Abstract
Objective
To analyse the technical quality of electronic patient records in relation to legislation and to evaluate their quality associated with the quality of consultations as rated by patients and GPs.
Design
Cross-sectional study of electronic patient records.
Setting
Four primary healthcare (PHC) centres in Finland using three different electronic patient record systems.
Subjects
Patient records of 175 PHC consultations by 50 GPs, rated as the best (n=86) and the worst (n=89) of a total of 2191 consultations.
Main outcome measures
Documentation of records compared with legislation, the general informative value of records, and its relation to the experienced quality of consultations and to the electronic system employed.
Results
Reason for encounter was mentioned in 79% of cases and patient history in 32%. An acute problem was described moderately well or well in 84%, examination findings in 62%, medical problem or diagnosis in 90%, and treatment in 95% of cases. Medication was documented adequately in 38% of the cases where medication was documented. Concerning general informative value, 18% were assessed as poor, 62% as moderate, and 20% as good. No correspondence was found between experienced quality of consultation and general informative value in the patient records. The quality of patient records was found to change according to the electronic system employed.
Conclusions
Finnish patient records are inadequate documents of consultations and below the standard of that country's legislation. Developing better models of recording would guarantee a higher quality of work.
Keywords: Family medicine, family practice, patient record, quality of consultation
Patient records form an elementary part in every consultation. There is legislation governing patient records in Finland as in other Nordic countries.
The patient records in Finnish primary healthcare are of unsatisfactory quality and do not meet the requirements of the legislation satisfactorily.
The quality of the consultations as rated by GPs and patients is not associated with the informative value of the records.
The electronic patient record system seems to have an impact on the quality of the patient records and should be improved.
Good documentation of patient records has been considered as a basis for good healthcare. In the World Health Organization's (WHO's) “The Role of General Practice in Primary Health Care” the authors claim: “the availability at the time of consultation of high-quality medical records is essential to continuity of care”. The WHO demands that appropriate and systematic updating of medical records is carried out [1].
The patient records are the legal documents of general practitioners’ consultations. For a GP the patient records prompt better care by creating the patient history and identifying episodes or changes of illness. Patient records represent a method of communication for different teams within healthcare. Through patient records healthcare personnel can organize and adjust their work better, and there is a constant communication channel to prevent overlapping procedures. Electronic patient record systems also enable medical data banks to be linked with the patient records [2], [3].
Patient records may also act as a source for scientific analysis. They can be used for statistical and epidemiological studies to monitor the health of a population. They are an essential requirement for quality development, audit of care, and peer review. Patient records can also be used for administration and teaching purposes [2], [3].
For the patient the records represent an opportunity for a better quality of treatment. For example in Finland patients have a legal right to access their own records [2]. As legal documents the patient records can be used in lawsuits alleging negligence. The accuracy of patient records has an increasingly important role to play from the legal viewpoint; similarly the security and confidentiality of the papers are of major importance to the patient.
The Ministry of Social Affairs and Health in Finland issued a decree concerning patient records in 2001. The decree includes rules for data security and rules for retention of patient records and it defines the content of the records in detail. According to the rules, each consultation should be documented correctly containing: reason for encounter; patient history with acute problem, physical examination, and investigations made; medical problem or diagnosis or health-related risk; conclusions; laboratory, imaging, and other investigation referrals; treatment; referrals to hospitals and other institutions; and future treatment plans [3]. Detailed information on prescriptions, the names of the drugs, their dose, and frequency have to be mentioned, according to the decree by the Ministry of Social Affairs and Health concerning the prescription of medication [4].
The legislation in Sweden, Denmark, and Norway comprises similar parameters to those in Finland [5–7]. In 1998, the WHO summed up in its “Framework for professional and administrative development of general practice/family medicine in Europe” what these laws demand: “systematically keeping detailed, problem-oriented and complete records of all encounters is important” [8]. The European definition of general practice/family medicine does not mention patient records at all, although it carefully defines the good quality of general practice [9]. The objective of the European Institute for Health Records, the EUROREC Institute, is to promote the use of high-quality electronic health record systems in Europe rather than to improve the content of patient records [10]. The primary healthcare units in Finland have used electronic patient record systems widely [11] and there is a tradition of keeping accurate records. Therefore, they could be recognized as models of good practice in recording.
