Abstract
Objective
To study the association between metabolic syndrome (MetS) and self-perceived depression.
Design
A cross-sectional community-based study.
Setting
Semi-rural community of Lapinlahti in eastern Finland in 2005.
Subjects
A total of 416 subjects in eight adult birth cohorts (55%) with complete Beck Depression Inventory (BDI-21) questionnaire data.
Main outcome measures
The values of the 21 BDI items and the BDI-21 total score with a cut-off point of 14/15 were used to study the association between MetS and depression. National Cholesterol Education Programme (NCEP) 2005 criteria were used for MetS classification.
Results
The total BDI-21 score was significantly higher in the subjects with MetS than in the subjects without MetS (p=0.020). Men with MetS were significantly worse off than men without MetS in the BDI-21 items of irritability (p=0.008), work inhibition (p=0.008), fatigability (p=0.037), weight loss (p=0.045), and loss of libido (p=0.014), while women were only so on the item of loss of libido (p=0.007). In a logistic regression analysis using a BDI-21 cut-off point of 14/15 adjusted for age, marital status, vocational education, and working status, significant association was retained between perceived depression and elevated blood glucose among men (OR=1.697) and large waist circumference among women (OR=1.066).
Conclusion
Elevated plasma glucose in men and central obesity in women are associated with self-perceived depression. This co-occurrence deserves attention in clinical practice.
Keywords: Adult population, depression, family practice, fasting plasma glucose, metabolic syndrome, waist circumference
There is growing evidence of the association between metabolic syndrome (MetS) and depression, but it is doubtful whether the association is independent of other risk factors.
Subjects with MetS are significantly worse off than subjects without MetS on various items of depression measured by Beck Depression Inventory.
Self-perceived depression is associated with large waist circumference among women and elevated plasma glucose among men when adjusted for background variables.
Frequent co-occurrence of MetS and depression should be recognized in clinical practice.
Depression is a chronic and recurrent disorder that causes disability [1], morbidity [2], [3], and increased mortality [4]. Depressed subjects also seem to be at a high risk of cardiovascular disease and diabetes [2], [3]. The pathogenesis of Metabolic Syndrome (MetS) is complex and incompletely understood, but the interaction between obesity, sedentary lifestyle, and dietary as well as genetic factors is known to contribute to its development [5]. MetS is associated with a five- to ninefold increase in the risk of type 2 diabetes mellitus and an increased risk of cardiovascular diseases [6], [7].
There is growing evidence of the co-occurrence of depression and MetS, especially in the elderly population [8]. The connection of depression, mental disability, and psychological distress with insulin resistance and metabolic syndrome has been the focus of particular attention during the last few years [9–11]. Recently, it has been shown in population-based studies that psychosocial factors, anger, anxiety, and tension may predict the risk for developing the metabolic syndrome [12–15]. In a Finnish six-year clinical follow-up study, the prevalence of MetS in depressive outpatients was 36% using the NCEP 2001 criteria. The prevalence of MetS was highest in the subgroup of patients who were diagnosed as still having major depression [16].
Our purpose was to study the association between self-perceived depression, metabolic syndrome, and its components (large waist circumference, elevated plasma glucose level, elevated blood pressure, lowered serum HDL-cholesterol level, and elevated serum triglyceride level) by analysing Beck Depression Inventory (BDI-21) profiles and its total score in an adult general population.
Material and methods
Study population and procedure
The Lapinlahti 2005 study at the University of Kuopio, Finland, involved all 760 adult Lapinlahti residents in eastern Finland (10% of the total population) born in 1939, 1944, 1949, 1954, 1959, 1964, 1969, and 1974. Altogether 594 subjects responded satisfactorily to a postal questionnaire, and 480 (230 men and 250 women) underwent a complete health survey including anthropometric measurements, laboratory tests, and an extensive questionnaire. The questionnaire covered all the background variables used in this article and a BDI-21 inventory. The participation rate was higher among women than among men. It was also higher among older than younger subjects among both genders (Table I).
Table I.
