results are concerned [9], 55% of Romanians were screened (n = 11.1 million), 9.9 mn covered by social health insurance and 1.2 million not insured; roughly 43% of screened patients were male. 37% of screened people (n = 4.1 million) were identified as being at risk for various diseases (30% at risk for diabetes, 7% at risk for CVD, 6% at risk for cancer).
In terms of lifestyle and diet, <34% of screened daily serve high-fat meat and 76–80% have fresh fruits and vegetables on a daily basis. Up to 30% of population consummes alcohol and up to 29% are smokers (11–12% planning to quit ‘next year’). Although 67–68% of screened walk at least 30 min per day just 1–2% of them exercise regularly. 156,000 patients were diagnosed with various diseases in early stages.
The health ministry at that time (E. Nicolaescu) reported that the program was a success, being a first step towards the implementation of evidence-based medicine and towards recognizing the central, key-role of the family doctor in prevention and prophylaxis. The PNESS also allegedly helped in updating population records where inaccurate and in identifying nationwide healthcare coverage (and deficits). The suggested strategies designed based on PNESS results were primary prevention programs (a 3-year prevention program targeting diet risks and physical exercising, aimed at lowering CVD and cancer risks, and a national HPV vaccination program, aimed at lowering uterine cancer risks). Secondary prevention programs targeted at screening for uterine, breast and colon cancer were subsequently adopted, and there has been some concern about issuing diagnostic and therapeutic guidelines and protocols.
However, since the MoH is prone to political interference, the following ministry of health severely criticized the program deeming it “a complete failure” and “the most costly and illogical assessment of population health” and considering that “a considerable amount of money was spent for finding out nothing” [8].
Still, in spite of political and party differences, some of the conclusions iterated by the initiating ministry in the initial report were put into practice [9].
Healthcare and policy-making
The latest available report of the Presidential Commission on Health, when analyzing the public healthcare [3] states: “Currently there is no coherent policy regarding healthcare information”. Indeed, there is no national coverage IT&C infrastructure capable of supporting a centralized database of all insured patients, there is no integrated solution enabling medical staff (family practitioners, hospital doctors etc.) and pharmacies to exchange information in real time about their patients. Efforts are made towards designing an integrated, electronic patient card system, which would lessen bureaucracy and improve effectiveness of diagnostic and therapeutic interventions. Improving the centralized management and accuracy of healthcare data may indeed lead to improved policy-making.
However such efforts may seem futile, since there are still reports of few distant, difficult-access rural areas lacking electricity and/or internet coverage.
The same report suggested a reorganization of the system based on institutional and decisional decentralization. Although steps are being taken to decentralize hospitals and transfer them to local authorities, this decision does not seem to work—at least not for the present time: most hospitals are burdened with huge debts accumulated due to chronic underfunding, and transferring them to local authorities seems just a desperate attempt to get rid of debts by transferring them from the MoH to the local administrations.
Another recommendation addresses the development of a quality assurance system targeting improved quality of medical care. This is expected to be performed by means of annual healthcare service and technology/performance assessments, but although such assessments are most welcome, it is still unclear who is expected to cover such costs. As far as family practice offices are concerned (which should be first-handedly included in such assessments) the annual costs required for such assessments may lead, due to severe and chronic underfunding, to financial bankruptcy for some practices (especially for those high-needed offices located in poor, rural areas).
In-hospital care
Romania has one of the highest in-hospital admission rates in the world [10], with in-hospital care constantly exhausting about 50% of health insurance budgets (Table 2, Fig. 2).
Table 2.
Distribution of national health insurance house funds as expected for 2011; based on the budgeted unified health insurance fund (FNUASS), according to [5]
| Type of expenditures | Amounts (billion EUR) |
|---|---|
| Drugs, supplies, medical devices | 1.2 |
| Ambulatory care services | 0.4 |
| In-hospital services | 1.7 |
| Other expenditures | 0.6 |
| GRAND TOTAL | 3.9 |
Fig. 2.
