Abstract
Purpose
We describe current trends in robotic and open radical prostatectomy in the United States after examining case logs for American Board of Urology certification.
Materials and Methods
American urologists submit case logs for initial board certification and recertification. We analyzed logs from 2004 to 2010 for trends and used logistic regression to assess the impact of urologist age on robotic radical prostatectomy use.
Results
A total of 4,709 urologists submitted case logs for certification between 2004 and 2010. Of these logs 3,374 included 1 or more radical prostatectomy cases. Of the urologists 2,413 (72%) reported performing open radical prostatectomy only while 961 (28%) reported 1 or more robotic radical prostatectomies and 308 (9%) reported robotic radical prostatectomy only. During this 7-year period we observed a large increase in the number of urologists who performed robotic radical prostatectomy and a smaller corresponding decrease in those who performed open radical prostatectomy. Only 8% of patients were treated with robotic radical prostatectomy by urologists who were certified in 2004 while 67% underwent that procedure in 2010. Median age of urologists who exclusively performed open radical prostatectomy was 43 years (IQR 38–51) vs 41 (IQR 35–46) for those who performed only robotic radical prostatectomy.
Conclusions
While the rate was not as high as the greater than 85% industry estimate, 67% of radical prostatectomies were done robotically among urologists who underwent board certification or recertification in 2010. Total radical prostatectomy volume almost doubled during the study period. These data provide nonindustry based estimates of current radical prostatectomy practice patterns and further our understanding of the evolving surgical treatment of prostate cancer.
Keywords: prostate, prostatic neoplasms, prostatectomy, robotics, physician’s practice patterns
Approximately a third of the more than 200,000 men diagnosed with PC in the United States annually undergo RP.1,2 For years open RP was the standard surgical management of PC but in the last 5 years robotic RP has become the most common surgical approach to this disease. Data comparing RP techniques are limited but large population based studies show minimal differences in the outcome of robotic vs open RP.3,4
The exact proportion of RPs done using the open or robotic technique is not known. The most commonly reported estimates stem from SEER (Surveillance, Epidemiology and End Results)-Medicare data and are not current.3,4 In the SEER-Medicare cohort the minimally invasive RP rate increased from 9% in 2003 to 42% in 2006.3 In 2009 The New York Times® reported that 86% of patients in the United States who underwent PC surgery were treated with a robotic procedure.5 These numbers were based on industry estimates from the only manufacturer of the surgical robot and to our knowledge they were not independently verified. Furthermore, despite growing concerns about overtreatment of low risk PC the number of RPs appears to be increasing. Data from the Nationwide Inpatient Sample indicate that RP hospital discharges increased by 60% from 2005 through 2008.6
Little is known about how the diffusion of robotics has influenced urological individual practice patterns. We questioned whether the uptake of robotics has resulted in a larger or smaller proportion of urologists performing RP in the United States and whether surgeon age was associated with the likelihood that a urologist would perform robotic RP. Using ABU data we describe robotic and open RP current practice patterns, focusing on the annual number of RPs and the proportion of urologists performing RP in the United States. We also examined the impact of surgeon age on the likelihood of performing robotic RP. We hypothesized that due to robotic adoption the annual RP volume was increasing but the proportion of urologists performing RP was decreasing. We also hypothesized that older urologists would be less likely to report experience with robotic RP.
MATERIALS AND METHODS
Data
We used self-reported operative logs from the ABU, the agency responsible for urology board certification in the United States. The ABU evaluates candidates who are licensed to practice medicine and performs examinations for urological certification, recertification and ongoing maintenance of certification. Candidates for board certification or recertification must submit an operative case log for 6 consecutive months from the 17-month period before the case log due date. A notarized practice log verification statement must be submitted with the final case log. The first and second board recertifications occur 10 and 20 years, respectively, after the original certification and also rely on 6-month practice logs. Urologists who were certified before 1985 are not required submit case logs for recertification. For this study the ABU provided de-identified case log data on RP that were used in accordance with ABU regulations.
Cohort
We identified all urologists who applied for original ABU certification, or the first or second board recertification from 2004 through 2010. The procedures recorded in the individual 2004 to 2010 case logs were done from 2003 through 2009. Surgical procedures were identified by Healthcare Common Procedural Coding System codes in physician case logs (55866 for laparoscopic RP, and 55801, 55810, 55812, 55815, 55821, 55831, 55840, 55842 and 55845 for open RP). The robotic RP group includes traditional laparoscopic RP cases.