There are relatively few studies concerning the quality of patient records and the ones we found concern mainly numerical data and identification of certain parameters [12], [13]. Most studies of patient records concern different electronic patient record systems versus manual systems and the data security of electronic patient records [14–17].
The aims of this study were, first, to find out what the technical quality of the patient records was in Finnish healthcare centres, second, to compare the contents of patient records with the existing legislation, and third, to evaluate whether the quality was associated with quality experienced during consultations. We also studied the impact of the electronic patient record system on the quality of the patient records. Finally, through this pilot study we hope to promote discussion of patient records as one indicator of good quality work.
Material and methods
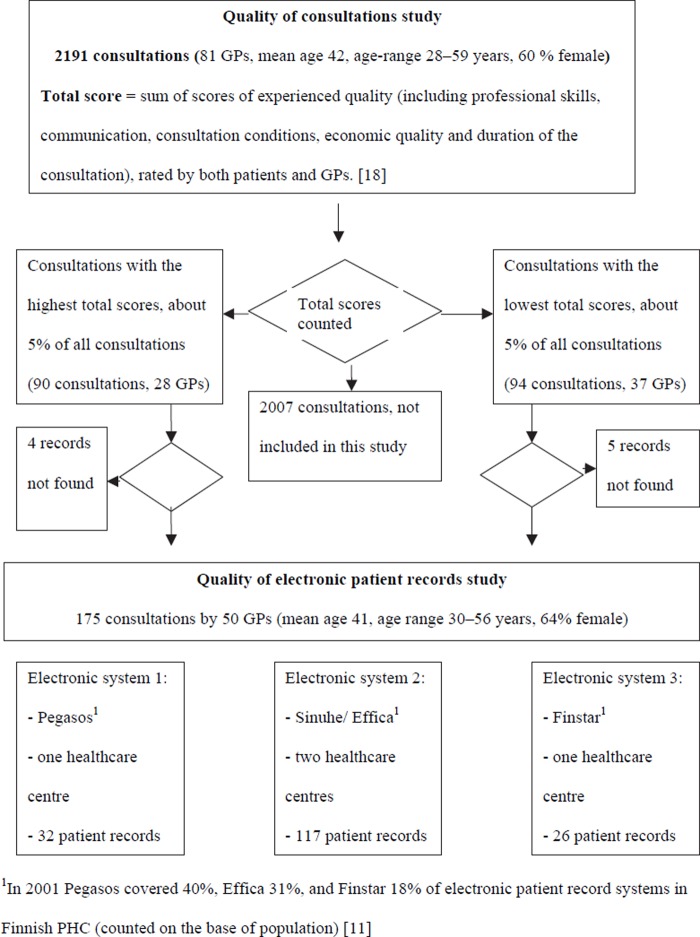
The material for this study consists of 175 patient records of consultations, part of our total material of 2191 consultations gathered in 2000 from four PHC centres in Finland and presented in detail earlier in this journal [18]. Three different electronic patient record systems, Sinuhe/Effica, Pegasos, and Finstar, were used in these PHC centres (Figure 1).
Figure 1. .
Selection of material used in the study.
The basis of selection for this study was the experienced quality of consultations rated by patients and GPs. Altogether, 86 consultations which were scored to represent the highest quality and 89 consultations of the lowest quality were included. In the highest quality group there were consultations with 27 GPs and in the lowest quality group 37 GPs; 15 GPs had consultations in both groups. The mean age of the GPs was 41.4 and 64% of them were female (see Figure 1).
