Abstract
Out-of-body experiences are the phenomena of seeing the image of one's body from an external perspective. We report the case of a patient affected by psychophysiological insomnia who presents hallucinatory phenomenon, successfully treated with haloperidol.
We hypothesize that these hallucinations during psychophysiological insomnia are expression of an alteration of specific neurocognitive networks that regulate the cognitive arousal systems.
Citation:
Occhionero M; Natale V; Martoni M; Tonetti L. Mind's eye: a case of out-of-body experiences. J Clin Sleep Med 2012;8(4):445-446.
Keywords: Out-of-body experiences, psychophysiological insomnia, sleep assessment, dreaming
Autoscopic phenomena (AP) are hallucinatory visual experiences that consist of seeing the physical body placed in external visual space, like a reflection in a mirror. Many diseases, brain lesions, pharmacological agents, and altered psychological states are reportedly associated with these phenomena.1 An interesting feature of this type of hallucination is that it can be observed in the absence of neurological and/or psychiatric diseases. Favorable conditions seem to include the wake-sleep and sleep-wake transitions.2
There are three main types of autoscopic phenomena, characterized by different phenomenology: out-of-body experiences (OBEs), autoscopic hallucinations (AH), and heautoscopy (HAS).3 In OBEs, the patient sees himself outside his own body, has the impression of seeing the environment around oneself and one's own body from an external perspective, and finally had the feeling of a body-mind separation. In AH, the patient sees a reduplication of himself in his extrapersonal space without disembodiment, a sort of mirror image of oneself. Generally, self-perception (feelings, emotions, thoughts) remains anchored to one's own body. It is a pure duplication of the body, not of the mind. HAS represents an intermediate form between the out-of-body experience and autoscopic hallucination, with a confused or double allocation of the self. The patient isn't able to decide if he is disembodied or not, and his experience is similar to a “double consciousness,” but the body perception is confused (single, double, or disembodied).
In the present case report, we discuss OBEs in a patient affected by psychophysiological insomnia who presented hallucinatory phenomena during spontaneous infra-sleep awakenings.
REPORT OF CASE
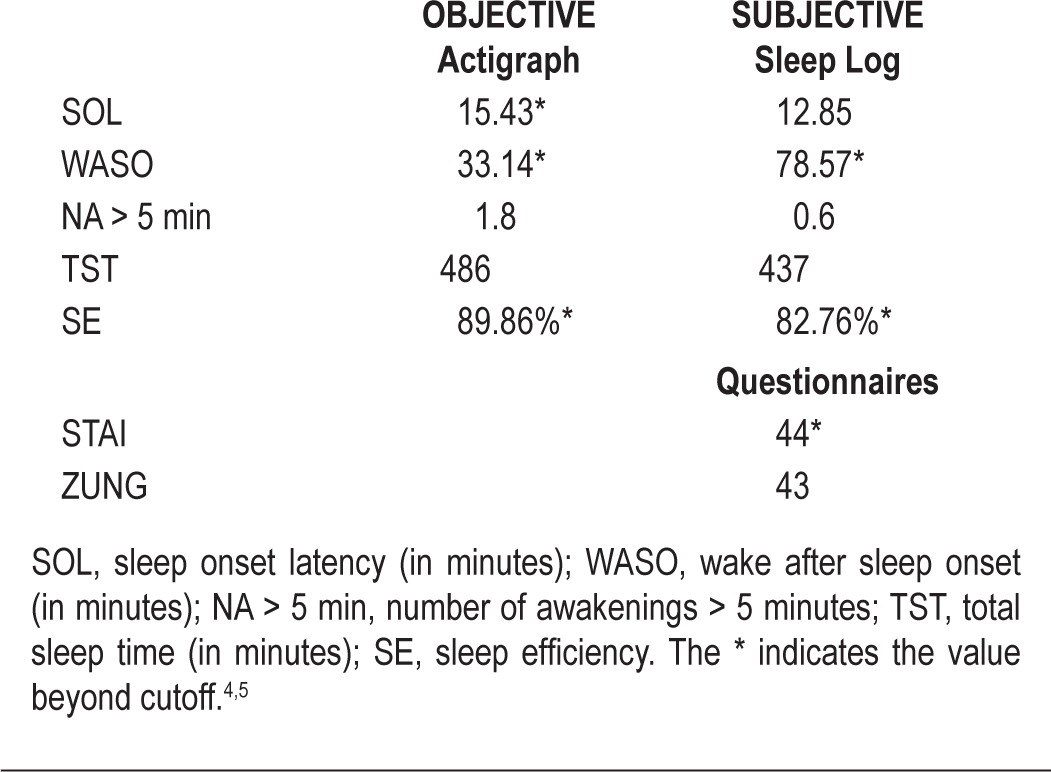
SC, a 50-year-old female, reported a history of insomnia for approximately 3 years. To permit a correct diagnosis, the assessment protocol provides a sleep log, actigraphy, and anxiety (STAI) and depression (ZUNG) questionnaires. The patient evaluation was carried out through 4 sessions, during which other sleep disorders were excluded. The diagnosis was psychophysiological insomnia characterized by difficulty maintaining sleep (see Table 1).
Table 1.
Mean of measurements from actigraph, sleep log and questionnaires
