Abstract
This unit describes the utility of various mouse models of infection for studying pathogenesis and adaptive immune responses to the facultative intracellular bacteria pathogen Francisella tularensis. By judicious use of different combinations of mouse and bacterial strains, as well as different routes of infection, murine tularemia models may be used to explore a complete picture of F. tularensis infection and immunity. Moreover, studies using Francisella, particularly the Live Vaccine Strain (LVS), serve as a convenient and tractable model system that appears to be representative of mammalian host responses to intracellular pathogens in general.
Keywords: Francisella tularensis, intracellular bacteria, mouse models, systemic infection, respiratory infection, biosafety issues
INTRODUCTION
A variety of mouse models of infection with the facultative intracellular bacterium Francisella tularensis are available for studying general, pathogen-specific, and tissue-specific cell-mediated immunity. This unit presents general methods (systemic, respiratory, and oral) for infecting mice with Francisella tularensis for such purposes. Francisella is not a notable public health concern, but is representative of this large and important class of human pathogens, which include Mycobacteria, Chlamydia, Salmonella, Listeria, Legionella, Brucella, and Burkholderia. Common to all are the induction of strong innate immune responses that control initial infection, followed by adaptive T cell–mediated responses that are critical for arresting and resolving both primary infection and secondary exposure. The precise nature and effectiveness of such immune responses are influenced by multiple factors, including the route and dose of the primary and secondary challenge, the virulence of the infecting strain, the site of infection, and the host genetic background. Mouse models of infection with Francisella tularensis offer unique opportunities to examine these influences and immune responses that models of infection with similar pathogens often do not. For example, some intracellular pathogens are not natural disease agents of mice, or do not readily infect other experimental animals, or must be introduced using artificial routes of infection that are not related to natural infection in humans. In contrast, F. tularensis is a highly promiscuous pathogen that naturally infects a wide variety of mammals, including humans and rodents, via multiple epithelial portals including the respiratory and gastrointestinal tracts, the skin, and the conjunctiva (Sjostedt, 2007). Regardless of the route of entry, infection is followed by dissemination to the organs of the reticuloendothelial system, including liver, spleen, lymph node, and lungs—and, in the case of lethal infection, by terminal septicemia. In particular, F. tularensis naturally infects the skin and lungs, and thus can be used to determine the requirements for protective immunity in these important tissues. The principal drawback to the use of Francisella infection of mice as an experimental model for human tularemia per se is the discrepancy between mice and humans in outcomes with particular bacterial subspecies. Specifically, two subspecies, F. tularensis tularensis and F. tularensis holarctica, are natural pathogens of humans and rodents. However, only subspecies F. tularensis tularensis can cause lethal infection in humans, especially when inhaled, whereas F. tularensis holarctica infection in humans can be severe and protracted, but is rarely if ever lethal. In contrast, all strains of inbred mice tested rapidly succumb to transdermal or respiratory infection with either subspecies at doses of <10 cfu, and with similar times to death.
The attenuated Live Vaccine Strain, LVS, of F. tularensis subspecies holarctica, is used to vaccinate humans against infection with clinical holarctica and tularensis subspecies. In the U.S., LVS is an investigational vaccine under study, and is not licensed for general use (Dennis et al., 2001). When administered to mice by certain routes, LVS behaves like fully virulent clinical isolates of this subspecies in humans. Consequently, LVS has been extensively studied in mice to reveal mechanisms of virulence as well as innate and acquired immunity (Elkins et al., 2003). As in humans, LVS administered to mice via the skin establishes a sublethal vaccinating infection and exhibits a high LD50 (>106 cfu). Showing a similarity to more limited data in humans, dermal vaccination of mice with highly attenuated LVS confers excellent long-lasting immunity against dermal challenge with fully virulent F. tularensis subspecies tularensis, but poor protection against respiratory challenge. The latter can be significantly improved by enteral or respiratory vaccination with LVS. On the other hand, LVS is quite virulent and causes a lethal disease when administered to mice via the lungs, intraperitoneally, intravenously, or intramuscularly. Thus, via these routes, LVS can also be used to examine mechanisms of acquired immunity generated by sublethal infection that allow the host to combat otherwise lethal challenge infection. Most usefully, and in contrast to clinical isolates of F. tularensis species, LVS is specifically exempt from Select Agent Registration in the U.S. and can be used under BSL-2 conditions. The present unit provides techniques for infecting mice via various routes to enable further research into the nature of protective immunity against intracellular bacteria using various strains of Francisella, but with LVS as the main example. Basic Protocol 1 describes how to systemically infect mice with F. tularensis LVS. Alternate Protocol 1 describes an infection method in which mice are injected in the ear pinna with Francisella. Basic Protocol 2 details a method for intranasal respiratory infection of mice with the organism. Similarly, a method for respiratory infection using aerosolized Francisella is described in Alternate Protocol 2. Finally, intragastric infection with Francisella is described in Basic Protocol 3. Support Protocols describe how to prepare bacterial stocks of Francisella (Support Protocols 1 and 2) and how to evaluate immune responses to the organism (Support Protocol 3).
STRATEGIC PLANNING
Because of its infectivity and historical development as a bioweapon, virulent Francisella tularensis spp. have been designated as Select Agents in the U.S. More generally, they are considered to be Biosafety Level 3 (BSL-3) pathogens in the U.S.A. and many other countries. Thus, their use is governed by regulations that are lengthy to navigate. Laboratory and biosafety practices are similar to those described for handling Mycobacterium tuberculosis (UNIT 19.5). In contrast, LVS and Francisella novicida are exempt from Select Agent registration, and require only Biosafety Level 2 conditions (APPENDIX 1V). For all experiments conducted in Animal Biosafety Level 3 (ABSL-3) facilities, the mice should be acclimated and moved into the ABSL-3 facility at least 3 to 4 days before the manipulation.
BASIC PROTOCOL 1 SYSTEMIC INFECTIONS OF MICE WITH F. tularensis
This protocol describes methods for generating sublethal and lethal infections of mice with F. tularensis via various systemic routes. Primary infection with a sublethal dose of LVS induces long-lasting, specific immunity in wild-type, immunologically competent mice against subsequent lethal infection with LVS itself, or, to a varying degree, against infection with fully virulent clinical strains of subspecies holarctica or tularensis initiated via various systemic routes. Although LVS infections can be initiated via a variety of routes, the intradermal (i.d.) and subcutaneous (s.c.) routes exhibit the highest LD50 values (i.e., ≥ 106 cfu in C57BL/6J or BALB/c mice). Thus, these routes allow the use of a wide range of doses to establish a systemic sublethal, vaccinating LVS infection. Depending on the mouse strain and infection dose, a sublethal inoculum of LVS will disseminate to the organs of the reticuloendothelial system (spleen, liver, lung, and lymph nodes), achieve peak numbers between approximately days 4 to 7, and be completely cleared from the tissues between days 14 and 21. In contrast, a lethal inoculum of LVS will kill wild-type mice between 4 and 8 days, depending on the route of infection. Lethal s.c. or i.d. infection (LD50< 10 cfu) with fully virulent clinical isolates will kill mice within ~1 week.
