Abstract
Objective
Patients with heart failure (HF) have high rates of rehospitalization. Home health care (HHC) patients with HF are not well studied in this regard. The objectives of this study were to determine patient, HHC agency, and geographic (i.e., area variation) factors related to 30-day rehospitalization in a national population of HHC patients with HF, and to describe the extent to which rehospitalizations were potentially avoidable.
Data Sources
Chronic Condition Warehouse data from the Centers for Medicare & Medicaid Services.
Study Design
Retrospective cohort design.
Data Extraction
The 2005 national population of HHC patients was matched with hospital and HHC claims, the Provider of Service file, and the Area Resource File.
Principal Findings
The 30-day rehospitalization rate was 26 percent with 42 percent of patients having cardiac-related diagnoses for the rehospitalization. Factors with the strongest association with rehospitalization were consistent between the multilevel model and Cox proportional hazard models: number of prior hospital stays, higher HHC visit intensity category, and dyspnea severity at HHC admission. Substantial numbers of rehospitalizations were judged to be potentially avoidable.
Conclusions
The persistently high rates of rehospitalization have been difficult to address. There are health care-specific actions and policy implications that are worth examining to improve rehospitalization rates.
Keywords: Heart failure, epidemiology, outcomes research, home health care
Rehospitalization rates have become a focus of national interest as they are associated with high health care expenditures and questions concerning the quality of care provided during and following hospitalization. Two recent reports identify a 20 percent rehospitalization rate within 30 days of the initial hospital discharge: Bueno and colleagues (Bueno et al. 2010), in a population-based study specific to patients with heart failure, reported that 20 percent of Medicare beneficiaries were rehospitalized within 30 days of discharge while Jencks et al. studied a heterogeneous group of Medicare beneficiaries and found the same rehospitalization rate (Jencks, Williams, and Coleman 2009). Of note within the Jencks report is the prominent role of the diagnosis of heart failure (HF): a HF diagnosis was the most frequent reason for a medical diagnosis-based rehospitalization and the most frequent diagnosis associated with a surgical diagnosis-based rehospitalization. Thus, heart failure, as a syndrome, is clearly identified as a consistent diagnosis associated with persistently high rates of rehospitalization (Ross et al. 2010).
Home health care is an essential part of the U.S. health care system with more than 10,000 agencies providing care to more than 3 million patients (Medicare Payment Advisory Commission 2010). Home health care services are available to Medicare beneficiaries who meet the guidelines for services: in need of skilled services for an intermittent period (not continuous care) and homebound where substantial effort is required to leave the home. Home health care patients may represent some of the “sicker” patients with HF because of the Medicare homebound requirements. Moreover, they also represent patients whose health care provider or family member identified a need for professional care in the home. However, it is not clear how home health care need or referrals are identified among hospitalized patients, regardless of diagnosis, or how home health care is integrated with other parts of the post-acute care system (Kane 2011; Mor and Besdine 2011).
Research indicates that referral rates to home health care from the hospital for patients with HF have increased over time: from 13 percent in 1993 to 18 percent in 2006 (Bueno et al. 2010). There is preliminary evidence of factors associated with rehospitalization among home health care patients in a large diagnostically heterogeneous population, including increased severity of dyspnea, more functional status impairment, and guarded rehabilitation prognosis (Fortinsky et al. 2006). In addition, patients with skin or wound conditions and diabetes were more likely to be hospitalized. In most cases, however, this home health patient hospitalization research has been conducted within one or a geographically limited group of home health care agencies, limiting our understanding of the broader geographic or agency-specific factors associated with rehospitalization.
In addition, potentially avoidable hospitalizations are a priority national interest because these are hospitalizations that presumably could have been averted with high-quality care. Studies of potentially avoidable hospitalizations among nursing home residents (Ouslander et al. 2010) found that 67 percent of the hospitalizations were potentially avoidable. There has been no research in home health care that identifies the extent to which hospitalizations among home health care patients are potentially avoidable, despite the currently high rates of hospitalization among home health care patients in the United States, where risk-adjusted rates have been consistently 29 percent or higher. It is not clear the extent to which home health care agencies can reduce and control potentially avoidable hospitalizations because some hospitalizations occur outside the control of the home health care agency (e.g., family calls 911 and the patient goes to emergency department with or without prior physician contact).
Gaps in this body of research are attributable to the narrow focus on patient factors associated with rehospitalization, leading to the lack of attention to area variation (e.g., number of providers in a geographic area) or home health care agency factors (e.g., association with a hospital system; agency profit status) that could guide additional research and policy changes for patients with HF. There also has not been any identification of the reasons for rehospitalization for home health care patients with HF and whether there are potentially avoidable rehospitalizations. In addition, national population-based studies are needed to expand the understanding beyond small numbers of home health care agencies.
Thus, the purposes of this study were to (1) identify patient-level factors in a national sample of HF patients (which as stated has not been previously reported); (2) determine whether agency level and geographic or agency factors add any additional explanatory value in a national population of home health care patients; and (3) describe the extent to which observed rehospitalizations were potentially avoidable.
Conceptual Framework
We used the Andersen model to organize the potential variables for inclusion in the study by identifying geographic-, agency-, and patient-level variables (Andersen 1995). Within the patient-level variables, we identified, following Andersen, predisposing, enabling, need, and resource use variables. See Table 1 for the list of variables and data sources and Figure 1 for the conceptual model.
Table 1.