Statistical Methods
We used summary statistics to describe current RP practice patterns after stratifying urologists into 3 groups by the types of RP that they performed, including 1) open only, 2) robotic only or 3) open and robotic procedures. Since urologists submitting case logs for the initial certification were on average younger (mean age 36 years) than those seeking a first and second recertification (mean ages 44 and 53 years, respectively), we analyzed each certification type separately. Since urologists could have exclusively robotic, exclusively open or a combination of robotic and open experience, we used 2 outcomes, including 1) any robotic RP experience and 2) exclusively robotic RP experience. We created 2 logistic regression models for each outcome. To determine the association with age we plotted the predicted probability of each outcome as a function of age. All statistical analysis was done using STATA® 11.0.
RESULTS
A total of 4,709 nonpediatric urologists submitted case logs to the ABU for certification or recertification between 2004 and 2010, of whom 3,374 (72%) included at least 1 RP case. Of surgeons performing RPs 961 (28%) reported doing at least 1 robotic RP, including 308 who performed exclusively robotic and 653 who performed open and robotic RP. In contrast, 2,413 surgeons performed exclusively open RP (table 1). Median age was 43 years (IQR 38–51) for surgeons who performed only open RP, which was 2 years greater than the age of surgeons who performed robotic only and open plus robotic RP (41 years, IQR 35–46 and 41, IQR 36–45, respectively). Robotic RP surgeons and those who performed a combination of open and robotic RP had substantially higher annual case volume than surgeons who performed only open RP (median 20, IQR 8–49 and 28, IQR 16–50, respectively, vs 8, IQR 4–16).
Table 1.
Characteristics of 3,374 certifying and recertifying urologists who performed RP
| No. Open (%) | No. Robotic (%) | No. Open + Robotic (%) | |
|---|---|---|---|
| Male | 2,261 (94) | 291 (94) | 625 (96) |
| Yr: | |||
| 2004 | 396 (16) | 13 (4) | 18 (3) |
| 2005 | 370 (15) | 11 (4) | 40 (6) |
| 2006 | 443 (18) | 19 (6) | 69 (11) |
| 2007 | 390 (16) | 37 (12) | 93 (14) |
| 2008 | 292 (12) | 50 (16) | 117 (18) |
| 2009 | 270 (11) | 83 (27) | 163 (25) |
| 2010 | 252 (10) | 95 (31) | 153 (23) |
| Specialty: | |||
| Andrology | 20 (1) | 1 (less than 0.5) | 3 (less than 0.5) |
| Endourology | 75 (3) | 42 (14) | 45 (7) |
| Female | 44 (2) | 6 (2) | 5 (1) |
| General | 2,088 (87) | 226 (73) | 487 (75) |
| Oncology | 132 (5) | 31 (10) | 106 (16) |
| Pediatrics | 17 (1) | 2 (1) | 2 (less than 0.5) |
| Urolithiasis | 37 (2) | 0 | 5 (1) |
| Certification type: | |||
| Original | 762 (32) | 153 (50) | 320 (49) |
| 1st Recertification | 899 (37) | 99 (32) | 216 (33) |
| 2nd Recertification | 752 (31) | 56 (18) | 117 (18) |
Table 2 shows that the number of certifying or recertifying urologists who performed RP increased with time from 427 in 2004 to 500 in 2010. However, this increase appeared to mirror the general increase in the total number of urologists certified since the proportion that performed RP remained relatively consistent across the years. We noted a large increase in the number and proportion of urologists who performed robotic RP and a smaller corresponding decrease in the number and proportion doing open RP. Median annual RP volume increased during the study period. For urologists who performed at least 1 robotic RP the median annual volume peaked in 2008 at 34 cases (IQR 18–58) while it was 26 (IQR 14–47) in 2010.
Table 2.
