Abstract
Transcatheter aortic valve implantation (TAVI) has proven to be a viable alternative for patients with symptomatic severe aortic stenosis who are at high risk for surgical aortic valve replacement. At the same time, there is increasing evidence that moderate-to-severe periprosthetic aortic regurgitation after TAVI is associated with dramatically increased mortality and morbidity. The issue of proper positioning of the valve, including the ability to reposition and recapture the device, must be dealt with before the use of TAVI can be extended to younger, healthier patients. The next generation of transcatheter heart valves will most likely address repositionability to facilitate accurate placement with additional features that minimize paravalvular leakage. Upcoming devices promise to improve outcomes and usability of current TAVI systems.
Keywords: Aortic stenosis, transcatheter aortic valve implantation, periprosthetic regurgitation, paravalvular leakage, TAVI


Introduction
With more than 60,000 implanted transcatheter heart valves in patients around the world, TAVI has been shown to be a viable treatment for patients with symptomatic severe aortic stenosis who are at high risk for traditional surgical aortic valve replacement (SAVR).1-4 The PARTNER trial was the first randomized controlled trial to demonstrate that TAVI is not inferior to SAVR in high-risk patients, since both procedures had similar rates of survival at 1 year.4 According to the German TAVI registry, approximately one-third of all implanted aortic valve prostheses in 2011 were anticipated to be transcatheter heart valves.5
Although the PARTNER trial recently underscored the value of TAVI for high-risk patients, distinct TAVI-related drawbacks have been identified, including important differences in periprocedural risks, periprosthetic aortic regurgitation (AR), and the occurrence of significant conduction disturbances. Concerns remain around the higher, mostly procedure-related incidence of paravalvular leakage compared to SAVR. Since transcatheter heart valves are implanted without sutures, using oversizing to expand a stent at the level of the aortic annulus, several etiologies can be invoked to explain periprosthetic AR after TAVI, such as heavily calcified cusps, misplacement of the prosthesis, and/or annulus-prosthesis-size mismatch. Recently published studies report an incidence of periprosthetic AR in more than 70% of all TAVI patients that is graded as moderate or severe in approximately 10% to 20% of them.4, 6-11 Since there is growing evidence that more-than-mild periprosthetic AR after TAVI is associated with dramatically increased mortality and morbidity, this issue must be addressed before TAVI can be extended to younger and healthier patients.6
This next generation of transcatheter heart valves addresses the issue of repositionability to facilitate accurate placement and include additional features to minimize paravalvular leakage, which should further improve TAVI outcomes.
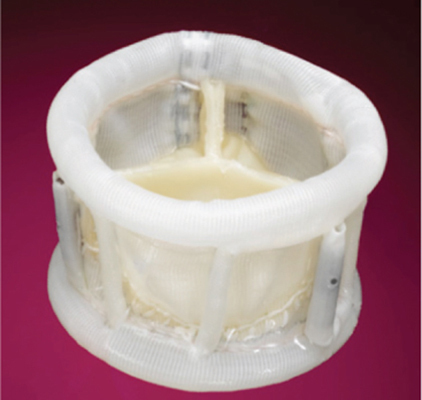
Sadra Medical Lotus™ Aortic Valve
The Sadra Medical Lotus valve (Boston Scientific, Natick, Massachusetts) consists of a tri-leaflet bovine pericardial tissue valve mounted on a braided nitinol stent structure that expands in the native annulus as it shortens (the “Chinese finger trap” principle). This deployment procedure enables a more flexible delivery system, provides radial strength, and makes repositioning or recapturing of the device possible at any time prior to release. The accurate placement of the valve is facilitated by a radiopaque center marker that allows alignment with the native valve. The preloaded prosthesis is positioned over a three-armed, self-centering system (Figure 1). An additional so-called “adaptive seal” at the lower part of the prosthesis skirt helps to conform to irregular surfaces of the native anatomy and to further reduce periprosthetic AR. The Sadra Lotus system is delivered percutaneously over an 18-Fr introducer sheath. In 2011, the REPRISE CE Mark trial with two valve sizes, 23 mm and 27 mm, was initiated in Germany, France, the United Kingdom, and Australia.
Figure 1.
Sadra Medical Lotus™ aortic valve.
Courtesy of Sadra Medical, Inc./Boston Scientific, Natick, Massachusetts.

