Abstract
To facilitate sequence-specific detection of DNA amplified in a diagnostic reverse transcription (RT)-PCR for Lassa virus, we developed an array featuring 47 oligonucleotide probes for post-PCR hybridization of the amplicons. The array procedure may be performed with low-tech equipment and does not take longer than agarose gel detection.
TEXT
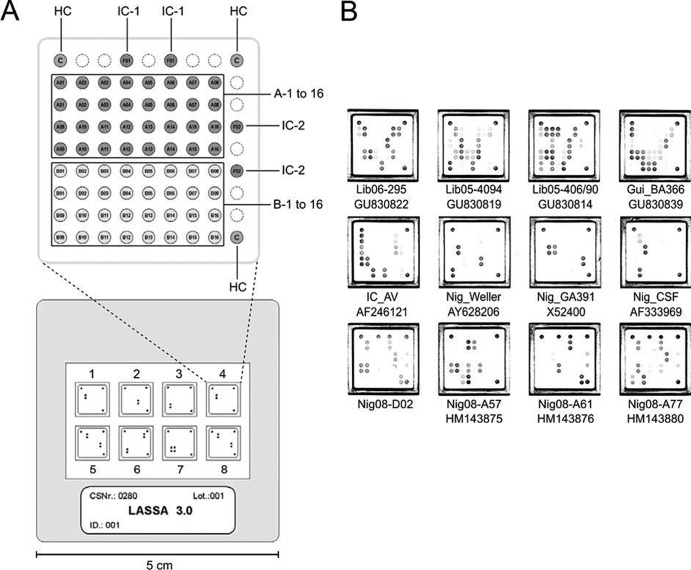
The method of choice for rapid detection of Lassa virus in blood is reverse transcription (RT)-PCR (2, 4, 7). However, the high genetic variability of the virus (1) prevents the design of probe-based real-time RT-PCR assays that reliably detect all virus strains. Current PCR assays for Lassa virus are based on agarose gel or real-time Sybr green detection. As both approaches are not sequence specific, amplified DNA is sequenced to confirm the PCR diagnosis. We have developed an oligonucleotide array for sequence-specific post-PCR hybridization of the amplicons as a rapid alternative to sequencing. The array chip is the size of a photo slide and can be scanned with a slide scanner or evaluated with a magnifying glass (Fig. 1A). It was used in conjunction with an existing RT-PCR assay targeting the glycoprotein precursor (GPC) gene of Lassa virus (5). To facilitate detection of the PCR products on the array, one primer was synthesized with a 5′ biotin and used in excess in the PCR (asymmetric PCR), thus generating biotinylated single-stranded amplicons. These were hybridized to the complementary oligonucleotide probes on the array, bound by streptavidin-horseradish peroxidase conjugate via the 5′ biotin, and detected by substrate staining. The array also offered the possibility to implement an internal control in the PCR to identify false-negative reactions.
Fig 1.
Lassa virus hybridization array. (A) The chip contains 8 wells for hybridization of 8 PCRs (lower panel), with 81 (9 × 9) spots per well for binding oligonucleotide probes (upper panel). Each spot diameter is 0.35 mm. Spots for the hybridization control (HC) are at the corners. Spots for the internal control (IC-1 and IC-2) are on the upper and right sides. The main field is divided into the upper part for 16 probes of Lassa virus set A (dark gray) and the lower part for 16 probes of Lassa virus set B (light gray). Two probes were combined at each of 15 spots, while single probes were bound at the remaining 17 spots. Each probe was spotted in duplicate for redundancy. (B) Representative patterns observed after hybridization of amplified Lassa virus sequences. Lassa virus RNA of clinical samples or in vitro transcripts of reference strains were amplified, and the amplicons were hybridized to the array. Nig08-D02, Nig08-A57, and Nig08-A77 did not match perfectly to any of the probes. The origin of each strain is indicated by a prefix: GUI, Guinea; LIB, Liberia; IC, Côte d'Ivoire; NIG, Nigeria. Available GenBank accession numbers are indicated below the strain designation.