Materials
F. tularensis (see UNIT 14.25; also see Support Protocols 1 and 2 in this unit)
Phosphate-buffered saline (PBS), low endotoxin (Lonza, cat. no. 17-512F), sterile
Modified Mueller-Hinton agar plates (see recipe)
Naïve adult BALB/cByJ, C57BL/6J, or other suitable strains of laboratory mice
Mouse restraining device (optional)
1-ml plastic syringes, sterile
27-G, ½-in. sterile needles
Additional reagents and equipment for preparing F. tularensis frozen stocks (UNIT 14.25 and Support Protocols 1 and 2 in this unit) and parenteral injections of mice (UNIT 1.6)
NOTE: All media components and additives should be sterile, free of antibiotics, and selected from sources that rigorously quantitate and report endotoxin levels; purchase those with the lowest possible endotoxin content.
-
1
Prepare F. tularensis frozen stocks (see UNIT 14.25 and Support Protocols 1 and 2 in this unit).
Unlike some pathogenic bacterial species, it is not necessary to use actively growing cultures for infection with F. tularensis. Instead, the use of frozen, previously enumerated bacterial stocks is sufficient, and enhances consistency.
For skin infections (sublethal for LVS; lethal for virulent strains)
-
2a
Thaw a frozen stock vial, and dilute bacteria in sterile PBS to achieve the intended inoculation dose in a 100 μl-volume (e.g., to deliver 103 LVS per mouse, dilute the stock to a concentration of 103 cfu/100 μl, or 104 cfu/ml). Plate an appropriate dilution of the inoculum on modified Mueller-Hinton plates in order to verify the infecting dose retrospectively.
The choice of inoculation dose will depend on the mouse strain and the intended use for the infected mice. For LVS, an inoculation dose that is 1/100th of the LD50 will yield readily detectable cfu values in the host spleen and liver by day 7 post-infection, but does not result in significant symptoms or mortality (BALB/c mice might exhibit slightly ruffled fur and/or lethargy). However, doses as low as 102 to 103 cfu LVS will reliably provide long-term, specific immunity to lethal challenge with LVS, or lethal systemic challenge with clinical isolates. Note that with LVS, it is not uncommon for an occasional mouse to die regardless of the inoculating dose. There is no sublethal dose of fully virulent clinical isolates of Francisella. Instead, regardless or inoculum size, mice infected s.c with subspecies tularensis die within 4 to 7 days; with subspecies holarctica, mice die 1 to 2 days later. -
3a
For s.c. administration (also see UNIT 1.6), place the mouse in a mouse restraining device and inoculate 0.1 ml of diluted inoculum into the skin at the base of tail (i.e., the location where the fur of the rump ends, and the skin of the tail begins), using a 1-ml syringe and 27-G ½-in. needle.
Ideally, the needle should be angled so as to slide horizontally under the thick skin at the base of the tail, parallel to the tail such that the needle maintains a shallow depth and does not further penetrate the tissue. The 100-μl inoculum should result in a visible “bubble” under the skin that contains the injected fluid. Subcutaneous (s.c.) inoculation is an alternative method for infection that yields results similar to those obtained via the intradermal route. -
4a
For i.d. administration, grip the mouse by its scruff and tail, pulling its abdomen taut (UNIT 1.6, Fig. 1.6.1.), and shave its belly fur. Angle the needle bevel up at a shallow angle and insert into the most superficial layer of shaved skin (the needle tip should still be visible through the skin). Inject 50 μl (the maximum recommended volume for i.d. inoculation at a single site), and ensure that a bleb forms at the inoculation site. To restrict leakage, twist the syringe through 180° while removing it.
For systemic (non-skin) infections (lethal for LVS as well as all virulent strains)
-
1b
Thaw a frozen LVS stock vial and dilute bacteria in sterile PBS to achieve the intended inoculation doses as follows:
For intraperitoneal (i.p) injections, a 500-μl volume (i.e., to deliver 103 LVS per mouse, dilute the stock to a concentration of 103 cfu/500 μl, or 2 × 103 cfu/ml).
For intravenous (i.v.) injections, a 200-μl volume (i.e., to deliver 103 LVS per mouse, dilute the stock to a concentration of 103 cfu/200 μl, or 5 × 103 cfu/ml).
For intramuscular (i.m.) injections, a 100-μl volume (i.e., to deliver 103 LVS per mouse, dilute the stock to a concentration of 103 cfu/500 μl, or 2 × 103 cfu/ml).
Dilute the inoculum in PBS as needed, and plate on modified Mueller-Hinton plates in order to verify the infecting dose, as above.
-
2b
Administer the injection using standard techniques for each route of injection (see UNIT 1.6).
ALTERNATE PROTOCOL 1 EAR PINNA INFECTION OF MICE WITH F. tularensis LVS
The ear pinna provides a more straightforward site than the abdomen from which to isolate and examine immune cells that accumulate in the skin to combat infection therein. To date, this approach has been applied to sublethal infections with LVS, but rarely to infections with fully virulent clinical isolates.
Additional Materials (see Basic Protocol 1)
1-ml plastic sterile syringes and 25-G needle, sterile
0.3-ml insulin syringe fitted with 30-G needle, sterile
Flat-pronged forceps
Additional reagents and equipment for (ketamine/xylazine) anesthesia of the mouse (UNIT 1.4)
Prepare F. tularensis frozen stocks (see UNIT 14.25 and Support Protocols 1 and 2 in this unit).
Thaw a frozen stock vial, and dilute bacteria in sterile PBS to achieve the intended inoculation dose in a 10 μl volume (e.g., to deliver 103 LVS per mouse, dilute the stock to a concentration of 103 cfu/10 μl, or 105 cfu/ml). Dilute the inoculum in PBS and plate on Mueller-Hinton plates in order to verify the infecting dose.
-
Using a 1-ml syringe fitted with a 25-G needle, anesthetize the mouse by injecting 100 μl of the ketamine/xylazine solution intraperitoneally.
Ketamine/xylazine anesthesia is described in detail in UNIT 1.4. Once the mouse is anesthetized and no longer responds to a toe pinch, gently grasp the ear pinna with the forceps. Fold the pinna around the forceps once to form a taut, flat surface for injection.
Using a 0.3-cc syringe fitted with a 30-G needle, gently inject 0.01 ml of the inoculum in between the dermal sheets of the ear pinna. Immediately after injection, release the ear.
BASIC PROTOCOL 2 RESPIRATORY INFECTION OF MICE WITH Francisella VIA INTRANASAL INSTILLATION
The protocol provided here is very similar to that used for intranasal infections with influenza virus, described in UNIT 19.11. There are slight variations, such as the volume used for instillation, that have been successful used specifically for Francisella.
As with the i.p. and i.v. routes of administration, LVS is relatively lethal for mice when delivered directly to lungs by intranasal instillation, or especially when it is inhaled as a small particle aerosol, as described in Alternate Protocol 2. Thus, intranasal (i.n.) challenge with lethal doses of LVS can be used to examine potential protective mechanisms elicited by vaccination. Furthermore, to date, respiratory vaccination of LVS and other experimental tularemia vaccines elicits better protection than parenteral vaccination against a subsequent respiratory challenge with the fully virulent F. tularensis subspecies tularensis. Note also that inbred mouse strains differ in the degree to which they can be protected against respiratory challenge. Models of respiratory vaccination and challenge are therefore more useful than parenteral models for studying pulmonary immunity. This protocol describes a general method for immunizing/challenging mice intranasally with F. tularensis via the lungs. Note that mice have a relatively simple bronchial tree structure, and it is therefore widely assumed that intranasal and aerosol challenge are essentially equivalent in this species. Certainly, the LD50 of clinical strains is identical and very small (<10 cfu) by either route. However, the LD50 of LVS delivered as an aerosol is reportedly 100-fold lower than when delivered i.n.
