Abstract
The contribution of environmental surface contamination with pathogenic organisms to the development of health care-associated infections (HAI) has not been well defined. The microbial burden (MB) associated with commonly touched surfaces in intensive care units (ICUs) was determined by sampling six objects in 16 rooms in ICUs in three hospitals over 43 months. At month 23, copper-alloy surfaces, with inherent antimicrobial properties, were installed onto six monitored objects in 8 of 16 rooms, and the effect that this application had on the intrinsic MB present on the six objects was assessed. Census continued in rooms with and without copper for an additional 21 months. In concert with routine infection control practices, the average MB found for the six objects assessed in the clinical environment during the preintervention phase was 28 times higher (6,985 CFU/100 cm2; n = 3,977 objects sampled) than levels proposed as benign immediately after terminal cleaning (<250 CFU/100 cm2). During the intervention phase, the MB was found to be significantly lower for both the control and copper-surfaced objects. Copper was found to cause a significant (83%) reduction in the average MB found on the objects (465 CFU/100 cm2; n = 2714 objects) compared to the controls (2,674 CFU/100 cm2; n = 2,831 objects [P < 0.0001]). The introduction of copper surfaces to objects formerly covered with plastic, wood, stainless steel, and other materials found in the patient care environment significantly reduced the overall MB on a continuous basis, thereby providing a potentially safer environment for hospital patients, health care workers (HCWs), and visitors.
INTRODUCTION
Despite best efforts promoting infection control protocols (28, 33), hospital-acquired infections (HAI) remain a common complication of hospital care, occurring at an estimated rate of 2 million infections annually in the United States (30). At issue is the source of the microbes responsible for HAI. Much work has focused on the transfer of microbes from patients to health care workers (HCWs) and vice versa, and it is likely that commonly touched items serve as significant reservoirs for these microbes.
Microbes have an inherent ability to colonize any surface. Studies have shown that microbes can persist for weeks on stainless steel surfaces and polymeric materials used to fabricate touch surfaces in hospitals (22). Methicillin-resistant Staphylococcus aureus (MRSA) may exist on surfaces for as long as 360 days (37, 38), and spore-forming bacteria, including Clostridium difficile, can survive for months. The longer a nosocomial pathogen persists on a surface, the longer it may be a source for transmission to a susceptible patient or HCW (5, 13, 17, 21, 26, 29). Frequently touched surfaces such as doorknobs, push plates, bed rails, faucet handles, and poles supporting intravenous fluid supplies (IV poles) have been identified as reservoirs for the spread of pathogenic microbes (3, 27) which can easily contaminate hands and equipment of HCWs, who, in turn, can transmit these pathogens to patients during routine care.
A concentration of less than 250 aerobic CFU per 100 cm2 of surface area has been proposed as a standard for being considered benign immediately after terminal cleaning (11, 19). When the microbial burden (MB) exceeds this level, transmission from the surfaces to health care workers and/or patients likely increases. To date, while there have been multiple protocols for hand hygiene and room cleaning, there have been few strategies that can consistently minimize the MB found in the environment. CDC guidelines for disinfection and sterilization of healthcare facilities (28) describe reducing rates of HAI through appropriate use of disinfection and sterilization of the patient care environment. These guidelines incorporate a disinfection strategy devised more than 40 years ago (34) on the basis of the predicted degree of risk involved in the use of inanimate objects: “critical” risk, which includes items that enter sterile tissue (surgical instruments); “semicritical” risk, which includes items that come into contact with mucous membranes or nonintact skin (endoscopes); and “noncritical” risk, which includes items that come in contact only with skin. Environmental surfaces fall within the noncritical category (16, 31, 34). Increasing evidence suggests that enhanced cleaning/disinfection of environmental surfaces can reduce contamination of HCWs and thus reduce transmission of hospital pathogens (4). However, numerous reports indicate that a high percentage of environmental surfaces are not terminally cleaned well (7–9). When samples from objects in hospital rooms were cultured, 94% of those from rooms housing vancomycin-resistant enterococcus (VRE)-infected patients and 100% of those from rooms housing C. difficile patients were extensively contaminated with the organisms (12).
In vitro (24, 25, 39) and in vivo (10, 15, 20) studies have established the effectiveness of metallic copper surfaces as an antimicrobial material for its ability to reduce the concentration of bacteria on hard surfaces. In this study, we have expanded on these observations by characterizing the MB associated with commonly touched objects surfaced with and without copper in the intensive care unit (ICU) in order to understand the risk that the MB might represent and the benefit that a perpetually active copper material might offer in continuously reducing the MB in the built hospital environment.
MATERIALS AND METHODS
Setting.
A multisite study was conducted within the ICUs of three separate U.S. hospitals. The study was approved by the institutional review boards for all sites as well as by the Office of Risk Protection of the United States Army, the sponsor of the work. The Medical University of South Carolina (hospital 1) located in Charleston, South Carolina, is a 660-bed academic facility with 17 medical ICU beds. The Memorial Sloan Kettering Cancer Center (hospital 2) located in New York, New York, is a 432-bed cancer hospital with 20 medical-surgical ICU beds. The Ralph H. Johnson Veterans Administration Medical Center (hospital 3), also in Charleston, is a 98-bed hospital with 8 medical ICU beds.
