Abstract
Mounting evidence indicates that vitamin B6 is a protective factor for colon cancer. Elevations in colonic damage, cell proliferation and heat shock proteins (HSPs, molecular chaperones) have been suggested to be associated with colon carcinogenesis. This study was performed to examine the effect of dietary levels of vitamin B6 (1, 7 or 35 mg pyridoxine HCl/kg diet) for 22 weeks on colon damage, epithelial cell proliferation and expression of HSPs in rats exposed to 1,2-dimethylhydrazine (DMH). Supplemental vitamin B6 with a low vitamin B6 diet (1 mg pyridoxine HCl/kg diet) significantly reduced fecal activity of intestinal alkaline phosphatase (an index of intestinal damage) and the colonic epithelium PCNA labeling index (a marker of cell proliferation). Analysis using ELISA indicated that supplemental vitamin B6 significantly lowered protein levels of colonic HSP70 and heme oxygenase-1, HSP32 (HO-1). However, real-time RT-PCR analysis revealed that the mRNA levels of these HSPs were not decreased by supplemental vitamin B6, suggesting that the lowering effect of vitamin B6 on the colon protein expression of the HSPs is mediated by mechanisms not involving altered gene expression. This study provided evidence that dietary supplemental vitamin B6 suppresses colon damage, epithelial cell proliferation and protein expression of HSP70 and HO-1, the targets for anti-tumor agents, in rats exposed to DMH.
Keywords: vitamin B6, colon damage, HSP70, HO-1, cell proliferation
Introduction
In previous studies, we provided the first evidence for the anti-colon tumor effect of dietary vitamin B6 in azoxymethane (AOM)-treated mice (1,2). In accordance with this finding, accumulating epidemiological evidence indicates an inverse association between vitamin B6 status and colon cancer (3–5). It has been suggested that the anti-tumor effect of vitamin B6 is mediated by lowering cell proliferation, inflammation, angiogenesis, oxidative stress and DNA damage (6–10). However, the underlying mechanism has yet to be clarified.
Colon damage and loss of epithelial cells was considered to be a risk factor for colon carcinogenesis (11,12). Epidemiological studies indicated that the association between vitamin B6 status and colon cancer is particularly significant in males consuming alcohol (3). Consumption of alcohol has been reported to cause colonic epithelium damage, which has been considered to promote colon carcinogenesis (13). Evidence suggests that vitamin B6 has a protective role against cytotoxicity in cell culture studies (14,15), although the mechanism remains unclear. Thus, the protective effect of vitamin B6 on colonic damage caused by a carcinogen should be determined.
In general, tissue damage caused by stress exposure (heat shock, oxidative stress and hypoxia) is associated with a higher expression of heat shock proteins (HSPs, molecular chaperones) (16–18). HSPs are overexpressed in a variety of human cancers, and are involved in tumor cell proliferation, differentiation, invasion, metastasis, death and recognition by the immune system (16–18). Conversely, HSPs are well known for their cytoprotective factor in response to cell injury. Accordingly, it is of interest to examine whether dietary vitamin B6 modulates the expression of colonic HSPs. The present study was performed to examine the effect of dietary vitamin B6 on colonic damage and expression of HSPs in 1,2-dimethylhydrazine (DMH)-treated rats.