Materials
F. tularensis (see UNIT 14.25; also see Support Protocols 1 and 2 in this unit)
Phosphate-buffered saline (PBS; APPENDIX 2A), low endotoxin, sterile
Modified Mueller-Hinton agar plates (see recipe)
Naïve adult BALB/cByJ, C57BL/6J, or other suitable strains of laboratory mice
1-ml plastic syringes and 25-G needles, sterile
Pipet with sterile tip for instillation
Additional reagents and equipment for (ketamine/xylazine) anesthesia of the mouse (UNIT 1.4)
Prepare F. tularensis frozen stocks (see UNIT 14.25 and Support Protocols 1 and 2 in this unit).
Thaw a frozen stock vial, and dilute bacteria in sterile PBS to achieve the intended inoculation dose in a 20-μl volume (e.g., to deliver 103 cfu per mouse, dilute the stock to a concentration of 103 cfu/20 μl, or 5 × 104 cfu/ml). Dilute the inoculum in PBS and plate on Mueller-Hinton plates in order to verify the infecting dose.
-
Using a 1-ml syringe fitted with a 25-G needle, anesthetize the mouse by injecting 100 to 150 μl of the ketamine/xylazine solution intraperitoneally.
Ketamine/xylazine anesthesia is described in detail in UNIT 1.4. -
Once the mouse is anesthetized and no longer responds to a toe pinch, grasp the mouse by the loose skin at the scruff, and hold upright with its head tilted back and the nose pointed up. Using a pipet with a sterile tip, administer 10 μl of the bacterial suspension to each nostril. Maintain the mouse upright for another 10 to 15 sec.
A fully anesthetized mouse will readily inhale the inoculum. If bubbles form around the nostrils, or if the mouse shows signs of respiratory stress (labored breathing), this likely indicates a failed exposure, and the mouse should be removed from the experiment or tracked separately. Place the animal on its stomach in a warm, level area. Monitor until the mouse fully regains consciousness (about 30 to 45 min).
ALTERNATE PROTOCOL 2 RESPIRATORY AEROSOL INFECTIONS OF MICE WITH Francisella
Respiratory infection can also be initiated by exposing mice to small particle aerosols (≤5.0 μm) of Francisella. Though not suitable for depositing large inocula (e.g., > 106 cfu), lethal aerosol doses of LVS or clinical subspecies can be delivered to naïve or immunized animals. One advantage of aerosol challenge over i.n. challenge (described in Basic Protocol 2) is that it allows a large number of mice to be exposed simultaneously to the inoculum without having to anesthetize them. There are two general types of apparatus that can be used to expose mice to aerosols of infectious agents. In one type (e.g., http://www.glascol.com/index.php?sid=27&cid=74), the whole mouse is exposed to an aerosol cloud; in the other type, supplied, e.g., by In-Tox Products (http://www.intoxproducts.com/exposuresystempackage), only the nose of the animal is exposed to the aerosol. Because of the technical complexities of the devices used to expose mice to aerosolized bacteria, and the likely need to customize them to each laboratory, only a general outline is provided here. For more detailed advice, the reader should contact the manufacturer or researchers active in this area.
One example of a whole-body exposure chamber is detailed in UNIT 19.5, which can expose up to 125 mice in several hours. Respiratory exposure of mice to LVS using a whole-body inhalation exposure system (i.e., a GlasCol apparatus) has also been successfully performed, in a manner similar to that commonly used for aerosol infection of mice with M. tuberculosis. The methodological details are available elsewhere in some detail (Collazo et al., 2009), but the approach has significant limitations. For unclear reasons, the LD50 of LVS via whole-body exposure was very low, approaching only 50 cfu, and clearly less than that using intranasal instillation or nose-only exposure. As a practical matter, therefore, whole-body exposure offers no advantage over intranasal or nose-only exposure, since it is very difficult to perform sublethal infections even with LVS (and presumably with more virulent strains). A major disadvantage is the potential for exposure via eyes or skin wounds, not just inhalation, since Francisella (unlike Mycobacteria) readily establishes infection via these portals. Therefore, based on the collective experience to date with this technique, it is not generally recommended for further Francisella studies.
We also have had extensive experience exposing mice to LVS and clinical isolates using a nose-only apparatus. This technique avoids the possibility of initiating infection via other portals, as discussed above. In-Tox Products, referenced above, supplies such apparatus in multiple configurations, and the authors have found it necessary to modify the commercial apparatus substantially. Thus, it is not possible to describe a general protocol for using such an apparatus. In our hands, 48 mice may be exposed simultaneously, and three independent exposures performed in a day. The entire apparatus should be permanently enclosed in a suitable biological containment chamber. The apparatus requires a supply air source capable of delivering 40 psi, a vacuum pump, and a humidifier capable of providing moist air at ≥70% relative humidity; each component must be fitted with appropriate filtration to avoid contamination with infectious aerosol.
BASIC PROTOCOL 3 INTRAGASTRIC INFECTION OF MICE WITH Francisella
Although skin- or aerosol-initiated infections are the most common forms of naturally occurring tularemia, outbreaks of water- and foodborne tularemia, due to contaminated drinking water and food, have occurred around the world, and gastrointestinal tularemia is a recognized clinical form of F. tularensis infection (Hornick et al., 1966). Experimentally, oral administration of 1010 cfu of virulent type A F. tularensis to human volunteers resulted in enlarged painful cervical lymph nodes, and all recipients required prompt antibiotic therapy to prevent further morbidity (Hornick et al., 1966). Oral inoculation of mice with virulent Francisella can therefore be used to study the pathogenesis of water- and food-borne tularemia (KuoLee et al., 2007a). In addition, oral inoculation of mice with sublethal doses of LVS or F. novicida induces both mucosal and systemic specific immune responses, and protects mice against respiratory challenge with the highly virulent type A F. tularensis (KuoLee et al., 2007b; Cong et al., 2009; Ray et al., 2009). Thus, oral infection with less virulent Francisella strains (such as LVS and F. novicida) can also be used as a model of mucosal immunization. A method of oral exposure to Francisella is presented below. Note that intragastric inoculation avoids potential exposure to the oropharynx that might occur from eating or drinking contaminated food, and which could affect both pathogenesis and immunity. However, intragastric inoculation is necessary to study the effects of GI-tract infection and immunity in isolation from potential confounding factors arising from true orally initiated infection.