Certifying and recertifying urologists by procedure and certification year
| Total No. Urologists* |
At Least 1 RP Open or Robotic RP |
At Least 1 Open RP |
At Least 1 Robotic RP |
||||
|---|---|---|---|---|---|---|---|
| No. Urologists (%) | Median Vol (IQR) | No. Urologists (%) | Median Vol (IQR) | No. Urologists (%) | Median Vol (IQR) | ||
| 2004 | 607 | 427 (70) | 10 (4–16) | 414 (68) | 10 (4–16) | 31 (5) | 20 (8–36) |
| 2005 | 603 | 421 (70) | 10 (4–18) | 410 (68) | 10 (4–18) | 51 (8) | 20 (12–44) |
| 2006 | 685 | 531 (78) | 12 (6–22) | 512 (75) | 12 (6–20) | 88 (13) | 21 (14–51) |
| 2007 | 721 | 520 (72) | 12 (6–23) | 483 (67) | 12 (6–22) | 130 (18) | 28 (14–50) |
| 2008 | 680 | 459 (68) | 14 (6–32) | 409 (60) | 12 (6–28) | 167 (25) | 34 (18–58) |
| 2009 | 687 | 516 (75) | 14 (6–28) | 433 (63) | 12 (6–26) | 246 (36) | 26 (14–46) |
| 2010 | 726 | 500 (69) | 14 (6–28) | 405 (56) | 12 (4–26) | 248 (34) | 26 (14–47) |
|
|
|
|
|
||||
| Totals | 4,709 | 3,374 (72) | 3,066 (65) | 961 (20) | |||
Includes certifying and recertifying urologists who did not perform RP, excluding those certifying for pediatric urology, and urologists may be counted in multiple categories if they performed open and robotic RP.
We identified a large increase in the total number of RPs done during the study period. A total of 6,188 RPs were logged for the 427 urologists who were certified or recertified in 2004 while for the 500 who certified or recertified in 2010 the total number of RPs logged increased to 11,290 (table 3 and fig. 1).
Table 3.
Patients treated with open or robotic RP by certification and recertification year
| Any RP (No. urologists) |
Total No. RPs |
No. Open RPs (%) |
No. Robotic RPs (%) |
|
|---|---|---|---|---|
| 2004 | 427 | 6,188 | 5,690 (92) | 498 (8) |
| 2005 | 421 | 6,692 | 5,512 (82) | 1,180 (18) |
| 2006 | 531 | 9,494 | 7,032 (74) | 2,462 (26) |
| 2007 | 520 | 10,110 | 6,092 (60) | 4,018 (40) |
| 2008 | 459 | 11,000 | 5,344 (49) | 5,656 (51) |
| 2009 | 516 | 12,404 | 4,500 (36) | 7,904 (64) |
| 2010 | 500 | 11,29 | 3,770 (33) | 7,520 (67) |
|
|
|
|
|
|
| Totals | 3,374 | 67,178 | 37,940 | 29,238 |
Figure 1.

Trends in robotic (green curve) and open (red curve) RP. Blue curve indicates total.
Figure 2 shows the proportion of urologists who performed at least 1 robotic RP, by certification type and year. For each certification type we noted a large increase during the years in the proportion of physicians who performed at least 1 robotic RP. For example, of those presenting for the initial certification the proportion that reported at least 1 robotic case in 2004 was 11% while in 2010 it was 64%. Of those presenting for first and second recertifications we observed a similar increase with time, although the overall robotic use rate was lower, including 6% in 2004 and 48% in 2010, and 3% in 2004 and 35% in 2010, respectively.
Figure 2.

Proportion of physicians who performed at least 1 robotic RP by certification year and type.
Figure 3 shows the predicted probability of performing at least 1 robotic RP as a function of urologist age according to certification type. The interaction term between age and certification type was not statistically significant (p = 0.7) but the effect of age appeared stronger among recertifying urologists than among those receiving the initial certification. Table 4 shows the association between age and performing any or all robotic cases by certification type. For urologists receiving the initial board certification we found no evidence that age was significantly associated with the probability of performing at least 1 robotic procedure (OR 0.98, p = 0.3). After adjusting for recertification year physician age was significantly inversely associated with performing at least 1 robotic procedure among those receiving the first or second recertification (annual OR 0.94, p = 0.013 and OR 0.92, p = 0.018, respectively).
Figure 3.