Materials and methods
Animals
Male Sprague Dawley rats (4 weeks of age) were purchased from the Hiroshima Laboratory Animal Center (Hiroshima, Japan) and maintained according to the Guide for the Care and Use of Laboratory Animals established by Hiroshima University. The study was approved by the ethics committee of the same university. The animals were individually housed in an air-conditioned room at 23–24°C with a 12 h light cycle (light, 8:00–20:00). The animals received two intraperitoneal injections of DMH (20 mg/kg) and were fed a stock diet (MF, Oriental Yeast Co., Ltd., Tokyo) for 2 weeks. The rats were then divided into three groups of 12–13 rats per group and provided free access to experimental diets and tap water. The composition of the basal diet (% w/w) was corn oil, 20; casein, 24; L-cystine, 0.2; cellulose, 5; sucrose, 20; corn starch, 26.3; vitamin mixture (vitamin B6-free), 1 (19); and salt mixture, 3.5 (19). Pyridoxine (PN) HCl was supplemented to the basal diet at a dose of 1, 7 or 35 mg/kg. The level of PN HCl recommended in the AIN-93 diets was 7 mg/kg. A 1-mg/kg dose was reported to be the minimum level required for preventing growth depression caused by vitamin B6 deficiency (19). Feces were collected for the final 3 days. After 22 weeks of administering the experimental diets, the animals were sacrificed by decapitation with an anesthetic of diethyl ether. The colon was removed and stored at −70°C until analysis.
Materials
The activity of intestinal-derived alkaline phosphatase in feces was determined according to the method described elsewhere (20). p-Nitrophenyl phosphate was used as the substrate, and the absorbance of the reaction product p-nitrophenol was determined spectrophotometrically at 405 nm. Intestinal alkaline phosphatase activity was inhibited using 60 mM L-phenylalanine, which acts as a specific non-competitive inhibitor of the intestinal isozyme. The difference between total activity (non-inhibited) and the activity following inhibition with L-phenylalanine is the activity of the intestinal isoenzyme. One unit of the activity was defined as μmol p-nitrophenol/min, and the fecal activity was expressed as units/3 days of feces collected. The colonic epithelium PCNA labeling index was determined according to the method described elsewhere (21).
Protein and mRNA analyses
Colon protein levels of HSP70 and heme oxygenase-1 (HO-1) were determined by ELISA kits (Stressgen, MI, USA). Protein concentration was determined by the Bradford method with a standard of bovine serum albumin (22). HSP70, HO-1 and β-actin gene primers were purchased from Qiagen (QT00187397, QT00175994 and QT00193473, respectively; Helden, Germany). A single melt curve was observed for each primer set in all real-time RT-PCR reactions. Real-time RT-PCR was conducted using an iQ5 real-time PCR detection system (Bio-Rad Laboratories, CA, USA). Gene expressions were quantitated using Bio-Rad iQ5 optical system software (Bio-Rad Laboratories).
Statistical analysis
Statistical analysis was conducted by one-way analysis of variation (ANOVA) and Scheffe’s multiple range test (Excel Statistics 2006 for Windows, Social Survey Research Information Co., Ltd., Tokyo, Japan). P<0.05 was considered to be statistically significant.
Results
Growth was unaffected by dietary treatment (data not shown). Food intake (for 3 days) at 8, 15 and 22 weeks was also not affected by the dietary level of vitamin B6. Two rats in the 1 mg vitamin B6/kg group had an adenoma in the colon, and were not used for the further analysis of colon parameters. Fecal activity of intestinal alkaline phosphatase was significantly lower in the 7 and 35 mg PN HCl/kg diet groups (−58 and −64%, respectively) as compared to the 1 mg PN HCl/kg group (P<0.05, Fig. 1A). The activity of intestinal microbial-derived alkaline phosphatase was unaffected by dietary vitamin B6 (data not shown). The PCNA labeling index of the colonic epithelium was also significantly lower in the 7 and 35 mg PN HCl/kg diet groups (−38 and −42%, respectively) as compared to the 1 mg PN HCl/kg group (P<0.05, Fig. 1B).
Figure 1.