Lapinlahti 2005 study: Subjects in the original study sample, respondents to the postal questionnaire survey, study subjects included in the complete health survey, and Beck Depression Inventory (BDI-21) respondents.
| Original sample (n = 760) |
Respondents to postal questionnaire (n = 594) |
Participants in health survey (n = 480) |
BDI–21 respondents(n = 442) |
BDI–21 respondents with complete questionnaires (n = 416) |
||||||||||||||
| Men |
Women |
Men |
Women |
Men |
Women |
Men |
Women |
Men |
Women |
|||||||||
| Year of birth | n | n | n | % of original sample | n | % of original sample | n | % of original sample | n | % of original sample | n | % of original sample | n | % of original sample | n | % of original sample | n | % of original sample |
| 1939 | 32 | 41 | 25 | 78.1 | 37 | 90.2 | 23 | 71.9 | 33 | 80.5 | 23 | 71.9 | 31 | 75.6 | 22 | 68.8 | 30 | 73.2 |
| 1944 | 38 | 34 | 35 | 92.1 | 27 | 79.4 | 28 | 73.7 | 23 | 67.6 | 25 | 65.8 | 22 | 64.7 | 23 | 60.5 | 21 | 61.8 |
| 1949 | 82 | 69 | 68 | 82.9 | 60 | 87.0 | 55 | 67.1 | 51 | 73.9 | 53 | 64.6 | 47 | 68.1 | 45 | 54.9 | 45 | 65.2 |
| 1954 | 64 | 57 | 43 | 67.2 | 47 | 82.5 | 32 | 50.0 | 41 | 71.9 | 30 | 46.9 | 37 | 64.9 | 29 | 45.3 | 34 | 59.6 |
| 1959 | 48 | 50 | 35 | 72.9 | 40 | 80.0 | 28 | 58.3 | 32 | 64.0 | 24 | 50.0 | 30 | 60.0 | 23 | 47.9 | 28 | 56.0 |
| 1964 | 49 | 45 | 37 | 75.5 | 34 | 75.6 | 27 | 55.1 | 28 | 62.2 | 22 | 44.9 | 23 | 51.1 | 21 | 42.9 | 22 | 48.9 |
| 1969 | 41 | 43 | 27 | 65.9 | 31 | 72.1 | 22 | 53.7 | 27 | 62.8 | 19 | 46.3 | 26 | 60.5 | 19 | 46.3 | 24 | 55.8 |
| 1974 | 39 | 28 | 25 | 64.1 | 23 | 82.1 | 15 | 38.5 | 15 | 53.6 | 15 | 38.5 | 15 | 53.6 | 15 | 38.5 | 15 | 53.6 |
| Total | 393 | 367 | 295 | 75.1 | 299 | 81.5 | 230 | 58.5 | 250 | 68.1 | 211 | 53.7 | 231 | 62.9 | 197 | 50.1 | 219 | 59.7 |
The BDI-21 questionnaire was sent to 405 subjects after the health survey, while it was included in the master health survey questionnaire of 75 subjects. Of the 480 study participants in the health survey, 442 (211 men and 231 women) filled in the BDI-21 inventory [17]. Of these, 26 subjects with incomplete data were excluded from the analysis leaving a total of 416 subjects (55% of the age cohorts) for the final analysis. The BDI-21 total score was the sum score of the 21 separate BDI items which contain four statements each, reflecting the intensity of a particular item of mood. The respondents selected the most appropriate statement of each BDI-21 item. For the statistical analysis, these statements were given numeric values (0 = no symptoms, 1 = mild symptoms, 2 = moderate symptoms, 3 = severe symptoms). The BDI-21 items are: mood, pessimism, sense of failure, lack of satisfaction, guilty feelings, sense of punishment, self-hate, self-accusation, self-punitive wishes, crying spells, irritability, social withdrawal, indecisiveness, body image, work inhibition, sleep disturbances, fatigability, loss of appetite, weight loss, somatic preoccupation, and loss of libido.
We used a BDI-21 cut-off point of 14/15 (total score range 0–63) to categorize the study subjects as perceived depressive (total score 15 or higher) or non-depressive (total score 14 or lower) [18]. For further analysis, we compared a BDI-21 total score and level values of single items (range 0–3) between the subjects with and without MetS. The Cronbach's alpha reliability coefficient of the BDI-21 in this sample was 0.887.
We used the National Cholesterol Education Programme (NCEP) 2005 criteria for MetS definition [19]. In a population study in the US, the NCEP 2005 definition gave an unadjusted MetS prevalence of 34% among men and 35% among women, and led to slightly lower estimates of prevalence in all demographic groups than did the International Diabetes Federation (IDF) 2005 criteria with the same population (40% among men and 38% among women). However, the two definitions similarly classified 93% of the participants as having or not having MetS [20]. The prevalence figures in the US are quite close to those found in a Finnish population study [21].
MetS was defined from anthropometric measurements and blood test results. The presence of at least three of the five NCEP 2005 MetS criteria classified the subject as having MetS. The criteria are as follows: (1) fasting plasma glucose level of 5.6 mmol/l or higher and/or use of diabetes medication or previously diagnosed adult type diabetes, (2) serum triglyceride level of 1.7 mmol/l or higher and/or medication, (3) serum HDL-cholesterol level lower than 1.0 mmol/l in men and lower than 1.3 mmol/l in women and/or medication, (4) systolic blood pressure of 130 mmHg or higher and/or diastolic blood pressure at 85 mmHg or higher and/or use of antihypertensive drug(s), (5) waist circumference larger than 102 cm for men and larger than 88 cm for women.
