Abstract
Study Objectives:
To examine the impact of mode of anesthesia on perceived quality of sleep and to analyze the perceived quality of sleep in affecting recovery from surgery.
Methods:
A randomized, controlled, open multicenter trial was conducted in 5 hospitals in Southeast Sweden. One-hundred eighty women scheduled for fast-track abdominal hysterectomy for benign conditions were randomized to spinal anesthesia or general anesthesia; 162 women completed the trial; 82 allocated to spinal anesthesia and 80 to general anesthesia. Symptoms and perceived quality of sleep after surgery were registered daily in the Swedish Postoperative Symptoms Questionnaire.
Results:
Women in the general anesthesia group experienced bad quality of sleep the night after surgery significantly more often than the women who had spinal anesthesia (odds ratio [OR] 2.45; p = 0.03). This was almost exclusively attributed to a significantly higher consumption of opioids postoperatively in the general anesthesia group. Risk factors for bad quality of sleep during the first night postoperatively were: opioids (OR 1.07; p = 0.03); rescue antiemetics (OR 2.45; p = 0.05); relative weight gain (OR 1.47; p = 0.04); summary score of postoperative symptoms (OR 1.13; p = 0.02); and stress coping capacity (OR 0.98; p = 0.01). A longer hospital stay was strongly associated with a poorer quality of sleep the first night postoperatively (p = 0.002).
Conclusions:
The quality of sleep the first night after abdominal hysterectomy is an important factor for recovery. In fast-track abdominal hysterectomy, it seems important to use anesthesia and multimodal analgesia reducing the need for opioids postoperatively and to use strategies that diminish other factors that may interfere negatively with sleep. Efforts to enhance quality of sleep postoperatively by means of preventive measures and treatment of sleep disturbances should be included in fast-track programs.
Clinical Trial Information:
The study was registered in ClinicalTrial.gov Protocol Registration System (NCT00527332) with initial release September 7 2007.
Citation:
Kjølhede P; Langström P; Nilsson P; Wodlin NB; Nilsson L. The impact of quality of sleep on recovery from fast-track abdominal hysterectomy. J Clin Sleep Med 2012;8(4):395-402.
Keywords: Abdominal hysterectomy, fast track, general anesthesia, quality of sleep, postoperative recovery, spinal anesthesia
The purpose of fast-track programs in surgery is to enhance postoperative recovery.1 Fast-track programs usually involve modalities to optimize preoperative conditions, including the provision of detailed information about the cause of events peri- and postoperatively. In the operative period, the use of regional anesthesia and minimally invasive surgery are advocated. Multimodal pain control, antiemetic prophylaxis, early mobilization, and enteral nutrition are encouraged. Fast-track programs almost unanimously recommend use of opioid-free or opioid-reduced multimodal analgesia postoperatively.1
BRIEF SUMMARY
Current Knowledge/Study Rationale: Surgery may cause significant sleep disturbances that may influence the postoperative recovery. This study sought to evaluate the impact of mode of anesthesia on perceived quality of sleep postoperatively and to analyze the perceived quality of sleep in affecting recovery after abdominal hysterectomy in a fast track program.
Study Impact: Perceived quality of sleep was significantly better after spinal anesthesia mainly due to the significantly lower need of opioids postoperatively. The quality of sleep is an important factor for postoperative recovery and efforts to enhance quality of sleep postoperatively by means of prevention and treatment of sleep disturbances should consistently be included in fast-track programs.
One of the most prevalent postoperative symptoms following hysterectomy is disturbed sleep.2 Postoperative sleep disturbances may affect mood, resulting in decreased vigor and an increase in the subjective feeling of sleepiness and fatigue. Thus, postoperative sleep disturbance may be an important factor for postoperative recovery and consequently an important issue to be considered in programs to enhance postoperative recovery. However, fast-track programs seldom include concepts to improve sleep postoperatively1; it was only recently that Krenk et al. suggested that prophylactic intervention to improve sleep architecture be included in fast-track methodology.3
The impact of surgery and anesthesia on postoperative sleep after hysterectomy in a fast-track setting has not been carefully studied. Surgery has been shown to cause circadian disturbances on several levels, including a disrupted sleep pattern.4–7 A substantial decrease in REM sleep occurs on the first postoperative night,6,7 followed by a profound rebound phenomenon on the second to fourth postoperative night, when REM sleep increases in both intensity and amount.4,6,7 Opioid use, whether acute (as when used postoperatively) or chronic, has been associated with abnormal sleep architecture.8 Gögenur et al. found that the subjective quality of sleeping was significantly worse during the first 4 days postoperatively after abdominal surgery.5 This might indicate that this period is the most important if sleep disturbance is to have an impact on postoperative recovery. Although Rosenberg-Adamsen et al. concluded that general anesthesia per se is not an important factor for sleep disturbance postoperatively when comparing general and regional anesthesia,6 the studies to which they referred used different anesthetic agents. In addition, their studies were not conducted on fast-track programs.