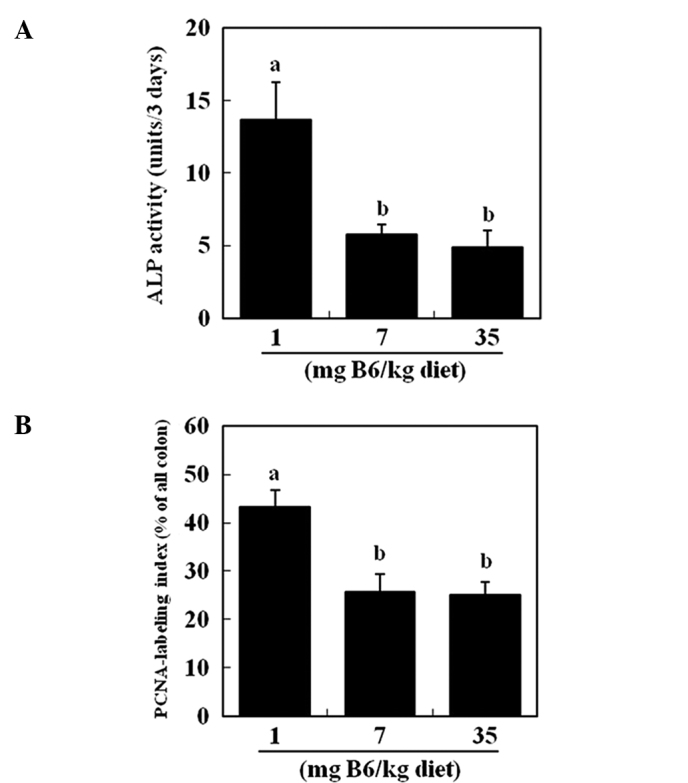
Effect of dietary level of vitamin B6 on the activity of intestinal alkaline phosphatase (ALP) in (A) feces and the (B) labeling index of PCNA in the colonic epithelium of rats receiving DMH. The results are presented as the means ± SE (n=6). a,bSignificantly different by Scheffe’s multiple range test (P<0.05).
Dietary supplemental vitamin B6 appeared to decrease colonic HSP70 protein in a dose-dependent manner (Fig. 2A). Compared to the 1 mg PN HCl/kg diet, the colonic level of HSP70 protein was significantly reduced in the 35 mg PN HCl/kg diet group (−49%) (P<0.05, Fig. 2A). Colonic levels of HO-1 protein were significantly lower in the 7 and 35 mg PN HCl/kg diet groups (−32 and −37%, respectively) compared to the 1 mg PN HCl/kg diet group (P<0.05, Fig. 2B). Colonic mRNA levels of HSP70 were unaffected by dietary levels of vitamin B6 (Fig. 3A). Colonic levels of HO-1 mRNA were significantly elevated in the 7 and 35 mg PN HCl/kg diet groups (+48 and +62%, respectively) compared to the 1 mg PN HCl/kg diet group (P<0.05, Fig. 3B).
Figure 2.
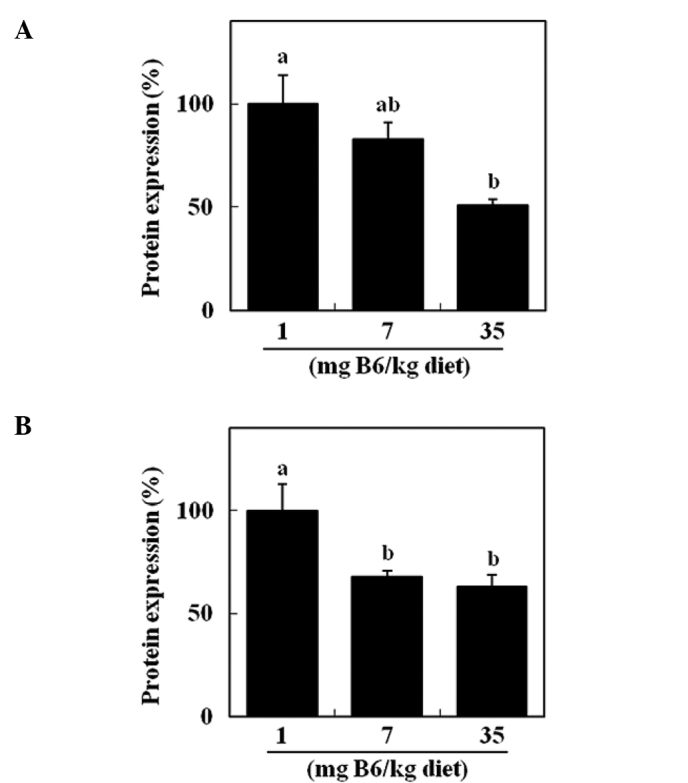
Effect of dietary level of vitamin B6 on colonic protein levels of HSP70 and HO-1 in rats receiving DMH. The protein expression of (A) HSP70 and (B) HO-1 were analyzed by ELISA. The results are presented as the means ± SE (n=6–7). a,bSignificantly different by Scheffe’s multiple range test (P<0.05).
