Abstract
We examined the association between sleep duration and body mass index in young adults, and, specifically, in possible gender differences. The population-based sample included 955 young men and 1,051 young women (mean age=25.3 years, SD=1.7) who participated in Project EAT-III (Eating and Activity in Teens and Young Adults). In 2008–2009, study participants completed a survey, on which they reported their weight, height, and typical bed and awakening times. Gender-specific regression models estimated cross-sectional associations between sleep duration and weight status, adjusting for age, race, SES, family structure, depressive symptoms, physical activity, and sedentary and dietary behaviors. In multivariable-adjusted linear regression models, an hour increase in sleep was associated with a −0.38 (−0.70, −0.048) BMI in men. Men who slept <7 hours had a 1.4 unit higher mean BMI (27.9; 95% CI: 26.9, 28.9) than men who slept 7–9 hours/day (26.5; 95% CI: 26.1, 27.0). Prevalence estimates of overweight (BMI≥25) and obesity (BMI≥30) were also inversely associated with sleep duration among men. Sleep duration was not associated with BMI, overweight, or obesity in women. Among women, but not men, there was a statistically significant positive association between trouble falling or staying asleep and mean BMI. Sleep may be an important modifiable risk factor for obesity, particularly in young adult men.
Keywords: Adults, gender, obesity, population studies, risk factors
INTRODUCTION
Efforts to decrease obesity in the population have not yielded great success, despite the dedication of substantial resources (1). Continued work is needed to identify modifiable risk factors for obesity. Recently, the possibility that sleep may contribute to obesity has received consideration (2–4). On a population level, sleep duration has declined over time (5), while obesity has increased (6).
Several literature reviews support the possibility that short sleep duration may be a risk factor for increased BMI in both children and adults (2–4). Still, associations between sleep and BMI have not been consistently observed. In part, variability across study findings may reflect differences in statistical adjustment for potential confounders or differences in exposure or outcome definitions, as studies have examined both continuous and categorical forms of sleep duration and BMI variables. Furthermore, questions remain about the specific nature of the epidemiologic association and possible differential associations among population subgroups (7).
One question relates to the shape of the association between sleep duration and BMI. Some studies have found linear inverse associations, in which shorter sleep duration is associated with greater BMI, while others have reported a U-shaped relationship, whereby both short and long sleep duration appear to be associated with higher BMIs. If the relationship is U-shaped, short and long sleep duration may operate through different mechanisms. Acute sleep deprivation has been found to lead to weight-gain-promoting changes in leptin and ghrelin, and to increased hunger (8); another study documented decreased physical activity following sleep loss (9). These study findings are consistent with a role for short sleep duration in weight-related risk behaviors. Mechanisms for an effect of long sleep duration are less clear, but may relate to decreased energy expenditure if time spent sleeping displaces time from physical activity. A survey of time use among Americans documented that sleep time is often sacrificed by time spent working, traveling, or engaging in leisure activities (10). It is also possible that associations are confounded by variables that relate to both sleep duration and BMI, such as socioeconomic status, family situation, dietary and sedentary behaviors, physical activity, and psychosocial status (11).
Another unresolved question is whether sleep duration is differentially associated with BMI across population subgroups, such as gender or age. Some studies that have examined gender-specific associations have found stronger associations among males (12–14). Other studies, however, have shown stronger effects among women or no gender difference (15–17). It has also been hypothesized that the sleep-BMI association may weaken with age. Studies in children have yielded stronger and more consistent estimates of effect than studies in adults (2–4). A prospective study of adults undergoing psychiatric treatment found that sleep duration was negatively associated with BMI when the study sample was 28, but not after the sample had aged to 40 years (18). To our knowledge, no study has examined the association in a representative sample of young adults. This age group merits attention, as the transition to adulthood is associated with important changes in personal circumstances and behaviors that may impact both sleep and BMI, such as changes in physical activity, diet, and social structures (19). In addition, there is evidence that both sleep and BMI are associated with ethnicity and socioeconomic status, but little is known about whether the association between sleep and BMI differs across these demographic measures.
We studied the cross-sectional association between sleep duration and body mass index (BMI) in a large, diverse, population-based sample of young adults. We sought to quantify the association between sleep duration and BMI. We were specifically interested in examining gender-specific associations, given the conflicting results in the literature around possible gender differences. We also explored differences in the association between sleep and BMI by ethnicity and socioeconomic status. Our study was rich in covariate data, allowing us to control for a range of potential confounding variables, and to examine possible mediators such as diet and physical activity. Because published studies have differed with respect to outcome definition, we included analyses of BMI, overweight, and obesity to provide more comparable estimates and to test the consistency of the finding within our dataset.
METHODS AND PROCEDURES
Sample and Study Design
Data for this cross-sectional analysis were drawn from Project EAT (Eating and Activity in Teens and Young Adults)-III, the third wave of a population-based study designed to examine dietary intake, physical activity, and weight-related variables among young adults. At baseline (1998–1999), junior and senior high school students from 31 public schools in the Minneapolis/St. Paul metropolitan area of Minnesota completed surveys and anthropometric measures (20). Ten years later (2008–2009), original participants were mailed letters inviting them to complete online or paper versions of the Project EAT-III survey and a food frequency questionnaire. Questions on sleep duration were first added to the Project EAT-III survey. A total of 955 men and 1,051 women (mean age = 25.3±1.6 years) completed the Project EAT-III survey, representing 66.4% of participants who could be contacted and 48.2% of the original school-based sample. All study protocols were approved by the University of Minnesota’s Institutional Review Board Human Subjects Committee. Participants reviewed a consent form, including acknowledgement of the researchers’ intent to publish the results, as part of the online survey or were mailed a consent form with their paper survey. Completion of the Project EAT-III survey implied written consent.
Survey Development and Measures
The original Project EAT survey (20) was modified at follow-up to improve the relevance of items for young adults. New items were also added to the survey to address areas of growing research interest, such as sleep duration and patterns. The revised survey was pre-tested by 27 young adults in focus groups and test-retest reliability was examined in a sample of 66 young adults. Additional details of the survey development process are described elsewhere (21).