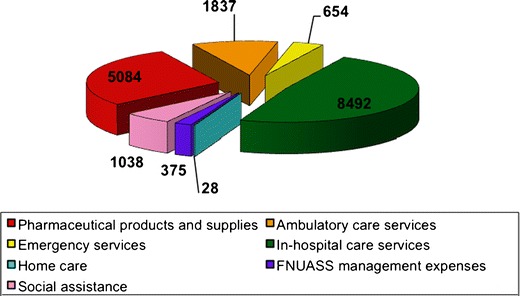
Execution of the 2010 FNUASS budget (2010 annual report of the National Health Insurance House); main expenditures according to [11]
However, although many in-hospital cases may have been solved (i.e. diagnosed, treated and monitored) by family practices and ambulatory care offices, the lack of a structured territorial network of family practitioners and ambulatory care specialized medical offices makes patients address big city hospitals (i.e. university hospitals). Patients often report having to walk several kilometers to the nearest family doctor or drug store (sometimes with no road access to the nearest point of care). This leads to an unnecessary burden for hospitals, in terms of admissions and therefore costs, which further leads to severe population dissatisfaction about hospitals and doctors. The Eurostat 2009 report claims that 63% of Romanians are dissatisfied with hospital services and further 52% of them are dissatisfied with doctors [12].
It is however fair to state that some of this burden is due to population habits, remnants from the communist ages when in-hospital care was in some instances the sole way to get adequate care and free access (as stated by the social health insurance) to drugs and specialized care.
The current trends in decision-making policies aim to restructure in-hospital care and to improve primary and ambulatory care. However, there is much need for dedicated facilities and services capable to deal with chronic care patients, palliation, elders and social cases.
Further development of nursing services is also required.
Even if doctors in most university hospitals relate to international and (when existing) national guidelines and protocols, the actual (as opposed to mostly declarative and outdated) implementation of a continuously updated set of guidelines may lead to decreased in-hospital costs. Transferring more diagnostic responsibilities to the family doctors may lessen the financial burden for hospitals. For example, according to current regulations, family doctors cannot recommend certain diagnostic procedures (i.e. MRI, CT, serology and immunology tests, etc.) unless if such (quite costly) procedures are paid in full by patients, and therefore need to refer the case to their fellows working in ambulatory care (where available) or in hospitals. Hospital doctors willing to solve referred cases have no option but to admit (hospitalize) the patient thus over-burdening the social health care funds with unnecessary accommodation and meal costs.
At least in part, some of the in-hospital burden may be eased by developing a home-care specialized network which would enable earlier hospital dismissing of patients while still providing them with an optimal home care package.
A lesser patient load for family doctors (since family doctors willing to join the social health insurance system currently have to maintain a capitation list of at least 1,000 patients) and an adequate remuneration based on quality of care, on patient satisfaction and, of course, on an increased provision of preventive, predictive and personalized services should lessen the financial burden on the social healthcare system.
Recent mass-media reports attribute to the Romanian President a declaration stating that Romania needs “(…) a system in which hospitals are no longer state-owned. Hospitals should become foundations or companies, hiring contractor physicians and nurses and clearly stating what any citizen should expect when admitted into a hospital (…)” [13].
Indeed, quite recently (April 2011) a number of 67 low-performance state-owned hospitals were closed under the promise of later developing them into elderly care facilities. The decision to close the hospitals was at that time justified by increased hospital expenses; however, at of the present time (September 2011) mass media reports state that only seven of those hospitals are now elderly care facilities [14] in spite of nation-wide estimates of at least 5,000 people in need of care (that is, admission) in specialized old-age and chronic care facilities [15].
Still, the longest journey begins with the first step; even though the criteria for selecting the hospitals that needed to be closed and changed into old-care facilities may be debatable, there was much need for sealing off “black holes” in health funding and, undoubtedly, there was also need for creating specialized facilities for providing healthcare to chronic and old-age patients.
Ambulatory care
Before 1999 territorial healthcare used to be provided in roughly 6,000 dispensaries, administered through local hospitals and based on centralized and local funding. They included enterprise-based dispensaries for employees, school offices, and community-based dispensaries and provided coverage for all the population residing within a specific perimeter, regardless of their employment (i.e., social health insured) status. Following the implementation of family doctor based care (hence, based on patient’s choice instead of territorial coverage) a large number of dispensaries were divided into private family practice offices and many specialists’ offices were closed (Table 3).
Table 3.