Figure 3.
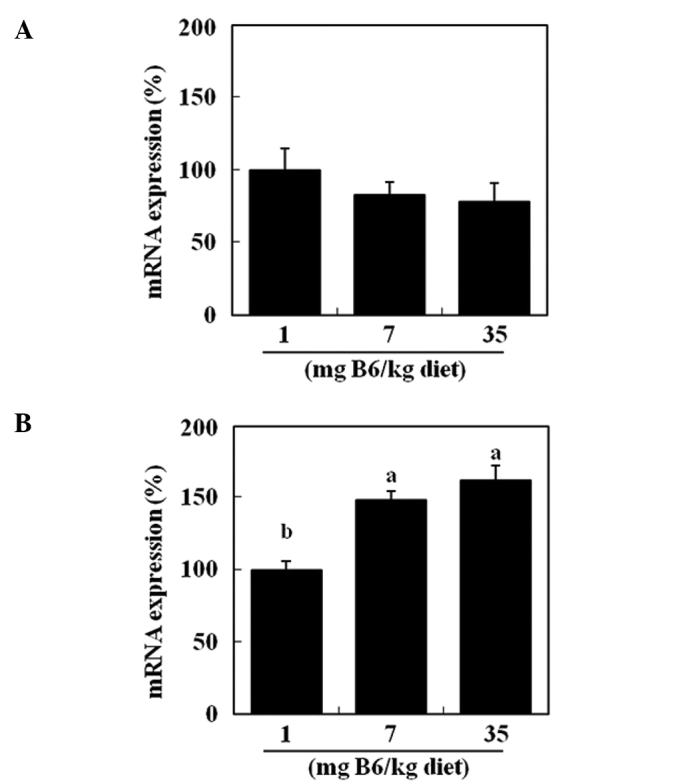
Effect of dietary level of vitamin B6 on colonic mRNA levels of HSP70 and HO-1 in rats receiving DMH. The mRNA expression of (A) HSP70 and (B) HO-1 were normalized to the amount of β-actin. The results are presented as the means ± SE (n=6). a,bSignificantly different by Scheffe’s multiple range test (P<0.05).
Discussion
This study has shown that dietary supplemental vitamin B6 suppressed DMH-induced colon damage as evidenced by the data pertaining to fecal alkaline phosphatase activity (Fig. 1). Our previous study indicated that dietary vitamin B6 lowered colonic levels of oxidative stress markers, including 8-hydroxyguanosine and 4-hydroxynonenal, and inflammatory mediators, such as COX-2 and iNOS in AOM-treated mice (10). Therefore, the protective effect of vitamin B6 against colon damage appears to be, at least in part, explained by the lower oxidative stress and inflammation. Further study is in progress to fully elucidate the molecular basis of the underlying mechanisms of the protective role of vitamin B6.
The cytotoxicity of colonic components, including secondary bile acids and oxygen radicals, may cause epithelial cell loss in the large bowel, leading to a compensatory crypt cell proliferation and the development of colon cancer (13,14). In the DMH-treated rats, supplemental vitamin B6 caused a significant reduction in the PCNA labeling index, an index of cell proliferation as well as fecal intestinal phosphatase activity (Fig. 1). This finding suggests that the reduced intestinal damage by supplemental vitamin B6 decreases cell proliferation in the colonic epithelium. Previously, we reported that dietary supplemental vitamin B6 caused reduced colonic epithelial cell proliferation despite no alteration in apoptosis and the total cell number in the epithelium of AOM-treated mice (1). The reduced colonic cell proliferation by dietary vitamin B6 may be counteracted by the reduced loss of the epithelial cells.