Weight was taken in light clothing and height was measured in a standing position. Body mass index (BMI) was calculated from the formula: weight/height2. Waist circumference was measured at the midpoint between the lowest rib and the iliac crest, and blood pressure was taken in a sitting position at five-minute intervals after 10 minutes of rest. For the statistical analysis, we calculated the means of the three measurements. Glucose level was tested from capillary blood with a glucometer calibrated for plasma glucose level, and other laboratory tests were conducted from the serum of a venous blood sample after 12 hours of fasting. All laboratory investigations were performed according to the routine protocol of the Kuopio University Hospital's medical laboratory.
Statistical analysis
SPSS 14.0 for Windows statistical software (SPSS Inc., Chicago, IL) was used with a p-value of less than 0.05 for statistically significant differences. Genders were analysed separately based on earlier literature reports [22] and marked differences in our preliminary analyses. We used an independent samples t-test to compare the BDI-21 total scores and all the values of the 21 BDI items between subjects with and without MetS. Furthermore, with a multiple logistic regression analysis of the BDI-21 total score with a cut-off point of 14/15, we studied the associations of perceived depression with MetS status (absent vs. present) as well as its components as continuous variables: waist circumference, fasting plasma glucose, serum HDL-cholesterol, serum triglyceride, systolic blood pressure, and diastolic blood pressure. These were adjusted for the following background variables: age (continuous variable), marital status (married or cohabiting vs. single, divorced, or widowed), vocational education (high vocational education or university degree vs. low vocational education or none), and employment status (employed vs. unemployed or retired).
Ethical approval
The Ethics Committee of Kuopio University Hospital and the University of Kuopio approved the study. All the study subjects gave written informed consent before entering the study.
Results
Basic characteristics of the sample
We included in the report the results of the respondents (n = 416) who gave complete answers to all 21 items of the BDI questionnaire. MetS prevalence was 37% (39% in men and 35% in women) among the BDI-21 respondents (n = 416), while it was 44% (42% in men and 45% in women) among the BDI-21 non-respondents and respondents with incomplete answers (n = 64). The difference was not statistically significant.
Table II summarizes the basic characteristics of the 416 study subjects. The mean age of the subjects with MetS was significantly higher than that of the subjects without MetS (54 vs. 49 years). Furthermore, the subjects with MetS had a significantly lower vocational education level than the subjects without MetS. The mean BDI-21 total score was 7.07 among the subjects with MetS and 5.49 among the subjects without MetS (mean difference −1.585 and 95% CI −2.917; − 0.253). The mean BDI-21 total score of men with MetS was 7.17 and without MetS 5.52 (mean difference −1.650 and 95% CI −3.757;0.456), while the total score of women with MetS was 6.97 and without MetS 5.46 (mean difference −1.516 and 95% CI −3.210;0.178).
Table II.
Lapinlahti 2005 study: Basic characteristics of the subjects with complete BDI-21 questionnaire data (n = 416).
| All (n = 416) | *MetS absent (n = 263) | *MetS present (n = 153) | p-value | |
| Age in years1 | 50.4 (10.5) | 48.5 (10.4) | 53.7 (9.8) | <0.001 |
| Gender male/female (%) | 47/53 | 46/54 | 50/50 | 0.47 |
| Marital status (% single, divorced or widowed)2 | 18 | 16 | 22 | 0.152 |
| Vocational education (% lower-level education)3 | 69 | 64 | 77 | 0.006 |