Independent Variables and Data Sources
| Variable Name | Source |
|---|---|
| County-level variables | |
| Rural-urban continuum code | Area resource file |
| No. of home health care agencies/100 k population | |
| No. of skilled nursing facilities/100 k population | |
| No. of hospitals/100 k population | |
| Agency-level variables | |
| Hospital-based agency (yes/no) | Provider of service file |
| Agency profit status (for profit, nonprofit, govt) | |
| Patient-level variables | |
| Predisposing | |
| Age (<85 years, ≥85 years) | Beneficiary file |
| Gender | |
| Race (African American, not African American) | |
| Enabling | |
| Has a primary caregiver (yes/no) | OASIS B1 |
| Lives alone (yes/no) | |
| Dually eligible for Medicare + Medicaid (yes/no) | |
| Need | |
| Dyspnea interfering with activity | OASIS B1 |
| Cognitive functioning | |
| Any anxiety (0–3, increasing severity) | |
| Any depressive symptoms (out of 6 possible symptoms) | |
| High risk behaviors (smoking, alcohol intake, illegal drug use) | |
| Problematic behaviors (memory deficit, impaired decision making, aggression) | |
| Life expectancy (<6 months, ≥6 months) | |
| Severity of primary diagnosis (0–4, increasing severity) | |
| Overall prognosis (good/fair or poor) | |
| Overall rehabilitation prognosis (good or guarded) | |
| Total number of comorbidities | |
| Urinary incontinence | |
| Functional status items | |
| Oral medication management | OASIS B1 |
| Ambulation | |
| Bathing | |
| Dressing lower body | |
| Dressing upper body | |
| Feeding | |
| Grooming | |
| Toileting | |
| Transferring | |
| Resource use | |
| Number of prior hospital stays | MedPAR |
| Visit intensity category | Home health SAF |
| Any physical therapy visits | |
| Any occupational therapy visits | |
| Any medical social work visits | |
| Any Speech/language pathology visits | |
| Any home health aide visits | |
Figure 1.
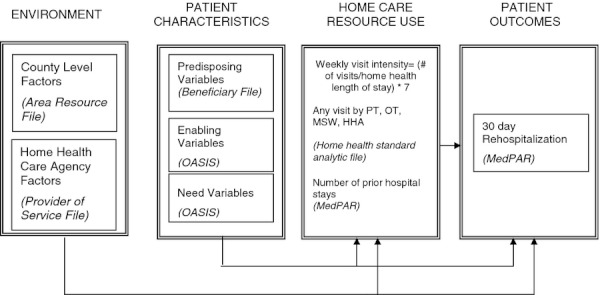
Andersen Model Adaptation for the Present Study
Methods
Population
The national population used for the present study included all home health care patients with a primary home health care diagnosis of heart failure (ICD-9 code 428 and sub-groups) who received home health care services in 2005 and whose care was paid for by the traditional Medicare fee-for-service program. Medicare managed care programs (Medicare Advantage) did not allow the tracking of the numbers of home health care visits. Thus, these patients (∼10 percent of the population) were excluded as were patients whose care was paid for by Medicaid alone or private health insurance. Dually eligible (traditional Medicare and Medicaid) patients were included if traditional Medicare was the primary payer, which is most often the case as payment under Medicare is higher than Medicaid. Patients (n = 1,316) who died before the end of the 30-day period were excluded as their follow-up period for a rehospitalization was censored.
Data Sources
Data were obtained from the Medicare Chronic Conditions Warehouse (CCW), which is a data system designed by the Centers for Medicare & Medicaid Services (CMS) to increase access to Medicare data for researchers studying a specific set of chronic diseases. In addition to a more streamlined application process, the CCW also provides a CCW-specific patient identifier, developed by the CMS contractor, which provides a linking variable across CMS data sets that does not require the use of Social Security or Medicare numbers (Centers for Medicare & Medicaid Services 2009). This then provides additional identity protections to Medicare beneficiaries. Like other studies using identifiable Medicare data, however, a data use agreement with CMS and local institutional review board approval were required and obtained prior to data release.
Patient Level Clinical and Demographic Data: OASIS and Beneficiary File
Home health care patient-level data were derived from the Outcome and Assessment Information Set (OASIS) B1 version. See Table 1. OASIS data are collected on admission to home health care (i.e., start of care), when care resumes following a hospital stay (i.e., resumption of care), at transfer to a hospital, upon death, when the patient is discharged from home health care services (remaining at home), transferred to another site of care (i.e., hospice or nursing home), and at least every 60 days. The most complete versions of the OASIS are collected at start of care and home health care discharge with abbreviated versions collected at the other time points.
For the purpose of the multivariate analyses, individual activities of daily living were coded so that 0 represented “totally independent”; 1 represented “some dependence”; and 2 represented “totally dependent.” Because of small numbers associated with some categories, severity of primary diagnosis was coded such that codes 0, 1, and 2 (asymptomatic, symptoms well controlled, and symptoms controlled with difficulty) were the reference group and codes 3 (“symptoms poorly controlled; patient needs frequent adjustment in treatment and dose monitoring”) and 4 (“symptoms poorly controlled; history of re-hospitalizations”) were compared with the combined group.
There is evidence that OASIS B1 is reliable using inter-rater reliability measures for functional status (Hittle et al. 2003; Madigan and Fortinsky 2004). Madigan and Fortinsky (2004) report that the measure of agreement, kappa, for the functional status items range between .72 (transferring) and .89 (dressing upper body), similar to the findings from Hittle et al. (2003). There is one report on the concurrent validity of the OASIS with evidence that the functional status items performed best when compared to gold standard measures of functional status (Tullai-McGuinness, Madigan, and Fortinsky 2009). OASIS reliability for determination of the use of hospital care in the 14 days prior to initiating home health care has been identified as problematic with a sensitivity of 55 percent (Wolff et al. 2008). For hospitalizations following home health care, the sensitivity is much better (97 percent).
Patient Demographics
The CMS beneficiary file provided us with patient age, gender and race/ethnicity.
Patient-Level Data for Hospitalizations: MedPAR
Hospital-level data were derived from the Medicare Provider and Review file (MedPAR). This file provided us with the numbers and timing of hospitalizations and rehospitalizations in addition to the causes of hospital admissions.
Patient Level Data for Home Visits: Standard Analytic File for Home Health Care
Home health care visit data were derived from the home health care standard analytic file (SAF), which provides home health care visit-level detail by provider type and date. Providers for home health care include skilled nursing (RNs primarily but also LPNs in some agencies), physical therapists (PT), and physical therapy assistants, occupational therapists (OT), and certified occupational therapy assistants, speech and language pathologists (SLP), medical social workers (MSW), and home health aides (HHA). As most (99 percent) of the patients received skilled nursing visits, we identified whether patients received any PT, OT, SLP, MSW, or HHA visits, each coded as yes or no.