Study design.
The MBs associated with six common, frequently touched objects with which patients, HCWs, and visitors routinely interact between daily routine cleanings (Table 1) were measured weekly for 43 months using 6 rooms each from hospitals 1 and 2 and 4 rooms from hospital 3 for a total of 16 rooms. Commencing during month 23 (intervention phase), the six objects associated with half of the study rooms were surfaced with a continuously active antimicrobial material, metallic copper, in order to determine the effect on the MB.
Table 1.
Antimicrobial copper alloys used to surface or fabricate frequently touched items
| Object | Copper alloy(s) | Component(s) fabricated | Description | % copper content |
|---|---|---|---|---|
| IV stand | C710 and C706 | Pole(s) | Copper nickel | 80 and 90 |
| C693 | IV hanger loops | Brass | 75 | |
| C87610 | Base | Silicon bronze | 90 | |
| C706 | Handle | Copper nickel | 90 | |
| C706 | Brackets | Copper nickel | 90 | |
| Patient bed—side rails | C110 | Top of rails | Copper | 99.99 |
| Over-bed table | C706 | Table top | Copper nickel | 90 |
| C110 | Table bottom | Copper | 99.9 | |
| C464 | Release lever | Naval brass | 60 | |
| Visitor chair (arms) | C706 | Arm rests | Copper nickel | 90 |
| Nurse call button | C638 | Buttons | Aluminum bronze | 80 |
| C260 | Clamshell (hospitals 1 and 3) | Cartridge brass | 80 | |
| Computer mouse | C260 | Computer mouse (hospital 2 only) | Cartridge brass | 70 |
| Data input device | C524 | Base of monitor bezel (hospitals 1 and 2) | Phosphor-bronze | 90 |
| C710 | Laptop palm rest (hospital 3 only) | Copper nickel | 80 |
Fabrication of items surfaced with copper alloys.
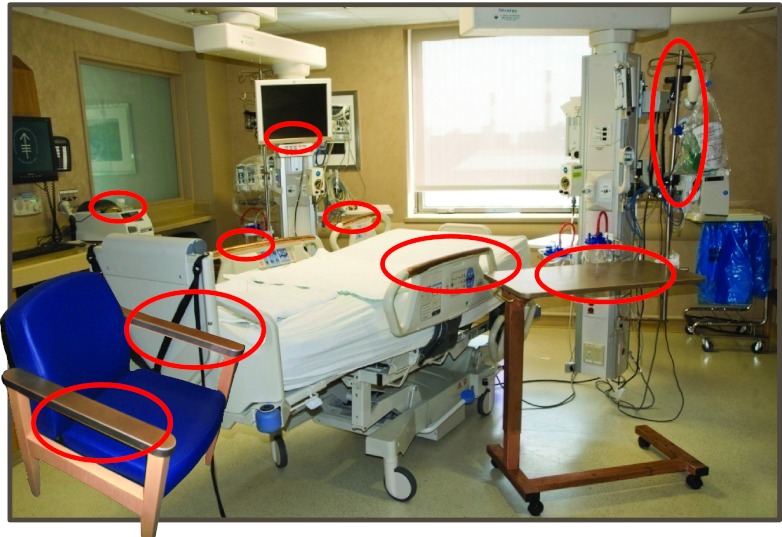
The objects surfaced with copper were fabricated using copper alloys registered with the U.S. EPA for their inherent ability to kill bacteria (36). Four items were common to all hospitals: the side rails of the patient bed, the over-bed tray table, the IV pole, and the contact surface of the arm rests of the visitor's chair (Fig. 1). Two other frequently touched objects were also sampled from each site (Table 1). For additional details on fabrication, please see the supplemental material.
Fig 1.
Representative frequently touched objects and their respective placements in the ICU.
Environmental cleaning regimens.
Each of the study sites followed routine standards of environmental cleaning and disinfection as prescribed by their respective infection control programs. This required that all objects and surfaces be cleaned at least once each day using a prescribed hospital-grade disinfectant and upon patient discharge. Three U.S. EPA-registered disinfectants were used during the intervention. Virex 256 disinfectant was used for routine and terminal cleaning. Dispatch disinfectant was used to clean rooms housing patients with a confirmed case of Clostridium difficile, and Cavicide disinfectant was used for spot cleaning. Additionally, during the preintervention phase, one site, hospital 2, used the disinfectant Elimstaph no. 2 (Walter G. Legge Company, Inc., Peekskill, NY) rather than Virex 256 for its routine and terminal cleaning. The products were all used according to the label instructions and were consistently applied.
Sample collection procedure.