Sleep
Sleep was assessed through the following questions: “On an average weekday (Monday-Friday) a) What time do you go to bed (to go to sleep)? b) What time do you get out of bed (to start your day)?” The same question was asked replacing “weekday” with “weekend day (Saturday-Sunday).” These items were drawn from a validated questionnaire (22), and have been used in published reports of sleep and body weight among adolescents (23). Average weekday and weekend sleep duration were calculated from the times provided. An overall average daily sleep duration was calculated as: (weekday duration*5/7)+(weekend duration*2/7). In addition, we assessed the difference between weekday and weekend sleep duration, defined as weekday duration subtracted from weekend duration, and whether reported sleep patterns varied within the week by comparing weekday and weekend bedtimes. We also examined typical sleep times by creating a 3-level variable to represent bedtimes between 8 p.m. and midnight, midnight and 3 a.m., and 3 a.m. and 8 p.m.
A separate question drawn from a previously developed measure of depressive symptoms (27) queried participants about the frequency with which they had trouble falling or staying asleep in the past 12 months (test-retest r = 0.64). Response categories were “not at all,” “somewhat,” and “very much.” We examined responses to this question as a measure of sleep quality.
Weight status
Weight status was assessed using self-reported height and weight, from which body mass index (BMI, kg/m2) was calculated (test-retest r for both weight and height =0.99). Self-report of height and weight were validated in a subsample of 63 male and 62 female participants in Project EAT-III for whom height and weight measurements were completed by trained research staff. Results showed very high correlations between self-reported BMI and measured BMI in males (r=0.95) and females (r=0.98). Weight status was defined according to current BMI guidelines for adults (overweight or obese: BMI>25 kg/m2; obese: BMI>30 kg/m2).
Covariates
Many variables that are considered obesity risk factors have also been found to be associated with sleep duration (11,24). Thus, we selected potential confounding variables from among several broad areas, including socioeconomic and family status, dietary and physical activity habits, and psychosocial health.
Socioeconomic and family status
Participants indicated the highest level of education they had completed and whether they were enrolled full-time or part-time in a two-year college, four-year college, or graduate degree program (test-retest agreement=97%). Financial stress was assessed with the question: “How difficult is it for you to live on your total household income right now?” Response options were “not at all difficult,” “somewhat difficult,” “very difficult or can barely get by,” and “extremely difficult or impossible” (test-retest r=0.83). In addition, participants indicated if they were single, in a committed dating relationship, or married (test-retest agreement=98%). Parental status (any children/no children) (test-retest r=1.0) was assessed with the question: “How many children do you have (including step-children or adopted children)?”
Dietary and physical activity habits
We included variables measuring the frequency of breakfast (test-retest r=0.82) and fast food (test-retest r=0.48) consumption in the past week, and variables derived from the food frequency questionnaire, including total daily energy intake and the consumption of sugar-sweetened beverages (servings per day) (25). Physical activity was assessed using questions adapted from the widely used Godin Leisure-Time Exercise Questionnaire; participants reported the number of hours they engaged in strenuous and moderate activities during a usual week (test-retest r =0.85) (26). Participants were also separately asked the number of hours on an average weekday and on an average weekend day they watched television/videos, used the computer, and played sedentary video games. Total weekly hours of screen time were calculated as the weighted sum of time spent watching television/videos, using the computer, and playing sedentary video games: (weekday sum*5/7)+(weekend sum*2/7).
Psychosocial health
Participants indicated whether they had ever been diagnosed with depression (test-retest agreement = 100%). To address possible undiagnosed depression, symptoms of depression were assessed using selected items from the Kandel and Davies depression scale (test-retest r = 0.51–0.67) (27). We excluded items from the depression scale that related to sleep quality: 1) trouble falling or staying asleep and 2) feeling tired during the day.
Statistical analysis
Given previously reported associations between both short and long sleep duration with weight status, we considered non-linear approaches to modeling sleep duration in addition to linear analysis of sleep duration. We created categories of average sleep duration of <7 hours, 7–9 hours, and >9 hours of sleep per day based on a priori and empirical considerations. Studies of sleep and health vary in cut-points of sleep duration (3, 4), but our classification is consistent with published studies (4, 14, 18). Also, our category of shortest sleep duration identifies participants not meeting the Healthy People 2020 recommendation that adults aged 22 and older (99% of our sample) rest for at least 7 hours per day (28). In addition, we examined a plot of sleep duration against BMI for inflection points, and conducted sensitivity analysis of different categorical cut-points. We determined the appropriateness of including sleep as a linear variable by examining associations across categories of sleep duration and by testing quadratic sleep duration terms in regression models.
Descriptive statistics for potential confounding or mediating variables are presented as means and standard deviations or percentages according to sleep duration categories (<7, 7–9, >9 hours/day) and by gender. Differences across sleep categories were tested with analysis of variance (ANOVA) for continuous predictors and with χ2 statistics for categorical predictors.
We studied three BMI measures as dependent variables: continuous BMI, overweight (BMI≥25), and obesity (BMI≥30). We used linear regression to examine associations with continuous BMI, and reported adjusted regression coefficients for continuous sleep duration and adjusted mean BMI for each sleep duration category. We used logistic regression to estimate adjusted odds ratios for overweight and obesity with continuous sleep duration and used a generalized linear regression model with binomial distribution and logit link function to estimate the mean adjusted prevalence of overweight and obesity across sleep duration categories. For the categorical sleep analysis, we used moderate sleep duration (7–9 h/day) as the reference; P values are shown for pairwise comparisons between <7 and 7–9 h/day and between >9 and 7–9 h/day.
A minimal multivariable-adjusted model included age (continuous), gender (male, female), and ethnicity (white, black, Hispanic, Asian, other or mixed race). A multivariable-adjusted model additionally controlled for measures of socioeconomic and family status, diagnosed depression and depressive symptoms, and measures of dietary and physical activity behaviors as these factors may act as intermediates in the association between sleep duration and body weight. We examined the sensitivity of adjustment by controlling first for socioeconomic and family status, then adding measures of depression, and finally including potential dietary and physical activity intermediates.
Previous studies indicate possible differential effects by gender, and we were interested a priori in gender-specific results. BMI and overweight/obesity results are shown for the total sample as well as within strata of gender. Still, we formally tested statistical interaction between sleep duration and gender, between sleep and ethnicity, and between sleep and socioeconomic status by including in the regression model main effect terms for sleep and the potential modifier and their cross-product term. Stratum-specific estimates were obtained from subgroup-specific regression models.