For resource use, we used a measure of visit intensity instead of raw numbers of visits or length of stay, as home health care patients have widely varying patterns of home health care visits. A visit intensity measure accounts for the heterogeneous patterns and is calculated as follows: the number of visits divided by the length of stay, multiplied by 7, and then categorized into <1 visit/week, 1–2 visits/week, 3–4 visits/week and >4 visits/week.
Geographic-Level Data: Area Resource File
The Area Resource File (ARF) is county-level data that provide the number of providers in the county for short-term hospitals, skilled nursing facilities, and home health care agencies and the Rural-Urban Continuum Code (RUCC) for the county as an indicator of rurality. These variables represent geographic-level factors.
Agency Level Data: Provider of Service File
The Provider of Service file (POS) is home health care agency-specific, uses the agency's Medicare provider number for linking with the OASIS, and provided us information on the agency's organizational characteristics, including the profit status (for profit, nonprofit, governmental) and whether the agency was affiliated with a hospital (yes or no).
Determination of Rehospitalization
To enter the analytic file for the study, patients needed to have an index hospital stay, defined as a hospital discharge within 14 days of entering home health care. The hospital discharge date was derived from the MedPAR data set and matched by date to the OASIS start of care form (OASIS item M0030). MedPAR has been found to have more accurate data for determination of hospital care when compared to OASIS (Wolff et al. 2008). This time frame was chosen as a longer period between hospital discharge and home health care admission may have resulted in intervening health status changes that would influence the likelihood of rehospitalization. In part, the selection of 14 days between hospital discharge and home health care admission reflects an OASIS item (M0200) that indicates changes in patient condition in the 14 days prior to home health care admission and is consistent with past research in this area (Wolff et al. 2008). Rehospitalization was defined as a subsequent hospital stay within 30 days of the index hospital discharge.
We also determined the number of hospitalizations that occurred within the 6 months prior to the index hospital stay as there is indication from existing research that more hospital stays increase the likelihood of subsequent rehospitalizations (Fonarow 2008; Wolff et al. 2008). The count of the prior hospitalizations was used as an independent variable.
Reasons for Rehospitalization
The reasons for the rehospitalization were determined from the MedPAR files using the diagnostic codes determined at the time of discharge as diagnoses generated on admission are often subject to change during the hospital episode. We categorized the diagnoses as all-cause and cardiac-related according to the categories used by DeBusk (DeBusk et al. 2004) and then used the Agency for Healthcare Research and Quality (AHRQ) Prevention Quality Indicators guidelines to determine whether the rehospitalizations were potentially avoidable (Agency for Healthcare Research and Quality 2004). Both classification systems use hospital claim diagnoses to determine cause. Extensive information regarding the AHRQ Prevention Quality Indicators is available online (http://www.qualityindicators.ahrq.gov/pqi_overview.htm).
Analysis
Descriptive analyses were used to explore the characteristics of the population. We examined rehospitalization using a multilevel model for dichotomous dependent variables (implemented by the GLIMMIX procedure in SAS 9.2) and using a survival analysis approach for the time to rehospitalization (implemented using the PHREG procedure in SAS 9.2 for the Cox proportional hazards model). To address the nesting of the patient data within the agency and the agency within the geographic area, the relationship of the dichotomous outcome (rehospitalization: yes versus no) was first examined using the GLIMMIX procedure in SAS 9.2 The intraclass correlation of subjects nested within counties was very low (.00098), indicating that results using standard logistic regression (SAS LIFETEST) with the county code used as a fixed variable would be sufficient and in fact results were almost identical to those obtained from using the GLIMMIX procedure. Because of the large sample size, even very small effect sizes had very high significance levels; therefore, the relationship of the independent variables to the outcomes was judged by examining their effect sizes as well as their statistical significance levels.
Results
Description of the Analytic Sample
There were 74,580 patients who had an index hospitalization and thus constituted the analytic data set. These patients were, on average, 80.4 years old (SD = 9.6), most were women (61 percent, n = 45,429), white (83.5 percent, n = 62,255), or African American (13 percent, n = 9,775). Most lived in urban areas (83.5 percent) and with others (68 percent, n = 50,973), although a substantial number lived alone (32 percent, n = 23,607). Approximately one-third (35.5 percent, n = 26,463) were cared for by a hospital-based agency. Most of the patients were cared for by nonprofit agencies (65 percent, n = 48,178) followed by proprietary (29 percent, n = 21,893) or governmental (6 percent, n = 4509) agencies.
See Table S1 (supplementary data files) for detailed description of the sample.
The 30-day rehospitalization rate was 26 percent with 19,714 patients having a rehospitalization. Most of these patients (81 percent or 16,027) had only one rehospitalization within this time frame while 16.4 percent (n = 3,234) had two and the remainder (2.3 percent or 453) had three or more. The mean and median length of hospital stay were 6.5 (SD = 6.14) and 5 days, respectively. The mean, median, and range of time to rehospitalization were 13.6 days (SD = 8.2), 13 days, and 0–30 days, respectively.
Causes and Potentially Avoidable Hospitalizations
Using the DeBusk classification for all-cause and cardiac-related rehospitalization, the largest proportion of rehospitalizations was associated with a cardiac-related diagnosis (42 percent or 8,315). Following the AHRQ PQI measure for potentially avoidable hospitalizations, about one-third of the patients (34 percent, n = 6,514) had a primary diagnosis of heart failure for the rehospitalization. For secondary diagnoses, there were substantial numbers of patients with heart failure, hypertension, and chronic obstructive pulmonary disease (COPD) (32–55 percent), urinary tract infections (11.5 percent), and dehydration (10.6 percent). See Table 2 for the list of potentially avoidable hospitalizations.
Table 2.