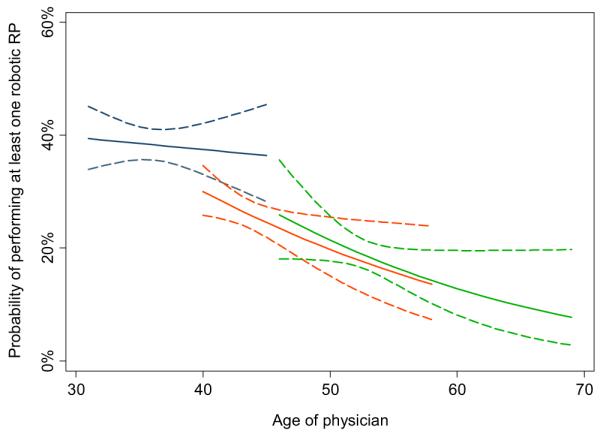
Estimated predicted probability of performing at least 1 robotic RP as function of physician age by original certification (blue curve), and first (orange curve) and second (green curve) recertifications.
Table 4.
Urologist age and certification year by any robotic RP or exclusively robotic RP according to certification type
| Any Robotic RP |
Only Robotic RP |
|||
|---|---|---|---|---|
| OR (95% CI) | p Value | OR (95% CI) | p Value | |
| Original certification: | ||||
| Age/yr | 0.98 (0.94–1.02) | 0.3 | 0.96 (0.90–1.02) | 0.2 |
| Currrent yr | 1.61 (1.50–1.73) | <0.005 | 1.44 (1.30–1.60) | <0.005 |
| 1st Recertification: | ||||
| Age/yr | 0.94 (0.89–0.99) | 0.013 | 1.00 (0.93–1.07) | >0.9 |
| Currrent yr | 1.51 (1.40–1.63) | <0.005 | 1.63 (1.43–1.86) | <0.005 |
| 2nd Recertification: | ||||
| Age/yr | 0.92 (0.85–0.99) | 0.018 | 0.93 (0.83–1.04) | 0.2 |
| Currrent yr | 1.59 (1.44–1.75) | <0.005 | 1.53 (1.30–1.80) | <0.005 |
Figure 4 shows the proportion of urologists who performed robotic RP exclusively by certification type and year. Again, we noted a large increase withtime in each certification type. The proportion of urologists who treated cases only robotically increased from 5% in 2004 to 24% in 2010 among those receiving the initial board certification. Similarly the proportion increased from 1% in 2004 to 20% in 2010 among those receiving the first recertification and from 2% to 12% among those receiving the second recertification. We found no evidence that age was significantly associated with exclusively robotic RP (each p ≥0.2, table 4 and fig. 5).
Figure 4.
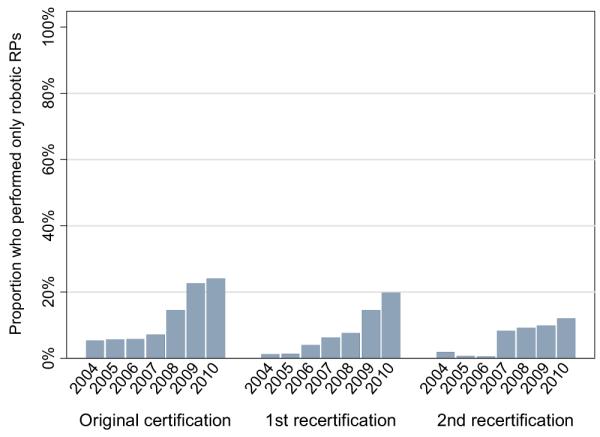
Proportion of physicians who performed exclusively robotic RPs for certification by certification year and type.
Figure 5.
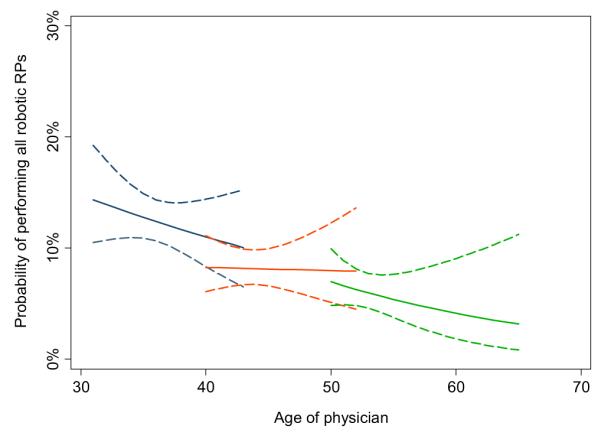
Estimated probability of performing exclusively robotic RP as function of physician age by original certification (blue curve), and first (orange curve) and second (green curve) recertifications.
