Abstract
Despite increasing evidence for an association between posttraumatic stress disorder (PTSD) and deliberate self-harm (DSH), few studies have examined the factors that moderate this association or the impact of co-occurring personality disorders among individuals with PTSD on DSH frequency. Given the high rates of co-occurrence between PTSD and two personality disorders of particular relevance to DSH, borderline personality disorder (BPD) and avoidant personality disorder (AVPD), this study examined the moderating role of these personality disorders in the association between PTSD and DSH frequency among a sample of substance use disorder patients (N=61). Patients completed structured clinical interviews assessing PTSD, BPD, and AVPD and a questionnaire assessing DSH. Results revealed more frequent DSH among patients with (vs. without) PTSD and provided evidence for the moderating role of AVPD in this association. Specifically, results revealed heightened levels of DSH only among PTSD patients with co-occurring AVPD. Findings are consistent with past research demonstrating that the presence of co-occurring AVPD among patients with other Axis I and II disorders is associated with worse outcomes, and highlight the importance of continuing to examine the moderating role of AVPD in the association between PTSD and a variety of health-risk behaviors.
Keywords: self-injury, axis II disorders, substance dependence, cocaine, comorbidity, emotional avoidance
1. Introduction
Posttraumatic stress disorder (PTSD) is an anxiety disorder characterized by the development and persistence of re-experiencing, avoidant, and hyperarousal symptoms following direct or indirect exposure to a traumatic event (Blake et al., 1990). PTSD is a serious clinical concern, associated with considerable functional impairment (Kessler and Frank, 1997), high rates of co-occurring psychiatric disorders (Kessler et al., 1995), and heightened levels of numerous self-destructive and health-compromising behaviors, including suicide attempts (Nepon et al., 2010) and illicit substance abuse (Brady et al., 2004). One particularly clinically-relevant behavior receiving increasing attention among patients with PTSD is deliberate self-harm (DSH), defined as the deliberate, direct destruction of body tissue without conscious suicidal intent (Chapman et al., 2006). Indeed, rates of DSH among individuals with PTSD exceed 50% (Zlotnick et al., 1999; Sacks et al., 2008; Dyer et al., 2009), and there is evidence to support the role of PTSD symptoms in the development and maintenance of this behavior (Harned et al., 2006; Bornovalova et al., 2011).
Despite evidence for elevated rates of DSH within PTSD, few studies have examined the subset of PTSD patients most at-risk for this behavior. In particular, little research has examined the moderating role of personality pathology in the association between PTSD and DSH or the specific co-occurring personality disorders that may increase the risk for DSH among individuals with PTSD. However, emerging research on the phenomenon of complex PTSD (a multifaceted syndrome encompassing both trauma-related symptoms and personality disturbance; Herman, 1992) suggests that the co-occurrence of PTSD and personality disorders may be especially relevant to DSH. Specifically, complex PTSD includes engagement in self-destructive behavior as a key feature (Herman, 1992; Dyer et al., 2009) and has been found to evidence stronger associations with DSH than PTSD (Dyer et al., 2009). Thus, this literature highlights the importance of examining the intersection of trauma-related difficulties and personality disorders in the risk for DSH.
Two personality disorders that warrant particular consideration in this regard are borderline personality disorder (BPD) and avoidant personality disorder (AVPD), both of which are common among patients with PTSD (Southwick et al., 1993; Bollinger et al., 2000) and considered relevant to DSH. Indeed, BPD is the disorder most often associated with DSH (Chapman et al., 2006), with as many as 70-75% of individuals with BPD reporting a history of DSH (Gunderson, 2001). Moreover, emerging evidence highlights the relevance of AVPD to DSH, with studies finding an association between AVPD symptoms and DSH among both non-clinical young adult (Klonsky et al., 2003) and incarcerated adult (Haines et al., 1995) samples.
The relevance of BPD and AVPD to DSH is further supported by theoretical literature on the pathogenesis of these disorders. Specifically, both BPD and AVPD are considered to be strongly linked to an intolerance of emotional distress and related difficulties regulating distress (Linehan, 1993; Taylor et al., 2004) – two of the mechanisms implicated in the development and maintenance of DSH (Chapman et al., 2006; Gratz et al., 2010). Furthermore, there is some evidence to suggest that the co-occurrence of these personality disorders among individuals with PTSD is associated with a number of negative outcomes and maladaptive behaviors (Heffernan and Cloitre, 2000; Miller and Resick, 2007), including suicidal and other health-risk behaviors (Connor et al., 2002). Although no studies have examined the extent to which these disorders moderate the association between PTSD and DSH in particular, recent findings that BPD pathology moderates the association between DSH and emotional responding (Gratz et al., 2010) highlight the importance of examining the moderating role of personality disorders in the association between DSH and other factors.