Potentially Avoidable Hospitalizations for Home Health Care Patients with Heart Failure (N = 19,326)
| PQI | Primary Diagnosis (% of Total; N) | Secondary Diagnosis (% of Total; N) * |
|---|---|---|
| Heart failure (PQI 8) | 34% (6,514) | 55%(10,589) |
| Hypertension (PQI 7) | 0.14% (27) | 34%(6,588) |
| COPD (PQI 5) | 2.6% (494) | 32% (6,184) |
| Urinary tract | ||
| Infections (PQI 12) | 1.6% (312) | 11.5% (2,214) |
| Dehydration (PQI 10) | 2.2% (431) | 10.6% (2,041) |
| Bacterial pneumonia | ||
| (PQI 11) | 4.7% (913) | 6.8% (1,305) |
| Diabetes, long-term | ||
| (PQI 3) | 1.3% (244) | 6.4% (1,235) |
| Angina without procedure | ||
| (PQI 13) | 0.2% (47) | 4.4% (847) |
| Adult asthma (PQI 15) | 0.4% (85) | 4.2% (820) |
| Diabetes, uncontrolled | ||
| (PQI 14) | 0.12% (23) | 1.67% (311) |
| Diabetes, short-term (PQI 1) | (**) | 0.08% (15) |
| Lower-extremity | ||
| amputations (PQI 16) | 0% (0) | 0% (0) |
| Perforated appendix (PQI 2) | 0% (0) | (**) |
Totals exceed 100 percent since patients have more than one secondary diagnosis.
Omitted to ensure current CMS privacy guidelines are followed.
Multivariate Analyses
First, the relationship of the probability of rehospitalization with all variables identified as potentially important was examined using SAS LIFETEST. Within the context of the logistic regression, the county code of residence of the patient was also included; however, it did not attain statistical significance. There were significant and positive coefficients (higher likelihood of rehospitalization) for the following (in the order of larger Wald chi-square score indicating a greater role in explaining variations in the probability of hospitalization): total number of hospitalizations in the 6 months prior to the index hospital stay, guarded rehabilitation prognosis, age less than or equal to 85 years, overall poor prognosis, urinary continence (compared to incontinence), better cognitive functioning, receiving any physical therapy visits, female gender, receiving any home health aide visits, and being served by a non-hospital-based agency.
There were negative coefficients (less likelihood of rehospitalization) for the following variables: lower levels of dyspnea (compared to the reference group of dyspnea at rest), toileting (independence or some dependence compared to total dependence), grooming (independence or some dependence compared to total dependence), having only Medicare (versus being dually eligible), bathing (independence or some dependence compared to total dependence), having fewer symptoms associated with HF, oral medication management (independence or some dependence compared to total dependence), and having no comorbid diabetes. Odds ratios for rehospitalization and their 95 percent confidence intervals are reported in Table 3.
Table 3.
Contribution to the Variation in the Probability of Rehospitalization (0 = No, 1 = Yes) within 30 Days Using Logistic Regression with a Sample Size of 72,842
| Effect | Wald Chi-square % * | Point Estimate | 95% Wald Confidence Limits |
|---|---|---|---|
| Total number of hospitalizations in 6 months prior to index hospitalization | |||
| For each unit increase | 47.4 | 1.245 | (1.229, 1.261) |
| Visit intensity category | |||
| 0 = <1 visit/week | 33.7 | 0.552 | (0.513, 0.595) |
| 1 = 1–1.99 visits/week | 0.496 | (0.470, 0.522) | |
| 2 = 2–2.99 visits/week | 0.527 | (0.501, 0.554) | |
| 3 = 3–3.99 visits/week | 0.593 | (0.562, 0.626) | |
| 4 = ≥4 visits/week (Reference) | 1.000 | ||
| Dyspnea interfering with activity | |||
| 0 = no dyspnea | 13.3 | 0.553 | (0.507, 0.605) |
| 1 = when walking > 20 feet, climbing stairs | 0.649 | (0.603, 0.699) | |
| 2 = with moderate exertion | 0.699 | (0.652, 0.750) | |
| 3 = with minimal exertion | 0.784 | (0.730, 0.842) | |
| 4 = at rest (Reference) | 1.000 | ||
| Toileting | |||
| 0 = Independent | 4.78 | 0.765 | (0.677, 0.864) |
| 1 = Some dependence | 0.857 | (0.763, 0.963) | |
| 2 = Dependent (Reference) | 1.000 | ||
| Rehabilitation prognosis | |||
| 0 = Guarded | 2.80 | 1.128 | (1.081, 1.177) |
| 1 = Good (Reference) | 1.000 | ||
| Age | |||
| ≤85 | 1.89 | 1.131 | (1.088, 1.174) |
| >85 (Reference) | 1.000 | ||
| Grooming | |||
| 0 = Independent | 1.05 | 0.839 | (0.753, 0.934) |
| 1 = Some dependence | 0.922 | (0.834, 1.019) | |
| 2 = Dependent (Reference) | 1.000 | 1.000 | |
| Overall prognosis | |||
| 0 = poor | 0.75 | 1.145 | (1.08, 1.211) |
| 1 = good/fair (Reference) | 1.000 | ||
| Urinary incontinence | |||
| 0 = no | 0.65 | 1.085 | (1.044, 1.127) |
| 1 = yes (Reference) | 1.000 | ||
| Cognitive functioning | |||
| 0 = alert/oriented | 0.60 | 1.458 | (1.102, 1.928) |
| 1 = requires prompting | 1.415 | (1.070, 1.871) | |
| 2 = requires assistance | 1.357 | (1.024, 1.799) | |
| 3 = requires considerable asst | 1.031 | (0.765, 1.390) | |
| 4 = totally dependent (Reference) | 1.000 | ||
| Dual eligibility for Medicare and Medicaid | |||
| 0 = no | 0.545 | 0.917 | (0.880, 0.955) |
| 1 = yes (Reference) | 1.000 | ||
| Bathing | |||
| 0 = Independent | 0.51 | 0.785 | (0.691, 0.893) |
| 1 = Some dependence | 0.866 | (0.774, 0.970) | |
| 2 = Dependent (Reference) | 1.000 | ||
| Any physical therapy visits received | |||
| 0 = No | 0.47 | 1.085 | (1.045, 1.127) |
| 1 = Yes (Reference) | 1.000 | ||
| Severity of primary diagnosis | |||
| 0 = asymptomatic | 0.45 | 0.630 | (0.229, 1.738) |
| 1 = symptoms controlled | 0.825 | (0.704, 0.967) | |
| 2 = symptoms controlled w difficulty | 0.891 | (0.837, 0.948) | |
| 3 = symptoms poorly controlled | 0.924 | (0.867, 0.985) | |
| 4 = poorly controlled, hx of hospitalizations (Reference) | 1.000 | ||
| Oral medication management | |||
| 0 = Independent | 0.43 | 0.890 | (0.840, 0.944) |
| 1 = Some dependence | 0.927 | (0.882, 0.974) | |
| 2 = Dependent (Reference) | 1.000 | ||
| Gender | |||
| 0 = male | 0.43 | 1.081 | (1.043, 1.121) |
| 1 = female (Reference) | 1.000 | ||
| Comorbid diabetes | |||
| 0 = no | 0.26 | 0.944 | (0.909, 0.980) |
| 1 = yes (Reference) | 1.000 | ||
| Any home health aide visits received | |||
| 0 = No | 0.23 | 1.067 | (1.020, 1.115) |
| 1 = Yes (Reference) | 1.000 | ||
| Hospital-based agency | |||
| 0 = no | 0.17 | 1.046 | (1.009, 1.084) |
| 1 = yes (Reference) | 1.000 | ||
Expressed as a percent of the total model chi-square.