Direct Flow Medical Aortic Valve
The Direct Flow Medical Aortic Valve (Direct Flow Medical, Santa Rosa, California) consists of a bovine pericardial tissue valve that is mounted between two inflatable polyester rings (Figure 2). These two rings are able to adapt to the native aortic annulus and the left-ventricular outflow tract to prevent periprosthetic AR. The device is delivered over an 18-Fr catheter-based, four-armed system after balloon valvuloplasty (BAV) of the native aortic valve. To better visualize the prosthesis under fluoroscopy for optimal positioning, the polyester rings of the prosthesis are filled with a mix of saline and contrast dye. Before final deployment of the valve, this fluid is exchanged against a hardening medium to firmly anchor the prosthesis in the native annulus. If necessary, the rings can be fully deflated and the valve prosthesis can be retrieved with a net basket. The profile size has been reduced from 22 Fr to 18 Fr with the second-generation transcatheter heart valve. CE Mark approval is anticipated at the end of 2012.
Figure 2.
Direct Flow Medical aortic valve.
Courtesy of Direct Flow Medical, Inc., Santa Rosa, California.
Symetis Acurate TA™ Aortic Bioprosthesis
The Symetis Acurate valve (Symetis, Lausanne, Switzerland) consists of an aortic stentless porcine valve that is mounted and sutured in a self-expanding nitinol alloy stent (Figure 3) with a Dacron interface at the lower part of the stent frame. This transcatheter heart valve comes in three sizes and can accommodate native annulus sizes of 21-27 mm. After BAV, device deployment begins with the release of the stabilization arches and the upper crown of the valve in the ascending aorta. Two radiopaque markers help deploy the valve in a proper axial position. After the upper crown has engaged the cusps of the native leaflets, the lower crown is fully expanded and anchors the new valve in the native annulus. During release, the stabilization arches self-position the device with axial alignment. The Dacron skirt at the lower valve crown provides a seal at the level of the native aortic annulus, reducing paravalvular leakage to a minimum.
Figure 3.
Symetis Acurate TA™ Aortic Bioprosthesis.
Courtesy of Symetis SA, Lausanne, Switzerland.

Symetis received CE Mark approval for the Acurate transapical TAVI system at the end of September 2011. The prosthesis has shown promising results with a 30-day survival rate of 92% in the first 90 patients.12 The commercial launch of the transapical Acurate valve took place during the European Association for Cardio-Thoracic Surgery meeting in Lisbon/Portugal in October 2011, with an initial focus on Europe. In parallel, a 150-patient, 15-center pivotal trial will be conducted in the United States. The CE Mark trial for the transfemoral version of the Symetis Acurate will be finished until August 2012.
St. Jude Medical Portico™ Aortic Valve
The Portico valve (St. Jude Medical, St. Paul, Minnesota) is comprised of leaflets made of bovine pericardial tissue that have been treated with anti-calcification technology and sutured in a nitinol self-expanding stent. This valve is designed for transfemoral (18-Fr delivery system via transfemoral sheath) and transapical use (24-Fr delivery system with integrated sheath) (Figure 4). The open cell design of the stent frame allows access to the coronaries and a low crimp profile. A tissue cuff at the lower part of the valve frame has been designed to minimize periprosthetic AR. After deployment of the valve, the prosthesis frame only minimally protrudes into the left-ventricular outflow tract, which is made possible by the low placement of the leaflets within the stent frame. This might help to reduce significant conduction system interference and the need for pacemaker implantation. The Portico valve can be completely resheathed, allowing it to be repositioned at the implant site or retrieved before it is released from the delivery system. A first-in-man study with 10 patients evaluated the technical feasibility, safety, and device deployment characteristics of the 23-mm Portico valve transfemoral delivery system. The study showed promising results at 30 days, with no device- or procedure-related adverse events or death and only trivial or no paravalvular leak. Both a European and US trial are planned for 2012.
Figure 4.
St. Jude Medical Portico™ Transcatheter Aortic Heart Valve
Courtesy of St. Jude Medical, St. Paul, Minnesota.

Edwards SAPIEN® 3 and Edwards CENTERA Aortic Valve
Edwards (Edwards Lifesciences, Irvine, California) will unveil two next-generation transcatheter heart valve platforms in 2012. The Edwards SAPIEN 3 is a lower profile, balloon-expandable valve that is designed to further reduce paravalvular leak. For percutaneous use, this valve has treated bovine pericardial tissue leaflets and is delivered through a 14-Fr sheath that might help to further reduce vascular complications. The profile for the transapical approach will also be reduced considerably. The new Edwards CENTERA valve is an ultra-low profile, self-expanding transcatheter heart valve that is repositionable and delivered with a motorized system for single operator use. First-in-man results with this device were very promising. European clinical trials for both of these new products will start in 2012.
