Abstract
Objective
To analyse which interventions are effective in influencing morbidity, quality of life, and healthcare utilization of frequently attending patients (FAs) in primary care.
Methods
A systematic literature search was performed for articles describing interventions on FAs in primary care (Medline, Embase, and PsycINFO). Outcomes were morbidity, quality of life (QoL), and use of healthcare. Two independent assessors selected all randomized clinical trials (RCT) and assessed the quality of the selected RCTs.
Results
Five primary care based RCTs were identified. Three RCTs used frequent attendance to select patients at risk of distress, major depression, and anxiety disorders. These RCTs applied psychological and psychiatric interventions and focused on undiagnosed psychiatric morbidity of FAs. Two of them found more depression-free days and a better QoL after treating major depressive disorder in FAs. No other RCT found any positive effect on morbidity or QoL. Two RCTs studied an intervention which focused on reducing frequent attendance. No intervention significantly lowered attendance. Due to the difference in study settings and the variation in methods of selecting patients, meta-analysis of the results was not possible.
Conclusion
No study showed convincing evidence that an intervention improves QoL or morbidity of frequent attending primary care patients, although a small effect might be possible in a subgroup of depressed frequent attenders. No evidence was found that it is possible to influence healthcare utilization of FAs.
Keywords: Family practice, frequent attendance, frequent attender, health services/utilization, intervention studies, RCT, review
There is little knowledge on whether interventions are effective in influencing morbidity, quality of life, or healthcare utilization of frequent attenders in primary care.
After a systematic search five randomized clinical trials were found describing interventions on frequent attenders.
No study showed convincing evidence that an intervention improves quality of life or morbidity of frequent attending primary care patients, although a small effect might be possible in a subgroup of depressed frequent attenders.
No evidence was found that it is possible to influence healthcare utilization of frequent attenders.
Primary care physicians (PCP) spend about 80% of their time on 20% of their patients: about one in every seven consultations concerns the top 3% of attenders [1]. Two systematic reviews confirm that these frequent attenders (FAs) have high rates of physical disease, emotional distress, psychiatric illness, and social difficulties [2], [3].
Frequent attenders can be divided into five sub-groups: patients with purely somatic illness (28%), patients with clear psychiatric illness (21%), patients in temporary crisis (10%), chronically somatizing patients (21%), and those with multiple problems (20%) [4]. In most cases somatic and psychiatric illnesses are accepted reasons for frequent consultation. Crises pass and are a reason for frequent consultation for a short time. However, frequent attendance by multi-problem patients with related but undetected psychiatric morbidity is thought to lead to unnecessary consultations and therefore to ineffective healthcare [5]. Detecting, diagnosing, and treating this morbidity should improve FAs’ quality of life as well as lower the impact of frequent attending on the healthcare system [6].
The objective of this study is to analyse which interventions might be effective in reducing morbidity and consultation frequency while improving the quality of life of FAs. We performed a systematic review of interventions on FAs aimed at answering three questions: (1) which interventions have been studied, (2) at which group of FAs were these targeted, and (3) what was the effect of the interventions in terms of morbidity, quality of life, and consultation frequency?
Material and methods
Literature search
We searched the databases Medline, Embase, and PsycINFO (1980–November 2006) with the following MESH headings: “health services/utilization”, “health services misuse” and “healthcare utilization”, and the following truncations as text words: “frequent attend*”, “frequent consult*”, “high utiliz*”, “high consultation frequency”, “high consultation rate”. To obtain maximal sensitivity we combined all search terms with “or” and used no additional restrictions. In addition we checked the references of all included articles for other relevant but not yet retrieved articles.
Selection of articles
We used title and abstract to select articles, which described interventions in FAs in primary care, and were written in the English, French, Dutch, or German language. We included only studies on FAs older than 14 years. We included all possible FA definitions, also definitions based on specific (sub-)groups of primary care patients. We defined primary care as all first points of consultation sites, non-in-hospital care. When there was any doubt about the setting or the kind of included patients we assessed the full paper. The FA definitions used in the final selection of articles are presented in Table I.