C statistic, a concordance measure of accuracy of model predictions = 0.640.
We then proceeded to examine time to rehospitalization with a Cox proportional hazard regression using SAS PROC PHREG. We report the findings of the time to rehospitalization, in the order of the greater Wald Chi-square statistic, which indicates shorter times to rehospitalization. The total number of hospitalizations in the 6 months prior to the index hospitalization, guarded rehabilitation prognosis, age less than or equal to 85, receiving any physical therapy visits, receiving any home health aide visits, male gender, poor overall prognosis, better cognitive functioning, urinary continence (as compared to incontinence), and receiving care from a non-hospital-based agency were associated with shorter time to rehospitalization. Greater times to rehospitalization were associated with lower levels of dyspnea (compared to the reference group of dyspnea at rest), toileting (independence or some dependence compared to total dependence), grooming (independence or some dependence compared to total dependence), bathing (independence or some dependence compared to total dependence), having fewer symptoms associated with HF, having only Medicare (versus being dually eligible), oral medication management (independence or some dependence compared to total dependence), and having no comorbid diabetes. Hazard ratios and their 95 percent confidence intervals are reported in Table 4. For both analyses, visit intensity category again had a mixed effect with nonlinear relationships with the outcomes.
Table 4.
Contribution to the Variation in the Time to Rehospitalization using Cox Proportional Hazards Model with a Sample Size of 72,842
| Effect | Wald Chi-square % * | Hazard Ratio | 95% Wald Confidence Limits |
|---|---|---|---|
| Total number of hospitalizations in 6 months prior to index hospitalization | |||
| For each unit change | 40.1 | 1.177 | (1.166, 1.188) |
| Visit intensity category | |||
| 0 = <1 visit/week | 31.1 | 0.567 | (0.532, 0.604) |
| 1 = 1–1.99 visits/week | 0.503 | (0.481, 0.527) | |
| 2 = 2–2.99 visits/week | 0.540 | (0.517, 0.536) | |
| 3 = 3–3.99 visits/week | 0.614 | (0.587, 0.643) | |
| 4 = ≥4 visits/week (Reference) | 1.000 | ||
| Dyspnea interfering with activity | |||
| 0 = no dyspnea | 12.1 | 0.596 | (0.554, 0.642) |
| 1 = when walking > 20 feet, Climbing stairs | 0.683 | (0.644, 0.724) | |
| 2 = with moderate exertion | 0.731 | (0.693, 0.772) | |
| 3 = with minimal exertion | 0.811 | (0.768, 0.858) | |
| 4 = at rest (Reference) | 1.000 | ||
| Toileting | |||
| 0 = Independent | 4.01 | 0.816 | (0.741, 0.898) |
| 1 = Some dependence | 0.908 | (0.830, 0.994) | |
| 2 = Dependent (Reference) | 1.000 | ||
| Rehabilitation prognosis | |||
| 0 = Guarded | 2.41 | 1.112 | (1.073, 1.153) |
| 1 = Good (Reference) | 1.000 | ||
| Age category | |||
| ≤85 | 1.57 | 1.113 | (1.078, 1.150) |
| >85 (Reference) | 1.000 | ||
| Any physical therapy visits received | |||
| 0 = No | 1.41 | 1.149 | (1.112, 1.187) |
| 1 = Yes (Reference) | 1.000 | ||
| Any home health aide visits received | |||
| 0 = No | 0.98 | 1.132 | (1.091, 1.175) |
| 1 = Yes (Reference) | 1.000 | ||
| Grooming | |||
| 0 = Independent | 0.90 | 0.866 | (0.795, 0.942) |
| 1 = Some dependence | 0.941 | (0.870, 1.017) | |
| 2 = Dependent (Reference) | 1.000 | 1.000 | |
| Gender | |||
| 0 = male | 0.63 | 1.079 | (1.047, 1.112) |
| 1 = female (Reference) | 1.000 | ||
| Overall prognosis | |||
| 0 = poor | 0.57 | 1.117 | (1.067, 1.168) |
| 1 = good/fair (Reference) | 1.000 | ||
| Bathing | |||
| 0 = Independent | 0.49 | 0.796 | (0.718, 0.882) |
| 1 = Some dependence | 0.876 | (0.802, 0.956) | |
| 2 = Dependent (Reference) | 1.000 | ||
| Severity of primary diagnosis | |||
| 0 = asymptomatic | 0.42 | 0.690 | (0.287, 1.659) |
| 1 = symptoms controlled | 0.856 | (0.746, 0.982) | |
| 2 = symptoms controlled w diff | 0.904 | (0.860, 0.951) | |
| 3 = symptoms poorly controlled | 0.939 | (0.892, 0.989) | |
| 4 = poorly controlled, hx of hospitalizations (Reference) | 1.000 | ||
| Cognitive functioning | |||
| 0 = alert/oriented | 0.39 | 1.292 | (1.029, 1.623) |
| 1 = requires prompting | 1.257 | (1.001, 1.578) | |
| 2 = requires assistance | 1.223 | (0.972, 1.539) | |
| 3 = requires considerable asst | 1.008 | (0.789, 1.287) | |
| 4 = totally dependent (Reference) | 1.000 | ||
| Dual eligibility for Medicare and Medicaid | |||
| 0 = no | 0.37 | 0.936 | (0.904, 0.968) |
| 1 = yes (Reference) | 1.000 | ||
| Oral medication management | |||
| 0 = Independent | 0.36 | 0.904 | (0.860, 0.949) |
| 1 = Some dependence | 0.939 | (0.901, 0.979) | |
| 2 = Dependent (Reference) | 1.000 | ||
| Urinary incontinence | |||
| 0 = no | 0.35 | 1.069 | (1.035, 1.105) |
| 1 = yes (Reference) | 1.000 | ||
| Comorbid diabetes | |||
| 0 = no | 0.17 | 0.957 | (0.927, 0.988) |
| 1 = yes (Reference) | 1.000 | ||
| Hospital-based agency | |||
| 0 = no | 0.11 | 1.036 | (1.006, 1.068) |
| 1 = yes (Reference) | 1.000 | ||
Expressed as a percent of the total model score chi-square.