Materials
Naïve adult BALB/cByJ, C57BL/6J, or other suitable strains of laboratory mice
F. tularensis LVS bacteria (see UNIT 14.25; also see Support Protocols 1 and 2 in this unit)
Phosphate-buffered saline (PBS; APPENDIX 2A), low endotoxin, sterile
Alcohol wipes
Modified Mueller-Hinton agar plates (see recipe)
Sterile stainless steel 18-G, 2-in. (5.1 cm) curved gavage needle (Harvard Apparatus or equivalent); note that if gavage is performed on young mice, a smaller-sized gavage needle or feeding tube will be required
1-ml tuberculin syringe
Additional reagents and equipment for evaluation of immune responses to Francisella (Support Protocol 3)
-
On the experimental day, fast animals for several hours, if desired.
Fasting and neutralization of gastric acid do not appear to be essential for successful infection by virulent F. tularensis strains. -
Prepare the F. tularensis inoculum by diluting bacterial stock with PBS, and adjust to desired final concentration of inoculum (106 to 1010 cfu per 0.2 ml, or 5 × 106 to 5 × 1010 cfu/ml).
Always use a freshly prepared inoculum. Multiple inoculations are not essential to ensure that all animals are infected. Fit the gavage needle to a 1-ml tuberculin syringe and fill the syringe with 1.0 ml of bacterial suspension prepared in step 2 (for use on five mice). Wipe the gavage needle with an alcohol wipe to remove any residual bacterial cells on the outside surface of the needle.
-
Stretch a fully conscious mouse by holding its tail and allowing it to grasp a stainless steel cage top with its forelegs. Pull gently on the tail with one hand, and grasp the mouse firmly by the scruff of the neck with the other hand, using thumb and index finger, so that the forelegs are extended out to the side, preventing the front feet from pushing the gavage needle away.
Sedation or anesthesia of mice for this procedure is unnecessary for trained, experienced personnel; the procedure should generally be completed in less than 5 sec with only minimal discomfort to the animal (due to restraint). Lift the mouse from the cage top and secure the tail between the palm and little finger of the hand holding the mouse, freeing the other hand for gavage.
-
Gently pull the head back and immobilize it so as to create a straight line through the neck and esophagus, while placing the gavage needle in one side of the mouth, over the tongue. Advance the needle towards the pharynx. Pivot up the tuberculin syringe such that the syringe is parallel to the body of the animal, then gently pass the needle down the esophagus in one smooth motion. Slowly deliver 0.2 ml of the bacterial inoculum.
If there is any resistance, do not force the needle. Pull the needle out and try again. This is particularly important with younger animals (<15 g). Gently press the tip of gavage needle over the pharynx a few times while advancing the needle to provoke the mouse to swallow. -
After administering the inoculum, pull back on the syringe plunger slightly before removing the gavage needle, gently following the same angle as used for insertion.
The intragastric inoculation (oral gavaging) per se should take less than 1 min including syringe filling with the bacterial inoculum, mouse restraint, and inoculum administration.If small amounts of bacterial suspension are inadvertently introduced into the trachea and the mouse exhibits breathing problems, the mouse should be euthanized, since any results from resuscitated animals may reflect a combination of oral and respiratory infection. Observe the mouse for a regular breathing pattern for 1 to 2 min, to ensure proper delivery of the inoculum into the stomach.
Return the animal to the cage and monitor for 5 to 10 min, looking for any signs of labored breathing or distress. Monitor animals again between 12 and 24 hr after dosing.
Dilute an aliquot of the inoculum in PBS, and plate on Mueller-Hinton plates in order to verify the infecting dose.
-
At predesignated time points, sacrifice mice and assess the progression of infection and/or immune responses (see Support Protocol 3).
Alternatively, challenge LVS- or F. novicida–vaccinated mice ≥6 weeks later with an appropriate F. tularensis strain and dose for the evaluation of protective immunity.
PREPARATION OF Francisella BACTERIAL STOCKS
Support Protocols 1 and 2, below, describe how to culture Francisella tularensis using commercially available sources of the organism. See UNIT 14.20 for protocols for the preparation of F. tularensis LVS bacterial stocks and associated quality-control testing of the stocks prior to in vivo use.
Support Protocols 1 and 2, below, briefly describe how to culture Francisella. See UNIT 14.20 for detailed protocols for the preparation of F. tularensis LVS bacterial stocks and associated quality-control testing of the stocks prior to in vivo use.
SUPPORT PROTOCOL 1 Preparation of F. tularensis (e.g., LVS) Working Stocks
To prepare working bacterial stocks of F. tularensis, e.g., LVS, streak out the original master stock of viable bacteria on MH agar plates. Pick a typical isolated colony for further expansion, and inoculate into a 250-ml Erlenmeyer flask containing 50 ml of modified Mueller-Hinton (MH) broth (see recipe), prewarmed in a 5% CO2 incubator. Incubate broth cultures at 37°C with gentle shaking until they reach early-to-mid-log phase (an OD600 of 0.25 to 0.4; ~8 to 10 hr). For use as infection stocks, Francisella can be frozen in broth without glycerol and stored at −80°C, with minimal loss in viability, for over 2 years. Longer-term stocks should be frozen in broth with 2.6% gelatin or 10% glycerol. Aliquots of frozen stocks are thawed and enumerated by dilution in PBS and plating on modified MH plates to determine colony-forming units. An aliquot should be thawed after freezing, counted for cfu, and tested for viability and lethality before use (see UNIT 14.20 for quality-control procedures).
F. tularensis subspecies tularensis strain SCHU S4, and other F. tularensis subspecies holarctica strains, are available to qualified laboratories from BEI Resources (http://www.beiresources.org/). Stocks are prepared in the same way as stocks of LVS (see UNIT 14.20).
SUPPORT PROTOCOL 2 Preparation of F. novicida Bacterial Stocks
F. novicida is currently available from BEI Resources (http://www.beiresources.org/) or ATCC, and also available from multiple research laboratories. Although morphologically similar to F. tularensis subspecies tularensis and holarctica, F. novicida is less fastidious than these other tularensis subspecies. While growth of all tularensis subspecies is markedly enhanced by cysteine, F. novicida growth is considerably faster than that of the other subspecies, producing visible colonies plates within 24 to 48 hours, as opposed to 72 to 96 hours for F. tularensis subspecies). F. novicida does not exhibit phase variation and does not appear to be otherwise altered during different phases of growth, and thus growth to high densities is acceptable. A wide variety of solid and liquid media containing cysteine can support the growth of F. novicida, including tryptic soy broth or agar supplemented with 0.1% cysteine (TSB-C or TSA-C, respectively), as well as modified Mueller-Hinton broth or agar. The intraperitoneal and intranasal LD50 of F. novicida in male BALB/cByJ mice should approach a single cfu.
SUPPORT PROTOCOL 3 EVALUATION OF IMMUNE RESPONSES TO Francisella
Typically, Francisella-immune lymphocytes and sera are obtained from mice that have resolved a sublethal vaccinating infection with LVS. There are a variety of published methods for assessing the nature of the immune response, most of which are similar to those used for assessing T cell and antibody responses to other intracellular pathogens. Briefly:
-
Determination of systemic bacterial burdens in vivo: On selected days after infection (e.g., days 1, 3, 7, 10, 14, and 21), dissect the spleen, liver, lung, and skin patches, and homogenize in 5 ml PBS (10 ml for liver). Organs may be homogenized using commercially available devices that provide suitable containment of the tissue (e.g., a Stomacher Lab Blender made by Seward, with sterile disposable bags; http://www.seward.co.uk/). For skin, disinfect the surface of a shaved area of skin with 70% ethanol, and then cut out a 1-cm2 section; if the inoculation site is of interest, cut such that the inoculation site is the center (between 3 to 8 days after infection, this area should be overtly inflamed). Note that Francisella is extremely susceptible to ethanol, so the skin should be washed with PBS after alcohol treatment and also submerged in 10 ml sterile PBS immediately after dissection (to neutralize any residue). The skin is a more difficult tissue to homogenize than liver, spleen, and lungs, and should first be minced with scissors. Perform 1:10 serial dilutions of the lysates in PBS (changing pipets or tips between dilutions), and plate 100 μl of a range of dilutions (in triplicate) as needed to achieve countable numbers of bacterial colonies (<100 cfu per plate section). Incubate plates for 2 to 3 days at 37°C in 5% CO2 humidified atmosphere.