We have previously presented the results of the primary and secondary objectives of an open randomized multicenter study comparing general anesthesia and spinal anesthesia in fast-track abdominal hysterectomy for benign conditions (the “GASPI study”) with focus on postoperative recovery.9–11 The trial showed a significantly better outcome for patients given spinal anesthesia, with fewer perceived symptoms postoperatively, faster recovery of quality of life, and shorter sick leave. In addition, the consumption of opioids was significantly lower in the spinal group, almost 5-fold lower on the first postoperative day. Based on these results and applying the philosophy of the fast-track concepts, we hypothesized that women having abdominal hysterectomy for benign conditions conducted in spinal anesthesia perceive the quality of sleep postoperatively as being better than do women who have had a hysterectomy carried out under general anesthesia.
The aims of this secondary post hoc analysis of the GASPI study were to examine the impact of mode of anesthesia on perceived quality of sleep and to analyze the perceived quality of sleep in affecting recovery from surgery.
METHODS
This open, controlled, randomized multicenter study compared the results of elective abdominal hysterectomy in a fast-track program for benign conditions conducted under general anesthesia with results of operations conducted under spinal anesthesia. Five hospitals in the Southeast of Sweden participated in the trial, which was conducted between March 2007 and December 2009. The study was approved by the Regional Ethical Board in Linköping (registration no. M159-06).
The study has been presented in detail previously.9–11 Inclusion criteria were ASA 1-2 women age 18-60 years with benign gynecological disorders. Exclusion criteria were former or planned concomitant bilateral oophorectomy, postmenopausal women without hormone therapy, gynecological malignancy, morphine allergy, physically disabled, severe psychiatric or mental disorder, and any condition contraindicating regional anesthesia. The patients signed informed consent forms prior to inclusion in the study. One-hundred eighty women were randomized and 162 completed the study; 80 were allocated to general anesthesia and 82 to spinal anesthesia.
Fast-Track Program
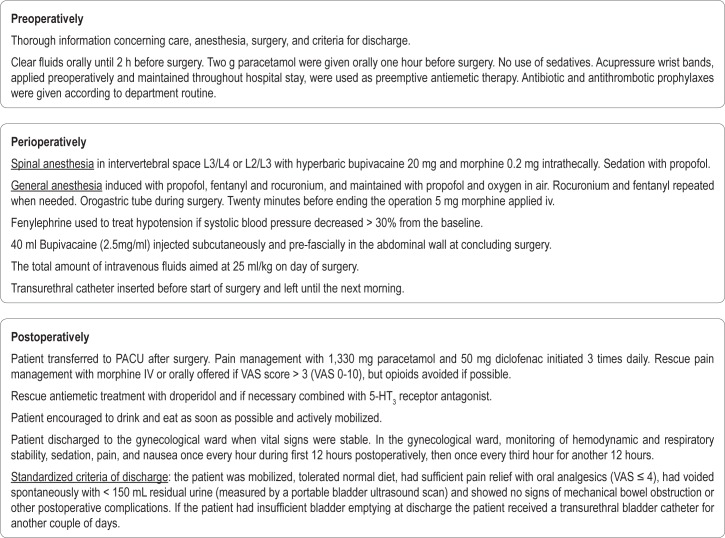
The fast-track program is described in Figure 1.
Figure 1. Summary of the fast-track program and anesthesia.
5-HT3, 5-hydroxytryptamine type 3; IV, intravenous; PONV, postoperative nausea and vomiting; PACU, post anesthesia care unit; VAS, visual analogue scale.
Anesthesia
Both modes of anesthesia were standardized. In summary, general anesthesia was based on propofol 1-2 mg/kg given for induction, followed by a maintenance dose of 6-10 mg/kg/h given continuously as intravenous (IV) infusion. The patients were intubated after fentanyl 0.1-0.2 mg and rocuronium 0.6 mg/kg were administered and ventilated with oxygen in air. Rocuronium and fentanyl were repeated during anesthesia when the attending anesthetist saw they were needed. Twenty minutes before completing surgery 5 mg morphine was given IV
The spinal anesthesia was administered using a 25-gauge needle in the L3/L4 or L2/L3 intervertebral space. The anesthetic consisted of 20 mg hyperbaric bupivacaine (5 mg/mL) and 0.2 mg morphine (0.4 mg/mL). Fifteen minutes after administration of anesthesia, the level of the neural blockade was determined with a cold test and registered. The patients were sedated throughout the operation with a continuous IV infusion of propofol 2-5 mg/kg/h. The patient received general anesthesia according to the protocol described above if the spinal anesthesia was insufficient for the surgery.