All analyses were weighted using the response propensity method (29) to account for differential loss to follow-up. Non-response weights were created using logistic regression to estimate the probability of responding to the Project EAT-III survey based on a large number of questions from the Project EAT-I survey. Weights were calibrated so that analysis sample sizes reflected actual study samples of young men and women (29). All analyses were conducted in SAS 9.2. Statistical significance was based on an alpha of 0.05.
RESULTS
Sample characteristics and bivariate associations
Mean sleep duration was 8.2 hours per day (SD=1.2). Twelve percent of the sample reported sleeping <7 h/day, 67% reported sleeping 7–9 h/day, and 21% reported sleeping >9 h/day. On average, weekend day sleep duration was 30 minutes longer than weekday sleep duration (data not shown). Compared to young men, young women were less likely to report sleeping <7 h/day (14.7% and 9.8%, respectively) and more likely to report sleeping >9 h/day (18.1% and 24.0%, respectively). Sleep duration was associated with having trouble going to sleep or staying asleep. Compared to men and women who reported sleeping at least 7 h/day, a greater percentage of those who slept <7 h reported that they had trouble falling or staying asleep (Table 1) and that they were tired during the day (data not shown).
Table 1.
Selected personal characteristicsa of study sample, according to gender and sleep duration
| Males | Females | |||||||
|---|---|---|---|---|---|---|---|---|
| Sleep duration (hours/day) | Sleep duration (hours/day) | |||||||
| <7 | 7–9 | >9 | p-value | <7 | 7–9 | >9 | p-value | |
| n (%) | 140 (14.7) | 642 (67.2) | 173 (18.1) | 103 (9.8) | 696 (66.2) | 252 (24.0) | ||
| Trouble going to sleep/staying asleep, % very much | 32.1 | 14.9 | 13.5 | <0.001 | 45.7 | 29.0 | 20.0 | <0.001 |
| Age, mean (SD) | 25.5 (1.8) | 25.5 (1.5) | 25.0 (1.8) | <0.0011 | 25.2 (1.6) | 25.4 (1.6) | 25.0 (1.9) | 0.008 |
| Ethnicity (%): | <0.001 | 0.011 | ||||||
| White | 42.8 | 57.5 | 41.8 | 43.2 | 52.6 | 42.2 | ||
| Black | 17.6 | 12.1 | 21.9 | 26.2 | 17.3 | 25.1 | ||
| Hispanic | 7.9 | 6.6 | 4.0 | 2.6 | 6.0 | 3.5 | ||
| Asian | 22.0 | 17.1 | 26.1 | 18.3 | 17.3 | 18.6 | ||
| Mixed/Otherb | 9.7 | 6.7 | 6.1 | 9.8 | 6.9 | 10.7 | ||
| SES and family structure: | ||||||||
| Parent (%) | 28.7 | 26.0 | 20.1 | 0.18 | 44.1 | 30.2 | 36.7 | 0.008 |
| Married/significant partner (%) | 37.1 | 46.3 | 33.3 | 0.007 | 39.4 | 33.2 | 27.3 | 0.021 |
| Not difficult to live on income (%) | 20.4 | 28.9 | 18.8 | 0.008 | 15.8 | 26.8 | 18.7 | 0.013 |
| College graduate (%) | 12.8 | 34.9 | 19.6 | <0.001 | 30.2 | 40.0 | 27.0 | <0.001 |
| Psychosocial and comorbid conditions: | ||||||||
| Depression, ever diagnosed (%) | 18.2 | 12.6 | 13.2 | 0.21 | 39.2 | 23.6 | 34.1 | <0.001 |
| Depressive symptoms scale, mean (SD) | 7.3 (2.3) | 6.8 (2.2) | 6.8 (2.2) | 0.035 | 8.0 (2.2) | 7.8 (2.2) | 7.4 (2.1) | 0.004 |
| Diet and physical activity: | ||||||||
| Breakfast on 5–7 days/ past week (%) | 33.9 | 36.8 | 24.4 | 0.010 | 22.0 | 33.3 | 22.6 | <0.001 |
| No fast food in past week (%) | 23.0 | 24.4 | 15.2 | 0.037 | 35.0 | 39.4 | 29.6 | 0.34 |
| Total energy intake (kcal/day), mean (SD) | 2,430 (1,053) | 2,099 (918) | 2,228 (862) | 0.012 | 1,819 (807) | 2,093 (953) | 1,946 (773) | 0.017 |
| Sugar-sweetened beverage (svg/d), mean (SD) | 1.2 (1.5) | 1.2 (1.8) | 1.0 (1.2) | 0.13 | 0.82 (1.1) | 0.72 (1.1) | 0.63 (1.0) | 0.23 |
| MVPAc (hours/week), mean (SD) | 5.0 (4.9) | 5.1 (4.1) | 4.2 (4.8) | 0.057 | 3.6 (4.0) | 3.6 (3.4) | 3.0 (3.3) | 0.039 |
| Screen time (hours/week), mean (SD)d | 49.0 (31.1) | 52.0 (27.4) | 41.5 (24.8) | <0.001 | 29.9 (18.5) | 34.9 (20.1) | 32.1 (19.6) | 0.053 |
P-value for continuous variables from type III sum of squares.
Mixed/other ethnicity includes study participants who identified as Native American or who identified as more than one listed ethnicity.
MVPA=moderate/vigorous physical activity.
Screen time is the sum of reported time spent watching TV/videos, using the computer, or playing sedentary video games.
Sleep duration was significantly associated with many of the studied covariates (Table 1). For example, participants who slept 7–9 hours/day were more likely to report being college graduates and not having difficulty living on their income, compared to both short and long sleepers. Screen time was positively associated and physical activity was negatively associated with sleep duration in males, and, to a lesser extent, in females.
Many covariates were also associated with BMI, and in the expected direction. For example, compared to white women, black women were more likely to be overweight or obese. In both men and women, overweight and obesity were negatively associated with measures of socioeconomic status, breakfast consumption, and physical activity, and were positively associated with screen time, consumption of sugar-sweetened beverages, and depressive symptoms (data not shown).
Association between sleep duration and continuous BMI
When modeled as a continuous variable, sleep was not significantly associated with BMI in the total sample. Sleep was inversely associated with BMI among men, but not women (p-value, interaction=0.035) (Table 2); an hour increase in sleep was associated with a 0.38 lower BMI in men. There was not strong statistical evidence for interaction by ethnicity (p-value, interaction=0.097); stratum-specific analysis revealed a significantly inverse association between sleep duration and BMI among whites only (beta=−0.41; 95% CI: −0.72, −0.11).