| Employment status (% unemployed or retired)4 | 29 | 26 | 34 | 0.114 |
| On antidepressive medication (%) | 3 | 2 | 5 | 0.195 |
| On diabetes medication (%) | 5 | 2 | 9 | 0.002 |
| On antihypertensive medication (%) | 23 | 11 | 43 | <0.001 |
| On lipid medication (%) | 14 | 9 | 22 | <0.001 |
| Waist circumference in men (cm)1 | 98.3 (12.0) | 92.2 (8.0) | 108.0 (10.9) | <0.001 |
| Waist circumference in women (cm)1 | 84.5 (13.5) | 77.4 (8.1) | 97.2 (11.6) | <0.001 |
| Systolic blood pressure (mmHg)1 | 138.9 (18.6) | 135.2 (18.1) | 145.0 (17.9) | <0.001 |
| Diastolic blood pressure (mmHg)1 | 82.7(10.4) | 80.6 (10.0) | 86.4 (10.2) | <0.001 |
| Fasting plasma glucose (mmol/l)1 | 5.57 (1.19) | 5.26 (0.96) | 6.10 (1.37) | <0.001 |
| HDL-cholesterol in men (mmol/l)1 | 1.09 (0.33) | 1.22 (0.30) | 0.89 (0.28) | <0.001 |
| HDL-cholesterol in women (mmol/l)1 | 1.40 (0.43) | 1.55 (0.40) | 1.11 (0.31) | <0.001 |
| Serum triglyceride (mmol/l)1 | 1.36 (0.80) | 1.04 (0.41) | 1.89 (0.97) | <0.001 |
| BDI-21 score1 | 6.07 (6.70) | 5.49 (6.37) | 7.07 (7.14) | <0.020 |
Notes: BDI-21: Beck Depression Inventory (21 items). *MetS: Metabolic syndrome. NCEP 2005 criteria. At least three of the five of the following criteria classified the subject as having MetS: p-glucose ≥5.6 mmol/L and/or use of diabetes medication or previous diagnosis of adult type diabetes; s-triglyceride level ≥1.7 mmol/L and/or medication; s-HDL cholesterol < 1.0 mmol/L in men and<1.3 mmol/l in women and/or medication; systolic blood pressure ≥130 mmHg and/or diastolic blood pressure ≥85 mmHg and/or use of antihypertensive drug(s); waist circumference > 102 cm for men and > 88 cm for women, 1Values given as means (SD). 2Marital status: single, divorced, or widowed vs. married or cohabiting. 3Vocational education: low-level vocational education or none vs. higher-level vocational education or university degree. 4Employment status: employed vs. unemployed or retired.
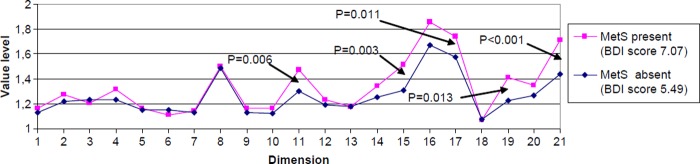
In the whole sample of 416 respondents, the subjects with MetS were significantly worse off than the subjects without MetS on the items of irritability (p = 0.006), work inhibition (p = 0.003), fatigability (p = 0.011), weight loss (p = 0.013) and loss of libido (p < 0.001) (Figure 1). Men with MetS had a significantly higher mean score than men without MetS on the BDI-21 items irritability (1.61 vs. 1.33; p = 0.008), work inhibition (1.61 vs. 1.33; p = 0.008), fatigability (1.76 vs. 1.56; p = 0.037), weight loss (1.46 vs. 1.24; p = 0.045), and loss of libido (1.62 vs. 1.36; p = 0.014), while for women this was only on the BDI-21 item of loss of libido (1.81 vs. 1.51; p = 0.007).
Figure 1. .
Lapinlahti 2005 study: BDI-21 profiles by metabolic syndrome (MetS) status (n = 416).
Legend:
1 Mood
2 Pessimism
3 Sense of failure
4 Lack of satisfaction
5 Guilty feeling
6 sense of punishment
7 Self-hate
8 Self-accusation
9 Self-punitive wishes
10 Crying spells
11 Irritability
12 social withdrawal
13 Indecisiveness
14 Body image
15 Work inhibition
16 Sleep disturbances
17 Fatigability
18 loss of appetite
19 Weight loss
20 Somatic preoccupation
21 Loss of libido
In a logistic regression analysis using a BDI-21 cut-off point of 14/15 (adjusted for age, marital status, vocational education, and working status) no significant association was found between perceived depression and MetS in either gender, but significant association was retained between perceived depression and elevated plasma glucose level (continuous variable) among men (OR = 1.697, 95% CI 1.185;2.430, p = 0.004,) and large waist circumference (continuous variable) among women (OR = 1.066, 95% CI 1.009;1.127, p = 0.024) (Tables III and IV).
Table III.
Lapinlahti 2005 study: Odds ratios of men for high BDI-21 total score (cut-off point of 14/15) in multivariate logistic regression analysis.