Overall number of ambulatory care facilities in Romania
| Type/year | 1997(7) | 2000(2) | 2001(2) | 2002(2) | 2003(2) | 2004(2) | 2005(2) | 2006(2) | 2007(2) |
|---|---|---|---|---|---|---|---|---|---|
| Dispensaries | 3,970 | 908 | 406 | 442 | 304 | 267 | 224 | 211 | 208 |
| State-owned | n/a | 908 | 406 | 442 | 304 | 267 | 223 | 210 | 206 |
| Private-owned, | n/a | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 2 |
| Family doctor offices | 0 | 9,026 | 8,937 | 8,803 | 9,278 | 10,924 | 10,939 | 10,969 | 11,048 |
| Polyclinics | 507 | 253 | 202 | 205 | 208 | 236 | 249 | 260 | 263 |
| State-owned | n/a | 90 | 62 | 44 | 40 | 32 | 30 | 28 | 22 |
| Private-owned | n/a | 163 | 140 | 161 | 168 | 204 | 219 | 232 | 241 |
These data suggest that decision and policy-makers are paying less and lesser attention to preventive and predictive services
Drug policies
Following staff wages, the cost of drugs is the second biggest financial burden on the Romanian social health insurance system [3], exceeding a share of 25% of overall expenditures. Access to drugs is however difficult, since although about 50% of Romanians live in rural areas, only about 30% of pharmacists and 20% of physicians actually work in rural areas [3]. The analysis of the top 20 best prescribed drugs revealed that most of them are newly-emerged, highly costly drugs, preference being given to prescribing imported drugs. Instead of having patients treated with cheaper, local or generic drugs, this leads to having about 8% of patients spend around 70% of pharmaceutical expenditures [3] (Fig. 3).
Fig. 3.
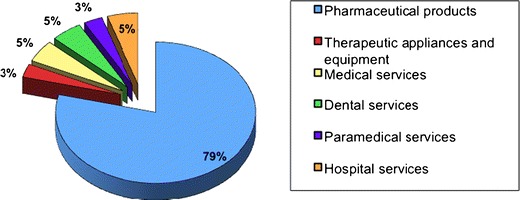
Structure of consumption expenditure on health, 2005 [12]
Given that the patient access to compensated drugs is conditioned by the lists of compensated drugs published by the NHIH, such inequities could probably be solved by an improved, more transparent process of selecting compensation levels and drug lists. An improved (perhaps electronic) system for checking prescriptions is needed. This should however be linked with the need for involving healthcare professionals and patient representatives.
The most recent initiative for limiting drug expenditures covered from FNUASS (entering in force in September 2011) sets limitations in the costs supported for certain national programs. According to this MoH ordinance (no. 1275/2011) the social health insurance plan will no longer support the whole market value for specific innovative drugs listed on a quarterly-updated list of drugs; instead, provided that there is an equivalent, generic drug being available on the market, the social health insurance will only cover at most 120% of the end-sale price for the cheapest equivalent generic drug on the market. However, if no equivalent generic drugs are marketed, innovative drugs will still be fully covered by social health insurance.
Although this decision is expected to limit drug expenditures, the officials made no estimates publicly available.
Solutions for better public health funding
The first and most upfront solution would be an increase in public health funding. Projections of a 2009 legislative initiative of general practitioners estimated that a rough 6% of the GDP would be the minimum financing level required for improving visibly the healthcare system functioning.
There are also talks about reconsidering the ‘financial’ issues of public health, i.e. in reconsidering public health as a long-term productivity sector (a long-term investment which brings along both increased expenditures and improved public health).
A continuous and predictable growth of public health resources, given a multi-annual budget (instead of annual budgets which need reconsidering several times a year) would probably create the adequate premises for recovering the financial deficit due to previous underfunding and should also allow future planning of investment in medical research.
Boosting the private health insurance and adequately defining the services covered by the social health insurance system might be the golden answers for additionally funding the public health system (private insurances may cover at least in part some of the expenses currently covered by social health insurance).
Additional improvements are expected if a transparent decision-making process and evidence-based management of public health financial management are further developed and implemented.
Additional funding needs to be specifically forecasted for preventive and prophylactic services; there seems to be great need for public awareness campaigns (some deficits in overall population medical background seem to exist, as proven by still ongoing ‘ancient’ practices and misconceptions).