Table 2.
Gender-and ethnic-specific multivariable-adjusteda estimates (95% confidence interval) for BMI (regression beta coefficients), overweight (odds ratios), and obesity (odds ratios) associated with 1 hour increase in sleep
| BMI | Overweight | Obese | |||||||
|---|---|---|---|---|---|---|---|---|---|
| n | Beta (95% CI) | p-value | n overweight | Odds ratio (95% CI) | p-value | n obese | Odds ratio (95% CI) | p-value | |
| Total sample | 2,006 | −0.19 (−0.42, 0.044) | 0.11b | 1,038 | 0.86 (0.78, 0.93) | 0.0005 | 444 | 0.96 (0.87, 1.06) | 0.42 |
| Gender | 0.035c | 0.11 | 0.085 | ||||||
| Male | 955 | −0.38 (−0.70, −0.048) | 0.025 | 545 | 0.79 (0.69, 0.90) | 0.0007 | 197 | 0.84 (0.71, 0.98) | 0.031 |
| Female | 1,051 | −0.11 (−0.44, 0.23) | 0.53 | 483 | 0.93 (0.82, 1.05) | 0.25 | 247 | 1.02 (0.88, 1.19) | 0.76 |
| Ethnicity | 0.097 | 0.58 | 0.078 | ||||||
| White | 1,004 | −0.41 (−0.72, −0.11) | 0.0083 | 477 | 0.82 (0.72, 0.94) | 0.0036 | 193 | 0.88 (0.75, 1.04) | 0.13 |
| Black | 348 | −0.39 (−1.12, 0.33) | 0.29 | 206 | 0.77 (0.61, 0.98) | 0.032 | 99 | 0.86 (0.67, 1.09) | 0.21 |
| Hispanic | 112 | 1.18 (−1.24, 3.59) | 0.33 | 70 | 1.15 (0.29, 4.62) | 0.84 | 30 | 3.44 (1.08, 10.95) | 0.036 |
| Asian | 367 | −0.77 (−0.64, 0.47) | 0.77 | 193 | 0.75 (0.61, 0.94) | 0.011 | 73 | 1.12 (0.86, 1.46) | 0.41 |
| Other | 151 | 0.84 (−0.10, 1.77) | 0.08 | 83 | 1.27 (0.79, 2.02) | 0.32 | 46 | 1.59 (0.95, 2.67) | 0.078 |
Adjusted for age, race, gender, student status, college graduate, parental status, ability to live on income, depressive symptoms, depression diagnosis (ever), breakfast consumption, fast food consumption, total energy intake, consumption of sugar-sweetened beverages, MVPA, screen time. Gender- and ethnic-specific analyses are not adjusted for gender or ethnicity, respectively.
P-values for presented beta coefficient or odds ratio.
P-values for an interaction term between gender and sleep (gender row) or ethnicity and sleep (ethnicity row).
In the total sample, study participants who reported sleeping <7 hours/day had a statistically non-significant higher mean BMI than participants who reported sleeping 7–9 hours/day (Table 3). In gender-specific multivariable-adjusted models, a significant positive association between short sleep duration and mean BMI was observed among males, but not females. The test for interaction was not statistically significant (p=0.31) (Table 3). Mean BMI estimates among those who slept >9 hours/day did not differ from those who slept 7–9 hours/day group in gender-specific or total sample analyses (Table 3).
Table 3.
Gender-and ethnic-specific multivariable-adjusteda mean BMI (95% confidence interval) estimates according to category of sleep duration
| < 7 hr/d | 7–9 hr/d | >9 hr/d | p-value, interaction | |
|---|---|---|---|---|
| Total sample, n | 243 | 1,338 | 425 | |
| Mean BMI (95% CI) | 26.8 (26.0, 27.6) | 26.2 (25.9, 26.6) | 25.9 (25.3, 26.5) | |
| p-valueb | 0.072 | ref | 0.39 | |
| Gender | 0.31 | |||
| Male, n | 140 | 642 | 173 | |
| Mean BMI (95% CI) | 27.9 (26.9, 28.9) | 26.5 (26.1, 27.0) | 26.2 (25.2, 27.1) | |
| p-value | 0.012 | ref | 0.49 | |
| Female, n | 103 | 696 | 252 | |
| Mean BMI (95% CI) | 25.6 (24.4, 26.9) | 26.0 (25.5, 26.5) | 25.6 (24.8, 26.4) | |
| p-value | 0.95 | ref | 0.40 | |
| Ethnicity | 0.005 | |||
| White, n | 102 | 725 | 177 | |
| Mean BMI (95% CI) | 27.1 (26.0, 28.1) | 25.9 (25.5, 26.3) | 25.1 (24.3, 25.8) | |
| p-value | 0.0026 | ref | 0.058 | |
| Black, n | 52 | 196 | 100 | |
| Mean BMI (95% CI) | 28.5 (25.9, 31.0) | 26.8 (25.6, 28.1) | 25.9 (23.9, 27.9) | |
| p-value | 0.13 | ref | 0.46 | |
| Hispanic, n | 13 | 83 | 16 | |
| Mean BMI (95% CI) | 28.3 (21.7, 35.0) | 28.6 (26.2, 31.0) | 32.4 (24.1, 40.7) | |
| p-value | 0.44 | ref | 0.40 | |
| Asian, n | 49 | 227 | 91 | |
| Mean BMI (95% CI) | 25.5 (23.5, 27.5) | 25.8 (24.9, 26.7) | 25.9 (24.5, 27.2) | |
| p-value | 0.79 | ref | 0.93 | |
| Other, n | 23 | 91 | 37 | |
| Mean BMI (95% CI) | 27.4 (24.0, 30.7) | 26.5 (25.1, 27.9) | 31.0 (28.6, 33.3) | |
| p-value | 0.081 | ref | 0.0028 |
Adjusted for age and race, and gender in the total sample analysis, student status, college graduate, parental status, ability to live on income, depressive symptoms, depression diagnosis (ever), breakfast consumption, fast food consumption, total energy intake, consumption of sugar-sweetened beverages, MVPA, screen time.
P-values correspond to separate pair-wise comparisons of <7 hours/day to 7–9 hours/day and of >9 hours/day to 7–9 hours/day.