The selected consultation records were analysed by two independent researchers (SV, MK). The main focus was on the correspondence of the patient records with legislation. Patient records were analysed by using a reference list based on the decrees issued by the Finnish Ministry of Health and Social Affairs [3], [4]. The following parameters were surveyed: The existence of reason for encounter and medical problem or diagnosis was recognized. Patient history and acute problem, physical examination findings, treatment, and prescriptions were graded separately as poor, moderate, or good. If information concerning one parameter was not mentioned, it was classified as poor.
In addition, the records were assessed and grouped by focusing on their general informative value: poor, moderate, and good. By “general informative value” we denote the general quality and relevance of the records and whether they described the appointment in a comprehensive way. By poor records we denote records that did not describe the consultation adequately and in which important information was probably missing. In good records the consultation was described well and in an understandable way. Moderately well-written records fell in between. These assessments were further compared according to the electronic system employed in each health centre.
Both researchers reviewed and assessed the papers independently twice with a high consecutive agreement. Comparison of results gave mutual agreement (κ 0.89–0.99). In the case of discrepancies the researchers consulted a third researcher (PV) leading to agreement. Statistical analyses were conducted with SAS (Version 8.01, SAS Institute Inc., Cary, NC). Categorical variables were analysed with chi-squared tests, and a two-sided p-value of<0.05 was considered statistically significant. Exact 95% confidence intervals for percentages were calculated.
Results
Quality of patient records relative to legislation
Reason for the encounter was mentioned in 79% of the patient records, while patient history was found in 32% of cases. An acute problem was described moderately well in 53% and well in 31% of the cases. Physical examination findings were mentioned in 62% of the records. The medical problem or diagnosis was mentioned in 90% of the records. Treatment was relatively well documented, when, according to the patient record, treatment was given. Treatment information was mentioned in 95% in the cases in which both researchers considered it self-evident that some treatment had in fact needed to be given during the consultation (Table I).
Table I.
Assessed quality of recorded parameters in patient records.
| Poor or not mentioned |
Moderate |
Good |
||||
| n | % (95% CI) | n | % (95% CI) | n | % (95% CI) | |
| Patient history | 119 | 68 (61–75) | 42 | 24 (18–31) | 14 | 8 (4–13) |
| Acute problem | 28 | 16 (11–22) | 92 | 53 (45–60) | 55 | 31 (25–39) |
| Status | 67 | 38 (31–46) | 52 | 30 (23–37) | 56 | 32 (25–39) |
| Treatment (n = 154) | 8 | 5 (2–10) | 103 | 67 (59–74) | 43 | 28 (21–36) |
Altogether 38% of the prescription records were made in an adequate manner. For the rest, some aspect of the prescription was missing: the drug name, dose or frequency. The consultations in which no medication according to the record was prescribed (n = 63) were excluded from the data at this point.
Quality of patient records relative to experienced quality of consultation
Concerning the general informative value of the records, altogether 18% of the documents were assessed to be poor, 62% moderate, and 20% good. The quality of recordings was not associated with the quality of the consultations assessed by the patients and GPs (Table II).
Table II.
General informative value of records assessed by the researchers relative to the quality of consultations assessed by the patients and GPs.
| General informative value of the records |
||||
| Poor | Moderate | Good | ||
| Quality of the consultations rated by the patients and GPs | Poor n | 12 | 54 | 20 |
| % (95% CI) | 14% (7–23) | 63% (52–73) | 23% (15–34) | |
| Good n | 20 | 54 | 15 | |
| % (95% CI) | 22% (14–33) | 61% (50–71) | 17% (10–26) | |
Quality of patient record relative to the electronic system
The quality of patient records was found to depend on the electronic system used. The electronic patient record system seemed to have an influence on the documentation procedure. The documentation of prescriptions seemed to differ most due to the electronic system. Two of these systems, Pegasos and Finstar, even copied the content of the prescription routinely in the patient record (Table III).
Table III.