Table I.
Overview of the selected randomized clinical trials.
| Setting | Definition Fas (kind of counted contacts) | Population | Identification | Number of intervention /control patients | Intervention | Follow-up | Outcomes | Results | |
| Simon8 | Primary care clinic, 3 prepaid health plans in Midwest, Northwest and New England (USA) | Top15% attenders during 2 consecutive years – outpatient medical visits | Age: 23–63 | Electronic data SCID: Pos MDD or MDD pos. last 2 yrs (=1475 pat) HDRS >14 163 General practices: Usual care: 81 Intervention: 82 | Intervention: 218 Usual care: 189 | Depression management programme (DMP): – 2 h training Evaluation contact Antidepressant medication (AD) Information material Treatment coordinator | 1 year after randomization. | Depression-free days Costs | More depression-free days (229– > 182) More costs (+$51.84 per additional depression-free day) |
| Katzelnick9 | Primary care clinic, 3 prepaid health plans in Midwest, Northwest and New England (USA) | Top15% attenders during 2 consecutive years – outpatient medical visits | Age: 25–63 | Electronic data SCID: Pos MDD or MDD pos last 2 yrs (= 1475 pat) HDRS > 14 163 General practices: Usual care: 81 Intervention: 82 | Intervention: 218 Usual care: 189 | Depression management programme (DMP): – 2 h training Evaluation contact – antidepressant medication – information material – treatment coordinator | 1 year after randomization | HDRS SF-20 score Use of antidepressant medication Attendance | Improvement HDRS (13.6–> 9.9 at 1 year) More use of AD (69.3% of DMP patients and 18.5% of usual-care patients with at least 3 prescriptions in 0.5 year) Better SF-20 scores for social function, mental health, gen. health perceptions More attendance in year after inclusion (+3, 2) |
| Katon10 | Primary care clinics of HMO, Washington State (USA) | Top 10% attenders in 1 year for sex and age – ambulatory healthcare visits | Age: 18–75 –18 GPs out HMO –300 000 patients | >2 Years in practice Selection from electronic data SCL-R one standard deviation above mean –> 339 patients – 251 Accepted randomization | Intervention: 124 Control: 127 | DIS by psychiatrist Interview by the psychiatrist with the GP present Jointly formulated treatment plan Written protocol of treatment for GP | 1 year after randomization | Use of antidepressant med. (AD) Rate of anxiety/depression Use (psych) healthcare | More AD (+38%) No better psych. State No lower use of healthcare and costs |
| Olbrisch11 | Primary healthcare for students: Florida State University (USA) | > 4 face-to-face contacts in first quarter of study year – outpatient medical visits | Freshmen, sophomores and juniors: students university health centre | 400 students – 300 got letter – 129 agreed – 112 randomized Plus “no contact” group | Intervention: 34 Control: 40 No contact: 30 | Brief educational programme (group of 3–8 students) | 1 year after intervention | Number of contacts primary care Use of other healthcare | Lower use of primary care in short term. Convergence towards same utilization during follow-up No differences in number of visits to other healthcare providers |
| Christensen12 | Primary care out-of-hours service, County of Northern Jutland (Denmark) | > 4 Out-of-hours contacts one year before inclusion – consultations, home visits and telephone calls | No age restriction | Consecutive patients Randomization per practice | Intervention practices: 83 GPs; 3500 patients Control practices: 93 GPs 4635 patients | Status consultation by GP Education of participating GPs Questionnaire patients Economic incentives GP | 1 year after the intervention | Number of contacts with the out-of-hours service Daytime contacts with the GP; hospital admissions; visits to hospital outpatient clinics | No convincing effect |
Notes: SCID = Structured Clinical Interview DSM; MDD = major depressive disorder; HDRS = Hamilton Depression Rating Scale; SF = social functioning; SCL-R Symptom Checklist – Revised; DIS = Diagnostic Interview Schedule.
All articles that met the inclusion criteria were read in detail to select only randomized controlled trials (RCT) and to re-check the inclusion and exclusion criteria. Two assessors (FS, KW) performed these procedures independently and the final selection was discussed in a consensus meeting with a third assessor (HW).