The multivariable-adjusted association between sleep duration and mean BMI appeared to be moderated by ethnicity (Table 3; p-value for interaction=0.005). Among whites, there was an inverse association between sleep duration and mean BMI, with declines across each sleep duration category (Table 3). A similar, though statistically non-significant, pattern was observed among blacks. Among Hispanics, estimated mean BMIs appeared to increase across categories of sleep duration, although estimates were imprecise, as reflected in the large confidence intervals, and statistically non-significant (Table 3). Among the mixed/other ethnic group, the mean BMI among those who slept >9 hours/day was significantly higher than among those who slept 7–9 hours/day; short sleep duration was positively associated with mean BMI, but was not statistically significantly (Table 3). There was no evidence of an association between sleep duration and mean BMI among Asians.
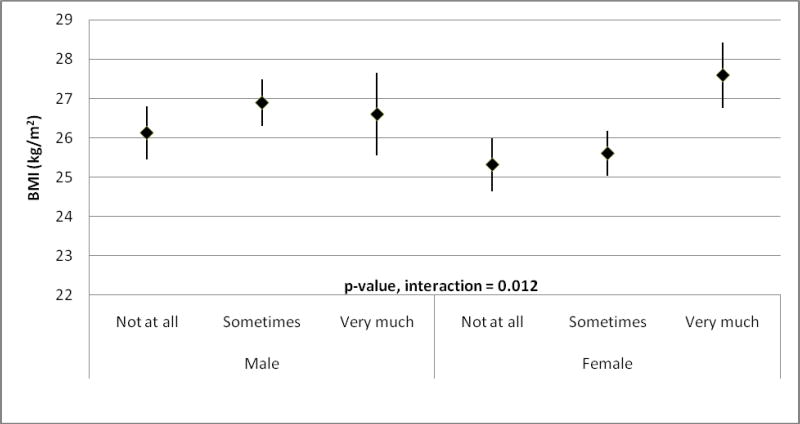
Among women, but not men, trouble falling or staying asleep was positively associated with mean BMI (Figure 1; p-value for interaction=0.012). Women who reported that they had “very much” trouble falling or staying asleep had a multivariable-adjusted mean BMI of 27.6 (95% CI: 26.8, 28.4), as compared to a mean BMI of 25.3 (24.6, 26.0) among women who reported “not at all” having trouble falling or staying asleep. In contrast, in men, the respective mean BMIs were 26.6 (25.6, 27.7) and 26.1 (25.5, 26.8), for “very much” and “not at all” trouble sleeping.
Figure 1.
Gender-specific multivariable-adjusteda mean BMI (and 95% confidence intervals) according to reported trouble falling or staying asleep.
a. Adjusted for age, race, student status, college graduate, married/significant other, parent, ability to live on income, depressive symptoms, depression diagnosis (ever), breakfast, fast food, total energy intake, consumption of sugar-sweetened beverages, moderate-vigorous physical activity, and screen time.
We did not find statistical evidence for interaction by socioeconomic status in the association between sleep duration and mean BMI (data not shown). Differences between weekday and weekend sleep duration or variation in typical bedtimes were not associated with mean BMI (data not shown).
Association between sleep duration and overweight and obesity
In multivariable-adjusted analysis, continuous sleep duration was inversely associated with overweight in the total sample. An hour increase in sleep was associated with a 0.14 reduction in the odds of overweight (odds ratio (OR)=0.86; 95% CI: 0.78, 0.93). Among men, but not women, sleep was inversely associated with the odds of obesity (OR=0.84; 95% CI: 0.71, 0.98).
Categorical sleep duration was inversely associated with overweight and obesity in the total sample, and among men, but not women (Table 4). Among men, as compared to 7–9 hours/day, sleeping <7 hours/day was positively associated, at marginal significance (p-value=0.062), with the prevalence of overweight, and sleeping >9 hours/day was inversely associated with prevalence of overweight (p-value=0.003).
Table 4.
Gender-specific multivariable-adjusteda prevalence(95% CI)estimates for overweight and obesity according to categories of sleep duration
| Overweight | Obesity | |||||||
|---|---|---|---|---|---|---|---|---|
| < 7 hr/d | 7–9 hr/d | >9 hr/d | p-value, interaction | <7 hr/d | 7–9 hr/d | >9 hr/d | p-value, interaction | |
| Overweight | ||||||||
| Total sample, n | 151 | 692 | 196 | 75 | 270 | 100 | ||
| Prevalence (95% CI) | 0.55 (0.47, 0.62) | 0.52 (0.49, 0.55) | 0.43 (0.37, 0.48) | 0.26 (0.20, 0.33) | 0.17 (0.15, 0.20) | 0.18 (0.14, 0.23) | ||
| p-value b | 0.53 | ref | 0.006 | 0.004 | ref | 0.63 | ||
| Gender | 0.30 | 0.047 | ||||||
| Men, n | 97 | 371 | 77 | 51 | 108 | 38 | ||
| Prevalence (95% CI) | 0.69 (0.59, 0.76) | 0.59 (0.54, 0.63) | 0.43 (0.34, 0.52) | 0.35 (0.26, 0.45) | 0.14 (0.11, 0.17) | 0.19 (0.13, 0.27) | ||
| p-value | 0.062 | ref | 0.0033 | <0.001 | ref | 0.17 | ||
| Women, n | 52 | 321 | 119 | 23 | 162 | 62 | ||
| Prevalence (95% CI) | 0.39 (0.28, 0.51) | 0.46 (0.42, 0.51) | 0.41 (0.34, 0.48) | 0.15 (0.09, 0.25) | 0.19 (0.16, 0.23) | 0.17 (0.12, 0.23) | ||
| p-value | 0.27 | ref | 0.21 | 0.41 | ref | 0.52 | ||
Adjusted for age and race, and gender in the total sample analysis, student status, college graduate, parental status, ability to live on income, depressive symptoms, depression diagnosis (ever), breakfastconsumption, fast foodconsumption, total energyintake, consumption of sugar-sweetened beverages, MVPA, screen time.
P-values correspond toseparate pair-wise comparisons of <7 hours/day to 7–9 hours/day and of >9 hours/day to 7–9 hours/day.
In both men and women, data were consistent with a positive association between trouble falling or staying asleep and overweight and obesity, although this association did not always achieve statistical significance (data not shown). There was not statistical evidence of interaction by socioeconomic status or ethnicity in the association between sleep duration and overweight or obesity, although ethnic-specific patterns were similar to those observed for sleep duration and mean BMI (data not shown). Differences between weekday and weekend sleep duration or variation in typical bedtimes were not associated with overweight or obesity (data not shown).