| Variable | Included in analysis (n) | OR (95% CI) | p-value |
| Age (years) | |||
| Continuous | 193 | 1.057(0.986;1.133) | 0.116 |
| Marital status | |||
| Married, cohabiting = 0, | 151 | 1 | |
| Single, divorced, or widowed = 1 | 42 | 2.231 (0.678;7.337) | 0.194 |
| Vocational education | |||
| High = 0, | 38 | 1 | |
| Low = 1 | 155 | 2.344 (0.267;20.533) | 0.442 |
| Employment status | |||
| Employed = 0 | 135 | 1 | |
| Unemployed/retired = 1 | 58 | 1.739 (0.5560;5.399) | 0.339 |
| MetS status | |||
| MetS absent | 118 | 1 | |
| MetS present | 75 | 2.339 (0.433;12.645) | 0.324 |
| Waist circumference (cm) | |||
| Continuous | 193 | 1.036 (0.974;1.103) | 0.258 |
| Fasting p-glucose (mmol/l) | |||
| Continuous | 193 | 1.697 (1.185;2.430) | 0.004 |
| s-HDL-cholesterol (mmol/l) | |||
| Continuous | 193 | 0.186 (0.026;1.348) | 0.096 |
| s-triglyceride (mmol/l) | |||
| Continuous | 193 | 0.338 (0.106;1.079) | 0.067 |
| Systolic blood pressure (mmHg) | |||
| Continuous | 193 | 0.979 (0.933;1028) | 0.397 |
| Diastolic blood pressure (mmHg) | |||
| Continuous | 193 | 1.069 (0.987;1.158) | 0.100 |
The following variables were entered into the model: Age: continuous variable; Marital status: single, divorced, or widowed vs. married or cohabiting; Vocational education: low vocational education or none vs. higher vocational education or university degree; Employment status: unemployed or retired vs. employed; Waist circumference: continuous variable; Fasting plasma glucose level: continuous variable; Serum HDL-cholesterol level: continuous variable; Serum triglyceride level: continuous variable; Systolic blood pressure: continuous variable; Diastolic blood pressure: continuous variable.
Table IV.
Lapinlahti 2005 study: Odds ratios of women for high BDI-21 total score (cut-off point of 14/15) in multivariate logistic regression analysis.
| Variable | Included in analysis (n) | OR (95% CI) | p-value |
| Age (years) | |||
| Continuous | 206 | 0.974 (0.911;1.041) | 0.436 |
| Marital status | |||
| Married, cohabiting = 0 | 175 | 0.806 (0.199;3.271) | 0.763 |
| Single, divorced, or widowed = 1 | 31 | 1 | 0.194 |
| Vocational education | |||
| High = 0 | 85 | 1 | |
| Low = 1 | 121 | 3.593 (0.947;13.638) | 0.060 |
| Employment status | |||
| Employed = 0 | 147 | 1 | |
| Unemployed/retired = 1 | 59 | 2.136 (0.673;6.779) | 0.198 |
| MetS status | |||
| MetS absent = 0 | 132 | 1 | |
| MetS present = 1 | 74 | 2.386 (0.452;12.586) | 0.305 |
| Waist circumference (cm) | |||
| Continuous | 206 | 1.066 (1.009;1.127) | 0.024 |
| Fasting p-glucose (mmol/l) | |||
| Continuous | 206 | 1.467 (0.759;2.835) | 0.255 |
| s-HDL-cholesterol (mmol/l) | |||
| Continuous | 206 | 1.148 (0.272;4.844) | 0.851 |
| s-triglyceride (mmol/l) | |||
| Continuous | 206 | 1.058 (0.552;2.028) | 0.864 |
| Systolic blood pressure (mmHg) | |||
| Continuous | 206 | 0.976 (0.928;1.025) | 0.331 |
| Diastolic blood pressure (mmHg) | |||
| Continuous | 206 | 1.033 (0.950;1.124) | 0.451 |
The following variables were entered into the model: Age: continuous variable; Marital status: single, divorced, or widowed vs. married or cohabiting; Vocational education: low vocational education or none vs. higher vocational education or university degree; Employment status: unemployed or retired vs. employed; Waist circumference: continuous variable; Fasting plasma glucose level: continuous variable; Serum HDLcholesterol level: continuous variable; Serum triglyceride level: continuous variable; Systolic blood pressure: continuous variable; Diastolic blood pressure: continuous variable.
Discussion
Main findings
The subjects with clinically verified MetS had a significantly higher total score and higher scores on several single items of the Beck Depression Inventory (BDI-21) than the subjects without MetS.
Further, perceived depression was significantly associated with waist circumference among women and with elevated plasma glucose level among men, even when adjusted for age, marital status, vocational education level, and working status. Therefore, the findings are in favor of a co-occurrence of perceived depression and emerging MetS.
Strengths and limitations of the study
The main strengths of the present study are its wide coverage of a single community and its comprehensive assessment of MetS. The fairly low participation rate in the BDI analysis (55% of the age cohorts) may have affected the results and therefore generalizations should be made with caution. The age and gender profiles of the BDI respondents differed slightly from those of the non-respondents. MetS prevalence was lower among the complete respondents (n = 416) than among the non-respondents or the respondents with incomplete answers (n = 64) with no statistical significance. The under-representation of MetS in the respondent group, if anything, weakened the associations detected.