Depending on the time point, dilutions ranging from 10−1 to 10−6 may be needed. Determination of anti-Francisella antibody responses: Antibody responses in body fluids (sera and bronchial lavage) may be assessed using conventional ELISA (Rhinehart-Jones et al., 1994) with plates coated with whole bacteria (i.e., LVS), Francisella LPS, and purified bacterial proteins, and developed with anti-IgM, anti-IgG, and anti-IgG secondary antibodies. Serum anti-LVS responses typically contain large amounts of anti-Francisella IgM (much of which reacts with the LPS) and IgG (dominated by IgG2a/2c).
-
Determination of Francisella-specific T cell functions and cytokine production: Specific responses of CD4+, CD8+, and “double negative” T cells can be assessed by determining the ability of whole or selected T cell subpopulations to control the intramacrophage growth of Francisella (see UNIT 14.25).
Although methods are less well developed, cytokine responses can also be detected via intracellular cytokine staining or secretion into supernatants by ex vivo stimulation with killed bacteria (See Chapter 6). Methods for demonstration of proliferative responses or cytotoxic T cell functions have been reported, but are not in common use.
REAGENTS AND SOLUTIONS
Use deionized, distilled water in all recipes and protocol steps. For common stock solutions, see APPENDIX 2A; for suppliers, see APPENDIX 5. Recipes for modified Mueller-Hinton agar plates and broth are also provided in UNIT 14.20.
Mueller-Hinton agar plates
21 g dehydrated Mueller-Hinton Broth (BD Difco)
5 g NaCl
10 g Proteose Peptone/Tryptone (BD Difco)
16 g Bacto-Agar (BD Difco)
950 ml deionized, distilled water
To prepare plates, mix the ingredients above in a large glass flask; stir and dissolve on hot plate until just boiling (watch carefully). Autoclave on liquid cycle at 121°C for 25 min. Place flask in a 56°C water bath and allow to cool before aseptically adding 10 ml of sterile 10% (w/v) glucose; 10 ml of sterile 2.5% (w/v) ferric pyrophosphate; 20 ml reconstituted, sterile IsoVitalex or Supplement VX (BD Difco ); and 25 ml sterile serum (calf or horse). Pour plates quickly in a biosafety cabinet, ~15 ml medium for plain plate, and ~20 ml (5 ml per quad) for quad plates. Allow the plates to solidify with the lids half-way off, then dry thoroughly, until no visible moisture remains on the surface of the agar (~1 hr). Store up to 1 month at 4°C, and dry again immediately before use.
Recipe adapted from Baker et al. (1985).
Mueller-Hinton broth
10.5 g dehydrated Mueller-Hinton Broth
0.69 g anhydrous CaCl2 (or 0.091 g CaCl2·2H2O)
0.105 g MgCl2·6H2O
490 ml deionized, distilled water
To prepare broth, mix the above ingredients in a large glass flask; stir and dissolve on hot plate until just boiling (watch carefully). Autoclave on liquid cycle at 121°C for 25 min. Place in a 56°C water bath and allow to cool before aseptically adding 5 ml of sterile 10% glucose, 5 ml of sterile 2.5% ferric pyrophosphate, and 10 ml reconstituted, sterile IsoVitalex or Supplement VX (BD Difco). Aliquot into 50-ml tubes, and up to 1 month at 4°C.
COMMENTARY
Background Information
In this unit, protocols for infecting mice via various routes with the facultative intracellular bacterium Francisella tularensis have been described. Similar approaches have been applied to many intracellular pathogens, particularly Listeria monocytogenes. As noted in the introduction to this unit, and elsewhere, murine infections with Francisella have a number of advantages as a means of studying immunity to intracellular pathogens generally, and, of course, provide approaches to studying immunity toward Francisella itself.
Francisella tularensis subspecies tularensis and holarctica are highly virulent for humans and many other mammalian species. These bacteria cause a spectrum of diseases collectively called tularemia, although there is a great deal of heterogeneity in the presentation of disease (Sjostedt, 2007). Infection initiated via the skin from insect bites or direct exposure to the pathogen is the most common, resulting in a characteristic ulcer and local lymphadenopathy; the course of infection, particularly with F. tularensis subspecies holarctica, may be protracted but is rarely lethal. In contrast, inhalation of F. tularensis subspecies tularensis gives rise to a more fulminant infection, starting with vague flu-like symptoms but rapidly and frequently progressing to fatal disease when untreated. This property made it attractive to develop subspecies tularensis as a biological weapon in the mid-20th century by both the U.S.A. and former U.S.S.R. (Dennis et al., 2001).
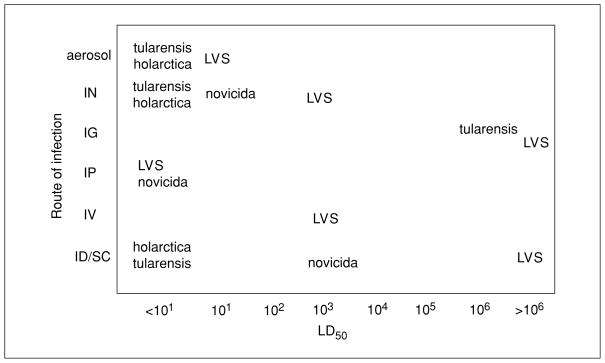
The choice of Francisella strain for use in mouse infections rests on both the scientific questions at issue and practical considerations (see Fig. 19.14.1). Clinical strains of F. tularensis subspecies tularensis and holarctica are highly infectious, and primary infection of mice initiated by any parenteral route is rapidly lethal at any dose for both immunocompetent and immunocompromised mice. Thus, mouse models of primary infection with clinical isolates cannot be readily used to study either innate immunity or to generate acquired immunity to re-infection. Note, however, that strategies for “rescuing” both wild-type and immunocompromised mice to permit survival of infection with either LVS or fully virulent Francisella, by in vivo treatment with antibiotics, have been recently reported (Elkins et al., 2010; Klimpel et al., 2008). Such approaches may be applied to expand the options for future studies of infection and immunity. Nevertheless, clinical strains require handling under BSL-3 conditions, and because of the association with bioterrorism are subject to Select Agent registration in the U.S. (http://www.selectagents.gov/). This heavily restricts their utility as model intra-cellular pathogens, and they are not recommended for this purpose. However, they are likely critical for a complete understanding of F. tularensis infection and immunity, since the behavior of less virulent strains or subspecies cannot be assumed to fully predict that of clinical isolates. In this regard, their greatest utility is as challenge organisms for putatively immune mice. Note that mice that are immune to lethal doses of LVS might succumb to challenge with clinical isolates. However, mice that fail to resist lethal challenge with LVS are unlikely to survive challenge with more virulent strains of the pathogen. Thus, immunity to lethal LVS infection can be used to pre-screen mice for their potential immunity against fully virulent clinical strains.