In detail, RNA was extracted from serum by using the QIAamp Viral RNA kit (Qiagen). The 25-μl RT-PCR assay was based on the OneStep RT-PCR kit (Qiagen) and contained 1× PCR buffer, 1× Q solution, 0.4 mM deoxynucleoside triphosphates (dNTPs), 0.2 μM primer 36E2 (ACCGGGGATCCTAGGCATTT), 0.8 μM LVS-339-rev (5′-biotin-GTTCTTTGTGCAGGAMAGGGGCATKGTCAT), 0.1 μM IC-fwd (TGAACATCACGTACGCGGA), 0.4 μM IC-rev (5′-biotin-GCATGCGAGAATCTGACGC), 1 μl enzyme, 5 μl RNA, and 500 copies of in vitro-transcribed RNA of the firefly luciferase gene as an internal control. The RT-PCR was carried out at 50°C for 30 min and 95°C for 15 min, with 45 cycles of 95°C, 52°C, and 72°C for 30 s each (5). The array was custom-made by Chipron Company, Berlin, Germany. Probe sequences are listed in Table S1 in the supplemental material. The biotin-labeled PCR products (15 μl directly from the PCR tube) were mixed with 19 μl hybridization buffer (Chipron) and incubated on the array for 30 min at 37°C. The array was washed in 1× washing buffer, dried by centrifugation in a special tabletop centrifuge (Chipron), and incubated with streptavidin-horseradish peroxidase conjugate. After washing and drying, 3,3′,5,5′-tetramethylbenzidine substrate was added. The staining pattern was documented with a 35-mm slide scanner and SlideReader software (Chipron).
Within a 50-nucleotide region of the amplicon, two partially overlapping sets (A and B) of 47 total oligonucleotide probes (see Table S1 in the supplemental material) were designed using Lassa virus sequences available by the end of 2009. The melting temperature of the probes was between 40°C and 43°C to facilitate binding of amplicons at 37°C even in the presence of one or two mismatches (see Table S1 in the supplemental material).
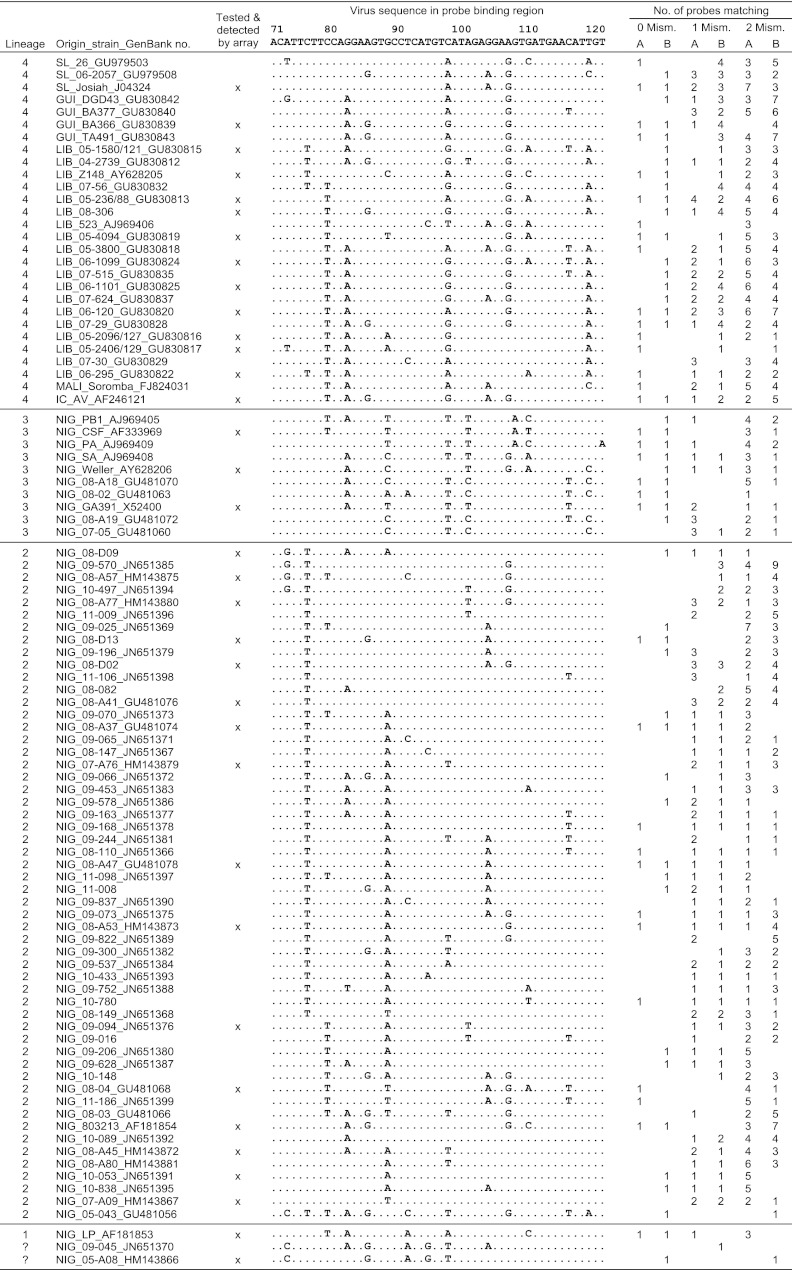
The assay was validated with serum samples from patients with laboratory-confirmed Lassa fever from Nigeria (n = 27) and Liberia (n = 49). Most of the clinical strains had previously been sequenced in the PCR target region (3, 5). In addition, in vitro transcripts of 11 reference strains were tested. Thus, the validation panel included 35 unique sequences of the probe-binding region which fairly well reflected the spectrum of known sequences (Fig. 2). All clinical and reference strains were detected by the new assay, corresponding to 