Surfaces were sampled once each week, excluding weeks with U.S. federal holidays, at approximately 9 a.m. using a sterile template measuring either 10 cm by 10 cm or 4 cm by 25 cm placed over each surface. The exposed area was vigorously wiped using uniform pressure and motion, 5 strokes horizontally and 5 strokes vertically, for a total of 10 strokes. Samples were transported to Medical University of South Carolina and processed as previously described (1). MB was reported as CFU per 100 cm2. For greater detail, see materials and methods in the supplemental materials.
Calculations and statistical analysis.
The average MB of each item was calculated, and the MB of each room was determined as the sum of the MBs of the six objects within that room. The Kruskal-Wallis test was used to compare the average MBs associated with objects and rooms (EpiInfo; CDC, Atlanta, GA) between the preintervention and intervention phases as well between copper-surfaced rooms and control-surfaced rooms. A P value of ≤0.05 was considered statistically significant. The antimicrobial efficacy of copper was calculated as the difference in average MBs between copper and noncopper objects and rooms and was expressed as the percentage with which copper reduced the MB.
RESULTS
Intrinsic microbial burden found on common, frequently touched objects.
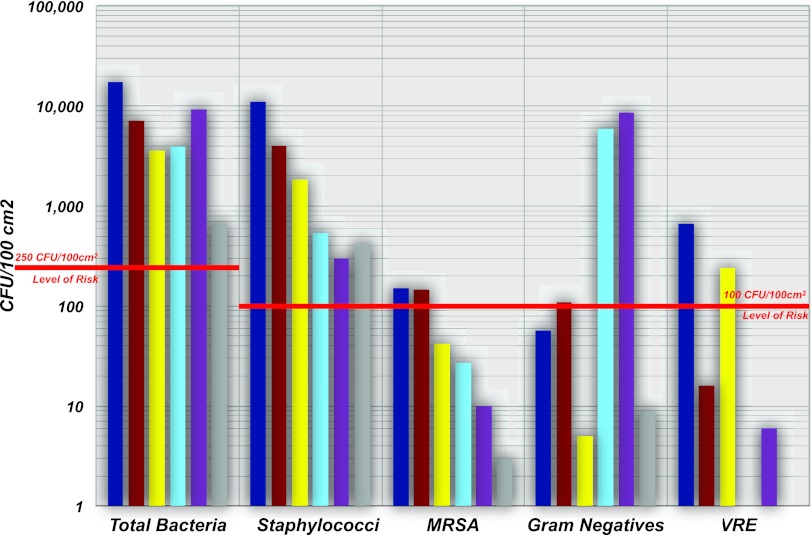
Over the 43 months of the study, samples were recovered from 9,522 objects in 1,587 rooms across three study sites. The average MB found for the six objects assessed in the clinical environment during the preintervention phase was 28 times higher (6,985 CFU/100 cm2; n = 3,977 objects sampled) than levels commonly accepted as benign, <250 CFU/100 cm2 (Fig. 2) (11, 18, 19, 23, 40). The latter value was exceeded for each object sampled. Bed rails were the most heavily burdened of the objects, averaging a concentration 69 times greater than the level proposed as benign immediately after terminal cleaning or 17,336 CFU/100 cm2, with a standard error of sampling of ±2,896 CFU/100 cm2. (For additional details, please see Table S1 in the supplemental material). The majority of microorganisms (64%) were staphylococci, and approximately 90% of the population recovered was coagulase negative.
Fig 2.
Assessment of the inherent microbial burden associated with frequently touched objects. The average concentrations of bacteria (classified by type) were determined from samples collected from six inanimate objects for a period of 23 months (n = 668 rooms). Bed rails, dark blue bars; call buttons (hospitals 1 and 3) and computer mice (hospital 2), red bars; arms of chairs, yellow bars; tray tables, light blue bars; data input devices (base of monitor bezel [hospitals 1 and 2] and palm rest of laptop computer [hospital 3]), purple bars; IV poles, gray bars. (The call button data represent values obtained from call buttons at 2 sites and from a computer mouse at the third due to the absence of a call button at that site.)
MRSA and VRE were also frequently recovered from objects. Bed rails had average concentrations of 151 CFU of MRSA/100 cm2 and of 667 VRE/100 cm2, and nurse call buttons had averages of 146 CFU of MRSA/100 cm2 and 16 CFU of VRE/100 cm2 (Fig. 2). The average concentrations of Gram-negative bacteria on bed rails and call buttons were 57 and 109 CFU/100 cm2, respectively, and the average concentrations of Gram-negative bacteria resident on the monitors and tray tables were higher at 5,914 and 8,572 CFU/100 cm2, respectively, reflecting a small number of outliers from samples collected from hospital 2.
Copper lowered the MB found on common, frequently touched objects.