Quality of patient records by electronic system.
| Effica |
Pegasos |
Finstar |
p-value | ||||
| N | % (95% CI) | n | %(95% CI) | n | % (95% CI) | ||
| Patient history | |||||||
| Poor | 87 | 74 (65–82) | 18 | 56 (38–74) | 14 | 54 (33–73) | 0.003 |
| Moderate | 24 | 21 (14–29) | 7 | 22 (9–40) | 11 | 42 (23–63) | |
| Good | 6 | 5 (2–11) | 7 | 22 (9–40) | 1 | 4 (0–20) | |
| Acute problem | |||||||
| Poor | 24 | 21 (14–29) | 2 | 6 (1–21) | 2 | 8 (1–21) | 0.140 |
| Moderate | 60 | 51 (42–61) | 16 | 50 (32–68) | 16 | 50 (32–68) | |
| Good | 33 | 28 (20–37) | 14 | 44 (26–62) | 14 | 44 (26–62) | |
| Status | |||||||
| Poor | 52 | 44 (35–54) | 5 | 16 (5–33) | 10 | 38 (20–60) | 0.006 |
| Moderate | 37 | 32 (23–41) | 18 | 28 (14–47) | 6 | 23 (9–44) | |
| Good | 28 | 24 (17–33) | 56 (38–74) | 10 | 38 (20–60) | ||
| Treatment | |||||||
| Poor | 7 | 6 (2–12) | 0 | 0 | 1 | 4 (0–20) | <0.001 |
| Moderate | 73 | 62 (53–71) | 13 | 41 (24–60) | 17 | 65 (44–83) | |
| Good | 22 | 19 (12–27) | 19 | 59 (41–76) | 2 | 8 (1–25) | |
| No treatment | 10 | 9 (4–15) | 0 | 0 | 6 | 23 (9–45) | |
| Only prescriptions | 5 | 4 (1–10) | 0 | 0 | 0 | 0 | |
| Prescriptions | |||||||
| Poor | 11 | 9 (5–16) | 1 | 3 (0–16) | 1 | 4 (0–20) | <0.001 |
| Moderate | 16 | 14 (8–21) | 7 | 22 (9–40) | 0 | 0 | |
| Good | 31 | 27 (19–35) | 1 | 3 (0–16) | 1 | 4 (0–20) | |
| Excellent | 14 | 12 (7–19) | 12 | 38 (21–56) | 17 | 65 (44–83) | |
| No prescriptions | 45 | 38 (30–48) | 11 | 34 (19–53) | 7 | 27 (12–48) | |
| General informative value | |||||||
| Poor | 22 | 19 (12–27) | 2 | 6 (1–21) | 8 | 31 (14–52) | 0.002 |
| Moderate | 78 | 67 (57–75) | 16 | 50 (32–68) | 14 | 54 (33–73) | |
| Good | 17 | 15 (9–22) | 44 (26–62) | 4 | 15 (4–35) | ||
Discussion
Finnish patient records are of unsatisfactory quality as documentation of consultations. Only one-fifth of the records analysed in this study were considered good in relation to their general informative value. One-fifth were assessed as poor and the rest were considered moderate. The records did not meet the requirements of the legislation satisfactorily. The quality of records seemed to have an association with the electronic system employed, but not with the quality of consultations experienced by patients and GPs.
We claim that patient records do not contain enough adequate information to be used in the way they should and could be used. There is a clear difference between the legislation and the practice of recording. If we cannot rely on patient records to describe the PHC processes accurately, it is questionable whether we are justified in assessing the quality of healthcare on the basis of the present documentation. Patient records are also legal documents and, currently, the legal security of both the patients and the GPs is poor.
Nevertheless, our legislation regulating patient records may not operate satisfactorily for PHC purposes. It is possible that the legislation sets too high requirements for the information in PHC where GPs have increasingly heavy workloads [19]. Continuing records are used, and therefore there is no need to indicate the same patient history repeatedly. Most of the consultations in our sample were recorded in a brief (decursus) manner. PHC patients have often many problems [18], [20], and this seems to make the recording of the encounter more difficult. Not all the requirements of the legislation are fulfilled usually by a separate remark on each problem. One possibility to help the deficiencies would be a good combination of information, which should be reviewed and referred to constantly.