The PARTNER II Trial, which is studying the Edwards SAPIEN XT valve in an expanded patient population, is currently underway in the United States. Enrollment in Cohort B of this trial was completed in January 2012. Enrollment also began in PARTNER II Cohort A, which is studying patients with a lower risk profile than those who were enrolled in The PARTNER Trial.
Medtronic Engager™ Aortic Valve
The Medtronic Engager aortic valve prosthesis has shown promising first results in a registered trial and will be launched soon.13 Designed for transapical use, this valve has a trileaflet bovine pericardial tissue design mounted on a self-expanding nitinol stent frame that is covered with a polyester skirt to prevent periprosthetic AR (Figure 5). In addition, this prosthesis has a low device implant height to ensure clearance from coronary ostia and positioning arms that are anchored over the native leaflets to enable optimal alignment of the valve in the native annulus and to prevent periprosthetic AR.
Figure 5.
Medtronic Engager™ Transcatheter Aortic Valve
Courtesy of Medtronic, Inc., Minneapolis, Minnesota.

JenaValve™ Aortic Valve
The JenaValve (JenaValve, Munich, Germany) consists of a porcine root valve sewn onto a Nitinol self-expanding stent (Figure 6). The JenaValve is available in three sizes (23 mm, 25 mm, and 27 mm) and covers aortic valve annuli from 21 mm to 27 mm. The Nitinol stent has three self-expanding feelers that allow the prosthesis to be accurately positioned in the aorta. Furthermore, before being sewn onto the stent, the lower part of the valve is fitted with an outer porcine pericardial skirt to minimize paravalvular leakage. The JenaValve system is fully repositionable and retrievable and is delivered transapically via a 32-Fr introducer sheath. After the feelers have been placed in the correct position in the sinuses of the native valve, the lower part of the prosthesis is released. The Nitinol stent self-expands to anchor in the native annulus, and the new valve immediately starts to function. During release, the native valve leaflets are clipped between the feelers and the base of the prosthesis. This JenaClip mechanism firmly anchors the JenaValve in the correct anatomical position and provides active fixation and resistance to migration. The delivery system can then be safely retracted. Results in 67 patients have been very promising, with a 30-day survival rate of 92%.14 JenaValve Technology received CE Mark approval for their device at the end of September 2011.
Figure 6.
JenaValve aortic valve prosthesis for transapical use
Courtesy of JenaValve™ Technology, Inc., Munich, Germany.

Conclusion
In conclusion, TAVI has been established as an alternative to surgical aortic valve replacement in inoperable and high-risk patients with severe, symptomatic aortic stenosis. Next-generation transcatheter aortic valves will facilitate the procedure and address remaining TAVI-specific drawbacks such as periprosthetic aortic regurgitation and conduction disturbance to further reduce the rate of complications. Upcoming devices promise to improve outcomes and usability of recent TAVI systems. Thus, younger and healthier individuals might benefit from TAVI in the near future.
Conflict of Interest Disclosure: All authors have completed and submitted the Methodist DeBakey Cardiovascular Journal Conflict of Interest Statement and the following was reported: Dr. Grube is a proctor for CoreValve/Medtronic.
Funding/Support: The authors have no funding disclosures.
Contributor Information
Jan-Malte Sinning, Medizinische Klinik und Poliklinik II, Universitätsklinikum Bonn, Rheinische Friedrich-Wilhelms-Universität, Bonn, Germany
Nikos Werner, Medizinische Klinik und Poliklinik II, Universitätsklinikum Bonn, Rheinische Friedrich-Wilhelms-Universität, Bonn, Germany
Georg Nickenig, Medizinische Klinik und Poliklinik II, Universitätsklinikum Bonn, Rheinische Friedrich-Wilhelms-Universität, Bonn, Germany
Eberhard Grube, Medizinische Klinik und Poliklinik II, Universitätsklinikum Bonn, Rheinische Friedrich-Wilhelms-Universität, Bonn, Germany
References