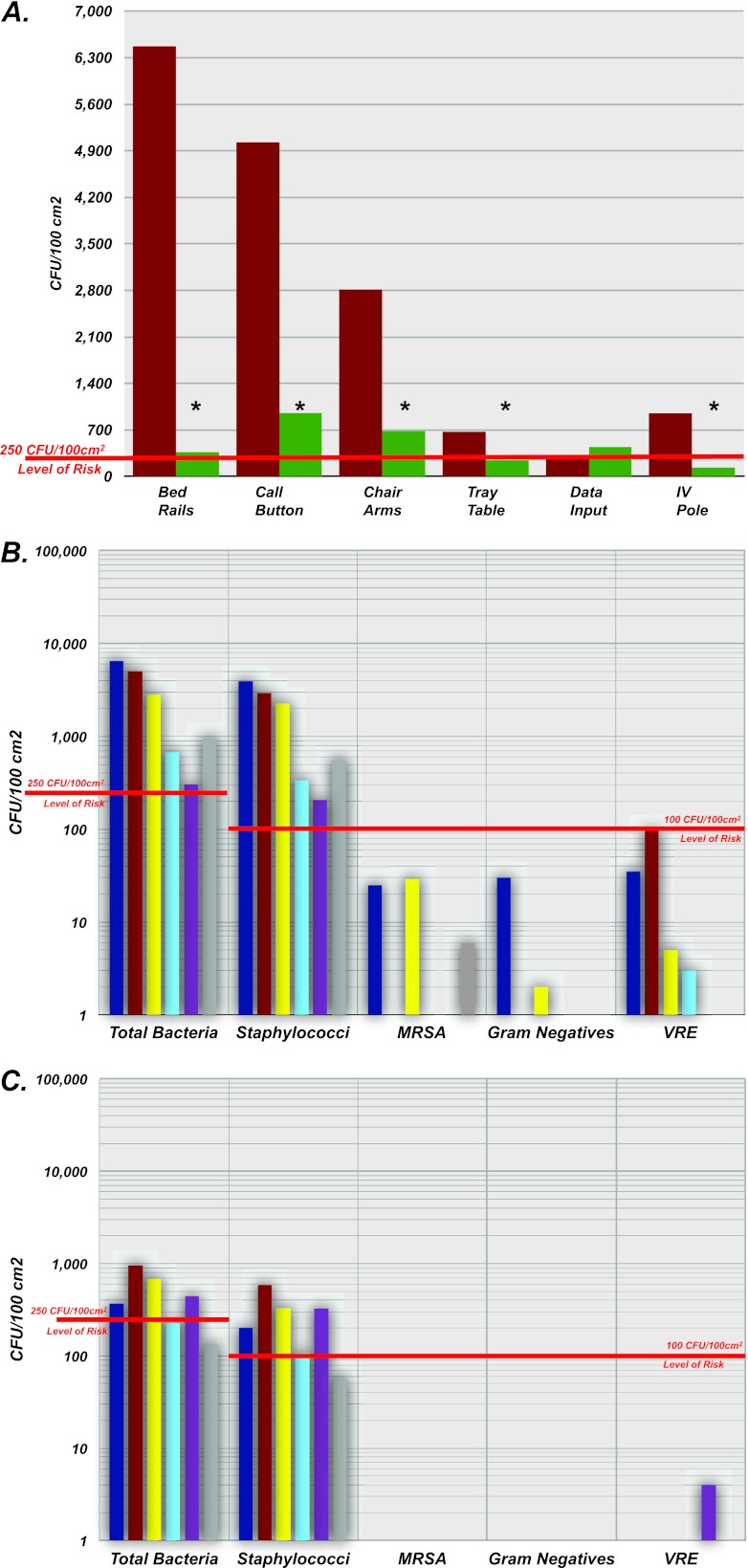
During the 21-month intervention, the antimicrobial effect exerted by metallic copper surfaces was immediate and consistently evident. A significant (83%) reduction in the average MB recovered from the copper-surfaced objects was seen. Collectively, the average MB likely to be encountered from one of the six copper-surfaced objects was 465 CFU/100 cm2 (n = 2,714 objects), while the average burden recovered from the control items was 2,674 CFU/100 cm2 (n = 2,831 objects; P < 0.0001). The summative MB average for the six objects surfaced in copper was also approximately 83% lower than the burden recovered from the control objects (2,521 versus 14,813 CFU/100 cm2) (see Table S2 in the supplemental material). Considered individually, 5 of the 6 objects surfaced in copper also saw significantly lower burdens (Fig. 3A; see also Table S2 in the supplemental material). Polypropylene bed rails were again the most heavily burdened of the control objects sampled, with an average MB of 6,456 CFU/100 cm2. In contrast, the MB recovered from copper bed rails was 94% lower (366 CFU/100 cm2) and this difference was significant (P < 0.0001). Finally, the antimicrobial activity of copper was found to be universal in its ability to kill many types of microbes (Fig. 3B and C).
Fig 3.
Copper lowered the MB found on common, frequently touched objects. (A) Comparison of the average MBs between rooms with (green bars; n = 501 rooms) and without (red bars; n = 511 rooms) copper-surfaced items. Samples were collected over a period of 21 months, processed, and statistically analyzed as described in Materials and Methods (*, P < 0.05). (B [noncopper objects] and C [copper objects]). Average concentrations of bacteria (classified by type) recovered from bed rails (dark blue bars), call buttons (hospitals 1 and 3) and computer mice (hospital 2) (red bars), arms of chairs (yellow bars), tray tables (light blue bars), data input devices (base of monitor bezel [hospitals 1 and 2] and palm rest of laptop computer [hospital 3]) (purple bars), and IV poles (gray bars). (The call button data represent values obtained from call buttons at 2 sites and from a computer mouse at the third due to the absence of a call button at that site.)