The earlier studies have seldom focused on legislation or quality standards of patient records. The main reason might be the variation in these standards. It is possible that the instructions and standards in the Nordic countries are more detailed than elsewhere in Europe.
Krish Thiru and associates studied the scope and quality of electronic patient records data in primary heathcare by reviewing 52 articles and suggest that an internal reference standard for data quality should be established. According to the present study it is easy to agree with the suggestions of earlier studies that all patient records should be evaluated using continuous standardized quality tools [13]. Electronic patient records have been claimed to have more content that manual records [21], but good recordings do not necessarily mean good care [22] and there is no evidence of their impact on patient outcomes and quality of care [23]. Accordingly, our present study claims that there is no correspondence between the experienced quality of the PHC appointment and the quality of the patient records.
The electronic patient record system seemed to have an influence on the contents of the records in our study. This aspect should be studied more carefully in order to develop electronic patient systems that would help physicians to record all the essential issues. The system should be able automatically to copy the contents of separate data, e.g. prescriptions or referrals, to the patient records.
According to this study, Finland is in no way an exemplary country in PHC recording practices. This presents a big challenge to GPs, but also to the electronic system providers in all countries.
Acknowledgements
The authors would like to thank Tero Vahlberg for biostatistical assistance and Mari Hakkala for language checking.
References
- 1.Boerma WGW, Fleming DM. 1998. The role of general practice in primary health care. Stationery Office for WHO Regional Office for Europe. [Google Scholar]
- 2.Laki potilaan asemasta ja oikeuksista (785/92) [Act on the Status and Rights of Patients in Finland].Helsinki. 1992. Available in English at: http://www.finlex.fi/en/laki/kaannokset/1992/en19920785.pdf. (accessed 15 October 2007) [Google Scholar]
- 3.Opas terveydenhuollon henkilöstölle: Potilasasiakirjojen laatiminen, sekä niiden ja muun hoitoon liittyvän materiaalin säilyttäminen [Drawing up of patient documents and retention of them and other material related to care and treatment. 2001. A guide for healthcare staff] Sosiaali- ja terveysministeriön oppaita, 2001: 3. Helsinki: Ministry of Social Affairs and Health in Finland; (English summary) [Google Scholar]
- 4.Lääkkeiden määrääminen. Sosiaali- ja terveysministeriön määräyskokoelma [Prescription of medication. Regulations of The Ministry of Social Affairs and Health]. Ministry of Social Affairs and Health in Finland; 1999. 50:10. [Google Scholar]
- 5.Socialstyrelsens föreskrifter och allmänna råd, Patientjournallagen [Directions and general advice of The National Board of Health and Welfare, Patient record legislation] Available at: http://www.sos.se/sosfs/1993_20/1993_20.htm. (accessed 15 October 2007) [Google Scholar]
- 6.Bekendtgørelse om lægers, tandlægers, kiropraktorers, jordemødres, kliniske diætisters, kliniske tandteknikeres, tandplejeres, optikeres og kontaktlinseoptikeres patientjournaler (journalføring, opbevaring, videregivelse og overdragelse m.v.) [Statement on the patient records of doctors, dentists, chiropractors, midwives, clinical dieticians, clinical dental technicians, dental nurses, opticians and contact lens opticians (documentation, preserving, forwarding and transfer of data etc.)] Available at: https://www.retsinformation.dk/Forms/R0710.aspx?id=11055. (accessed 15 October 2007) [Google Scholar]