Quality assessment
Two reviewers (FS, KW) appraised each RCT independently with the quality criteria for assessment of experimental studies of Khalid Khan et al. [7]. This checklist consists of nine items on methodological quality scored as yes, no, or uncertain. Points of disagreement were discussed with a third senior assessor (HW) for a final decision. Because of the differing study settings and the variation in studied populations, pooling of the results was not possible.
Results
Literature search
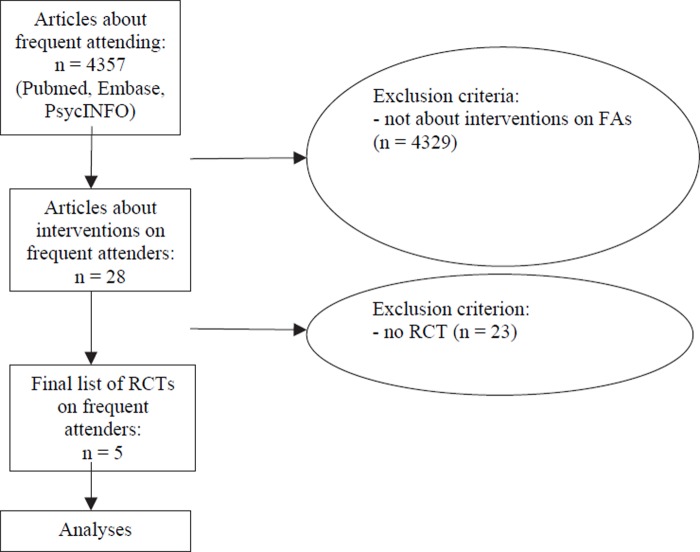
We found 4357 articles of which after the first selection 28 were retrieved for detailed reading (Figure 1). The second selection resulted in the identification of five RCTs (see Table I for a summary of the RCTs).
Figure 1. .
Flow diagram: Selection of articles.
Included studies
Simon et al. and Katzelnick et al. refer to the same research programme [8], [9]. Their main goal was the evaluation of a depression management programme among depressed FAs. The selected FAs (n = 7203) were screened using the depression module of the Structured Clinical Interview for DSM-IV. Finally, a total of 407 patients with a Hamilton Depression Rating Scale score of 15 or more consented to enrolment: 218 patients were randomized to the depression management programme and 189 patients received the usual care. Intervention: The programme included a two-hour physician training programme, an evaluation visit with their PCP immediately after enrolment, antidepressant medication if appropriate, written and videotaped educational materials, and treatment coordination. Outcome measures were number of depression-free days, prescription of antidepressants, improvement on the Hamilton and SF-20, and healthcare use and costs. Results: In the year following the intervention patients in the intervention group had a mean of 47 more depression-free days (CI 26.6–68.2), more prescriptions for antidepressants (69.3% of intervention patients and 18.5% of usual-care patients had filled at least three antidepressant prescriptions for the six-month period after enrolment; p < 0.001), more improvement on the Hamilton (change in 12 months for intervention patients 9.2 and for usual-care patients 5.6; p < 0.001), more improvement on the SF-20 scores for social functioning, mental health, and general health perceptions (p < 0.05), and intervention patients had 3.2 more contacts with the healthcare system (CI 0.70–5.80) as well as more costs (US$51.84 per additional depression-free day; CI 17.37–108.47).
Katon et al. evaluated a psychiatric consultation-liaison programme among distressed FAs [10]. They selected 1790 FAs, of which 339 distressed FAs were selected by using the Symptoms Checklist Revised; sum score 1 standard deviation above population mean. Of these distressed FAs, 251 gave consent for randomization, 124 patients were assigned to the intervention group, and 127 to the control group. The intervention consisted of a Diagnostic Interview Schedule by a psychiatrist with the family physician present, a jointly formulated treatment plan and a mutually accepted course of action (i.e. medication adjustment, referral, fixed-interval visits etc.). The outcome measures were rates of anxiety and depression, use of antidepressants and use of healthcare. Results: After one year Katon found no significant difference in improvement of psychopathology, more prescribed antidepressants (+ 38%; p < 0.01) in the intervention group and no consistently significant differences in any utilization measure between intervention and control groups.