100% sensitivity compared to the “gold standard.” Amplicons were detected by probes with up to two mismatches (Fig. 1B and 2). To test if all virus sequences available by the end of 2011 would probably be detected by the array, we performed an in silico analysis (Fig. 2). Out of the 60 unique sequences that were not tested experimentally, 34 showed a perfect match to a probe of set A and/or B. The rest showed one mismatch to at least one probe of set A and/or B and, with the exception of Nig09-045 (3), two mismatches to at least one probe of set A and/or B. Considering the experimental and in silico data, the array will probably detect all known sequences.
Fig 2.
Unique probe-binding sequences of Lassa virus (small [S] RNA segment positions 71 to 120) available by the end of 2011. Virus sequences that have been detected on the array are marked with an “x.” On the right, the numbers of probes on the array matching to the virus sequence with either 0, 1, or 2 mismatches are shown (columns 0 Mism., 1 Mism., and 2 Mism., respectively). For each mismatch category, the numbers of probes are shown separately for set A and set B (columns A and B, respectively). A “?” represents an unclassified new lineage (3). The origin of each strain is indicated by a prefix: SL, Sierra Leone; GUI, Guinea; LIB, Liberia; MALI, Mali; IC, Côte d'Ivoire; NIG, Nigeria.
Potential off-target sites were searched for by using BLASTN (http://blast.ncbi.nlm.nih.gov/). Each probe sequence was run as a query against all viruses (taxid, 10239; 1.3 Mio sequences), all bacteria (taxid, 2; 6.2 Mio sequences), all plasmodia (taxid, 5820; 0.4 Mio sequences), and human genome plus transcripts. No site with zero or one mismatch was found, and only 5 sites with 2 mismatches to 2 probes were found. All other probes had 3 to 9 mismatches (median, 6) to the best-matching sites (see Table S1 in the supplemental material). Given the millions of sequences representing billions of nucleotides that were browsed through and the fact that the DNA to be hybridized on the chip is preamplified with specific primers, the chance of false-positive reactions on the chip is considered to be negligible. As an experimental specificity control, 20 Lassa virus-negative serum samples were tested with the array. All samples were negative, while the internal control was positive.