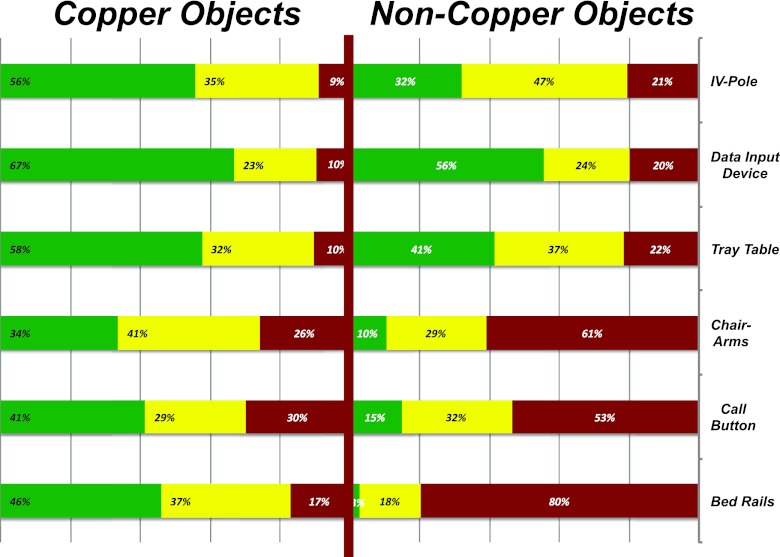
Copper surfaces were also found to attenuate the inherent variability associated with the MB resident on surfaces within the patient care areas. A total of 83% of samples recovered from copper bed rails were found to have an MB below 250 CFU/100 cm2, whereas only 20% of the samples recovered from the plastic rails were found below this level (Fig. 4), suggesting that copper might limit the heterogeneity of risk to the patient attributed to the variation in MB by limiting the range of MB resident on commonly touched surfaces. The dynamic nature of the MB resident on the objects sampled, attributed to stochastic processes, was evident throughout the trial (see Fig. S1 and S2 in the supplemental material). A comparison of the summative MBs from the preintervention and intervention phases found that the MB was 64.4% lower during the intervention period of the trial (41,586 CFU/100 cm2 [n = 668 rooms] versus 16,188 CFU/100 cm2 [n = 511 rooms]; P < 0.0001).
Fig 4.
Frequency distribution of the MB resident on all objects (classified by type) during the intervention. The MBs observed for each sample from rooms with copper-surfaced objects are represented on the left; those observed for each sample from rooms without copper-surfaced objects are represented on the right. The concentration of bacteria observed for each sample was placed into one of three categories, 0 CFU/100 cm2 (green bars), 1 to 250 CFU/100 cm2 (yellow bars), and >250 CFU/100 cm2 (red bars), and the final percentage, rounded to the nearest whole number, of each category was determined.
Effect of copper intervention on antibiotic-resistant bacteria.
Considering the frequency with which MRSA and/or VRE isolates were encountered over the study period, 169 (2.4%) of 7,005 control objects were found to harbor MRSA, while 239 (3.4%) were found to harbor VRE. During the intervention phase, MRSA and VRE were recovered with greater frequency from objects in rooms without copper surfaces. MRSA was recovered eight times (0.3%; n = 2,781 copper objects) compared to 19 times (0.63%; n = 3,004 [P = 0.0804; control]), while VRE was recovered 9 times from rooms with copper surfaces (0.3%) compared to 91 times (3%) from control rooms (P < 0.0001). On a per sample basis, copper surfaces were approximately six times less likely to harbor one of these organisms. Based on the summative MB measured for each of the surfaces sampled over the intervention period, the combined MRSA and VRE burdens were 96.8% lower on copper surfaces than on comparable plastic, wood, metal, and painted surfaces and were 98.8% lower on the bed rails, the most heavily burdened object.
DISCUSSION
The results of this study suggest that six common, frequently touched objects with which HCWs, patients, and visitors routinely interact carry a substantial MB and thus present a risk to patients. These data underscore the need to ensure that cleaning is completed in an effective manner, as bacterial concentrations resident on items sampled were well above the values recommended immediately after terminal cleaning (11, 18, 19, 23, 40). Concentrations of bacteria on objects differed substantially (Fig. 4). The stochastic behavior of the MB distributed across the three ICUs is likely attributable to the inherent dynamics of patient care, cleaning, and patient characteristics as well as to other, unknown factors.