Notably, this study has demonstrated that dietary supplemental vitamin B6 reduced the levels of colonic HSP70 and HO-1 proteins in DMH-treated rats (Fig. 2). Since tissue damage by stress exposure induces a higher expression of HSPs, reduced colon damage may result in a lower protein expression of HSP70 and HO-1. HSPs are considered to be novel targets for anti-tumor agents (16–18). HSP70 promotes cancer cell growth and prevents apoptosis, thereby increasing the survival of cells exposed to a wide range of otherwise lethal stimuli. HSP70 neutralization has been found to exert potent anti-tumor effects in animal models of colon cancer (23). It has been suggested that HO-1 protects tumor cells against oxidative stress and is regarded as an enzyme facilitating tumor progression (18,19). It has been demonstrated that pegylated zinc protoporphyrin, a potent HO inhibitor, administered in vitro induced apoptosis of human colon carcinoma SW480 cells and inhibited the growth of murine colon carcinoma in vivo (24). Thus, the results of the present study suggest that the anti-colon tumor effect of vitamin B6 is, at least in part, mediated by reducing the protein expression of HSP70 and HO-1. To the best of our knowledge, this is the first study to demonstrate the possible involvement of HSPs in the mechanism of anti-tumorigenesis by dietary nutrients. The expression of proinflammatory cytokines including TNF-α, IL-1α and IL-6 was up-regulated, and NF-κB was activated in monocytes by HSP70 (25). Our previous study indicated that dietary vitamin B6 decreased the colonic expression of COX-2 and iNOS in AOM-treated mice (10). Thus, it is of interest to test whether a reduced HSP70 protein expression by dietary vitamin B6 results in lower inflammatory mediators.
In the present study, colonic HSP70 and HO-1 mRNA levels were not reduced by dietary vitamin B6 (Fig. 3). Thus, the lower protein expression of HSP70 and HO-1 by dietary B6 appears not to be mediated by lowering the mRNA expression. These results are expected since a previous study has shown that HSP70 protein expression is regulated by the degradation of HSP70 proteins as well as transcriptional regulation (26). Further studies are required to examine the underlying mechanisms of a reduced protein expression of the HSPs by vitamin B6. In our preliminary study, no effect of dietary vitamin B6 was observed on the colonic protein expression of HSP90, HSP60 and HSP25 (Kayashima et al; unpublished data). At present, it is not known why the protein expression of HSP70 and HO-1 was specifically affected by dietary vitamin B6.
HSP70 has been suggested to be a cytoprotective factor by modulating protein unfolding and protein degradation (16). HO-1 has also been suggested to prevent cell damage and exhibit marked antioxidant activity (17). Thus, prior to this study, we considered the possibility that dietary vitamin B6 causes a higher expression of HSPs, leading to the protective function of vitamin B6 against colon damage by DMH. However, this possibility appears to be negated.
In conclusion, the present study provided the first evidence that dietary vitamin B6 lowers colonic damage and protein expression of HSP70 and HO-1 in rats exposed to DMH. These findings suggest novel mechanisms of an anti-colon tumor effect of dietary vitamin B6.
Acknowledgements
This study was supported in part by a Grant-in-Aid for Scientific Research from the Ministry of Education, Culture, Sports, Science and Technology of Japan.