Olbrisch refers to an intervention among frequent attending students [11]. Her purpose was to evaluate the effectiveness of an intervention aimed at making students aware of the psychological and social factors that make people prone to illness and to inappropriate use of healthcare. Three hundred randomly selected and eligible students were invited to participate, 129 agreed and 112, who kept appointments, were randomized to the intervention group (n = 34) or the control group (n = 40). Olbrisch also selected a matched group with no contacts (n = 30). The exact routing of all study participants is not clearly described. Her intervention consisted of a brief educational group programme (presentations, discussion, and a demonstration or audiotape of deep muscle relaxation). The outcome measure was use of healthcare facilities. Results: The intervention group showed reduced utilization of the university health centre for a short period of time (not adequately specified), with this effect dissipating over time and no significant differences on the number of visits to other healthcare providers (F(2.85) = 1.7; p = 0.19).
In the only RCT outside the USA, Christensen et al. studied an out-of-hours primary care service in Denmark [12]. They tested whether a combination of intervention strategies reduced healthcare utilization by FAs. In a cluster randomization, family physician practices were randomized to intervention practices (83 practices; 3500 patients) and control practices (93 practices; 4635 patients). The intervention consisted of (1) a patient questionnaire and an invitation for the FAs to contact their family physician for a status consultation, (2) information about the project and FAs for the PCP, (3) PCP group education on frequent attending (29% of all PCPs representing 40% of all practices participated), and (4) economic incentives for the PCP to perform the status consultation. Outcome measures were (1) the number and kind of contacts with the out-of-hours-service, and (2) daytime contacts with PCP, hospital admissions, and visits to hospital outpatient clinics and emergency departments. Results: They found no significant difference in the primary and secondary outcome measures.
Quality assessment
The quality assessment of the included RCTs is summarized in Table II. None of the RCTs fully complied with all quality criteria. In none of the RCTs were patient and care provider sufficiently blinded. Blinding of patients and physicians was not possible in the studies of Simon, Katzelnick, Olbrish, and Katon because psychological treatments do not allow concealment. Katon, Olbrisch, and Christensen did not include an intention-to-treat-analysis. Olbrisch did not describe whether the outcome assessors were blinded to the treatment allocation and did not give point estimates and measures of variability. Christensen did not go into detail about point estimates and measures of variability. All articles, except Christensen's, refer to various subgroups of FAs. Therefore it was not possible to generalize the results of these studies to all FAs.
Table II.
Qualitative assessment selected RCTs.
| Quality criteria7 | Simon8 | Katzelnick9 | Katon10 | Olbrisch11 | Christensen12 |
| Assignment to the treatment groups really random? | + | + | + | ? | + |
| Treatment allocation concealed? | + | + | ? | ? | − |
| Groups similar at baseline in terms of prognostic factors? | + | +1 | + | + | ? |
| Were the eligibility criteria specified? | + | + | + | + | + |
| Outcome assessors blinded to the treatment allocation? | + | + | + | − | n.a. |
| Was the care provider blinded? | − | − | − | − | − |
| Was the patient blinded? | − | − | − | − | − |
| Points estimates and measure of variability presented for the primary outcome measure? | + | + | + | − | − |
| Analyses included an intention to treat analysis? | +2 | + | − | − | − |
Notes: 1After correction no different result. 2Not mentioned in this article. Katzelnick does mention the criteria.