The sensitivity of amplicon detection on the array was comparable to that of ethidium bromide staining in agarose gel, though spots with mismatches preferentially disappeared with decreasing amounts of PCR product (see Fig. S1 in the supplemental material). The analytical sensitivity of the whole assay was determined by replicate testing of various concentrations of in vitro-transcribed RNA spiked into human serum (Table 1). The pooled data for all strains resulted in a 95% detection limit of 1,540 Lassa virus RNA copies/ml (see Fig. S2 in the supplemental material).
Table 1.
Detection limit of GPC RT-PCR with array hybridization for different Lassa virus strains, determined by replicate testing and probit analysisa
| Lassa virus strain | Origin of strain | Genetic lineage | 95% detection limit |
|
|---|---|---|---|---|
| No. of RNA copies/ml sample | No. of RNA copies/reaction mixture | |||
| Lib05-1580/121 | Liberia | IV | 2,216 | 25.9 |
| CSF | Nigeria | III | 1,036 | 12.1 |
| GA391 | Nigeria | III | 479 | 5.6 |
| 803213 | Nigeria | II | 347 | 4.0 |
| LP | Nigeria | I | 4,295 | 50.1 |
Virus RNA was in vitro transcribed from plasmid by using the MegaScript T7 kit (Ambion, Austin, TX), purified with the RNeasy minikit (Qiagen, Hilden, Germany), and quantified spectrophotometrically. Different RNA concentrations were tested with replicates, and the corresponding fraction of positive reactions was determined. The 95% detection limit of the assay was calculated from these data by probit analysis using PriProbit version 1.63 (6).
In summary, the chip offers sequence-specific detection of Lassa virus amplicons due to hybridization to a large number of probes, a result which is not yet feasible in real-time PCR. The disadvantage is the manipulation of the amplicons outside the PCR tube, increasing the risk of contamination. Array processing has to be strictly separated from pre-PCR procedures. The assay is suitable for low-throughput testing, e.g., in laboratories that might be confronted with imported cases of Lassa virus. The low-tech equipment needed for array detection also facilitates the use of the technique in the field, where sequencing machines are usually not available.
Supplementary Material
ACKNOWLEDGMENTS
The study was supported by grant E/B41G/1G309/1A403 from the Bundesamt für Wehrtechnik und Beschaffung, grant 228292 (European Virus Archive) from the European Community, and grant I/82 191 from the Volkswagen Foundation.
The Department of Virology of the Bernhard-Nocht-Institute is a WHO Collaborating Centre for Arbovirus and Haemorrhagic Fever Reference and Research (DEU-000115).
We thank Volker Heiser of Chipron Company for fruitful discussions and support. The array can be obtained via www.chipron.com/contact.html.
Footnotes
Published ahead of print 25 April 2012
Supplemental material for this article may be found at http://jcm.asm.org/.
REFERENCES
- 1. Bowen MD, et al. 2000. Genetic diversity among Lassa virus strains. J. Virol. 74:6992–7004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Demby AH, Chamberlain J, Brown DW, Clegg CS. 1994. Early diagnosis of Lassa fever by reverse transcription-PCR. J. Clin. Microbiol. 32:2898–2903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ehichioya DU, et al. 2011. Current molecular epidemiology of Lassa virus in Nigeria. J. Clin. Microbiol. 49:1157–1161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Lunkenheimer K, Hufert FT, Schmitz H. 1990. Detection of Lassa virus RNA in specimens from patients with Lassa fever by using the polymerase chain reaction. J. Clin. Microbiol. 28:2689–2692 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ölschläger S, et al. 2010. Improved detection of Lassa virus by reverse transcription-PCR targeting the 5′ region of S RNA. J. Clin. Microbiol. 48:2009–2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Sakuma M. 1998. Probit analysis of preference data. Appl. Entomol. Zool. (Japan) 33:339–347 [Google Scholar]
- 7. Trappier SG, et al. 1993. Evaluation of the polymerase chain reaction for diagnosis of Lassa virus infection. Am. J. Trop. Med. Hyg. 49:214–221 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.