Sensitivity analysis
Results were qualitatively robust to changes in the cut-points of sleep duration categories. Examination of a spline regression plot between sleep duration and BMI did not reveal clear inflection points. In a linear regression model with an 8-level sleep duration variable, representing even-hour cut-points for sleep duration from <6 hours/day through >12 hours/day, we observed positive associations between sleep duration and BMI for the <6 hours/day and the 6–7 hours/day categories, providing empirical support for our lower cut-point. These analyses were limited by small sample sizes, and did not indicate a gain of information at a lower sleep duration cut-point. For example, among the 32 men who reported sleeping <6 hours/day, the mean BMI (95% confidence interval) was 27.9 (26.0, 29.8), as compared to 26.7 (26.3, 27.2) and 26.1 (25.3, 26.9) for men sleeping 6–9 hours/day and >9 hours/day, respectively; these estimates are similar to those reported in Table 3. These results also supported the use of sleep duration as a linear term in regression models. Quadratic sleep duration terms were not statistically significant in regression models, and we modeled sleep duration as a continuous linear term in its original scale so that a unit increase in the regression (beta) coefficient indicates an increase in an hour of sleep.
DISCUSSION
In a multiethnic and socioeconomically diverse sample of young adults, sleeping <7 hours/day, as compared to 7–9 hours/day, was positively associated with BMI, overweight, and obesity among men, but not women. Self-reported trouble falling or staying sleeping, in contrast, was significantly associated with mean BMI among women, but not men. These findings were not explained by adjustment for potential confounding or mediating variables, including socioeconomic or family status, psychosocial health, diet, physical activity, or sedentary behavior. Our results do not corroborate a U-shaped association between sleep duration and BMI, found in some previous studies: results were generally consistent with inverse associations between sleep duration and BMI across categories of sleep duration as well as with the continuous linear sleep variable.
Prior evidence for a gender difference in the association between sleep and BMI is mixed (2–4, 12–17). Our finding of stronger sleep duration-BMI associations among, men is consistent with some (12–14), but not all (15–17), previous studies. We were interested, a priori, in examining gender-specific results. Gender differences were not always strong enough to yield statistical tests for interaction, but all results were consistent with a stronger association among men. We considered the possibility of differential confounding. Men and women had different covariate distributions (Table 1), the association among women appeared to be more affected by confounders. Adjustment for a broad range of potential confounders did not materially change effect estimates among men, while it generally attenuated effect estimates among women (data not shown).
There is evidence for gender differences in biologic aspects of sleep. Compared to women, men appear to have less efficient sleep (more nighttime awakenings) and to spend a lower percentage of sleep time in more restorative stages (30), which in turn has been associated with decreased insulin sensitivity (31). Gender differences may also relate to hormone concentrations. Sex hormone changes during menopause have been associated with both weight gain (32) and decreased sleep quality (33). It is further conceivable that hormone changes may contribute to observed differences in sleep associations across the life course (2–4, 18).
It is also possible that gender differences relate to the form of survey questions. Our finding that self-reported trouble falling or staying asleep was associated with weight among women may demonstrate the importance of considering sleep constructs beyond duration in understanding gender differences, particularly in studies based on self-reports of sleep, or it may indicate that sleep duration among women was better captured by the question about trouble sleeping, if, for example, women spend a longer time in bed, but with lower quality sleep.
We did not expect to observe a significant interaction between ethnicity and sleep duration in the association with mean BMI. Short sleep duration has been associated with increased BMI in Asian and Hispanic samples and in different countries (4, 34), suggesting that the association between sleep duration and BMI may be robust to ethnicity and cultural differences. Our study had small sample sizes for non-white ethnic groups, and results must be interpreted with caution. Studies of statistical interactions are scant, but there are reports of possible ethnic or cultural differences in the effect of sleep on health. For example, in the Insulin Resistance Atherosclerosis Study, a cohort of middle-aged Americans, sleep duration and diabetes incidence were inversely associated in non-Hispanic whites and Hispanics, but not in blacks (35). An analysis of data from the Hispanic Health and Nutrition Examination Survey suggests that there may be intra-ethnic differences, finding a stronger inverse association between sleep duration and body size among Mexican-Americans than among Cuban-Americans or Puerto-Ricans (34).
The current study has several strengths that enhance the utility of the findings. Project EAT-III is a population-based study of multiethnic young adults. The sample is diverse with respect to ethnicity, socioeconomic status, family status, and health-related behaviors, allowing us to test whether the sleep-BMI association may vary across demographic characteristics. To our knowledge, this is the first study of sleep duration and BMI in a representative sample of young adults, and it provides data on a life stage typically characterized by multiple transitions that may impact sleep, as well as health-related behaviors (36). The study’s comprehensive data collection enabled us to adjust for many variables that might confound the association between sleep duration and BMI, and to examine possible mediating effects of diet, physical activity, and sedentary behaviors. Our analysis encompassed approaches previously reported in the literature, including effect estimates of BMI as a continuous measure, as well as prevalence estimates of overweight and obesity.
Our study also has limitations. Sleep was not assessed in previous study waves, and we cannot establish temporal relations between sleep and weight. Longitudinal and intervention studies are needed for stronger evaluation of the association. Published longitudinal findings in other age groups have been mixed (37, 38). Our measure of sleep was based on a single self-report, which has been shown to underestimate sleep duration when compared to data from sleep diaries (39) or polysomnography (40). However, for this to bias the findings, however, sleep duration misclassification would need to be differential by weight status. This is not supported by a study that compared sleep diaries to a single self-report of typical patterns, which found that the magnitude of association between sleep duration and BMI was similar using either sleep duration assessment method (39). Weight and height were also self-reported. A validation sub-study in this sample indicated high agreement between BMI based on measured and self-reported data. BMI is not a direct measure of fat mass or fat distribution; it is not clear whether we would have observed gender differences in other measures, such as waist circumference.