Discussion
In summary, there was a substantial 30-day rehospitalization rate among these patients (26 percent), most of whom had a HF diagnosis (42 percent) and many rehospitalizations were considered potentially avoidable (34 percent for the primary diagnosis of HF). From the multivariate analyses, patient factors were the most influential variables with relatively little influence from the geographic and agency factors. Among the patient factors, the number of prior hospitalizations was the strongest factor within each model followed by dyspnea interfering with activity.
The rehospitalization rate of 26 percent found in this study falls between the national HF registry studies and other large studies that report 20–21 percent of patients having 30-day rehospitalization rates (Jencks, Williams, and Coleman 2009; Bueno et al. 2010) and the 29 percent rate from national risk-adjusted reports of hospitalization among Medicare home health care recipients. The Jencks et al. and risk-adjusted home health care reports include patients with all diagnoses and conditions versus a heart failure-specific population, suggesting that the HF-specific population is a “classic” condition for experiencing rehospitalization. Thus, a better understanding of and interventions that have an impact on patients with HF may also have an influence on patients with other chronic diseases and conditions (e.g., COPD) although more research would be needed on this.
The patient variables were the strongest factors associated with rehospitalization, regardless of whether the outcome was rehospitalization or time to rehospitalization. There were consistent findings between the models with only differences in the relative order of association with the outcome. The consistency of the results between the models indicates that the substantive influence of the patient variables on rehospitalization rates is where to focus practice and policy interventions.
The strongest factors predictive of rehospitalization were the number of prior hospital stays and dyspnea. Although there were other variables that met the statistical significance criteria, the coefficients and hazard ratios were more modest. Related to the number of prior hospital stays, past research has indicated that a greater number of hospital stays is associated with subsequent hospital admissions (Fonarow 2008; Jencks, Williams, and Coleman 2009). It is not clear whether this is a function of the patient's clinical condition (i.e., disease progression or the development of a new problem); physician provider behavior where a provider sends the patient to the hospital with the development of HF symptoms or new problems; patient preference for hospital care when health issues occur; home health care provider behavior that encourages patients to seek hospital care when symptoms occur; or, most likely, some combination of the above. As this was such a strong predictor of rehospitalization, home health care agencies would benefit from having this information as part of their identification of patients who may be a high risk for a rehospitalization. This may not be a challenge if the patient is “known” to the agency from past care episodes but can be difficult to determine for patients who are “new” to the agency. Regardless, the national focus on rehospitalization has identified how difficult the problem is to address. The current demonstration projects focused on the patient-centered medical home and transitional care models (Naylor et al. 2004; Holland et al. 2005; Konstam and Greenberg 2009; Parry et al. 2009) address some of these issues, although how the current home health care system will be integrated into these new models of care has yet to be determined. From a practice perspective, more research into what leads patients into a rehospitalization should inform interventions that may be effective in addressing this national priority.
The primary clinical variable associated with rehospitalization was dyspnea interfering with activity. As dyspnea is a cardinal symptom of HF exacerbation, higher levels of dyspnea interfering with activity would be expected to be associated with more likelihood of rehospitalization. The relationship between increasing levels of dyspnea interfering with activity and rehospitalization were consistent in both models and was not surprising. The etiology for dyspnea, however, is not straightforward as the dyspnea is likely to be influenced by both the disease process and deconditioning associated with inactivity. As well, home health care patients often have multiple diagnoses and conditions so that the dyspnea may be the result of other diagnoses (e.g., chronic lung disease). Our results for the potentially avoidable hospitalizations support this as 32 percent were identified as having a secondary diagnosis of COPD. Regardless of the etiology, identification of patients with dyspnea and clinical interventions to address dyspnea may be worth additional examination.
Visit intensity and its influence on rehospitalization as well as time to rehospitalization may be a result of the home health care provider judgment regarding patient needs where more visits are provided to patients who are more complex to manage (i.e., are more medically fragile, need more medication or self-management instruction or more frequent physical assessment). There is very little research on how home health care staff decide on visit frequency: in some agencies, the decisions are made by the frontline staff, whereas in other agencies the decisions are made at a supervisory level. There is some preliminary research that frontloading visits (providing the majority of the planned home health care visits earlier in the episode) are associated with lower rehospitalization rates for patients with HF in one study (Rogers, Perlic, and Madigan 2007), although additional research has not been done on this topic. Thus, the findings of the visit intensity association with longer time to rehospitalization may be a function of some agencies providing more visits earlier in the episode based on patient acuity, or patient need driving more visits for intensive monitoring and follow-up.