Surgery
Modes of skin incision and hysterectomy were decided on by the gynecologist prior to randomization. The hysterectomy was performed as a standard extrafascial hysterectomy according to the principles described by Thompson.12
Postoperative Care
After surgery, the patient was transferred to the post anesthesia care unit (PACU) for postoperative monitoring of hemodynamic and respiratory stability, degree of sedation, pain, and nausea. When the vital signs were stable and the patient was awake, she was discharged from PACU to the gynecological ward where the monitoring was continued. Provided that measures were within clinically normal limits, the monitoring was registered once every hour for 12 h, then once every third hour until 24 h after surgery. The monitoring was identical after both modes of anesthesia. Mobilization was initiated in PACU and actively encouraged in the ward. Similarly, eating and drinking were recommended as soon as possible after surgery. The patient was discharged from the hospital when the standardized criteria for discharge were obtained (Figure 1).
Clinical data including data on complications were collected continuously during hospital stay and at the follow-up visit 5 weeks postoperatively. Duration of hospital stay was defined as the time from start of anesthesia to the time the patient left the hospital.
Assessment of Postoperative Symptoms
Postoperative symptoms were assessed by the Swedish Postoperative Symptoms Questionnaire (SPSQ).10,13 The patient completed the form on a daily basis, preferably in the evening during the first 7 days postoperatively, starting in the evening after surgery (day 0) and thereafter once weekly until the 5-week postoperative visit. The questions were both open-ended and closed-ended. The closed-ended questions could be answered by choosing an answer from a set given on a Likert-type scale. The open-ended questions required written responses. The patient was initially asked if she at the moment of completing the form experienced a number of symptoms commonly reported after surgery (pain in the area of surgery, nausea, retching, headache, abdominal pain, tiredness, drowsiness, and blurred vision) and how she rated the intensity of each of these symptoms. The answers were rated on a 4-point scale: “none” (0), “yes, a little” (1), “yes, somewhat” (2), and “yes, a lot” (3). To estimate overall discomfort from the symptoms at the moment of completing the form, a sum score was calculated. The minimum sum score was zero and maximum 24. The higher the sum score, the greater the discomfort experienced. In order to obtain information about the quality of sleep postoperatively, we added the question in the SPSQ: How did you sleep during the recent night? The options for the answers were: “Excellent,” “Neither well nor badly,” and “Badly.”
Assessment of Stress Coping Capacity
The capacity to cope with stress was measured approximately 1 week preoperatively by the Stress Coping Inventory (SCI).14,15 The respondent rates how often she thinks she is able to cope with each of the 41 stressful situations described in the SCI form.15 The answers are rated on a 6-point Likert-type scale, ranging from “almost never” (1), “rarely” (2), “occasionally” (3), “rather often” (4), “very often” (5) to “almost always” (6). The minimum sum score is 41 and the maximum 246. The higher the SCI sum score, the greater the stress coping capacity. The SCI sum score was first calculated after termination of the study and thus blinded for the participant, staff, and investigators during the study period.
Sick Leave
At discharge from the hospital the patient was granted sick leave for 14 days. The research nurse contacted the patient by telephone the day after discharge and then once weekly until the visit 5 weeks postoperatively. At these contacts, the sick leave was prolonged by ≤ 7 days at a time until the patient considered she was able to return to work or felt sufficiently recovered. Duration of sick leave was defined as the time from the day of surgery to the day of return to work to the same extent as preoperatively. Women, who were on sick leave for reasons other than the hysterectomy, were unemployed, or had disability pension were excluded from the analysis of sick leave.
Statistics
Power calculation and estimation of sample size were based on the primary outcome measure of the trial, duration of hospital stay, and have previously been described.9 No power calculations were done a priori for the secondary outcomes. The analyses were conducted according to the intention-to-treat principles.
Data are presented as mean and one standard deviation (SD) or as number and frequency (%). Univariate analyses were conducted by means of nonparametric tests (Mann-Whitney U-test and Yates corrected χ2 test, as appropriate). Level of significance was set at 5%.
Factors associated with the perceived quality of sleep were analyzed by means of multiple logistic regression models. Adjustments were carried out simultaneously for factors known to be confounding factors of sleep disorders6: age, BMI, mode of hysterectomy (surgical stress, i.e., extent of surgery), stay in PACU after midnight for monitoring, interval of monitoring of vital signs, and SCI sum scores. Subsequently, other factors were added one by one separately as potential confounders in order to analyze whether they were independent risk factors for perceived bad quality of sleep. Results are reported as odds ratio (OR) and 95% confidence interval (CI).
Analysis of covariance (ANCOVA) models were used to investigate associations between outcome measures and perceived quality of sleep the first night after surgery. For the analysis of association between duration of hospital stay and quality of sleep, adjustments were performed simultaneously for the confounders depicted above and for the SPSQ sum score and the occurrence of complications during hospital stay. For the analysis of duration of sick leave, complications occurring perioperatively and during a 5-week period postoperatively were added as independent factors, as was the physical work load. Subsequent post hoc analyses were done with Fisher protected least significant difference (PLSD).