Figure 19.14.1.
Relative virulence of Francisella subspecies for mice by different routes of infection. The subspecies name is placed at the intersection of the route and the approximate corresponding LD50
LVS and F. novicida are exempt from Select Agent registration, and thus serve as potentially more useful model intracellular pathogens. However, in mouse models of infection, F. novicida may not be representative of either other Francisella species, or of intra-cellular pathogens in general. Thus, although F. novicida exhibits very low virulence for humans, F. novicida is relatively virulent for mice by all routes, and mice infected with F. novicida die faster than mice infected with clinical strains of subspecies holarctica and tularensis. This could be related to the observations that in mice, F. novicida is very pro-inflammatory compared to F. tularensis. Furthermore, various studies suggest that survival of mice following both primary and secondary F. novicida infections is much more dependent on antibodies and B cells than F. tularensis or other intracellular bacteria (Elkins et al., 2007; Ray et al., 2009). However, F. novicida is highly amenable to genetic manipulation, and has been successfully used to identify virulence factors common to it and F. tularensis. Thus, determining whether mutant strains of F. novicida are attenuated in mice is one approach to identifying potential virulence factors of F. tularensis.
Mouse models of infection with LVS have served well for more than 25 years for studying both Francisella-specific and more general mechanisms of intracellular parasitism and immunity. Indeed, they have been used to identify several unique host defense mechanisms that could be important for defense against other intracellular pathogens. Comprehensive reviews of the utility of the LVS mouse models for general and specific infection and immunity studies are available elsewhere (Elkins et al., 2003). The choice of route of infection relates to the pathogenesis and immunity questions of interest, and the target tissues desired for study. Mice infected with LVS by systemic routes universally exhibit infection in the spleen and liver before dissemination to the lungs, which may be quite limited when low doses are used. For infections initiated via the skin (i.d. and s.c), bacteria and responding cells can be readily recovered from patches of skin dissected from the injection site, as well as from skin removed at some distance from the injection (Elkins et al., unpub. observ.). Similarly, the peritoneal cavity of mice contains bacteria, infected macrophages, and responding cells within hours after i.p. infection. Mice infected by any respiratory approach, of course, exhibit a fulminant lung infection well in advance of dissemination out of the lung to the liver and spleen, probably via draining lymph nodes. It should be noted that infection and cell populations in lymph nodes have only infrequently been studied in Francisella-infected mice, probably due to practical limitations: unlike many infections, and in contrast to human infections, lymph node enlargement is not especially prominent, and little tissue or cells for study are recovered from infected mice.
LVS administered via the skin causes a systemic infection in mice similar to that caused by virulent holarctica strains in humans. LVS administered via the skin is highly attenuated for normal mice, but can be as virulent as wild-type F. tularensis subspecies holarctica and tularensis in immunocompromised mice, thereby providing insights into potential mechanisms of innate immunity in humans (Elkins et al., 2003). For example, T cell–deficient (or athymic) mice given an i.d. dose of LVS that is sublethal for wild-type mice survive initial LVS infection, but die after about a month. The time to death decreases to about 3 weeks in mice lacking all lymphocytes (RAG or scid mice). However, the initial 3- to 4-week survival period illustrates the development of powerful innate immune responses characteristic of reactions to intracellular infections. Studies using depletion and various knockout mice indicate that these include TNF-α, IFN-γ, and neutrophils, and that survival was further dependent on MyD88. The associated MyD88-linked ligands involved clearly include TLR-2, but neither TLR-2 nor other conventional TLRs appear to account entirely for the absolute requirement for MyD88 for survival of all strains of Francisella by all routes tested to date. As in humans, LVS administered through the skin can immunize mice against systemic challenge with the virulent subspecies holarctica and tularensis. Thus, mice vaccinated with LVS can be used to determine the plethora of immune responses elicited and their relative contributions to protection. For instance, various T cell phenotypes and the soluble mediators of CMI they produce have been shown to enhance the ability of macrophages to kill LVS. Moreover, neutralizing several of these factors has been shown to severely inhibit the ability of macrophages to kill LVS in vitro and to abolish protection in vivo against subsequent lethal infection with LVS or wild-type bacteria.
Although LVS is highly attenuated when given via the skin, it is highly virulent when given i.p. (LD50 < 1 cfu). This property can be exploited for a variety of purposes. For instance, LVS given i.p. has been used to identify a rapidly elicited B cell–dependent mechanism of host defense that can protect mice from a subsequent large, lethal i.p. LVS challenge. Primary i.p. challenge can also be used to identify critical virulence factors common to LVS and clinical strains of the pathogen; several mutants of LVS have been shown to be highly attenuated for infection of mice via the i.p. route, and the same virulence factors have been shown to be critical for the virulence of wild-type subspecies tularensis.
LVS is moderately virulent for mice when administered intranasally (LD50, ~103 cfu). Thus, it is possible to use this approach to establish both sublethal and lethal infections, as well as to demonstrate acquired immunity to secondary infection in immunized mice (by challenging them intranasally with LVS at doses that are exponentially greater than those required to kill naïve mice). Moreover, vaccinating mice i.n. with LVS elicits a more potent immune response to respiratory challenge with virulent subspecies tularensis than i.d. immunization. Therefore, i.n. vaccination is a better choice than i.d. vaccination for studies designed to determine mechanisms of defense against respiratory tularemia. Oral vaccination with LVS also elicits better protection than i.d. vaccination against respiratory challenge. On the other hand, a highly attenuated mutant of F. novicida elicited cross-protection to respiratory challenge with subspecies tularensis when administered orally, but not when administered nasally (Cong et al., 2009).
Most studies of infection and immunity using LVS in the literature have used C57BL/6J, BALB/c, or C3H mice. There are differences in susceptibility between inbred strains of mice, but these appear to be subtle and on a continuum (Anthony et al., 1988), without evidence for obvious single gene influences (such as the TLR4 defect in C3H/HeJ mice, the well known Nramp1 gene, or the genes implicated in murine susceptibility to Mycobacteria). However, A/J mice are noticeably more susceptible to i.d. LVS infection than all other common mouse strains that have been examined. Additionally, there is a clear difference between BALB/c and C57BL/6J mice in terms of the ability of LVS to provide protection against lethal challenge with fully virulent F. tularensis of either subspecies: while aerosol vaccination with LVS provides reasonable protection of BALB/c mice against subsequent lethal respiratory challenge with F. tularensis, C57BL/6J mice have been much more difficult to protect (Shen et al., 2004; Wu et al., 2005). These observations, which are somewhat paradoxical given the well-known propensity of C57BL/6J mice toward Th1 T cell responses, lack an obvious explanation and remain under study.