The patient spontaneously reported that she had OBEs 3 times in the previous 6 months during nighttime awakenings. The description provided by the patient was extremely detailed and vivid. She described her body split: “I see myself as if I was from an airplane and looking down at a distance of about five feet. I feel split and I see myself down. I have my body down, I'm not in my body, I'm out of my body. My mind sees my body, I see the shape of my body. The part of mine that is over…it seems strange to me looks like an angel, an entity. I see the body there but I'm like air…”
The patient estimated that the duration of each phenomenon was very short, but not static and therefore not comparable to a photograph. She describes the experience as a small video with an abrupt, approximately half-minute onset and offset. An interesting aspect was related to the uncertain reality testing: the patient was not able to determine whether the hallucinatory experience occurred in the real world or in her mind. Certainly, she was aware of the real nature of the phenomenon.
Given the unpredictable and rare nature of the phenomenon, it was not possible to perform a PSG recording to understand the physiological condition (sleep or wake) in which the OBEs occur.
The patient also reported that in recent months, her dreaming activity has significantly increased. The dreams had become very complex in content and very vivid regarding visual hallucinatory aspects.
She judged these hallucinatory experiences to be very real, but she was not worried about them. This condition was accompanied by feelings of strangeness, wonder, amazement, and happiness at seeing her body sleeping on the bed. During the day, she believed that these phenomena could be indicators of a severe psychological disorder.
The emotional dissociation related to the dream should not leave amazed. Cognitive research on dream bizarreness (and OBEs are a case of bizarreness in the representation of self) has amply demonstrated that rarely the dreamer has an oneiric awareness of any implausible content (it could be also a cognitive mechanism useful to the maintaining the continuity of sleep). The implausibility produces emotional incongruence during the dream recall.
At the time of assessment, the patient took one-half tab benzodiazepines (brotizolam 0.125 mg and 0.33 mg of lormetazepam) before bedtime. These drugs did not produce any improvement of her symptoms. We considered appropriate to redefine the therapy with an integrated approach, combining pharmacological (neuroleptic at low doses) and psychological support. The rationale for this choice was to use the neuroleptic, which has a hypnotic effect and an ideation reduction effect. The latter action was intended to counteract the OBEs and the excessive oneiric activity. Seven months after the beginning of therapy, a marked improvement of the subjective symptoms was observed, without any OBEs reported.