The benefits of sleep are accepted in the public health community, as evidenced by new Healthy People 2020 Objectives related to sleep duration and timing (28). Broader effects of sufficient sleep include improved school performance, increased work productivity, and decreased likelihood for medical errors and traffic accidents (28). However, the public health relevance of sleep as an important risk factor for obesity is not uniformly accepted. For example, Horne has cited small effects and low prevalence of short sleep duration, as reasons to consider sleep a relatively minor risk factor for obesity, as compared to lack of physical activity and poor diet (41). Our findings and those of others do not support this interpretation; associations between sleep duration and BMI appeared to be as strong as effects of physical activity or sedentary behavior (1). In our data, the percentage of overweight and obesity was roughly 15–25% higher among men who slept <7 hours/day than those who slept 7 or more hours per day; nearly 15% of men and 10% of women reported sleeping <7 hours/day.
In summary, we found that short sleep duration was positively associated with BMI, overweight, and obesity in men, but not women. The association was consistent across analytic approaches and independent of potential confounding variables. Our findings support previously-published studies indicating that the effect of short sleep duration on BMI may be stronger among, or restricted to, males (4). Among women, but not men, we observed that trouble falling or staying asleep was associated with increased mean BMI. To our knowledge, this is the first study of sleep and BMI among a population-based sample of young adults. The possibility that the relation between sleep and BMI may differ by ethnicity merits further study in larger samples. Future work into effective ways to intervene on sleep patterns—particularly with younger people is—needed.
Acknowledgments
Sources of Funding: This research was supported by grant R01-HL-084064 from the National Heart, Lung, and Blood Institute, National Institutes of Health, Coronary Artery Risk Development in Young Adults (Project EAT), and by grant T32 HL07779 from the National Heart, Lung, and Blood Institute, National Institutes of Health, Cardiovascular Disease Epidemiology and Prevention. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Heart, Lung, and Blood Institute or the National Institutes of Health.
Footnotes
Conflicts of interest: None.
References
- 1.Must A, Barish EE, Bandini LG. Modifiable risk factors in relation to changes in BMI and fatness: what have we learned from prospective studies of school-aged children? Int J Obes (Lond) 2009;33 (7):705–15. doi: 10.1038/ijo.2009.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chen X, Beydoun MA, Wang Y. Is sleep duration associated with childhood obesity? A systematic review and meta-analysis. Obesity (Silver Spring) 2008;16(2):265–74. doi: 10.1038/oby.2007.63. [DOI] [PubMed] [Google Scholar]
- 3.Cappuccio FP, Taggart FM, Kandala NB, et al. Meta-analysis of short sleep duration and obesity in children and adults. Sleep. 2008;31(5):619–26. doi: 10.1093/sleep/31.5.619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Patel SR, Hu FB. Short sleep duration and weight gain: a systematic review. Obesity (Silver Spring) 2008;16(3):643–53. doi: 10.1038/oby.2007.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Iglowstein I, Jenni OG, Molinari L, Largo RH. Sleep duration from infancy to adolescence: reference values and generational trends. Pediatrics. 2003;111(2):302–7. doi: 10.1542/peds.111.2.302. [DOI] [PubMed] [Google Scholar]
- 6.Mokdad AH, Bowman BA, Ford ES, Vinicor F, Marks JS, Koplan JP. The continuing epidemics of obesity and diabetes in the United States. JAMA. 2001;286(10):1195–200. doi: 10.1001/jama.286.10.1195. [DOI] [PubMed] [Google Scholar]
- 7.Marshall NS, Glozier N, Grunstein RR. Is sleep duration related to obesity? A critical review of the epidemiological evidence. Sleep Med Rev. 2008;12(4):289–98. doi: 10.1016/j.smrv.2008.03.001. [DOI] [PubMed] [Google Scholar]
- 8.Spiegel K, Tasali E, Penev P, Van Cauter E. Brief communication: Sleep curtailment in healthy young men is associated withdecreased leptin levels, elevated ghrelin levels, and increased hunger and appetite. Ann Intern Med. 2004;141(11):846–50. doi: 10.7326/0003-4819-141-11-200412070-00008. [DOI] [PubMed] [Google Scholar]
- 9.Schmid SM, Hallschmid M, Jauch-Chara K, et al. Short-term sleep loss decreases physical activity under free-living conditions but does not increase food intake under time-deprived laboratory conditions in healthy men. Am J Clin Nutr. 2009;90(6):1476–82. doi: 10.3945/ajcn.2009.27984. [DOI] [PubMed] [Google Scholar]
- 10.Basner M, Fomberstein KM, Razavi FM, et al. American time use survey: sleep time and its relationship to waking activities. Sleep. 2007;30(9):1085–95. doi: 10.1093/sleep/30.9.1085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stranges S, Dorn JM, Shipley MJ, et al. Correlates of short and long sleep duration: a cross-cultural comparison between the United Kingdom and the United States: the Whitehall II Study and the Western New York Health Study. Am J Epidemiol. 2008;168(12):1353–64. doi: 10.1093/aje/kwn337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Knutson KL. Sex differences in the association between sleep and body mass index in adolescents. J Pediatr. 2005;147(6):830–4. doi: 10.1016/j.jpeds.2005.07.019. [DOI] [PubMed] [Google Scholar]
- 13.Ko GT, Chan JC, Chan AW, et al. Association between sleeping hours, working hours and obesity in Hong Kong Chinese: the ‘better health for better Hong Kong’ health promotion campaign. Int J Obes (Lond) 2007;31(2):254–60. doi: 10.1038/sj.ijo.0803389. [DOI] [PubMed] [Google Scholar]
- 14.Gangwisch JE, Malaspina D, Boden-Albala B, Heymsfield SB. Inadequate sleep as a risk factor for obesity: analyses of the NHANES I. Sleep. 2005;28(10):1289–96. doi: 10.1093/sleep/28.10.1289. [DOI] [PubMed] [Google Scholar]