Of all the subjects in the health survey, 38 (8% of the health survey participants) did not respond at all to the BDI-21 questionnaire, which may be due to the fact that some of the statements in the depression inventory are quite sensitive, and for some subjects they might be too personal to be shared with others. Another 26 subjects (5% of the health survey participants) filled in the questionnaire incompletely, perhaps due to inadequate supervision during the completion procedure. As there were marked differences between genders, we reported the main results by gender. This may have affected the statistical power of the study.
The assessment of depression was based on a self-rating instrument, which bears three obvious limitations. First, subjects may exaggerate symptoms in order to make their situation worse. Second, they may under-report the severity or frequency of symptoms in order to minimize their problems. Third, due to the differences in the severity of the single BDI-21 items, simple addition of the item scores is problematic. However, BDI cut-off points are widely used by researchers all over the world.
Interestingly, change in waist circumference of 1 cm was associated with a 7% change in the risk of depression, even though the logistic regression was adjusted for the presence of MetS and variables closely associated with abdominal obesity. Therefore, increased waist circumference especially in women should prompt comprehensive assessment of physical and mental well-being.
Due to the cross-sectional nature of the study, it is not possible to measure the course of time of the change. Therefore, the question remains as to whether a large waist circumference and elevated plasma glucose level are preceded or followed by depression.
Comparison with existing literature
The present study recorded a prevalence of MetS similar to that reported in previous population studies in Finland [21]. There are several studies at the population level with conflicting findings on the association between MetS and depression [8–15]. It is noteworthy, however, that most of them have been done with depression cut-off points that classify subjects as either depressive or non-depressive. This bears obvious methodological weaknesses, and does not do justice to the diversity of depressive symptoms. Therefore, we added the BDI-21 profile by MetS status. It has been suggested earlier that possible mediating mechanisms of impaired mental performance in MetS may be multifactorial and may vary from one person to another [23].
The association of fatigue-related symptoms and sexual dysfunction with obesity is well documented [24–27], while with MetS without marked obesity it is only preliminary [10], [28–30]. Subjects with major depression are more likely to accumulate visceral fat, as assessed by computerized tomography [31]. Our results support this finding, especially among women, in which depressive symptoms showed a clear association with a large waist circumference, a surrogate marker of visceral fat. It is likely that a large waist circumference is associated with fatigue-related symptoms and loss of libido below the level of clinically significant obesity.
Depression is a known associate of diabetes, but association between depression and an elevated blood glucose level in non-diabetic subjects is open to doubt [11], [32], [33]. In our study, however, fasting plasma glucose level was significantly associated with self-perceived depression in men. Our novel finding is that perceived depression may be associated with an elevated plasma glucose level with or without diabetes especially among men. Therefore self-perceived depression may be one of the first signs of diabetes.
Implications for future research and clinical practice
Our findings support previous statements concerning the importance of assessing the association between MetS and self-perceived depression. Further research should throw more light on the course of time and the nature of their association. The association between MetS and depression is noteworthy in clinical practice, and therefore effective prevention and treatment of metabolic syndrome could also be important for the prevention of depression.
Acknowledgements
The authors would like to thank the participating Lapinlahti residents and the staff members of the Lapinlahti Primary Health Care Centre and the Kuopio University Hospital Laboratory. The study would not have been possible without the financial support of the municipality of Lapinlahti and the Development Programme for the Prevention and Care of Diabetes in Finland (DEHKO/D2D) through the Northern Savo Hospital District.