DISCUSSION
Among our study findings 4 salient observations merit further consideration. 1) Approximately 67% of RPs were done robotically in 2009 based on contemporary ABU certification data. This estimate is substantially less than industry based estimates, which are commonly quoted in the lay press and medical literature.5 2) These data suggest that there has been a considerable increase in the total number of RPs done annually in the United States while the proportion of urologists performing the procedure has remained relatively constant. The increase in RP volume occurred despite growing awareness of PC over diagnosis and overtreatment. 3) Urologists who performed robotic RP had a higher case volume than those who only performed open RP. The median annual case volume for urologists who did at least 1 robotic RP was 26 vs 8 for those who did only open RP. 4) As we hypothesized, age appeared to influence whether recertifying urologists performed robotic RP with older urologists less likely to use robotics.
RP Rate
Since the initial robotic RPs were done in the United States and Germany in 2000,7,8 there has been a substantial shift in surgical management of PC. Specifically in the last 5 years robotic RP has surpassed open RP as the most common surgical treatment for PC despite the lack of prospective evidence showing its oncological advantages or cost-effectiveness compared with open RP. Industry based estimates claim that 86% of RPs were done robotically in 2009.5 To our knowledge these data have not been independently verified and there are no contemporary data that accurately estimate current RP practice patterns.
In contrast to industry based estimates, we found that in 2010 case logs, reflecting 2009 practice patterns, 67% of RPs were done robotically while 33% were done in open fashion and this proportion appears to have attained a plateau (fig. 1). Unbiased estimates of open and robotic RP rates are important since they provide insight into evolving patient and physician preferences about PC treatment and allow researchers to better gauge the impact of robotic surgical technology on PC care in the United States.
RP Volume
Annual total
A second study finding is the substantial increase in the total volume of RPs in a 7-year period. In 2004, 427 (re)certifying urologists reported performing a total of 6,188 RPs in 2003 while in 2010, 500 reported performing a total of 11,290 RPs in 2009. These findings are consistent with those of other studies using a different data source. For example, information from the Nationwide Inpatient Sample revealed that RP hospital discharges increased 60% between 2005 and 2008.6 Together these data are striking, especially considering that the overall incidence of PC has recently decreased. According to National Cancer Institute data the annual percent change in the PC incidence from 2000 through 2007 showed a 2.0% decrease.9
Individual Surgeons
Well established medical literature suggests a strong association between surgical volume and clinical outcome for various complex surgical procedures, including open and robotic RP. Higher volume open RP surgeons tend to achieve fewer complications and better functional outcomes than their lower volume counterparts.10 Likewise, patients treated with minimally invasive RP by higher volume surgeons had a significantly better outcome and decreased hospital stay after surgery.4
We found that urologists who performed robotic RP had a substantially higher annual volume than those who performed only open RP. Based on these findings and those of others11,12 it appears that the uptake of robotics has contributed to the centralization of RP in the hands of higher volume surgeons. With time this may bode well for patients who require prostatectomy, the clinical outcome and the cost-effectiveness of robotic RP. From 2003 through 2005 a SEER-Medicare study found that in more than half of the men treated with minimally invasive RP the procedure was done by a urologist whose yearly Medicare volume was less than 5 RPs.4 If more patients are treated with RP by relatively higher volume surgeons, average outcomes should improve.
Impact of Surgeon Age on Robotic RP
Age impacted whether a recertifying urologist performed robotic RP. For each increasing year in age urologists had an average 6% to 8% lower odds of taking up the procedure depending on whether it was the first or second recertification. Age did not appear to impact whether an initially certifying urologist performed robotic RP. Intuitively these findings make sense since urologists applying for the initial ABUboard certification are within 5 years of training and more likely to have had robotic or traditional laparoscopic RP experience during residency or fellowship. Thus, their training experience would be likely to foster robotic RP uptake after they enter practice.
As with all studies, ours has some limitations. ABU initial certification and recertification are based on self-reported operative logs from 6 consecutive months in the year before certification. The ABU then doubles each log to provide an annual volume estimate. Based on this methodology there is no reason to suspect systematic case load overestimation or underestimation. We could not verify case logs but the ABU reserves the right to audit any questionable logs.
This study provides a cross-sectional view of RP practice patterns in the United States. We analyzed more than 67,000 procedures during a 7-year period. However, approximately 90,000 RPs are done annually in the United States. Our study provides estimates of RP use calculated from certifying urologists, who only represent a percent of all American urologists.