Among the geographic and agency factors, only hospital-based agencies were associated with time to rehospitalization and less likelihood of rehospitalization in 30 days. The hazard ratio was small but informative when considering that the patient factors are the most likely factors driving rehospitalization. Explanations for this finding are speculative as there is little research on agency differences but may be a function of closer communication with referring providers and more system level approaches (i.e., health system level disease management approaches) to managing HF care by hospital-based agencies. As health care reform measures consider such approaches as bundling payment for hospital and post-acute care, more research on how hospital-based agencies work within their hospital systems may inform practice and research. Our finding is in contrast to the findings of Brega, Jordan, and Schlenker (2003), who found that proprietary agencies had higher visit intensity and shorter lengths of stay whereas hospital-based agencies had shorter lengths of stay and somewhat shorter visit intensity. The samples were similar (HF as primary diagnosis in the present study while Brega et al. included HF or diabetes as the primary diagnoses) so the lack of effect in the present study is primarily attributed to the time difference (Brega's data collection was in 1998–2000, the same time that the prospective payment system was being implemented in home health care Medicare payment, while the present study used 2005 data). Access to home health care services is not a concern based on the 2010 Medicare Payment Advisory Commission report that indicates 99 percent of Medicare beneficiaries live in an area served by a home health care agency (Medicare Payment Advisory Commission 2010). However, based on the findings from the present study, the issues of concern are not access to home health care services but the persistent rates of rehospitalization. In some ways, the findings are not surprising as HF is a chronic and progressive disease that often requires hospital-level care for diuresis and medication titration. Although most of the factors identified with rehospitalization are not “actionable” per se, the findings do indicate that home health care agencies and referring providers might use the findings to identify the patients at highest risk for rehospitalization and target services to potentially reduce the rehospitalization rates among the highest risk patients. These targeted services might include telehealth, frontloading visits, prompt physician follow-up, patient education on self-management, and other evidence-based strategies (Jencks, Williams, and Coleman 2009; Bueno et al. 2010; Kane 2011). The extent to which these interventions are currently implemented in home health care is unknown but, based on the present rates of rehospitalization, there appears to be room for improvement in HF management in home health care and in coordination of care with physicians that may prevent or reduce the rehospitalization rate. It is clear that a “silo” approach where each type of provider focuses only on their own setting of care has not been successful in addressing rehospitalization rates. The extent to which the rehospitalizations were potentially avoidable needs additional research within home health care. Although there were many rehospitalizations that met the AHRQ criteria, it is not clear what interventions could be implemented within home health care to reduce these events.
For care coordination, recent policy changes as part of the 2010 Affordable Care Act may have a positive influence. Notably, a CMS policy change for Medicare home health care to be implemented in 2011 requires a face-to-face physician encounter within 90 days prior to or within 30 days following the start of home health care. This policy change requires the physician or other provider (physician assistant or nurse practitioner) to certify that the patient meets the homebound requirement and to indicate the patient-specific need for skilled services. For patients who have been in the hospital, a hospitalist may provide this certification. There is research by Wolff and colleagues (Wolff et al. 2009) reporting that more extensive physician involvement (through a process known as management and evaluation of the care plan) was associated with a higher likelihood of home health care patients being discharged from services and remaining at home (versus being discharged with a hospital stay). Thus, this policy change may improve care coordination between home health care staff and the ordering physician, which often has been anecdotally reported as a paper trail where the physician simply signs the paperwork versus true care coordination where the physician and home health care agency staff work together.
Another factor reported anecdotally as interfering with care coordination for home health care is the hospitalist-primary care physician relationship where the primary care physician may not have seen the patient following a hospital stay prior to the development of a medical problem. Depending on the health care system, the primary care physician may not have easy access to the hospital discharge summary from the hospitalist. If the patient develops symptoms of HF exacerbation or a new problem within a short time frame following the hospital discharge and prior to seeing the primary care physician, the primary care physician is understandably reluctant to provide additional home health care orders that would delay rehospitalization (i.e., changes in medication doses). Thus, there are system and policy issues interfering with care coordination that are outside the control of the home health care agency. There are, however, effective care management approaches that have been identified (as noted above) that can be used. Addressing this thorny and complex issue of rehospitalization will take concerted and coordinated effort.
There are a number of limitations to the study. First, we cannot compare those who used home health care with those HF patients who do not use home health care. Although our results for rehospitalization rates suggest our patients are representative of the larger HF population, we also recognize the complexity of the decision in how patients are admitted for a rehospitalization and that home health care patients are likely to be different (i.e., sicker, more proactive in seeking assistance at home). Second, we cannot claim that the variables identified are causally related to rehospitalization, although we do have associations that we think are worth additional exploration. We recommend instrumental variable (IV) analysis in future research to address these issues of endogeneity. Without such an approach, our estimates are likely to be biased and suggestive of causal relationships that may not be found with an IV approach. Third, there are remaining unknown influences among the variables used to predict rehospitalization, particularly visit intensity and type of provider that merits additional investigation. Finally, the use of clinical and administrative databases does not sufficiently represent all the variables of interest for the complex issue of rehospitalization. Additional variables such as the severity of illness during hospitalization or the use of HF-recommended medications are important in a better understanding of the phenomenon.
In conclusion, there are current policy and practice challenges to addressing the persistently high rates of rehospitalization among patients with HF. Health policy changes, both current and expected, may positively influence the rates, although there remains much uncertainty regarding the necessity of such care and for whom it is most beneficial.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: Funding for the study was provided by the National Heart, Lung and Blood Institute, National Institutes of Health, grant number R01HL085725-02, P.I. Madigan with co-investigators Gordon, Fortinsky, Koroukian, Pina, and Riggs.
Disclosures: None.
SUPPORTING INFORMATION
Additional supporting information may be found in the online version of this article:
Appendix SA1: Author Matrix.
Table S1: Demographic Description of Population.
Please note: Wiley-Blackwell is not responsible for the content or functionality of any supporting materials supplied by the authors. Any queries (other than missing material) should be directed to the corresponding author for the article.