References
- 1.Wells KB, Stewart A, Hays RD, Burnam MA, Rogers WH, Hays RD, et al. The functioning and well-being of depressed patients: Results from the Medical Outcomes Study. JAMA. 1989;262:914–9. [PubMed] [Google Scholar]
- 2.Evans DL, Charney DS, Lewis L, Golden RN, Gorman JM, Krishnan KR, et al. Mood disorders in the medically ill: Scientific review and recommendations. Biol Psychiatry. 2005;58:175–89. doi: 10.1016/j.biopsych.2005.05.001. [DOI] [PubMed] [Google Scholar]
- 3.Verhaak PF, Heijmans MJ, Peters L, Rijken M. Chronic disease and mental disorder. Soc Sci Med. 2005;60:789–97. doi: 10.1016/j.socscimed.2004.06.012. [DOI] [PubMed] [Google Scholar]
- 4.Wulsin LR, Vaillant GE, Wells VE. A systematic review of the mortality of depression. Psychosom Med. 1999;61:18–20. doi: 10.1097/00006842-199901000-00003. [DOI] [PubMed] [Google Scholar]
- 5.Eckel RH, Grundy SM, Zimmet PZ. The metabolic syndrome. Lancet. 2005;365:1415–28. doi: 10.1016/S0140-6736(05)66378-7. [DOI] [PubMed] [Google Scholar]
- 6.Laaksonen DE, Lakka HM, Niskanen LK, Kaplan GA, Salonen JT, Lakka TA. Metabolic syndrome and development of diabetes mellitus: Application and validation of recently suggested definitions of the metabolic syndrome in a prospective cohort study. Am J Epidemiol. 2002;156:1070–7. doi: 10.1093/aje/kwf145. [DOI] [PubMed] [Google Scholar]
- 7.Facchini FS, Hua N, Abbasi F, Reaven GM. Insulin resistance as a predictor of age-related diseases. J Clin Endocrinol Metab. 2001;86:3574–8. doi: 10.1210/jcem.86.8.7763. [DOI] [PubMed] [Google Scholar]
- 8.Guize L, Thomas F, Pannier B, Bean K, Danchin N, Benetos A. Metabolic syndrome: Prevalence, risk factors and mortality in a French population of 62000 subjects. Bull Acad Natl Med. 2006;190:685–97. (abstract in English) [PubMed] [Google Scholar]
- 9.Herva A, Rasanen P, Miettunen J, Timonen M, Laksy K, Veijola J, et al. Co-occurrence of metabolic syndrome with depression and anxiety in young adults: The Northern Finland 1966 Birth Cohort Study. Psychosom Med. 2006;68:213–16. doi: 10.1097/01.psy.0000203172.02305.ea. [DOI] [PubMed] [Google Scholar]
- 10.Timonen M, Laakso M, Jokelainen J, Rajala U, Meyer-Rochow VB, Keinanen-Kiukaanniemi S. Insulin resistance and depression: Cross sectional study. BMJ. 2005;330:17–18. doi: 10.1136/bmj.38313.513310.F71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schlotz W, Ambery P, Syddall HE, Crozier SR, Sayer AA, Cooper C, Phillips DI. The Hertfordshire Cohort Study Group. Specific associations of insulin resistance with impaired health-related quality of life in the Hertfordshire Cohort Study. Qual Life Res. 2007;16:429–36. doi: 10.1007/s11136-006-9129-5. [DOI] [PubMed] [Google Scholar]
- 12.Kinder LS, Carnethon MR, Palaniappan LP, King AC, Fortmann SP. Depression and the metabolic syndrome in young adults: Findings from the Third National Health and Nutrition Examination Survey. Psychosom Med. 2004;66:316–22. doi: 10.1097/01.psy.0000124755.91880.f4. [DOI] [PubMed] [Google Scholar]
- 13.Räikkonen K, Matthews KA, Kuller LH. The relationship between psychological risk attributes and the metabolic syndrome in healthy women: Antecedent or consequence? Metabolism. 2002;51:1573–7. doi: 10.1053/meta.2002.36301. [DOI] [PubMed] [Google Scholar]
- 14.Räikkönen K, Matthews KA, Kuller LH. Depressive symptoms and stressful life events predict metabolic syndrome among middle-aged women: A comparison of World Health Organization, Adult Treatment Panel III, and International Diabetes Foundation definitions. Diabetes Care. 2007;30:872–7. doi: 10.2337/dc06-1857. [DOI] [PubMed] [Google Scholar]
- 15.Engum A. The role of depression and anxiety in onset of diabetes in a large population-based study. J Psychosom Res. 2007;62:31–8. doi: 10.1016/j.jpsychores.2006.07.009. [DOI] [PubMed] [Google Scholar]
- 16.Heiskanen TH, Niskanen LK, Hintikka JJ, Koivumaa-Honkanen HT, Honkalampi KM, Haatainen KM, et al. Metabolic syndrome and depression: A cross-sectional analysis. J Clin Psychiatry. 2006;67:1422–7. doi: 10.4088/jcp.v67n0913. [DOI] [PubMed] [Google Scholar]