Abbreviations
- PN
pyridoxine
- HSP
heat shock protein
- HO-1
heme oxygenase-1
- DMH
1,2-dimethylhydrazine
- AOM
azoxymethane
References
- 1.Komatsu SI, Watanabe H, Oka T, Tsuge H, Nii H, Kato N. Vitamin B-6-supplemented diets compared with a low vitamin B-6 diet suppress azoxymethane-induced colon tumorigenesis in mice by reducing cell proliferation. J Nutr. 2001;131:2204–2207. doi: 10.1093/jn/131.8.2204. [DOI] [PubMed] [Google Scholar]
- 2.Komatsu S, Isobe M, Yanaka N, Kato N. A high-fat diet enhances the inhibitory effect of dietary vitamin B6 on colon cell proliferation in mice. Oncol Rep. 2005;14:265–269. [PubMed] [Google Scholar]
- 3.Ishihara J, Otani T, Inoue M, Iwasaki M, Sasazuki S, Tsugane S. Low intake of vitamin B-6 is associated with increased risk of colorectal cancer in Japanese men. J Nutr. 2007;137:1808–1814. doi: 10.1093/jn/137.7.1808. [DOI] [PubMed] [Google Scholar]
- 4.Theodoratou E, Farrington SM, Tenesa A, et al. Dietary vitamin B6 intake and the risk of colorectal cancer. Cancer Epidemiol Biomarkers Prev. 2008;17:171–182. doi: 10.1158/1055-9965.EPI-07-0621. [DOI] [PubMed] [Google Scholar]
- 5.Larsson SC, Orsini N, Wolk A. Vitamin B6 and risk of colorectal cancer: a meta-analysis of prospective studies. JAMA. 2010;303:1077–1082. doi: 10.1001/jama.2010.263. [DOI] [PubMed] [Google Scholar]
- 6.Matsubara K, Mori M, Matsuura Y, Kato N. Pyridoxal 5′-phosphate and pyridoxal inhibit angiogenesis in serum-free rat aortic ring assay. Int J Mol Med. 2001;8:505–508. doi: 10.3892/ijmm.8.5.505. [DOI] [PubMed] [Google Scholar]
- 7.Komatsu S, Watanabe H, Oka T, Tsuge H, Kato N. Dietary vitamin B6 suppresses colon tumorigenesis, 8-hydroxyguanosine, 4-hydroxynonenal, and inducible nitric oxide synthase protein in azoxymethane-treated mice. J Nutr Sci Vitaminol. 2002;48:65–68. doi: 10.3177/jnsv.48.65. [DOI] [PubMed] [Google Scholar]
- 8.Komatsu S, Yanaka N, Matsubara K, Kato N. Antitumor effect of vitamin B6 and its mechanisms. Biochim Biophys Acta. 2003;1647:127–130. doi: 10.1016/s1570-9639(03)00076-1. [DOI] [PubMed] [Google Scholar]
- 9.Yanaka N, Koyama TA, Komatsu S, Nakamura E, Kanda M, Kato N. Vitamin B6 suppresses NF-κB activation in LPS-stimulated mouse macrophages. Int J Mol Med. 2005;16:1071–1075. [PubMed] [Google Scholar]
- 10.Kanellis P, Gagliardi M, Banath JP, et al. A screen for suppressors of gross chromosomal rearrangements identifies a conserved role for PLP in preventing DNA lesions. PLoS Genet. 2007;3:1438–1453. doi: 10.1371/journal.pgen.0030134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lapre JA, van der Meer R. Diet-induced increase of colonic bile acids stimulates lytic activity of fecal water and proliferation of colonic cells. Carcinogenesis. 1992;13:41–44. doi: 10.1093/carcin/13.1.41. [DOI] [PubMed] [Google Scholar]
- 12.Lapre JA, De Vries HT, van der Meer R. Cytotoxicity of fecal water is dependent on the type of dietary fat and is reduced by supplemental calcium phosphate in rats. J Nutr. 1993;123:578–585. doi: 10.1093/jn/123.3.587. [DOI] [PubMed] [Google Scholar]
- 13.Wallace JL, Whittle BJ, Boughton-Smith NK. Prostaglandin protection of rat colonic mucosa from damage induced by ethanol. Dig Dis Sci. 1985;30:866–876. doi: 10.1007/BF01309518. [DOI] [PubMed] [Google Scholar]