Incorporation of inherently and continuously active antimicrobial copper onto frequently touched surfaces in the ICU offered an enhanced effect in combination with regular cleaning and infection control practices that resulted in significantly lower MB and potentially safer surfaces. Bed rails were the most heavily burdened control objects, with a maximum MB of 306,000 CFU/100 cm2, 17 times higher than the maximum value observed from a copper-surfaced rail. In fact, 80% of plastic bed rails had bacterial concentrations above the risk threshold for transferring infectious bacteria (Fig. 4). In contrast, 83% of copper bed rails had levels below this threshold. Thus, generally, during the conduct of patient care, objects surfaced with copper carried concentrations of bacteria at or below the threshold recommended immediately after terminal cleaning (11, 18, 19, 23, 40). The levels of antimicrobial activity of the metallic copper surfaces were equivalent throughout the course of the trial. This was evident from the observation that over the course of sampling, 46% of copper bedrails had no recoverable bacteria (Fig. 4). In contrast, only 3% of bed rails sampled in control rooms failed to yield viable bacteria.
Similarly, the five other copper items had remarkably lower burdens. The call button was the most heavily burdened of the copper-surfaced objects evaluated; however, 71% of the samples were below the proposed terminal cleaning threshold. The measured levels for 75% of chair arms sampled, 90% of tray tables, 91% of IV poles, and 90% of data input devices were below the proposed standard of <250 CFU/100 cm2. In total, 45% of control objects from the 511 rooms sampled exceeded an average MB considered to represent a risk to patients, compared to just 16% of copper-clad objects. The most surprising finding was the 64% decrease in MB between the preintervention and intervention phases in the control rooms. This might be accounted for as a consequence of a number of independent and uncontrolled variables: (i) the presence of copper on the unit might have resulted in better cleaning by the environmental services staff; (ii) the presence of copper might have resulted in an antimicrobial halo that limited the transfer of microbes between control rooms, as staff were common to both rooms; or (iii) variations in compliance with other infection control measures such as hand hygiene might account for the differences seen.
Unlike programs designed to improve compliance with infection control such as hand hygiene or barrier precautions, the antimicrobial activity of copper-surfaced objects was not dependent on additional training or supervision. It did not require alterations to existing cleaning practices or add to the annual environmental cleaning costs, as does the application of UV light and/or hydrogen peroxide vapor deposition for reduction in MB. Additionally, reductions to the MB manifested by the copper objects during active patient care approached the reduction level of 99.9% observed in tests conducted for registration of copper-based surfaces with the U.S. EPA.
Recent literature provides increased evidence that contaminated hospital surfaces may be a source of transmission of pathogens. Kramer et al. reported that, in hospitals, surfaces with hand contact are often contaminated with nosocomial pathogens and may serve as vectors for cross-transmission (17). Stiefel et al. found that in patient rooms with MRSA carriers, HCWs are just as likely to contaminate their hands or gloves from contact with commonly touched environmental surfaces as from direct contact with colonized patients (35). Boyce (6) demonstrated that nurses frequently acquired MRSA on their gloves after touching surfaces near colonized patients, and a report by Bhalla and others found that 53% of hand imprint cultures were positive for one or more pathogens after contact with surfaces near hospitalized patients (2). Other studies have found that patients treated in rooms previously occupied by individuals with colonization or infection with MRSA, VRE, and C. difficile are at a higher risk of acquiring the organism than patients admitted to rooms where the previous occupant did not have colonization or infection (14, 32).
The use of copper to control or reduce the MB on surfaces in health care has been previously reported (10, 15, 20). In a South African community health care facility, copper surfaces (desks, trolleys) were associated with a 71% reduction in MB compared to control surfaces when sampled every 6 weeks for a period of 6 months (20). A recent crossover study in a 19-bed acute medical ward found that many copper surfaces were associated with significantly decreased MB compared to control surfaces when sampled weekly for 24 weeks, with reductions ranging from −0.4 CFU/cm2 to −80.3 CFU/cm2 (15). Also, as was seen in our study, copper surfaces were significantly less likely to be contaminated with indicator organisms such as VRE and coliforms. Our study differs from those previous studies in several respects. Sampling in our study was performed over a substantially longer period of time (21 months), and the objects surfaced with copper were often medical devices in close proximity to the patient and used routinely during direct patient care. Additionally, the populations cared for in the rooms involved in our study were critically ill and generally not ambulatory, which reduced the influence of their interactions with other environmental surfaces within and outside the room.
Reducing the overall MB on a continuous basis with the introduction of continuously active antimicrobial copper surfaces, as evidenced in this study and others, may provide a safer environment for hospital patients, HCWs, and visitors.
Supplementary Material
ACKNOWLEDGMENTS
This work was supported by the U.S. Army Material Command (contract W81XWH-07-C-0053).
The views, opinions, and/or findings presented here are ours and should not be construed as an official position of the U.S. Department of the Army.
We acknowledge assistance and technical support from Chuck Stark, Dennis Simon, Alan Tolley, and Kathy Zolman of ATI, North Charleston, SC, and Adam Estelle, Wilton Moran, and Jim Michel of CDA.
Footnotes
Published ahead of print 2 May 2012
Supplemental material for this article may be found at http://jcm.asm.org/.