A more effective (and less financially scavenging) approach would be the implementation of a system valuing the quality and efficacy of the medical act; the current waging policies, disregards the number of patients treated complexity of the medical case etc. Further improvements would imply allowing the healthcare personnel to diversify their offer of medical services, allowing the healthcare personnel to contract services for various employers under different health insurance coverage (different, competing, private-held health insurance systems).
As previously noted, the fall of 2011 is expected to bring legislation changes; a new health law is expected, making room for competition in the management of social health insurance funds. Promises are that, besides building a coherent environment for private hospitals (albeit legally organized as foundations or as companies) this law would also finally clearly state which healthcare services will be charge-free and which ones will be billed to the patients, who will benefit from charge-free healthcare services and which patients will have to pay for such services.
A thorough reassessment of the pack of healthcare services provided at no charge for the patient, as covered by the national social health insurance plan, and clearly identifying which services are expected to be covered by the social insurance, which additional services will be covered by long-expected private health insurances and which healthcare services are to be billed to patients, regardless of their insurance plan, as well as limiting the number of patient requests for professional care would probably limit the expenditures and provide a better coverage.
Unfortunately none of the actual, or of the proposed future measures do not seem to give the proper attention and consideration to the importance of preventive actions, and even less to the importance of prediction and personalized treatment. The approach is once again tributary to the short or mid-term vision at its best, which has been characterizing the approach of the policy making in the healthcare system.
However, even under these circumstances, there is still hope that things can be changed and improved. In this direction our organization has taken a significant step towards educating a large number of specialists in the concept of PPPM, with a specific application in the area of brain aging, where our main expertise lies.
With the funding obtained from EU, a National Educational Program, called Brain Aging Project [16], that started in 2010 and will run till 2013, will educate almost 3,000 specialists (doctors and nurses) from seven different specialties (Geriatrics, Psychiatry, Neurology, Anesthesiology, Imagery, Molecular Medicine and General Practitioners). The curricula’s have been created under the integrative approach and aim to provide all the participants with a new way of thinking about their patients.
By implementing this project it is expected that a national network of specialists in the field of brain aging, with a PPPM type mindset will be developed, thus contributing to the change of paradigm in the healthcare system from bottom-up.
Conclusions
The Romanian health systems seems to be undergoing a never-ending transition with detrimental effects on all parties involved, starting with beneficiaries (the overall population) and ending with medical staff and policy makers.
Patients lack confidence in the system, on one hand, and unfortunately this lack of trust also seems to have a negative impact on doctors and on their capabilities (i.e. technical capabilities, up-to-date knowledge base and sometimes corruption).
The medical staff is severely underpaid, which further reflects in difficult access to updated reliable medical information (since journal subscriptions, courses, access to medical conferences and specialty textbooks seems too expensive for some of them). In spite of an adequate training, many physicians seem to feel entrapped in a system which does not allow them to use their hardly-acquired knowledge in a modern environment. Physicians are sometimes overburdened with an impressive number of patients and lack nurses.
Prophylactic and preventive services seem to be a ghost of the Christmas past, since the national health insurance system no longer values (i.e. remunerate) efforts made in this direction. Under these circumstances, a significant quota of the medical personnel chooses to migrate to better working conditions, thus loosening links of an already weakened healthcare system.
Policy makers tend to disregards basic principles like anticipative planning, feedback from patients and professionals, as well as elementary desiderates of a public health system.
Although the principles of preventive, predictive and personalized medicine are obviously important, their importance seems to be only declarative; urgent measures need to be taken for translating them into actual medical practice as part of an integrated, coherent, nationwide strategy. Such a huge effort in terms of time, funds and effort seems to be the sole means for accurately anticipating and (in the future) easing the financial burden on the healthcare system.
Patient and physician representatives need to step in and take action in regulating a system, which was originally designed for them; their expectations, needs and requirements need to be carefully analyzed and (up to the greatest extent possible) met. As outlined before, elementary fine-tunings of the system may lead to a less resource-scavenging balance which, in turn, may provide required resources for improving working conditions (leading to reduced medical staff migration), improved confidence of the patients and improved primary services (including prevention and prophylaxis).