Data were processed in the software StatView for Windows, Version 5.0.1 (SAS Institute Inc., SAS Campus Drive, Cary, NC, USA).
RESULTS
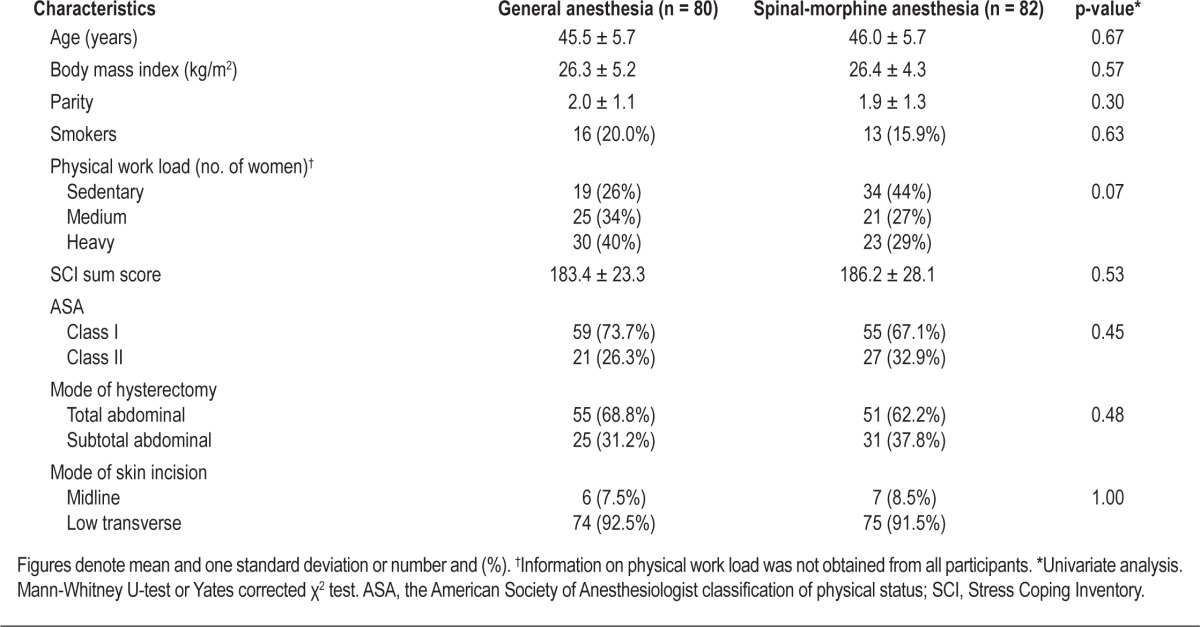
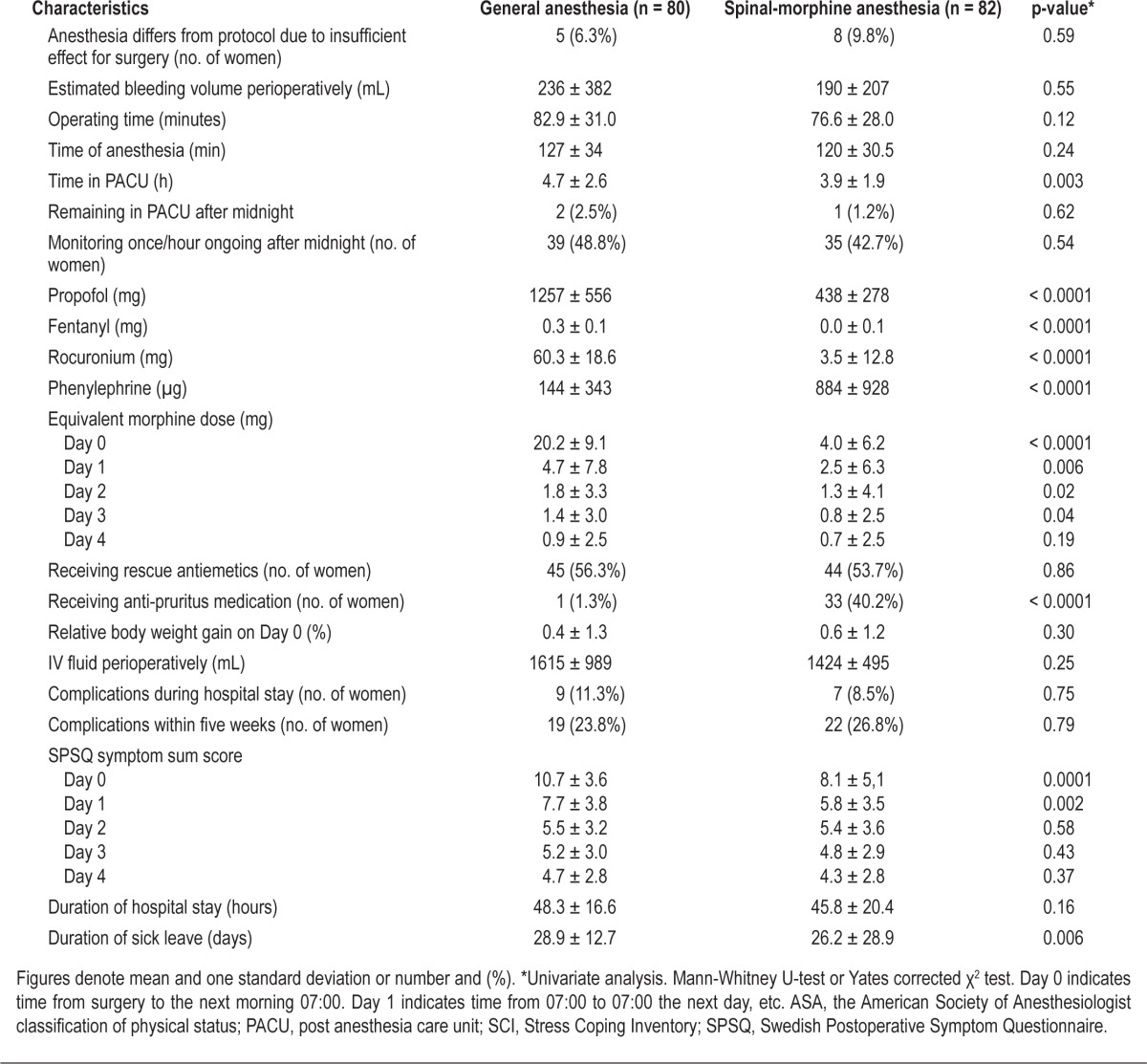
Demographic and descriptive data are presented in Table 1. The preoperative data were well balanced between the 2 groups, showing that the randomization process worked well. The clinical data and the outcome measures shown in Table 2 differed significantly in many aspects, often in favor of the SA group.
Table 1.
Demographic and descriptive data
Table 2.
Clinical data and outcome measures
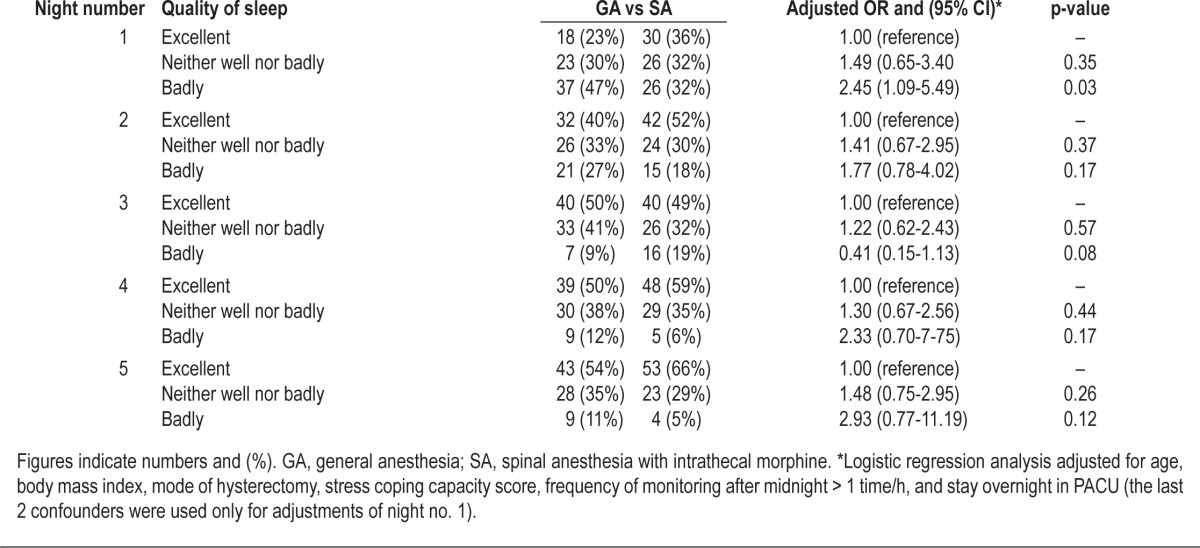
The self-reported perceived quality of sleep for the first 5 nights postoperatively is presented in Table 3. Significantly more women in the GA group reported that they slept badly the first night after surgery compared with women who had the operation in SA. This difference was almost exclusively attributed to the amount of opioids given postoperatively until the next morning. When adjusted for the amount of opioids, there was no statistical difference in the proportion of women who reported that they slept badly the first night between the GA and SA groups (OR 0.84; 95% CI 0.25-2.89; p = 0.79). The amount of opioids given postoperatively was an independent risk factor for experiencing bad quality of sleep the first night postoperatively (OR 1.07; 95% CI 1.01-1.14; p = 0.03). However, the statistically significant difference in quality of sleep between the 2 groups remained when adjustments were made for the fentanyl given perioperatively. In addition, fentanyl seemed to be an independent if weak protective factor for good quality of sleep (OR 0.02; 95% CI 0.00-0.90; p = 0.04). The use of a rescue antiemetic was also an independent risk factor for bad quality of sleep even when adjusted for the use of opioids (OR 2.45; 95% CI 1.02-5.92; p = 0.05). Similarly, relative body weight gain on day 0 was a risk factor for bad quality of sleep in the night after surgery (OR 1.47; 95% CI 1.02-2.10; p = 0.04).