REFERENCES
- 1. Attaway HH, III, et al. 22 February 2012, posting date Intrinsic bacterial burden associated with intensive care unit hospital beds: effects of disinfection on population recovery and mitigation of potential infection risk. Am. J. Infect. Control 10.1016/j.ajic.2011.11.019 [DOI] [PubMed]
- 2. Bhalla A, et al. 2004. Acquisition of nosocomial pathogens on hands after contact with environmental surfaces near hospitalized patients. Infect. Control Hosp. Epidemiol. 25:164–167 [DOI] [PubMed] [Google Scholar]
- 3. Blythe D, Keenlyside D, Dawson SJ, Galloway A. 1998. Environmental contamination due to methicillin-resistant Staphylococcus aureus (MRSA). J. Hosp. Infect. 38:67–69 [DOI] [PubMed] [Google Scholar]
- 4. Boyce JM. 2007. Environmental contamination makes an important contribution to hospital infection. J. Hosp. Infect. 65(Suppl. 2):50–54 [DOI] [PubMed] [Google Scholar]
- 5. Boyce JM, Havill NL, Otter JA, Adams NM. 2007. Widespread environmental contamination associated with patients with diarrhea and methicillin-resistant Staphylococcus aureus colonization of the gastrointestinal tract. Infect. Control Hosp. Epidemiol. 28:1142–1147 [DOI] [PubMed] [Google Scholar]
- 6. Boyce JM, Potter-Bynoe G, Chenevert C, King T. 1997. Environmental contamination due to methicillin-resistant Staphylococcus aureus: possible infection control implications. Infect. Control Hosp. Epidemiol. 18:622–627 [PubMed] [Google Scholar]
- 7. Carling PC, Parry MF, Von Beheren SM. 2008. Identifying opportunities to enhance environmental cleaning in 23 acute care hospitals. Infect. Control Hosp. Epidemiol. 29:1–7 [DOI] [PubMed] [Google Scholar]
- 8. Carling PC, et al. 2008. Improving cleaning of the environment surrounding patients in 36 acute care hospitals. Infect. Control Hosp. Epidemiol. 29:1035–1041 [DOI] [PubMed] [Google Scholar]
- 9. Carling PC, Von Beheren S, Kim P, Woods C. 2008. Intensive care unit environmental cleaning: an evaluation in sixteen hospitals using a novel assessment tool. J. Hosp. Infect. 68:39–44 [DOI] [PubMed] [Google Scholar]
- 10. Casey AL, et al. 2010. Role of copper in reducing hospital environment contamination. J. Hosp. Infect. 74:72–77 [DOI] [PubMed] [Google Scholar]
- 11. Dancer SJ. 2004. How do we assess hospital cleaning? A proposal for microbiological standards for surface hygiene in hospitals. J. Hosp. Infect. 56:10–15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Eckstein BC, et al. 2007. Reduction of Clostridium difficile and vancomycin-resistant Enterococcus contamination of environmental surfaces after an intervention to improve cleaning methods. BMC Infect. Dis. 7:61 doi:10.1186/1471-2334-7-61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Falk PS, Winnike J, Woodmansee C, Desai M, Mayhall CG. 2000. Outbreak of vancomycin-resistant enterococci in a burn unit. Infect. Control Hosp. Epidemiol. 21:575–582 [DOI] [PubMed] [Google Scholar]
- 14. Huang SS, Platt R. 2003. Risk of methicillin-resistant Staphylococcus aureus infection after previous infection or colonization. Clin. Infect. Dis. 36:281–285 [DOI] [PubMed] [Google Scholar]
- 15. Karpanen TJ, et al. 2012. The antimicrobial efficacy of copper alloy furnishing in the clinical environment: a crossover study. Infect. Control Hosp. Epidemiol. 33:3–9 [DOI] [PubMed] [Google Scholar]
- 16. Kohn WG, et al. 2003. Guidelines for infection control in dental health-care settings—2003. MMWR Recomm. Rep. 52:1–61 [PubMed] [Google Scholar]
- 17. Kramer A, Schwebke I, Kampf G. 2006. How long do nosocomial pathogens persist on inanimate surfaces? A systematic review. BMC Infect. Dis. 6:130 doi:10.1186/1471-2334-6-130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Lewis T, Griffith C, Gallo M, Weinbren M. 2008. A modified ATP benchmark for evaluating the cleaning of some hospital environmental surfaces. J. Hosp. Infect. 69:156–163 [DOI] [PubMed] [Google Scholar]
- 19. Malik RE, Cooper RA, Griffith CJ. 2003. Use of audit tools to evaluate the efficacy of cleaning systems in hospitals. Am. J. Infect. Control 31:181–187 [DOI] [PubMed] [Google Scholar]
- 20. Marais F, Mehtar S, Chalkley L. 2010. Antimicrobial efficacy of copper touch surfaces in reducing environmental bioburden in a South African community healthcare facility. J. Hosp. Infect. 74:80–82 [DOI] [PubMed] [Google Scholar]
- 21. Martínez JA, Ruthazer R, Hansjosten K, Barefoot L, Snydman DR. 2003. Role of environmental contamination as a risk factor for acquisition of vancomycin-resistant enterococci in patients treated in a medical intensive care unit. Arch. Intern. Med. 163:1905–1912 [DOI] [PubMed] [Google Scholar]