Discussion
Main findings
We identified five primary-care-based RCTs. Three RCTs used frequent attendance to select patients at risk of distress, major depression, and anxiety disorders. These RCTs applied psychiatric interventions and focused on undiagnosed psychiatric morbidity of FAs. Two of them found more depression-free days and reported a better QoL after treating a major depressive disorder in a subgroup of depressed FAs, but also more contacts, more prescriptions for antidepressants, and more costs in the intervention group within one year of follow-up [8], [9]. The net gain on a group level was disappointing: for every Structured Clinical Interview for DSM-IV 2.6 depression-free days could be achieved. One RCT found no effect on morbidity, but more prescription of antidepressants [10]. Except Simon and Katzelnick no other RCT included clear measures of QoL. Two RCTs studied an intervention which focused on reducing frequent attendance [11], [12]. All RCTs concluded that the studied interventions did not significantly lower attendance during one year of follow-up.
Strengths and limitations
A limitation was the differences in study settings and the variation in methods of selecting patients. Four studies were carried out in the USA (three Health Maintenance Organizations; one university healthcare), one in Denmark (out-of-hours-service). Frequent attendance is not a clearly defined concept. Two studies selected patients who were FAs for two consecutive years (Simon, Katzelnick). Other studies used three months (Olbrisch) or one year (Katon, Christensen). Three studies selected a percentile of most attending patients; two used a certain number of consultations as a selecting criterion. In three studies, frequent attendance was used to select a group of patients at risk for psychiatric disorders [8–10]. The other two made no selection and intervened in all FAs [11], [12].
Different interventions were used: in three studies interventions consisted of a screening and depression management programme and an intervention by a psychiatrist [8–10]. One used an educational group programme [11]. In only one study was the intervention carried out by a PCP and focused on diminishing attendance [12]. Due to the low number of PCPs trained, it is likely that the success of this intervention was underestimated.
Because of all these differences we can not generalize results to other (subgroups of) FAs or to a certain intervention. Frequent attendance is the result of many disease- and personality-linked factors which make FAs a heterogeneous group of patients [4]. Intervening on a specific aspect of frequent attendance, for instance depression, dilutes the outcome of an RCT which studies all FAs. Moreover, frequent attendance is not a consistent personality trait, but often a transitory characteristic. Some studies show that up to 60–70% of frequently attending patients change their health-seeking behaviour within 2–3 years [13–16]. Using healthcare utilization as an outcome measure therefore does not seem adequate in studying FAs, defined on a one-year basis. Studies that did find an effect used consultation patterns on a two-year basis [8], [9]. The net effect of an intervention on healthcare utilization in the short term logically is upwards and a follow-up of longer than one year is needed.
The strength of this study, the first that reviews interventions on FAs, is the sensitive search with both Mesh headings and text words without any prior limitation. We therefore expect not to have missed any RCT describing an intervention in FAs.
Comparison with relevant literature
There is an extensive literature about the characteristics of (sub-)groups of FAs. There are few studies (n = 28) which try to influence morbidity, QoL, and use of healthcare of FAs. Only five are RCTs. Definitions of FAs differed considerably. We propose to follow the advice of Vedsted et al. to define FAs as the top 10% of all enlisted patients [2].
Conclusion
We found a small number of studies that evaluated interventions on FAs. There is no evidence that it is possible to influence healthcare utilization by frequent attenders. Treatment of (not yet diagnosed) major depressive disorder might improve the symptoms and the quality of life of depressed FAs, but will not reduce their consultation rate within one year of follow-up.
Acknowledgements
Ethics committee: Not applicable.
Funding body: Stichting steunfonds medische en sociale dienstverlening Reigersbos (Foundation to support medical and social services Reigersbos).
Conflict of interest: The authors have stated that there are none.