- 15.Cournot M, Ruidavets JB, Marquie JC, Esquirol Y, Baracat B, Ferrieres J. Environmental factors associated with body mass index in a population of Southern France. Eur J Cardiovasc Prev Rehabil. 2004;11(4):291–7. doi: 10.1097/01.hjr.0000129738.22970.62. [DOI] [PubMed] [Google Scholar]
- 16.Chaput JP, Despres JP, Bouchard C, Tremblay A. Short sleep duration is associated with reduced leptin levels and increased adiposity: Results from the Quebec family study. Obesity (Silver Spring) 2007;15(1):253–61. doi: 10.1038/oby.2007.512. [DOI] [PubMed] [Google Scholar]
- 17.St-Onge MP, Perumean-Chaney S, Desmond R, et al. Gender Differences in the Association between Sleep Duration and Body Composition: The Cardia Study. Int J Endocrinol. 2010;2010:726071. doi: 10.1155/2010/726071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hasler G, Buysse DJ, Klaghofer R, et al. The association between short sleep duration and obesity in young adults: a 13-year prospective study. Sleep. 2004;27(4):661–6. doi: 10.1093/sleep/27.4.661. [DOI] [PubMed] [Google Scholar]
- 19.Nelson MC, Story M, Larson NI, Neumark-Sztainer D, Lytle LA. Emerging adulthood and college-aged youth: an overlooked age for weight-related behavior change. Obesity (Silver Spring) 2008;16 (10):2205–11. doi: 10.1038/oby.2008.365. [DOI] [PubMed] [Google Scholar]
- 20.Neumark-Sztainer D, Croll J, Story M, Hannan PJ, French SA, Perry C. Ethnic/racial differences in weight-related concerns and behaviors among adolescent girls and boys: findings from Project EAT. J Psychosom Res. 2002;53(5):963–74. doi: 10.1016/s0022-3999(02)00486-5. [DOI] [PubMed] [Google Scholar]
- 21.Larson N, Neumark-Sztainer D, Story M, van den Berg P, Hannan PJ. Identifying correlates of young adults’ weight behavior: survey development. American Journal of Health Behavior. In press. [PMC free article] [PubMed] [Google Scholar]
- 22.Pasch KE, Laska MN, Lytle LA, Moe SG. Adolescent sleep, risk behaviors, and depressive symptoms: are they linked? Am J Health Behav. 2010;34(2):237–48. doi: 10.5993/ajhb.34.2.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lytle LA, Pasch KE, Farbaksh K. The relationship between sleep and weight in a sample of adolescents. Obesity(Silver Spring) 2011;19(2):324–31. doi: 10.1038/oby.2010.242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Patel SR, Malhotra A, Gottlieb DJ, White DP, Hu FB. Correlates of long sleep duration. Sleep. 2006;29(7):881–9. doi: 10.1093/sleep/29.7.881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Feskanich D, Rimm EB, Giovannucci EL, et al. Reproducibility and validity of food intake measurements from a semiquantitative food frequency questionnaire. J Am Diet Assoc. 1993;93 (7):790–6. doi: 10.1016/0002-8223(93)91754-e. [DOI] [PubMed] [Google Scholar]
- 26.Godin G, Shephard RJ. A simple method to assess exercise behavior in the community. Can J Appl Sport Sci. 1985;10(3):141–6. [PubMed] [Google Scholar]
- 27.Kandel DB, Davies M. Epidemiology of depressive mood in adolescents: an empirical study. Arch Gen Psychiatry. 1982;39(10):1205–12. doi: 10.1001/archpsyc.1982.04290100065011. [DOI] [PubMed] [Google Scholar]
- 28.Healthy People. 2020 Topics and Objectives: Sleep Health. Washington D.C: U.S. Department of Health and Human Services; 2020. [Google Scholar]
- 29.Little R. Survey nonresponse adjustments for estimates of means. Int Stat Rev. 1986;54:139–157. [Google Scholar]
- 30.Roehrs T, Kapke A, Roth T, Breslau N. Sex differences in the polysomnographic sleep of young adults: a community-based study. Sleep Med. 2006;7(1):49–53. doi: 10.1016/j.sleep.2005.05.008. [DOI] [PubMed] [Google Scholar]
- 31.Tasali E, Leproult R, Ehrmann DA, Van Cauter E. Slow-wave sleep and the risk of type 2 diabetes in humans. Proc Natl Acad Sci U S A. 2008;105(3):1044–9. doi: 10.1073/pnas.0706446105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lovejoy JC. The influence of sex hormones on obesity across the female life span. J Women’s Health. 1998;10(7):1247–1256. doi: 10.1089/jwh.1998.7.1247. [DOI] [PubMed] [Google Scholar]
- 33.Sowers MF, Zheng H, Kravitz HM, Matthews K, Bromberger JT, Gold EB, et al. Sex steroid hormone profiles are related to sleep measures from polysomnography and the Pittsburgh Sleep Quality Index. Sleep. 2008;31(10):1339–49. [PMC free article] [PubMed] [Google Scholar]
- 34.Knutson KL. Association between sleep duration and body size differs among three Hispanic groups. Am J Human Biol. 2011;23:138–41. doi: 10.1002/ajhb.21108. [DOI] [PubMed] [Google Scholar]
- 35.Beihl DA, Liese AD, Haffner SM. Sleep duration as a risk factor for incident type 2 diabetesin a multiethnic cohort. Ann Epidemiol. 2009;19:351–57. doi: 10.1016/j.annepidem.2008.12.001. [DOI] [PubMed] [Google Scholar]
- 36.Arnett J. Emerging adulthood: a theory of development from the late teens through the twenties. Am Psychol. 2000;55:469–480. [PubMed] [Google Scholar]
- 37.Lauderdale DS, Knutson KL, Rathouz PJ, Yan LL, Hulley SB, Liu K. Cross-sectional and longitudinal associations between objectively measured sleep duration and body mass index: the CARDIA Sleep Study. Am J Epidemiol. 2009;170(7):805–13. doi: 10.1093/aje/kwp230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chaput JP, Despres JP, Bouchard C, Tremblay A. The association between sleep duration and weight gain in adults: a 6-year prospective study from the Quebec Family Study. Sleep. 2008;31(4):517–23. doi: 10.1093/sleep/31.4.517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Knutson KL, Lauderdale DS. Sleep duration and overweight in adolescents: self-reported sleep hours versus time diaries. Pediatrics. 2007;119(5):e1056–62. doi: 10.1542/peds.2006-2597. [DOI] [PubMed] [Google Scholar]
- 40.Walsleben JA, Kapur VK, Newman AB, et al. Sleep and reported daytime sleepiness in normal subjects: the Sleep Heart Health Study. Sleep. 2004;27(2):293–8. doi: 10.1093/sleep/27.2.293. [DOI] [PubMed] [Google Scholar]
- 41.Horne J. Short sleep is a questionable risk factor for obesity and related disorders: statistical versus clinical significance. Biol Psychol. 2008;77(3):266–76. doi: 10.1016/j.biopsycho.2007.12.003. [DOI] [PubMed] [Google Scholar]