Table 3.
Self-reported quality of sleep night 1-5 after fast-track abdominal hysterectomy in relation to mode of anesthesia
The SPSQ symptom sum scores measured day-by-day for the first 5 days postoperatively were concurrently statistically significantly associated with bad quality of sleep, even when adjusted for daily use of opioids. (OR Day 0 1.13; 95% CI 1.02-1.24; p = 0.02. OR Day 1 1.18; 95% CI 1.04-1.35; p = 0.01. OR Day 2 1.23; 95% CI 1.10-1.49; p = 0.001. OR Day 3 1.44; 95% CI 1.17-1.77; p = 0.0005. OR Day 4 1.57; 95% CI 1.23-2.00; p = 0.0003.)
None of the following variables were significantly associated with the quality of sleep the first night after surgery (data not shown): propofol, rocuronium, phenylephrine, administration of anesthesia that differed from the anesthesia specified in the protocol due to an initial effect insufficient for surgery, use of anti-pruritus medication, operating and anesthesia time, time in PACU, and intravenously given fluid perioperatively.
Of the confounding factors used in the multivariate models, only the SCI sum score was found to be an independent risk factor for occurrence of sleep of bad quality (OR 0.98; 95% CI 0.96-0.99; p = 0.01).
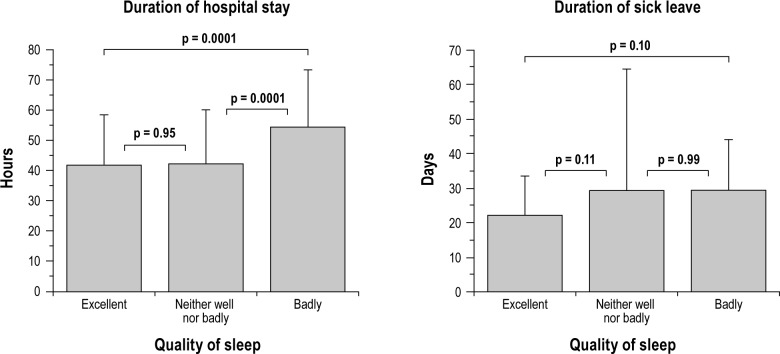
The ANCOVA models revealed that the quality of sleep the first night was strongly associated with duration of hospital stay (F2,157 = 6.695; p = 0.002) (Figure 2). Excellent quality of sleep was associated with a significantly shorter stay in hospital (42 ± 16 h) compared with 54 ± 10 h for those who perceived bad quality of the sleep. No such association was observed concerning duration of sick leave (F2,143 = 1.667; p = 0.19). The p-values of the Fisher PLSD post hoc tests are shown in Figure 2.
Figure 2. Associations between the quality of sleep the night after surgery and duration of hospital stay and sick leave.
Boxes represent mean and error bars represent SD; p-values represent results of Fisher PLSD post hoc tests.
DISCUSSION
The study demonstrated that sleep the first night postoperatively is an important quality to be given careful consideration even in fast-track program, as it affects the postoperative recovery substantially. Abdominal hysterectomy under spinal anesthesia offered significantly better quality of sleep than did general anesthesia, which led to a significantly shorter stay in the hospital. However, this effect was almost exclusively attributed to a significantly lower consumption of opioids postoperatively in the spinal anesthesia group. As shown in this study, quality of sleep after surgery is a feature that influences the recovery. Many factors, some of which can be treated or interfered with, seem to be associated with this phenomenon in fast-track abdominal hysterectomy.
There are some methodological concerns in this study. The study was not powered to detect differences in secondary outcome measures, and the study should therefore be seen as exploratory and hypothesis generating. There is a lack of baseline information about quality of sleep, and thus no adjustment has been made for this obvious potential confounder.6 However, the study was randomized and the allocation showed even distribution between the two groups for all other investigated preoperative variables, including psychological and quality of life measurements.11 We therefore find it less likely that baseline quality of sleep would be unevenly distributed between the two groups. The quality of sleep was determined by posing a simple question that could be answered by choosing an answer from a set of three options given on a Likert-type scale. This might be considered as a crude method and may lack the properties needed to detect possible subtle differences. However, other authors have used a simple visual analogue scale for the purpose of measuring the quality of sleep.5,16–18
Several factors contribute to disturbed sleep postoperatively.6 Use of opioids has been shown to change sleep architecture substantially in healthy subjects.19 This coheres with our findings that the amount of opioids given postoperatively was an independent risk factor for bad quality of sleep. Interestingly, we found that fentanyl improved quality of sleep. Fentanyl is a short-acting opioid and was given exclusively during surgery. Mustola et al. have recently shown that fentanyl given during general anesthesia reduces the surgical stress response.20 The injury caused by surgery provokes a complex stress response involving release of stress hormones, humoral mediators of the endocrine and metabolic system, and activation of the immune system.6 All these factors may influence sleep architecture adversely. Thus by reducing the stress response, fentanyl may consequently improve sleep architecture and quality of sleep. The relative body weight gain the first day after surgery was an independent risk factor for bad quality of sleep in the present study. Since we found no association between sleep and the volume of the IV fluid given perioperatively, the relative body weight gain may be an effect of increased release of stress hormones and inflammatory processes and thus may represent an increased stress response.