- 14.Geng M-Y, Saito H, Katsuki H. Effects of vitamin B6 and its related compounds on survival of cultured brain neurons. Neurosci Res. 1995;24:61–65. doi: 10.1016/0168-0102(96)81279-x. [DOI] [PubMed] [Google Scholar]
- 15.Geng M-Y, Saito H, Nishiyama N. Protective effects of pyridoxal phosphate against glucose deprivation-induced damage in cultured hippocampal neurons. J Neurochem. 1997;68:2500–2506. doi: 10.1046/j.1471-4159.1997.68062500.x. [DOI] [PubMed] [Google Scholar]
- 16.Calderwood SK, Khaleque MA, Sawyer DB, Ciocca DR. Heat shock proteins in cancer: chaperones of tumorigenesis. Trends in Biochem Sci. 2006;31:164–172. doi: 10.1016/j.tibs.2006.01.006. [DOI] [PubMed] [Google Scholar]
- 17.Was H, Dulak J, Jozkowicz A. Heme oxygenase-1 in tumor biology and therapy. Current Drug Targets. 2010;11:1551–1570. doi: 10.2174/1389450111009011551. [DOI] [PubMed] [Google Scholar]
- 18.Zhu X, Fan WG, Li DP, Lin MCM, Kung H. Heme oxygenase-1 system and gastrointestinal tumors. World J Gastroenterol. 2010;16:2633–2637. doi: 10.3748/wjg.v16.i21.2633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Reeves PG, Nielsen FH, Fahey GC., Jr AIN-93 purified diets for laboratory rodents: final report of the American Institute of Nutrition ad hoc writing committee on the reformulation of the AIN-76A rodent diet. J Nutr. 1993;123:1939–1951. doi: 10.1093/jn/123.11.1939. [DOI] [PubMed] [Google Scholar]
- 20.Davis CD. Low dietary copper increases fecal free radical production, fecal water alkaline phosphatase activity and cytotoxicity in healthy men. J Nutr. 2003;133:522–527. doi: 10.1093/jn/133.2.522. [DOI] [PubMed] [Google Scholar]
- 21.Teixeira CR, Tanaka S, Haruma K, Yoshihara M, Sumii K, Kajiyama G. Proliferating cell nuclear antigen expression at the invasive tumor margin predicts malignant potential of colorectal carcinomas. Cancer. 1994;73:575–579. doi: 10.1002/1097-0142(19940201)73:3<575::aid-cncr2820730313>3.0.co;2-0. [DOI] [PubMed] [Google Scholar]
- 22.Bradford MM. A rapid and sensitive method for the quantitation of microgram quantities of protein utilizing the principle of protein-dye binding. Anal Biochem. 1976;72:248–254. doi: 10.1016/0003-2697(76)90527-3. [DOI] [PubMed] [Google Scholar]
- 23.Schmitt E, Maingret L, Puig PE, et al. Heat shock protein 70 neutralization exerts potent antitumor effects in animal models of colon cancer and melanoma. Cancer Res. 2006;66:4191–4197. doi: 10.1158/0008-5472.CAN-05-3778. [DOI] [PubMed] [Google Scholar]
- 24.Hirai K, Sasahira T, Ohmori H, Fujii K, Kuniyasu H. Inhibition of heme oxygenase-1 by zinc protoporphyrin IX reduces tumor growth of LL/2 lung cancer in C57BL mice. Int J Cancer. 2007;120:500–505. doi: 10.1002/ijc.22287. [DOI] [PubMed] [Google Scholar]
- 25.Asea A, Kraeft SK, Kurt-Jones EA, et al. HSP70 stimulates cytokine production through a CD14-dependant pathway, demonstrating its dual role as a chaperone and cytokine. Nat Med. 2000;6:435–442. doi: 10.1038/74697. [DOI] [PubMed] [Google Scholar]
- 26.Qian S, McDonough H, Boellmann F, Cyr DM, Patterson C. CHIP-mediated stress recovery by sequential ubiquitination of substrates and Hsp70. Nature. 2006;440:551–555. doi: 10.1038/nature04600. [DOI] [PMC free article] [PubMed] [Google Scholar]