But until this stepping up will happen, those who share a clearer vision on how the future should look need to take faster action—and we believe this will prove to be the case with the national educational project that is under implementation through our organization.
Glossary
- GDP
Gross domestic product
- NHIH
National health insurance house
- MoH
Ministry of health
- PPPM
Predictive, preventive and personalized medicine
- RCoP
Romanian college of physicians
- PNESS
The national program for evaluating the health status of Romanians (Programul National de Evaluare a Starii de Sanatate)
- FNUASS
The national fund for social and health insurance (Fondul National Unitar de Asigurari Sociale si de Sanatate)
- CVD
Cardiovascular diseases
- HPV
Human papilloma virus
Footnotes
L. Spiru is National Representative of EPMA in Romania
References
- 1.Preker AS, Feachem RGA.“Market mechanisms and the health sector in Central and Eastern Europe”. World Bank Technical Paper No. 293, 1995.
- 2.2008 Romanian Statistical Yearbook, www.insse.ro. Accessed Jul 2010.
- 3.Raportul Comisiei Prezidenţiale pentru analiza şi elaborarea politicilor din domeniul sănătăţii publice din România, Bucuresti, 2008.
- 4.World Health Statistics 2010. Switzerland: WHO Press; 2010.
- 5.David I. Sănătatea ar putea avea o nouă lege. Pentru prima dată se discută despre spitale privatizate şi case de asigurări private. http://www.zf.ro/eveniment/sanatatea-ar-putea-avea-o-noua-lege-pentru-prima-data-se-discuta-despre-spitale-privatizate-si-case-de-asigurari-private-8587732. Accessed Sept 2011.
- 6.Ionescu V. Viitoarea Lege a Sănătăţii: Soluţii radicale—spargerea monopolului CNAS. Case de asigurări private, spitale-fundaţii, minister reglementator. http://cursdeguvernare.ro/viitoarea-lege-a-sanatatii-spargerea-monopolului-cnas-case-de-asigurari-private-spitale-fundatii-minister-reglementator.html. Accessed Sept 2011.
- 7.Budurcă D. Noul design al sănătăţii: case private, 1,5 miliarde de euro în plus, contracte cost-volum. Si fără scutiţi la contribuţia pentru sănătate! Medica Academica. 2011;22(3):13–5.
- 8.Ministry of Health press release, “Programul de Evaluare a Stării de Sănătate a Populaţiei, fără utilitate în sănătatea publică”, dated 05/27/2009, http://www.ms.ro/comunicate-presa-print.php?id=6643. Accessed Nov 2010.
- 9.Ministry of Health press release, “Rezultatele Programului de Evaluare a Starii de Sanatate la 1 an de la demararea acestuia”, dated 08/28/2008, http://vechi.ms.ro/comunicate-de-presa.php?com=1416. Accessed Nov 2010.
- 10.Vlădescu C, Scîntee G, Olsavszky V, Allin S, Mladovsky P. Romania: health system review. Health Syst Transit. 2008;10(3):1–172. [PubMed] [Google Scholar]
- 11.Casa Naţională de Asigurări de Sănătate. Raport de activitate 2010. -http://www.cnas.ro/informatii-publice/rapoarte-de-activitate, accessed Sep 2011.
- 12.Consumers in Europe. Luxembourg: Office for Official Publications of the European Communities; 2009.
- 13.Jitaru AA. Adio spitale de stat! http://www.telegrafonline.ro/1315774800/articol/173307/adio_spitale_de_stat.html. Accessed Sept 2011.
- 14.Mai multe spitale desfiinţate nu au fost transformate în azile de bătrâni. http://www.realitatea.net/mai-multe-spitale-desfiintate-nu-au-fost-transformate-in-azile-de-batrani_865187.html. Accessed Sept 2011.
- 15.Transformarea spitalelor în cămine pentru bătrâni, poveste fără sfârşit. http://www.antena3.ro/romania/transformarea-spitalelor-in-camine-pentru-batrani-poveste-fara-sfarsit-133009.html. Accessed Sept 2011.
- 16.Proiect European: Instruire in noile tehnologii medicale si perfectionare pentru medicii si asistentii medicalidin ambulatorii de specialitate si spitale in brain-aging—http://www.brainaging.ro/ro/proiect-european/. Accessed Nov 2011.