We found that quality of sleep in the first night postoperatively was associated with the length of hospital stay. This is to our knowledge the first report to show such a clinically important association. The standardized criteria for discharge were emphasized in the fast-track program. In the analysis, we adjusted for several confounders that might influence the hospital stay or quality of sleep. Still, we found a significantly longer stay in hospital for the group who perceived having had a bad quality of sleep the first night after surgery. This indicates that the quality of sleep is an important factor for postoperative recovery.
Our results seem to support the conclusion stated by Rosenberg-Adamsen et al.6 that mode of anesthesia—spinal or general anesthesia—per se does not influence the quality of sleep postoperatively. An anesthetic technique that gives good and prolonged analgetic effect with minimum use of opioids postoperatively should be chosen in fast-track programs. It is a common clinical impression that symptoms such as pain21 and postoperative nausea and vomiting (PONV) causes disturbed night sleep. Use of opioids and rescue antiemetics may be regarded as surrogate measures of pain and PONV. However, the drugs themselves may interfere with sleep, so it may be difficult to ascertain whether it is the symptom or the drug that affects the sleep. We found that postoperative symptoms in terms of the SPSQ symptom sum score, irrespective of treatment of symptoms, was a strong risk factor for bad quality of sleep the five first nights postoperatively. This is an important finding, indicating that fast-track programs should include the use of modalities designed to decrease troublesome postoperative symptoms in order to positively affect and maintain sleep of good quality.
In conclusion, the quality of sleep the first night after elective abdominal hysterectomy is an important factor for the recovery. In fast-track it seems important to use anesthesia and multimodal analgesia that reduce the need of opioids postoperatively and use strategies that diminish other factors that may interfere negatively with sleep. Efforts to enhance quality of sleep postoperatively by means of prevention and treatment of sleep disturbances should be included in fast-track programs. Further studies are needed.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
The study was financially supported by grants from the Medical Research Council of South East Sweden; Linköping University and the County Council of Östergötland.
ABBREVIATIONS
- ANCOVA
analysis of covariance
- ASA
American Society of Anesthesiologist classification of physical status
- BMI
body mass index
- CI
confidence interval
- 5-HT3
5-hydroxytryptamine type 3
- GA
general anesthesia
- IV
intravenous
- OR
odds ratio
- PACU
post anesthesia care unit
- PLSD
protected least significant difference
- PONV
postoperative nausea and vomiting
- SA
spinal anesthesia with intrathecal morphine
- SCI
Stress Coping Inventory
- SD
standard deviation
- SPSQ
Swedish Postoperative Symptom Questionnaire
- VAS
Visual Analogue Scale
REFERENCES
- 1.Kehlet H, Wilmore DW. Multimodal strategies to improve surgical outcome. Am J Surg. 2002;183:630–41. doi: 10.1016/s0002-9610(02)00866-8. [DOI] [PubMed] [Google Scholar]
- 2.Kim KH, Lee KA. Sleep and fatigue symptoms in women before and 6 weeks after hysterectomy. J Obstet Gynecol Neonatal Nurs. 2009;38:344–52. doi: 10.1111/j.1552-6909.2009.01029.x. [DOI] [PubMed] [Google Scholar]
- 3.Krenk L, Rasmussen LS, Kehlet H. New insights into the pathophysiology of postoperative cognitive dysfunction. Acta Anaesthesiol Scand. 2010;54:951–6. doi: 10.1111/j.1399-6576.2010.02268.x. [DOI] [PubMed] [Google Scholar]
- 4.Gögenur I, Wildschiotz G, Rosenberg J. Circadian distribution of sleep phases after major abdominal surgery. Br J Anaesth. 2008;100:45–9. doi: 10.1093/bja/aem340. [DOI] [PubMed] [Google Scholar]