In considering the moderating roles of BPD and AVPD in the association between PTSD and DSH, one population that may be especially important to study is patients with substance use disorders (SUD). SUD patients have elevated rates of both PTSD and BPD compared to the general population (Trull et al., 2000; Brady et al., 2004), and PTSD-SUD co-occurrence has been found to be associated with greater impairment and worse outcomes (Najavits et al., 1999; Back et al., 2000). Furthermore, there is some evidence to suggest heightened risk for DSH among PTSD-SUD patients (compared to those with either disorder alone; Harned et al., 2006).
Thus, the goal of the present study was to examine the moderating roles of BPD and AVPD in the association between PTSD and DSH frequency among SUD patients. We hypothesized significant main effects of PTSD, BPD, and AVPD diagnostic status on DSH frequency, such that the frequency of DSH would be higher among SUD patients with (vs. without) these disorders. Furthermore, we hypothesized significant interactions between PTSD and both BPD and AVPD, such that PTSD patients with co-occurring BPD or AVPD would report more frequent DSH than those with PTSD or these personality disorders alone.
2. Method
2.1. Participants
Participants were inpatient residents in a drug and alcohol abuse treatment center in Northeast Washington D.C. Data for this study were collected as part of a larger study focused on the functional relationship between PTSD and crack/cocaine use. To be eligible for the larger study, participants were required to: 1) be 18 to 65 years of age; 2) meet criteria for crack/cocaine dependence; 3) have been in residential treatment for at least 72 hours (to limit the interference of withdrawal symptoms on responding); 4) exhibit no significant cognitive impairment; and 5) not meet criteria for a current manic episode or psychotic disorder.
Based on these criteria, 61 participants (54% male) were included in the study. Participants were primarily African-American (97%), low-income (< $10,000 income = 79%), unemployed (89%), and single (75%), and ranged in age from 20 to 58 (mean age = 44.45±7.05).
2.2. Measures
2.2.1. Posttraumatic stress disorder
The Clinician-Administered PTSD Scale (CAPS; Blake et al., 1990), a widely-used structured PTSD diagnostic interview (Weathers et al., 2001), was used to diagnose PTSD. It assesses the frequency and intensity of the 17 DSM-IV PTSD symptoms (plus eight associated symptoms). The CAPS has adequate inter-rater reliability (0.92–0.99), internal consistency (0.73–0.85), and convergent validity with other established measures of PTSD (Weathers et al., 2001). In addition, the robust psychometric properties of the CAPS have been supported in a variety of combat and civilian (including inpatient SUD) samples, as well as across different racial/ethnic groups (Weathers et al., 2001). The CAPS was administered by trained interviewers, and all interviews were reviewed by the principal investigator (MTT).
2.2.2. Co-occurring borderline and avoidant personality disorders
Participants were also interviewed using the BPD and AVPD modules of the Diagnostic Interview for DSM-IV Personality Disorders (DIPD-IV; Zanarini et al., 1996). The DIPD-IV has demonstrated good reliability (Zanarini et al., 2000), with inter-rater kappa coefficients ranging from 0.68 to 0.73 and a test-retest kappa coefficient of 0.69 to 0.74. Interviews were administered by post-baccalaureate or doctoral-level clinical assessors trained to reliability with the investigators (KLG and MTT). All interviews were reviewed by the investigators, with diagnoses confirmed in consensus meetings. Of note, a discrepancy was evident in only three cases.
2.2.3. Deliberate self-harm
The Deliberate Self-Harm Inventory (DSHI; Gratz, 2001) is a 17-item self-report questionnaire that assesses lifetime history of various aspects of DSH, including frequency, duration, and type of DSH behavior (including cutting, burning, carving, bone-breaking, etc.). The DSHI asks participants whether and how often they have engaged in a variety of behaviors intentionally and without intending to kill themselves, and specifically instructs participants to exclude behaviors they engaged in with the sole purpose of delivering substances. The DSHI has demonstrated adequate test-retest reliability and construct, discriminant, and convergent validity among undergraduate student and patient samples (Gratz, 2001; Fliege et al., 2006). Consistent with past research using this measure (e.g., Gratz, 2001; Cerutti et al., 2011), a continuous variable measuring frequency of reported DSH was created by summing participants’ scores on the frequency questions. Internal consistency in this sample was adequate (α = 0.67).