References
- Agency for Healthcare Research and Quality. 2004. “AHRQ Prevention Quality Indicators Overview” [accessed on February 2, 2011]. Available at http://www.qualityindicators.ahrq.gov/pqi_overview.htm. [DOI] [PubMed]
- Andersen RM. “Revisiting the Behavioral Model and Access to Medical Care: Does It Matter?”. Journal of Health and Social Behavior. 1995;36(1):1–10. [PubMed] [Google Scholar]
- Brega AG, Jordan AK, Schlenker RE. “Practice Variations in Home Health Care”. Home Health Care Services Quarterly. 2003;22(3):41–64. doi: 10.1300/J027v22n03_03. [DOI] [PubMed] [Google Scholar]
- Bueno H, Ross JS, Wang Y, Chen J, Vidan MT, Normand SL, Curtis JP, Drye EE, Lichtman JH, Keenan PS, Kosiborod M, Krumholz HM. “Trends in Length of Stay and Short-Term Outcomes among Medicare Patients Hospitalized for Heart Failure, 1993–2006”. Journal of the American Medical Association. 2010;303(21):2141–7. doi: 10.1001/jama.2010.748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Medicare & Medicaid Services. 2009. “Chronic Condition Data Warehouse User Manual, Version 1.5” [accessed on January 27, 2011]. Available at http://ccwdata.org/downloads/CCWpercent20Userpercent20Manual.pdf. [PubMed]
- DeBusk RF, Miller NH, Parker KM, Bandura A, Kraemer HC, Cher DJ, West JA, Fowler MB, Greenwald G. “Care Management for Low-Risk Patients with Heart Failure: A Randomized, Controlled Trial”. Annals of Internal Medicine. 2004;141(8):606–13. doi: 10.7326/0003-4819-141-8-200410190-00008. [DOI] [PubMed] [Google Scholar]
- Fonarow GC. “Epidemiology and Risk Stratification in Acute Heart Failure”. American Heart Journal. 2008;155(2):200–7. doi: 10.1016/j.ahj.2006.10.043. [DOI] [PubMed] [Google Scholar]
- Fortinsky RH, Madigan EA, Sheehan TJ, Tullai-McGuinness S, Fenster JR. “Risk F for Hospitalization among Medicare Home Care Patients”. Western Journal of Nursing Research. 2006;28(8):902–17. doi: 10.1177/0193945906286810. [DOI] [PubMed] [Google Scholar]
- Hittle DF, Shaughnessy PW, Crisler KS, Powell MC, Richard AA, Stearns PM, Engle K. “A Study of Reliability and Burden of Home Health Assessment Using OASIS”. Home Health Care Services Quarterly. 2003;22(4):43–63. [PubMed] [Google Scholar]
- Holland R, Battersby J, Harvey I, Lenaghan E, Smith J, Hay L. “Systematic Review of Multidisciplinary Interventions in Heart Failure”. Heart. 2005;91(7):899–906. doi: 10.1136/hrt.2004.048389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jencks SF, Williams MV, Coleman EA. “Rehospitalizations among Patients in the Medicare Fee-for-Service Program”. New England Journal of Medicine. 2009;360(14):1418–28. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- Kane RL. “Finding the Right Level of Posthospital Care”. Journal of the American Medical Association. 2011;305(3):284–93. doi: 10.1001/jama.2010.2015. [DOI] [PubMed] [Google Scholar]
- Konstam MA, Greenberg B. “Transforming Health Care through the Medical Home: The Example of Heart Failure”. Journal of Cardiac Failure. 2009;15(9):736–8. doi: 10.1016/j.cardfail.2009.09.004. [DOI] [PubMed] [Google Scholar]
- Madigan EA, Fortinsky RH. “Interrater Reliability of the Outcomes and Assessment Information Set: Results from the Field”. The Gerontologist. 2004;44(5):689–92. doi: 10.1093/geront/44.5.689. [DOI] [PubMed] [Google Scholar]
- Medicare Payment Advisory Commission. 2010. “Home Health Care Services Payment System” [accessed on January 27, 2011]. Available at http://www.medpac.gov/documents/MedPAC_Payment_Basics_10_HHA.pdf.
- Mor V, Besdine RW. “Policy Options to Improve Discharge Planning and Reduce Rehospitalization”. Journal of the American Medical Association. 2011;305(3):302–3. doi: 10.1001/jama.2010.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naylor MD, Brooten DA, Campbell RL, Maislin G, McCauley KM, Schwartz JS. “Transitional Care of Older Adults Hospitalized with Heart Failure: A Randomized, Controlled Trial”. Journal of the American Geriatric Society. 2004;52(5):675–84. doi: 10.1111/j.1532-5415.2004.52202.x. [DOI] [PubMed] [Google Scholar]
- Ouslander JG, Lamb G, Perloe M, Givens JH, Kluge L, Rutland T, Atherly A, Saliba D. “Potentially Avoidable Hospitalizations of Nursing Home Residents: Frequency, Causes, and Costs”. Journal of the American Geriatrics Society. 2010;58(4):627–35. doi: 10.1111/j.1532-5415.2010.02768.x. [DOI] [PubMed] [Google Scholar]
- Parry C, Min SJ, Chugh A, Chalmers S, Coleman EA. “Further Application of the Care Transitions Intervention: Results of a Randomized Controlled Trial Conducted in a Fee-for-Service Setting”. Home Health Care Services Quarterly. 2009;28(2–3):84–99. doi: 10.1080/01621420903155924. [DOI] [PubMed] [Google Scholar]
- Rogers J, Perlic M, Madigan EA. “The Effect of Frontloading Visits on Patient Outcomes”. Home Healthcare Nurse. 2007;25(2):103–9. doi: 10.1097/00004045-200702000-00011. [DOI] [PubMed] [Google Scholar]
- Ross JS, Chen J, Lin Z, Bueno H, Curtis JP, Keenan PS, Normand SL, Schreiner G, Spertus JA, Vidán MT, Wang Y, Krumholz HM. “Recent National Trends in Readmission Rates after Heart Failure Hospitalization”. Circulation. Heart Failure. 2010;3(1):97–103. doi: 10.1161/CIRCHEARTFAILURE.109.885210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tullai-McGuinness S, Madigan EA, Fortinsky RH. “Validity Testing the Outcomes and Assessment Information Set (OASIS)”. Home Health Care Services Quarterly. 2009;28(1):45–57. doi: 10.1080/01621420802716206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolff JL, Meadow A, Weiss CO, Boyd CM, Leff B. “Medicare Home Health Patients’ Transitions through Acute and Post-Acute Settings”. Medical Care. 2008;46(11):1188–93. doi: 10.1097/MLR.0b013e31817d69d3. [DOI] [PubMed] [Google Scholar]
- Wolff JL, Meadow A, Boyd CM, Leff B. “Physician Evaluation and Management of Medicare Home Health Patients”. Medical Care. 2009;47(11):1147–55. doi: 10.1097/MLR.0b013e3181b58e30. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