- 22. Michels HT, Wilks SA, Noyce JO, Keevil CW. 2005. Copper alloys for human infectious disease control, p 1–11 In Proceedings of the Materials Science and Technology Conference, Copper for the 21st Century Symposium, Pittsburgh, PA, 25 to 28 September, 2005 [Google Scholar]
- 23. Mulvey D, et al. 2011. Finding a benchmark for monitoring hospital cleanliness. J. Hosp. Infect. 77:25–30 [DOI] [PubMed] [Google Scholar]
- 24. Noyce JO, Michels H, Keevil CW. 2006. Potential use of copper surfaces to reduce survival of epidemic meticillin-resistant Staphylococcus aureus in the healthcare environment. J. Hosp. Infect. 63:289–297 [DOI] [PubMed] [Google Scholar]
- 25. Noyce JO, Michels H, Keevil CW. 2006. Use of copper cast alloys to control Escherichia coli O157 cross-contamination during food processing. Appl. Environ. Microbiol. 72:4239–4244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. O'Doherty AJ, Murphy PG, Curran RA. 1989. Risk of Staphylococcus aureus transmission during ultrasound investigation. J. Ultrasound Med. 8:619–620 [DOI] [PubMed] [Google Scholar]
- 27. Oie S, Hosokawa I, Kamiya A. 2002. Contamination of room door handles by methicillin-sensitive/methicillin-resistant Staphylococcus aureus. J. Hosp. Infect. 51:140–143 [DOI] [PubMed] [Google Scholar]
- 28. Rutala WA, Weber DJ, and the Healthcare Infection Control Practices Advisory Committee (HICPAC) 2008. Guideline for disinfection and sterilization in healthcare facilities. Healthcare Infection Control Practices Advisory Committee, Centers for Disease Control and Prevention, Atlanta, GA: http://www.cdc.gov/hicpac/Disinfection_Sterilization/acknowledg.html [Google Scholar]
- 29. Schabrun S, Chipchase L. 2006. Healthcare equipment as a source of nosocomial infection: a systematic review. J. Hosp. Infect. 63:239–245 [DOI] [PubMed] [Google Scholar]
- 30. Scott RD., II 2009. The direct medical costs of healthcare-associated infections in U.S. hospitals and the benefits of prevention. Centers for Disease Control and Prevention, Atlanta, GA: http://www.cdc.gov/hai/pdfs/hai/scott_costpaper.pdf [Google Scholar]
- 31. Sehulster L, Chinn RY. 2003. Guidelines for environmental infection control in health-care facilities. Recommendations of CDC and the Healthcare Infection Control Practices Advisory Committee (HICPAC). MMWR Recomm. Rep. 52:1–42 [PubMed] [Google Scholar]
- 32. Shaughnessy MK, et al. 2011. Evaluation of hospital room assignment and acquisition of Clostridium difficile infection. Infect. Control Hosp. Epidemiol. 32:201–206 [DOI] [PubMed] [Google Scholar]
- 33. Siegel JD, Rhinehart E, Jackson M, Chiarello L. 2007. 2007 guideline for isolation precautions: preventing transmission of infectious agents in health care settings. Am. J. Infect. Control 35(Suppl. 2):S65–S164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Spaulding EH. 1968. Chemical disinfection of medical and surgical materials, p 517–531 In Lawrence C, Block SS. (ed), Disinfection, sterilization, and preservation. Lea & Febiger, Philadelphia, PA [Google Scholar]
- 35. Stiefel U, et al. 2011. Contamination of hands with methicillin-resistant Staphylococcus aureus after contact with environmental surfaces and after contact with the skin of colonized patients. Infect. Control Hosp. Epidemiol. 32:185–187 [DOI] [PubMed] [Google Scholar]
- 36. United States Environmental Protection Agency 2008. EPA registers copper-containing alloy products. United States Environmental Protection Agency, Washington, DC: http://www.epa.gov/opp00001/factsheets/copper-alloy-products.htm [Google Scholar]
- 37. Wagenvoort JH, Penders RJ. 1997. Long-term in-vitro survival of an epidemic MRSA phage-group III-29 strain. J. Hosp. Infect. 35:322–325 [DOI] [PubMed] [Google Scholar]
- 38. Wagenvoort JH, Sluijsmans W, Penders RJ. 2000. Better environmental survival of outbreak vs. sporadic MRSA isolates. J. Hosp. Infect. 45:231–234 [DOI] [PubMed] [Google Scholar]
- 39. Weaver L, Michels HT, Keevil CW. 2008. Survival of Clostridium difficile on copper and steel: futuristic options for hospital hygiene. J. Hosp. Infect. 68:145–151 [DOI] [PubMed] [Google Scholar]
- 40. White LF, Dancer SJ, Robertson C, McDonald J. 2008. Are hygiene standards useful in assessing infection risk? Am. J. Infect. Control 36:381–384 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.