Many parenteral studies with LVS have preferred the use of male mice over females, for two reasons. First, the most convenient route of lethal challenge is i.p., but macrophages in the peritoneum of female mice, which have a very short estrous cycle, fluctuate almost constantly under the influence of reproductive hormones; lethality and time to death of i.p. challenges is therefore somewhat more consistent and reproducible in male mice. Second, female mice exhibit about a 10-fold increase in the LD50 of LVS, as well as increased variability in lethality and time to death by almost all routes, which must be taken into account in the experimental design. However, there does not appear to be much if any difference in LD50 or time to death between male and female mice when respiratory routes of infection are used, and thus both sexes have been used for aerosol studies with LVS. With regard to age, adult mice between the ages of about 7 weeks to 4 to 5 months appear to have comparable survival outcomes and immune responses. However, we have recently noted an obvious influence of age in the intranasal LD50 for LVS in C57BL/6J mice; mice between 6 and 8 weeks of age exhibited an LD50 of ~5 × 103, but mice 4 months old had an LD50 approaching 105. Thus, caution in choosing ages of mice for respiratory infections is recommended. As in all murine studies, strict attention to gender and age-matching of all mice within an experiment and associated control mice is necessary and critical to appropriate interpretations.
At this time, there are two chief limitations to the LVS infection model as a general means to study T cell responses in vivo. First, no obvious dominant antigens or epitopes have been described; instead, the available evidence, which is limited, suggests that LVS-immune T cells recognize a wide range of proteins. Correspondingly, tetramers to follow particular LVS-specific T cells have not yet been developed. Although an important CD4+ epitope of a protein denoted TUL4 has been described, attempts to create stable tetramers have not yet been successful. Second, while transfer of serum or monoclonal antibodies to Francisella has reduced susceptibility to infection in several circumstances, the adoptive-transfer model used to study LVS-specific T cells is suboptimal. The approach that has been used relies on intraperitoneal transfer of enriched whole T cells or T cell subpopulations, followed by intraperitoneal challenge with a lethal dose of LVS. Under this particular set of circumstances, mice given LVS-specific T cells survive at least 1000× LD50 of challenge, but mice given naïve or Listeria-specific T cells do not. However, using either intact or irradiated mice, efforts to transfer T cells intravenously have not been successful against any dose of lethal challenge by any route. These observations imply that transfer does not really reconstitute adaptive immunity systemically, as appears to be the case in the Listeria or Mycobacteria infection models, but instead relies on very local interactions within the peritoneal cavity per se. This curious, and as yet unexplained, technical limitation must be remembered, and results obtained using the IP transfer-IP challenge approach should be interpreted cautiously and conservatively.
Critical Parameters and Troubleshooting
Although the infection strategies described herein are technically straightforward, a number of factors contribute to overall reproducibility and success. Unlike some bacteria, such as Listeria, virulence and infection by LVS, F. novicida, or virulent F. tularensis are not strictly dependent on actively growing cultures of bacteria, and thus can be started from frozen vials. This allows for a high degree of reproducibility between experiments, since several hundred vials of working stock can be prepared, and can be used over a period of months or years without any obvious deterioration. Nevertheless, vigilance in only using well-characterized bacterial infection stocks and appropriate quality control are critical to ensure reproducible results. This is particularly true in light of the well-known phenomenon of phase variation of all F. tularensis (not F. novicida) strains. Considerations for preparation of LVS stocks are provided in detail in UNIT 14.25, and will not be repeated here. In general, it is now apparent that growth conditions, including growth in different media, can affect the virulence of LVS and probably all F. tularensis. In the absence of data on human infection that inform the “right” growth conditions to mimic human disease, the experimentalist must rely only on choosing a consistent and well-documented approach. Normal flora can mask the presence of Francisella in the skin and lungs, especially when it is present in low numbers. For LVS and other holarctica strains, adding 50 μg/ml of erythromycin to the agar medium can be helpful. However, subspecies tularensis is susceptible to erythromycin.
Intragastric inoculation (oral gavage) is used when a specific volume of an agent needs to be administered solely to the GI tract, and is probably the least familiar of the administration techniques that can be used for Francisella infections. Although oral gavaging is a relatively simple and quick procedure, it should only be performed by trained personnel. The most common technical problems related to the procedure are perforation of esophagus or stomach during gavaging or accidental delivery of fluid into the lungs. A number of technical precautions have been recommended in the protocol to minimize such risks; these include wiping the outside of the gavage needle with an alcohol swab after each syringe filling, and slight aspiration of the syringe plunger before the withdrawal of the gavage needle from the animal. The mice should be closely monitored for 1 to 2 min immediately after the gavage and again within 12 to 24 hr after the procedure for their general appearance/activity level. Animals that display labored breathing or other signs of respiratory distress such as pale mucous membranes and listlessness should be euthanized, as noted in the protocol. Monitoring the relative bacterial burdens in the lungs and gastrointestinal tract (such as Peyer’s patches, mesenteric lymph nodes, and intestinal mucosa) at day 1 after inoculation should reveal any potential complications of respiratory-initiated infection (i.e., higher burdens in the lungs than the GI tract).
Alternative approaches, such as delivering bacteria via a water bottle, are inappropriate for intragastric Francisella inoculation due to associated complications of potential multiple routes of infection (such as via conjunctiva, and aerosol), and the biohazard risk.
Anticipated Results
As noted within the body of the protocols, sublethal infections with LVS achieve peak bacterial burdens within 4 to 7 days, and are cleared within 2 to 4 weeks depending on the mouse strain, dose, and route of inoculation. Lower initial doses result in longer times to peak bacterial burdens and clearance, while doses approaching the LD50 may peak within 3 to 4 days, and be clear by 10 to 14 days. Lethal infections with LVS or clinical strains result in death within 4 to 8 days, again depending on the dose and route of inoculation. BALB/c mice display more obvious visible symptoms of infection than C57BL/6 mice during the early stages of sublethal or lethal infection. Mice that resolve any sublethal infection produce readily detectable serum cytokines (e.g, IFN-γ and TNF-α); serum antibodies to bacterial LPS and proteins of both IgM and IgG subclasses; harbor memory CD4+, CD8+, and “double negative” T cells in spleens, livers, and lungs; and are generally resistant to large lethal challenge doses of LVS, and to a lesser degree fully virulent F. tularensis.
Time Considerations
The rate-limiting steps in establishing Francisella infection models are likely to be obtaining the necessary permissions for use of laboratory animals and virulent bacteria (if applicable), and then preparing and testing bacterial stocks. Growth of stocks requires 1 to 2 weeks, and in vivo testing for virulence up to a month (e.g., performing LD50 determinations in two mouse strains by both a sub-lethal route, such as i.d., and a lethal route, such as i.p. and/or i.n.). The actual inoculations and plating of bacteria to verify actual inocula will occupy approximately half a day; advanced preparation and testing of MH plates for cultivation is strongly recommended (occasional batches of plates may fail for unknown reasons). Plates are incubated for 2 to 3 days prior to counting visible LVS colonies; a 3-day incubation is generally preferable to allow readily visible and accurate counting. Satellite colonies are not generally observed with LVS, although any very small colonies that are not representative of the population as a whole are usually not included in the count.