- 17.Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–71. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 18.Viinamäki H, Tanskanen A, Honkalampi K, Koivumaa-Honkanen H, Haatainen K, Kaustio O, et al. Is the Beck Depression Inventory suitable for screening major depression in different phases of the disease? Nord J Psychiatry. 2004;58:49–53. doi: 10.1080/08039480310000798. [DOI] [PubMed] [Google Scholar]
- 19.Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, et al. Diagnosis and management of the metabolic syndrome: An American Hearth Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation. 2005;112:2735–52. doi: 10.1161/CIRCULATIONAHA.105.169404. [DOI] [PubMed] [Google Scholar]
- 20.Ford ES. Prevalence of the metabolic syndrome defined by the International Diabetes Federation among adults in the US. Diabetes Care. 2005;28:2745–9. doi: 10.2337/diacare.28.11.2745. [DOI] [PubMed] [Google Scholar]
- 21.Ilanne-Parikka P, Eriksson JG, Lindstrom J, Hamalainen H, Keinanen-Kiukaanniemi S, Laakso M, et al. Finnish Diabetes Prevention Study Group. Prevalence of the metabolic syndrome and its components: Findings from a Finnish general population sample and the Diabetes Prevention Study cohort. Diabetes Care. 2004;27:2135–40. doi: 10.2337/diacare.27.9.2135. [DOI] [PubMed] [Google Scholar]
- 22.Troxel WM, Matthews KA, Gallo LC, Kuller LH. Marital quality and occurrence of the metabolic syndrome in women. Arch Intern Med. 2005;165:1022–7. doi: 10.1001/archinte.165.9.1022. [DOI] [PubMed] [Google Scholar]
- 23.Gans RO. The metabolic syndrome, depression, and cardiovascular disease: Interrelated conditions that share pathophysiological mechanisms. Med Clin North Am. 2006;90:573–91. doi: 10.1016/j.mcna.2006.05.002. [DOI] [PubMed] [Google Scholar]
- 24.Vgontzas AN, Bixler EO, Chrousos GP. Obesity-related sleepiness and fatigue: The role of the stress systems and cytokines. Ann N Y Acad Sci. 2006;1083:329–44. doi: 10.1196/annals.1367.023. [DOI] [PubMed] [Google Scholar]
- 25.Lim W, Hong S, Nelesen R, Dimsdale JE. The association of obesity, cytokine levels, and depressive symptoms with diverse measures of fatigue in healthy subjects. Arch Intern Med. 2005;165:910–5. doi: 10.1001/archinte.165.8.910. [DOI] [PubMed] [Google Scholar]
- 26.Larsson U, Karlsson J, Sullivan M. Impact of overweight and obesity on health-related quality of life: A Swedish population study. Int J Obes Relat Metab Disord. 2002;26:417–24. doi: 10.1038/sj.ijo.0801919. [DOI] [PubMed] [Google Scholar]
- 27.Esposito K, Giugliano D. Obesity, the metabolic syndrome, and sexual dysfunction. Int J Impot Res. 2005;17:391–8. doi: 10.1038/sj.ijir.3901333. [DOI] [PubMed] [Google Scholar]
- 28.Niskanen L, Laaksonen DE, Punnonen K, Mustajoki P, Kaukua J, Rissanen A. Changes in sex hormone-binding globulin and testosterone during weight loss and weight maintenance in abdominally obese men with the metabolic syndrome. Diabetes Obes Metab. 2004;6:208–15. doi: 10.1111/j.1462-8902.2004.00335.x. [DOI] [PubMed] [Google Scholar]
- 29.Esposito K, Ciotola M, Marfella R, Di Tommaso D, Cobellis L, Giugliano D. Sexual dysfunction in women with the metabolic syndrome. Diabetes Care. 2005;28:756. doi: 10.2337/diacare.28.3.756. [DOI] [PubMed] [Google Scholar]
- 30.Korhonen S, Hippelainen M, Vanhala M, Heinonen S, Niskanen L. The androgenic sex hormone profile is an essential feature of metabolic syndrome in premenopausal women: A controlled community-based study. Fertil Steril. 2003;79:1327–34. doi: 10.1016/s0015-0282(03)00347-9. [DOI] [PubMed] [Google Scholar]
- 31.Weber-Hamann B, Werner M, Hentschel F, Bindeballe N, Lederbogen F, Deuschle M, et al. Metabolic changes in elderly patients with major depression: Evidence for increased accumulation of visceral fat at follow-up. Psychoneuroendocrinology. 2006;31:347–54. doi: 10.1016/j.psyneuen.2005.08.014. [DOI] [PubMed] [Google Scholar]
- 32.Adriaanse MC, Dekker JM, Spijkerman AM, Twisk JW, Nijpels G, van der Ploeg HM, et al. Diabetes-related symptoms and negative mood in participants of a targeted population-screening program for type 2 diabetes: The Hoorn Screening Study. Qual Life Res. 2005;14:1501–9. doi: 10.1007/s11136-004-0028-3. [DOI] [PubMed] [Google Scholar]
- 33.Earle CM, Stuckey BG. Biochemical screening in the assessment of erectile dysfunction: What tests decide future therapy? Urology. 2003;62:727–31. doi: 10.1016/s0090-4295(03)00508-9. [DOI] [PubMed] [Google Scholar]