References
- 1.Neal RD, Heywood PL, Morley S, Clayden AD, Dowell AC. Frequency of patients consulting in general practice and workload generated by frequent attenders: Comparisons between practices. Br J Gen Pract. 1998;48:895–8. [PMC free article] [PubMed] [Google Scholar]
- 2.Vedsted P, Christensen MB. Frequent attenders in general practice care: A literature review with special reference to methodological considerations. Public Health. 2005;119:118–37. doi: 10.1016/j.puhe.2004.03.007. [DOI] [PubMed] [Google Scholar]
- 3.Gill D, Sharpe M. Frequent consulters in general practice: A systematic review of studies of prevalence, associations and outcome. J Psychosom Res. 1999;47:115–30. doi: 10.1016/s0022-3999(98)00118-4. [DOI] [PubMed] [Google Scholar]
- 4.Karlsson H, Joukamaa M, Lahti I, Lehtinen V, Kokki-Saarinen T. Frequent attender profiles: Different clinical subgroups among frequent attender patients in primary care. J Psychosom Res. 1997;42:157–66. doi: 10.1016/s0022-3999(96)00287-5. [DOI] [PubMed] [Google Scholar]
- 5.Katon W, Von KM, Lin E, Lipscomb P, Russo J, Wagner E, et al. Distressed high utilizers of medical care. DSM-III-R diagnoses and treatment needs. Gen Hosp Psychiatry. 1990;12:355–62. doi: 10.1016/0163-8343(90)90002-t. [DOI] [PubMed] [Google Scholar]
- 6.Dowrick CF, Bellon JA, Gomez MJ. GP frequent attendance in Liverpool and Granada: The impact of depressive symptoms. Br J Gen Pract. 2000;50:361–5. [PMC free article] [PubMed] [Google Scholar]
- 7.Khan KS, ter Riet G, Popay J, Nixon J, Kleijnen J. Undertaking systematic reviews of research on effectiveness CRD's guidance for carrying out or commissioning reviews: 2. York: NHS Centre for Reviews and Dissemination (CRD), University of York; 2001. Study quality assessment. [Google Scholar]
- 8.Simon GE, Manning WG, Katzelnick DJ, Pearson SD, Henk HJ, Helstad CS. Cost-effectiveness of systematic depression treatment for high utilizers of general medical care. Arch Gen Psychiatry. 2001;58:181–7. doi: 10.1001/archpsyc.58.2.181. [DOI] [PubMed] [Google Scholar]
- 9.Katzelnick DJ, Simon GE, Pearson SD, Manning WG, Helstad CP, Henk HJ, et al. Randomized trial of a depression management program in high utilizers of medical care. Arch Fam Med. 2000;9:345–51. doi: 10.1001/archfami.9.4.345. [DOI] [PubMed] [Google Scholar]
- 10.Katon W, Von KM, Lin E, Bush T, Russo J, Lipscomb P, et al. A randomized trial of psychiatric consultation with distressed high utilizers. Gen Hosp Psychiatry. 1992;14:86–98. doi: 10.1016/0163-8343(92)90033-7. [DOI] [PubMed] [Google Scholar]
- 11.Olbrisch ME. Evaluation of a stress management program for high utilizers of a prepaid university health service. Med Care. 1981;19:153–9. doi: 10.1097/00005650-198102000-00003. [DOI] [PubMed] [Google Scholar]
- 12.Christensen MB, Christensen B, Mortensen JT, Olesen F. Intervention among frequent attenders of the out-of-hours service: A stratified cluster randomized controlled trial. Scand J Prim Health Care. 2004;22:180–6. doi: 10.1080/02813430410006576. [DOI] [PubMed] [Google Scholar]
- 13.Ward AM, Underwood P, Fatovich B, Wood A. Stability of attendance in general practice. Fam Pract. 1994;11:431–7. doi: 10.1093/fampra/11.4.431. [DOI] [PubMed] [Google Scholar]
- 14.Andersson S-O, Lynoe N, Hallgren C-G, Nilsson M. Is frequent attendance a persistent characteristic of a patient? Repeat studies of attendance pattern at the family practitioner. Scand J Prim Health Care. 2004;22:91–4. doi: 10.1080/02813430410005207. [DOI] [PubMed] [Google Scholar]
- 15.Carney TA, Guy S, Jeffrey G. Frequent attenders in general practice: A retrospective 20-year follow-up study. Br J Gen Pract. 2001;51:567–9. [PMC free article] [PubMed] [Google Scholar]
- 16.Botica MV, Kovacic L, Tiljak MK, Katic M, Botica I, Rapic M, et al. Frequent attenders in family practice in Croatia: Retrospective study. Croatian Med J. 2004;45:620–4. [PubMed] [Google Scholar]