Literature Cited
- Anthony LSD, Skamene E, Knogshavn PAL. Influence of genetic background on host resistance to experimental murine tularemia. Infect Immun. 1988;56:2089–2093. doi: 10.1128/iai.56.8.2089-2093.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker CN, Hollis DG, Thornsberry C. Anti-microbial susceptibility testing of Francisella tularensis with a modified Mueller-Hinton broth. J Clin Micro. 1985;22:212–215. doi: 10.1128/jcm.22.2.212-215.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collazo CM, Meierovics AI, De Pascalis R, Wu TH, Lyons CR, Elkins KL. T cells from lungs and livers of Francisella tularensis-immune mice control the growth of intracellular bacteria. Infect Immun. 2009;77:2010–2021. doi: 10.1128/IAI.01322-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cong Y, Yu JJ, Guentzel MN, Berton MT, Seshu J, Klose KE, Arulanandam BP. Vaccination with a defined Francisella tularensis subsp novicida pathogenicity island mutant (DeltaiglB) induces protective immunity against homotypic and heterotypic challenge. Vaccine. 2009;27:5554–5561. doi: 10.1016/j.vaccine.2009.07.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennis DT, Inglesby TV, Henderson DA, Bartlett JG, Ascher MS, Eitzen E, Fine AD, Friedlander AM, Hauer J, Layton M, Lillibridge SR, McDade JE, Osterholm MT, O’Toole T, Parker G, Perl TM, Russell PK, Tonat K. Tularemia as a biological weapon: Medical and public health management. JAMA. 2001;285:2763–2773. doi: 10.1001/jama.285.21.2763. [DOI] [PubMed] [Google Scholar]
- Elkins KL, Cowley SC, Bosio CM. Innate and adaptive immune responses to an intracellular bacterium, Francisella tularensis live vaccine strain. Microbes Infect. 2003;5:132–142. doi: 10.1016/s1286-4579(02)00084-9. [DOI] [PubMed] [Google Scholar]
- Elkins KL, Cowley SC, Bosio CM. Innate and adaptive immunity to Francisella. Ann NY Acad Sci. 2007;1105:284–324. doi: 10.1196/annals.1409.014. [DOI] [PubMed] [Google Scholar]
- Elkins KL, Colombini SM, Meierovics AI, Chu MC, Chou AY, Cowley SC. Survival of secondary lethal systemic Francisella LVS challenge depends largely on interferon gamma. Microbes Infect. 2010;12:28–36. doi: 10.1016/j.micinf.2009.09.012. [DOI] [PubMed] [Google Scholar]
- Hornick RB, Dawkins AT, Eigelsbach HT, Tulis JJ. Oral tularemia vaccine in man. Antimicrob Agents Chemother. 1966;6:11–14. doi: 10.1128/AAC.6.1.11. [DOI] [PubMed] [Google Scholar]
- Klimpel GR, Eaves-Pyles T, Moen ST, Taormina J, Peterson JW, Chopra AK, Niesel DW, Carness P, Haithcoat JL, Kirtley M, Nasr AB. Levofloxacin rescues mice from lethal intra-nasal infections with virulent Francisella tularensis and induces immunity and production of protective antibody. Vaccine. 2008;26:6874–6882. doi: 10.1016/j.vaccine.2008.09.077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- KuoLee R, Zhao X, Austin J, Harris G, Conlan JW, Chen W. Mouse model of oral infection with virulent Type A Francisella tularensis. Infect Immun. 2007a;75:1651–1660. doi: 10.1128/IAI.01834-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- KuoLee R, Harris G, Conlan JW, Chen W. Oral immunization of mice with the live vaccine strain (LVS) of Francisella tularensis protects mice against respiratory challenge with virulent type A F. tularensis. Vaccine. 2007b;25:3781–3791. doi: 10.1016/j.vaccine.2007.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Owen CR, Buker EO, Jellison WL, Lackman DB, Bell JF. Comparative studies of Francisella tularensis and Francisella novicida. J Bacteriol. 1964;87:676–683. doi: 10.1128/jb.87.3.676-683.1964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ray HJ, Cong Y, Murthy AK, Selby DM, Klose KE, Barker JR, Guentzel MN, Arulanandam BP. Oral live vaccine strain-induced protective immunity against pulmonary Francisella tularensis challenge is mediated by CD4+ T cells and antibodies, including immunoglobulin A. Clin Vaccine Immunol. 2009;16:444–452. doi: 10.1128/CVI.00405-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhinehart-Jones TR, Fortier AH, Elkins KL. Transfer of immunity against lethal murine Francisella infection by specific antibody depends on host gamma interferon and T cells. Infect Immun. 1994;62:3129–3137. doi: 10.1128/iai.62.8.3129-3137.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shen H, Chen W, Conlan JW. Susceptibility of various mouse strains to systemically-or aerosol-initiated tularemia by virulent type A Francisella tularensis before and after immunization with the attenuated live vaccine strain of the pathogen. Vaccine. 2004;22:2116–2121. doi: 10.1016/j.vaccine.2003.12.003. [DOI] [PubMed] [Google Scholar]
- Sjostedt A. Tularemia: History, epidemiology, pathogen physiology, and clinical manifestations. Ann NY Acad Sci. 2007;1105:1–29. doi: 10.1196/annals.1409.009. [DOI] [PubMed] [Google Scholar]
- Wu TH, Hutt JA, Garrison KA, Berliba LS, Zhou Y, Lyons CR. Intranasal vaccination induces protective immunity against intranasal infection with virulent Francisella tularensis biovar A. Infect Immun. 2005;73:2644–2654. doi: 10.1128/IAI.73.5.2644-2654.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
Key References
- Bosio CM, Elkins KL. Susceptibility to secondary Francisella tularensis LVS infection in B cell deficient mice is associated with neutrophilia but not with defects in specific T cell mediated immunity. Infect Immun. 2001;69:194–203. doi: 10.1128/IAI.69.1.194-203.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cowley SC, Elkins KL. Multiple T cell subsets control Francisella tularensis LVS intracellular growth without stimulation through macrophage interferon gamma receptors. J Exp Med. 2003;198:379–389. doi: 10.1084/jem.20030687. These two publications provide detailed accounts, and experimental examples, of an in vitro method for determining the contributions of various lymphocyte subsets to acquired immunity (see also UNIT 14.25) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conlan JW, Chen W, Shen H, Webb A, KuoLee R. Experimental tularemia in mice challenged by aerosol or intradermally with virulent strains of Francisella tularensis: Bacteriologic and histopathologic studies. Microbial Pathogenesis. 2003;34:239–248. doi: 10.1016/s0882-4010(03)00046-9. Provides detailed descriptions of the course of infection of mice with virulent F. tularensis subspecies holarctica and tularensis. [DOI] [PubMed] [Google Scholar]
- Elkins, et al. 2003 See above. A comprehensive review of the use of LVS infection of mice to examine innate and adaptive immunity. [Google Scholar]
- KuoLee, et al. 2007a,b See above. These references provide detailed descriptions of an experimental mouse model of oral infection with virulent F. tularensis. [Google Scholar]
- Lyons CR, Wu TH. Animal models of Francisella tularensis infection. Ann NY Acad Sci. 2007;1105:238–265. doi: 10.1196/annals.1409.003. A comprehensive review of the uses and limitations of mouse models of infection with virulent F. tularensis strains. [DOI] [PubMed] [Google Scholar]