- 5.Gögenur I, Bisgaard T, Burgdorf S, van Someren E, Rosenberg J. Disturbances in the circadian pattern of activity and sleep after laparoscopic versus open abdominal surgery. Surg Endosc. 2009;23:1026–31. doi: 10.1007/s00464-008-0112-9. [DOI] [PubMed] [Google Scholar]
- 6.Rosenberg-Adamsen S, Kehlet H, Dodds C, Rosenberg J. Postoperative sleep disturbances: mechanisms and clinical implications. Br J Anaesth. 1996;76:552–9. doi: 10.1093/bja/76.4.552. [DOI] [PubMed] [Google Scholar]
- 7.Rosenberg J. Sleep disturbances after non-cardiac surgery. Sleep Med Rev. 2001;5:129–37. doi: 10.1053/smrv.2000.0121. [DOI] [PubMed] [Google Scholar]
- 8.Wang D, Teichtahl H. Opioids, sleep architecture and sleep-disordered breathing. Sleep Med Rev. 2007;11:35–46. doi: 10.1016/j.smrv.2006.03.006. [DOI] [PubMed] [Google Scholar]
- 9.Borendal Wodlin N, Nilsson L, Kjølhede P for the GASPI study group. The impact of mode of anaesthesia on postoperative recovery from fast-track abdominal hysterectomy: a randomised clinical trial. BJOG. 2011;118:299–308. doi: 10.1111/j.1471-0528.2010.02697.x. [DOI] [PubMed] [Google Scholar]
- 10.Borendal Wodlin N, Nilsson L, Årestedt K, Kjølhede P for the GASPI study group. Mode of anesthesia and postoperative symptoms following abdominal hysterectomy in a fast-track setting. Acta Obstet Gynecol Scand. 2011;90:369–79. doi: 10.1111/j.1600-0412.2010.01059.x. [DOI] [PubMed] [Google Scholar]
- 11.Borendal Wodlin N, Nilsson L, Kjølhede P. Health-related quality of life and postoperative recovery in fast track hysterectomy. Acta Obstet Gynecol Scand. 2011;90:362–8. doi: 10.1111/j.1600-0412.2010.01058.x. [DOI] [PubMed] [Google Scholar]
- 12.Thompson JD. Hysterectomy. In: Thompson JD, Rock JA, editors. Te Lindeés Operative Gynecology. 7th edition. Philadelphia: JB Lippincott Company; 1992. pp. 687–706. [Google Scholar]
- 13.Alkaissi A, Gunnarsson H, Johnsson V, Evertsson K, Ofenbartl L, Kalman S. Disturbing post-operative symptoms are not reduced by prophylactic antiemetic treatment in patients at high risk of post-operative nausea and vomiting. Acta Anaesthesiol Scand. 2004;48:761–71. doi: 10.1111/j.0001-5172.2004.00403.x. [DOI] [PubMed] [Google Scholar]
- 14.Ryding EL, Wijma B, Wijma K, Rydhström H. Fear of childbirth during pregnancy may increase the risk of emergency caesarean section. Acta Obstet Gynecol Scand. 1998;77:542–7. [PubMed] [Google Scholar]
- 15.Persson P. On the mode of hysterectomy-with emphasis on recovery and well-being. Linköping University Medical Dissertations no. 1104. 2009 ISBN 978-91-7393-687-3. [Google Scholar]
- 16.Shell W, Bullias D, Charuvastra E, May LA, Silver DS. A randomized, placebo-controlled trial of an amino acid preparation on timing and quality of sleep. Am J Ther. 2010;17:133–9. doi: 10.1097/MJT.0b013e31819e9eab. [DOI] [PubMed] [Google Scholar]
- 17.Gögenur I, Middleton B, Burgdorf S, Rasmussen LS, Skene DJ, Rosenberg J. Impact of sleep and circadian disturbances in urinary 6-sulphatoxymelatonin levels, on cognitive function after major surgery. J Pineal Res. 2007;43:179–84. doi: 10.1111/j.1600-079X.2007.00460.x. [DOI] [PubMed] [Google Scholar]
- 18.Freedman NS, Kotzer N, Schwab RJ. Patient perception of sleep quality and etiology of sleep disruption in the intensive care unit. Am J Respir Crit Care Med. 1999;159(4 Pt 1):1155–62. doi: 10.1164/ajrccm.159.4.9806141. [DOI] [PubMed] [Google Scholar]
- 19.Dimsdale JE, Norman D, DeJardin D, Wallace MS. The effect of opioids on sleep architecture. J Clin Sleep Med. 2007;3:33–6. [PubMed] [Google Scholar]
- 20.Mustola S, Parkkari T, Uutela K, Huiku M, Kymäläinen M, Toivonen J. Performance of surgical stress index during sevoflurane-fentanyl and isoflurane-fentanyl anesthesia. Anesthesiol Res Pract. 2010;2010.pii:810721. doi: 10.1155/2010/810721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Closs SJ. Patients' night-time pain, analgesic provision and sleep after surgery. Int J Nurs Stud. 1992;29:381–92. doi: 10.1016/0020-7489(92)90016-a. [DOI] [PubMed] [Google Scholar]