Also, we used Healthcare Common Procedural Coding System codes to identify RP. Since robotic RP data also include traditional laparoscopic RP, we could not distinguish between the 2 procedures. By including the 2 types in the robotic group we may have overestimated robotic RP use.
Inaccurate RP coding may have biased our results. In addition, urologists who received the ABU board certification before 1985 are not required to recertify. Thus, we focused on a relatively younger group of urologists. As such, our estimate that 67% of RPs were done robotically in 2009 may be an overestimate.
CONCLUSIONS
In contrast to industry estimates of greater than 85%, among urologists undergoing board certification or recertification in 2010 only 67% of RPs were done robotically. We also found a substantial increase in the number of RPs done during the study period. Older urologist age was significantly associated with a lower likelihood of performing robotic RP among those recertifying. These data provide nonindustry based estimates of current RP practice patterns and further our understanding of how technological advances impact PC surgical treatment.
Acknowledgments
Supported by The Sidney Kimmel Center for Prostate and Urologic Cancers, Memorial Sloan-Kettering Cancer Center, National Institutes of Health Grant 1RC1CA146516-01 (WTL and JAE), National Institutes of Health Grant T32-CA82088 (WTL) and funds provided by David H. Koch through the Prostate Cancer Foundation.
Abbreviations and Acronyms
- ABU
American Board of Urology
- PC
prostate cancer
- RP
radical prostatectomy
REFERENCES
- 1.Jemal A, Siegel R, Xu J, et al. Cancer statistics, 2010. CA Cancer J Clin. 2010;60:277. doi: 10.3322/caac.20073. [DOI] [PubMed] [Google Scholar]
- 2.Underwood W, 3rd, Jackson J, Wei JT, et al. Racial treatment trends in localized/regional prostate carcinoma: 1992-1999. Cancer. 2005;103:538. doi: 10.1002/cncr.20796. [DOI] [PubMed] [Google Scholar]
- 3.Hu JC, Gu X, Lipsitz SR, et al. Comparative effectiveness of minimally invasive vs open radical prostatectomy. JAMA. 2009;302:1557. doi: 10.1001/jama.2009.1451. [DOI] [PubMed] [Google Scholar]
- 4.Lowrance WT, Elkin EB, Jacks LM, et al. Comparative effectiveness of prostate cancer surgical treatments: a population based analysis of post-operative outcomes. J Urol. 2010;183:1366. doi: 10.1016/j.juro.2009.12.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kolata G. Results Unproven, Robot Surgery Wins Converts. New York Times. 2010 Feb 14;:A1. [Google Scholar]
- 6.Barbash GI, Glied SA. New technology and health care costs—the case of robot-assisted surgery. N Engl J Med. 2010;363:701. doi: 10.1056/NEJMp1006602. [DOI] [PubMed] [Google Scholar]
- 7.Binder J, Kramer W. Robotically-assisted laparoscopic radical prostatectomy. BJU Int. 2001;87:408. doi: 10.1046/j.1464-410x.2001.00115.x. [DOI] [PubMed] [Google Scholar]
- 8.Menon M, Shrivastava A, Tewari A, et al. Laparoscopic and robot assisted radical prostatectomy: establishment of a structured program and preliminary analysis of outcomes. J Urol. 2002;168:945. doi: 10.1016/S0022-5347(05)64548-X. [DOI] [PubMed] [Google Scholar]
- 9.Altekruse SF, Krapcho M, Neyman N, et al. SEER Cancer Statistics Review, 1975–2007. National Cancer Institute; Bethesda: 2009. [Google Scholar]
- 10.Begg CB, Riedel ER, Bach PB, et al. Variations in morbidity after radical prostatectomy. N Engl J Med. 2002;346:1138. doi: 10.1056/NEJMsa011788. [DOI] [PubMed] [Google Scholar]
- 11.Makarov DV, Yu JB, Desai RA, et al. The association between diffusion of the surgical robot and radical prostatectomy rates. Med Care. 2011;49:333. doi: 10.1097/MLR.0b013e318202adb9. [DOI] [PubMed] [Google Scholar]
- 12.Stitzenberg KB, Wong YN, Nielsen ME, et al. Trends in radical prostatectomy: centralization, robotics, and access to urologic cancer care. Cancer. 2011;118:54. doi: 10.1002/cncr.26274. [DOI] [PMC free article] [PubMed] [Google Scholar]