- 7.Sosial- og helsedepartementet. Forskrift om pasientjournal 19/2002. [Ministry of Health and Care Services: Directions on patient records] Available at: http://www.lovdata.no/cgi-wift/ldles?doc=/sf/sf/sf-20001221-1385.html. (accessed 15 October 2007) [Google Scholar]
- 8.WHO Regional Office in Europe. Copenhagen: WHO Regional Office for Europe; 1998. Framework for professional and administrative development of general practice/family medicine in Europe. [Google Scholar]
- 9.Wonca Europe. Ljubljana: Wonca Europe; 2002. The European definition of general practice/family medicine. [Google Scholar]
- 10.European Institute for Health Records. Available at: http://www.eurorec.org. (accessed 15 October 2007) [Google Scholar]
- 11.Hartikainen K, Kuusisto-Niemi S, Lehtonen E. Sosiaali- ja terveydenhuollon tietojärjestelmäkartoitus 2001 [Survey on data systems in social welfare and health care services 2001] National Research and Development Centre for Welfare and Health, 2002. Available at: http://sty.stakes.fi/NR/rdonlyres/00BDBB83-AEE0-467B-949C-EB73DFE12704/1318/osve1_02.pdf. (accessed 15 October 2007) [Google Scholar]
- 12.Okuyemi KS, Harris KJ, Ahluwalia JS, Wallace DD. Documentation of smoking: Role of age, gender and ethnicity. J Assoc Acad Minor Phys. 2001;12:125–8. [PubMed] [Google Scholar]
- 13.Thiru K, Hassey A, Sullivan F. Systematic review of scope and quality of electronic patient record data in primary care. BMJ. 2003;326:1070–3. doi: 10.1136/bmj.326.7398.1070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McDonald T, Blignaut PJ. A. Comparison of a manual and a computer system in a primary health care clinic. Curationis. 1998;21:8–13. [PubMed] [Google Scholar]
- 15.Wager KA, Lee FW, White AW, Ward DM, Ornstein SM., McDonald T, Blignaut PJ. A. Impact of an electronic medical record system on community-based primary care practices. J Am Board Fam Pract. 2000;13:338–48. [PubMed] [Google Scholar]
- 16.Elson RB, Connelly DP. Computerized patient records in primary care: Their role in mediating guideline-driven physician behaviour change. Arch Fam Med. 1995;4:698–705. doi: 10.1001/archfami.4.8.698. [DOI] [PubMed] [Google Scholar]
- 17.Loomis GA, Ries JS, Saywell RM, Jr, Thakker NR. If electronic records are so great, why aren't family physicians using them? Fam Pract. 2002;51:636–41. [PubMed] [Google Scholar]
- 18.Kuusela M, Vainiomäki P, Hinkka S, Rautava P. The quality of GP consultation in two different salary systems. Scand J Prim Health Care. 2004;22:168–73. doi: 10.1080/02813430410006558. [DOI] [PubMed] [Google Scholar]
- 19.Kokko S. Towards fragmentation of general practice and primary healthcare in Finland? Scand J Prim Health Care. 2007;25:131–2. doi: 10.1080/02813430701576482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mäntyselkä P, Halonen P, Vehviläinen A, Takala J, Kumpusalo J. Access to and continuity of primary medical care of different providers as perceived by the Finnish population. Scand J Prim Health Care. 2007;25:27–32. doi: 10.1080/02813430601061106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hippisley-Cox J, Pringle M, Cater R, Wynn A, Hammersley V, Coupland C, et al. The electronic patient record in primary care: Regression or progression? A cross sectional study. BMJ. 2003;326:1439–43. doi: 10.1136/bmj.326.7404.1439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Goudswaard AM, Lam K, Stolk RP, Rutten GE. Quality of recording of data from patients with type 2 diabetes is not a valid indicator of quality of care: A cross-sectional study. Fam Pract. 2003;20:173–7. doi: 10.1093/fampra/20.2.173. [DOI] [PubMed] [Google Scholar]
- 23.Delpierre C, Cuzin L, Fillaux J, Alvarez M, Massip P, Lang T. A systematic review of computer-based patient record systems and quality of care: More randomized clinical trials or a broader approach? Int J Qual Health Care. 2000;16:407–16. doi: 10.1093/intqhc/mzh064. [DOI] [PubMed] [Google Scholar]