DISCUSSION
The interesting aspect of this case report is the occurrence of OBEs, likely triggered by the frequent night awakenings. Visual hallucinations are quite common occurrences during hypnagogic and hypnopompic hallucinations and are a physiological aspect of these phases.6 Such experiences, however, are usually simple visual images characterized by the presence of lines, flashes, and simple geometric shapes. In this case report we observed OBEs which are quite rare in a clinical setting and could be considered a particularly case of recurrent complex visual hallucinations (RCVH).7 In our opinion, the drowsiness can be considered a gray area characterized by the psychophysiological proximity to sleep on the one hand, and the state of low perceptual and sensory stimulation on the other. Both of these factors (physiological and environmental) destabilize the control processes and the levels of consciousness typical of wakefulness. It is possible that this situation could facilitate hallucinatory experiences of self as a result of two components: (1) insufficient neurofunctional integration and lack of binding information from different neural networks responsible for the perception of one's own body as an integral part of psychophysical self-awareness, and (2) the instability of psychophysiological arousal with rebound both on the maintenance of sleep and mental activity. Research on psychophysiological insomnia attributes a specific role to an excessive activation of the central and/or autonomic nervous system (hyperarousal hypothesis).8 According to this hypothesis, a high level of arousal could activate elaborative and mnemonic cortical processes. This condition could lead to the occurrence of hallucinations and excessively vivid oneiric activity as expressions of an alteration of specific neurocognitive networks that regulate the cognitive arousal systems. In selected cases with intense oniric activity and maintaining primary insomnia, pharmacological treatment with low doses of a neuroleptic should reduce cognitive iperarousal given its well-documented effects on the fronto-limbic dopaminergic pathway.
DISCLOSURE STATEMENT
This was not an industry supported study. The authors have indicated no financial conflicts of interest.
REFERENCES
- 1.Dening TR, Berrios GE. Autoscopic phenomena. Br J Psychiatry. 1994;165:808–17. doi: 10.1192/bjp.165.6.808. [DOI] [PubMed] [Google Scholar]
- 2.Bunning S, Blanke O. The out-of-body experience: precipitating factors and neural correlates. Progr Brain Res. 2005;150:331–50. doi: 10.1016/S0079-6123(05)50024-4. [DOI] [PubMed] [Google Scholar]
- 3.Blanke O, Mohr C. Out-of-body experience, heautoscopy, and autoscopic hallucination of neurological origin Implications for neurocognitive mechanisms of corporeal awareness and self-consciousness. Brain Res Rev. 2005;50:184–99. doi: 10.1016/j.brainresrev.2005.05.008. [DOI] [PubMed] [Google Scholar]
- 4.Lichstein KL, Durrence HH, Taylor DJ, Bush AJ, Riedel BW. Quantitative criteria for insomnia. Behav Res Ther. 2003;41:427–45. doi: 10.1016/s0005-7967(02)00023-2. [DOI] [PubMed] [Google Scholar]
- 5.Natale V, Plazzi G, Martoni M. Actigraphy in the assessment of insomnia: a quantitative approach. Sleep. 2009;32:767–71. doi: 10.1093/sleep/32.6.767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ohayon MM, Priest RG, Caulet M, Guilleminault C. Hypnagogic and hypnopompic hallucinations: Pathological phenomena? Br J Psychiatry. 1996;169:459–67. doi: 10.1192/bjp.169.4.459. [DOI] [PubMed] [Google Scholar]
- 7.Collerton D, Perry E, McKeith I. Why people see things that are not there: a novel Perception and Attention Deficit model for recurrent complex visual hallucinations. Behav Brain Sci. 2005;28:737–94. doi: 10.1017/S0140525X05000130. [DOI] [PubMed] [Google Scholar]
- 8.Perlis ML, Giles DE, Mendelson WB, Bootzin RR, Wyatt JK. Psychophysiological insomnia: the behavioural model and a neurocognitive perspective. J Sleep Res. 1997;6:179–88. doi: 10.1046/j.1365-2869.1997.00045.x. [DOI] [PubMed] [Google Scholar]