- 1.Cribier A, Eltchaninoff H, Bash A, Borenstein N, Tron C, Bauer F, et al. Percutaneous transcatheter implantation of an aortic valve prosthesis for calcific aortic stenosis: first human case description. Circulation. 2002 Dec 10;106(24):3006–8. doi: 10.1161/01.cir.0000047200.36165.b8. [DOI] [PubMed] [Google Scholar]
- 2.Grube E, Laborde JC, Gerckens U, Felderhoff T, Sauren B, Buellesfeld L, et al. Percutaneous implantation of the CoreValve self-expanding valve prosthesis in high-risk patients with aortic valve disease: the Siegburg first-in-man study. Circulation. 2006 Oct 10;114(15):1616–24. doi: 10.1161/CIRCULATIONAHA.106.639450. [DOI] [PubMed] [Google Scholar]
- 3.Leon MB, Smith CR, Mack M, Miller DC, Moses JW, Svensson LG, et al. Transcatheter aortic-valve implantation for aortic stenosis in patients who cannot undergo surgery. N Engl J Med. 2010 Oct 21;363(17):1597–607. doi: 10.1056/NEJMoa1008232. [DOI] [PubMed] [Google Scholar]
- 4.Smith CR, Leon MB, Mack MJ, Miller DC, Moses JW, Svensson LG, et al. Transcatheter versus surgical aortic-valve replacement in high-risk patients. N Engl J Med. 2011 Jun 9;364(23):2187–98. doi: 10.1056/NEJMoa1103510. [DOI] [PubMed] [Google Scholar]
- 5.Sinning JM, Walenta K, Werner N, Böhm M. Hotline update of clinical trials and registries presented at the 77th spring meeting of the German Society of Cardiology 2011. Clin Res Cardiol. 2011 Jul;100(7):553–60. doi: 10.1007/s00392-011-0325-0. [DOI] [PubMed] [Google Scholar]
- 6.Sinning JM, Hammerstingl C, Vasa-Nicotera M, Adenauer V, Lema Cachiguango SJ, Scheer AC, et al. Aortic regurgitation index defines severity of periprosthetic regurgitation and predicts outcome in patients after transcatheter aortic valve implantation. J Am Coll Cardiol. 2012 Mar 27;59(13):1134–41. doi: 10.1016/j.jacc.2011.11.048. [DOI] [PubMed] [Google Scholar]
- 7.Wenaweser P, Pilgrim T, Kadner A, Huber C, Stortecky S, Buellesfeld L, et al. Clinical outcomes of patients with severe aortic stenosis at increased surgical risk according to treatment modality. J Am Coll Cardiol. 2011 Nov 15;58(21):2151–62. doi: 10.1016/j.jacc.2011.05.063. [DOI] [PubMed] [Google Scholar]
- 8.Abdel-Wahab M, Zahn R, Horack M, Gerckens U, Schuler G, Sievert H, et al. Aortic regurgitation after transcatheter aortic valve implantation: incidence and early outcome. Results from the German transcatheter aortic valve interventions registry. Heart. 2011 Jun;97(11):899–906. doi: 10.1136/hrt.2010.217158. [DOI] [PubMed] [Google Scholar]
- 9.Sinning JM, Ghanem A, Steinhäuser H, Adenauer V, Hammerstingl C, Nickenig G, et al. Renal function as predictor of mortality in patients after percutaneous transcatheter aortic valve implantation. JACC Cardiovasc Interv. 2010 Nov;3(11):1141. doi: 10.1016/j.jcin.2010.09.009. [DOI] [PubMed] [Google Scholar]
- 10.Tamburino C, Capodanno D, Ramondo A, Petronio AS, Ettori F, Santoro G, et al. Incidence and predictors of early and late mortality after transcatheter aortic valve implantation in 663 patients with severe aortic stenosis. Circulation. 2011 Jan 25;123(3):299–308. doi: 10.1161/CIRCULATIONAHA.110.946533. [DOI] [PubMed] [Google Scholar]
- 11.Zahn R, Gerckens U, Grube E, Linke A, Sievert H, Eggebrecht H, et al. Transcatheter aortic valve implantation: first results from a multi-centre real-world registry. Eur Heart J. 2011 Jan;32(2):198–204. doi: 10.1093/eurheartj/ehq339. [DOI] [PubMed] [Google Scholar]
- 12.Kempfert J. Acurate TA: A Prospective Observational Study of a New Self-Expanding Transapical Bioprosthesis in Elderly High-Risk Patients with Aortic Stenosis. Paper presented at: TCT 2011: Transcatheter Cardiovascular Therapeutics 23rd Annual Scientific Symposium; 2011 Nov 7-11; San Francisco California. [Google Scholar]
- 13.Falk V, Walther T, Schwammenthal E, Strauch J, Aicher D, Wahlers T, et al. Transapical aortic valve implantation with a self-expanding anatomically oriented valve. Eur Heart J. 2011 Apr;32(7):878–87. doi: 10.1093/eurheartj/ehq445. [DOI] [PubMed] [Google Scholar]
- 14.Treede H. Results from the JenaValve. Second generation transcatheter aortic valve implantation system. Paper presented at: TCT 2011: Transcatheter Cardiovascular Therapeutics 23rd Annual Scientific Symposium; 2011 Nov 7-11; San Francisco California. [Google Scholar]