2.2.4. Depression and anxiety symptoms
The depression and anxiety subscales of the Depression Anxiety Stress Scales (DASS; Lovibond and Lovibond, 1995) were also administered. The DASS is a self-report questionnaire designed to differentiate between the core symptoms of depression, anxiety, and stress. The DASS has been found to have good test-retest reliability (subscale rs > 0.70; Brown et al., 1997) and adequate construct and discriminant validity, as evidenced by significant (and differential) associations with other established self-report and diagnostic assessments of depression and anxiety (Lovibond and Lovibond, 1995; Brown et al., 1997). The factor structure of the DASS has also been supported in clinical samples (Brown et al., 1997). The depression and anxiety subscales were examined as potential covariates in analyses. Their internal consistency in the current sample was excellent (αs = 0.87).
2.2.5. Substance use severity
Consistent with past studies of inpatient substance users (Lejuez et al., 2007; Bornovalova et al., 2009), past year severity of alcohol and drug use was assessed through a self-report measure of the frequency of use of a variety of substances (e.g., alcohol, cannabis, cocaine, stimulants, opiates) in the past year. Modeled after other well-established, empirically-supported measures (e.g., the Alcohol Use Disorders Identification Test; Saunders et al., 1993), this measure characterizes frequency of use in a manner consistent with the SUD module of the Structured Clinical Interview for DSM-IV (SCID-IV; First et al., 1996). Responses are summed to create an overall score representing past year substance use. In support of the measure's construct validity, scores on this measure have been found to be associated with a number of constructs theoretically- and empirically-linked to SUD, including impulsivity (Lejuez et al., 2007), emotion dysregulation (Bornovalova et al., 2009), and PTSD symptoms (Bornovalova et al., 2009). Further, scores on this measure demonstrate convergence with SCID-IV SUD diagnoses in associations with relevant outcomes (Lejuez et al., 2007). This variable was examined as a potential covariate in subsequent analyses. Internal consistency in the current study was adequate (α = 0.73).
2.2.6. Demographics
All participants completed a demographics questionnaire assessing age, gender, racial/ethnic background, marital status, annual income, and employment status.
2.3. Procedure
All study procedures received approval by the institution's Institutional Review Board. Eligible participants were informed that involvement in the study was voluntary and refusal to participate would not affect their treatment status. Participants who provided written informed consent were interviewed with the CAPS and DIPD-IV, and then completed the self-report measures described above. Participants were provided with a $30 gift card in exchange for their participation.
3. Results
3.1. Variable transformations
The raw scores for DSH frequency were highly positively skewed (4.32) and kurtotic (21.98), requiring transformation (Tabachnick and Fidell, 2007). Following logarithmic transformation, scores on this variable approximated a normal distribution (skewness = 1.61, kurtosis = 1.71).
3.2. Preliminary analyses
Within the present sample, 30% (n=18) of participants reported a history of DSH1, 49.2% (n=30) met criteria for current PTSD, 39.3% (n=24) met criteria for BPD, and 34.4% (n=21) met criteria for AVPD.
A series of correlation analyses were conducted to explore associations between DSH frequency and demographic factors (i.e., age, gender, income, marital status [married vs. not], and employment status [unemployed vs. employed]), depression and anxiety symptom severity, past year substance use severity, and psychotropic medication use (presence vs. absence) in order to identify potential covariates for the analysis of covariance (ANCOVA). DSH frequency was significantly positively associated with depression symptom severity (r = 0.30, p < 0.05) and anxiety symptom severity (r = 0.36, p < 0.01), and differed significantly across gender (t [59] = 2.01, p < 0.05), with women reporting more frequent DSH than men. No other associations were significant (rs < 0.22, ps > 0.10). Given evidence of substantial overlap between depression and anxiety symptom severity (r = 0.78) and high multicollinearity in the model with both included (as evidenced by squared multiple correlations [SMCs] of greater than 0.67 for both depression and anxiety; Tabachnick and Fidell, 2007), only gender and anxiety symptom severity were included as covariates in the primary ANCOVA (resulting in acceptable SMCs for all covariates)2.
3.3. Primary analyses
Prior to examining the interactive effects of PTSD, BPD, and AVPD on DSH frequency, we conducted a series of one-tailed independent t-tests to examine differences in DSH frequency as a function of PTSD, BPD, and AVPD status. Power analyses revealed power of > 0.60 to detect a medium-sized effect (d = 0.50) for PTSD and BPD status and power of 0.58 to detect a medium-sized effect for AVPD status (with N=61 and αs = 0.05). As expected, DSH frequency differed significantly across both PTSD (t [59] = -1.71, d = 0.44, p < 0.05) and AVPD (t [59] = -2.20, d = 0.57, p < 0.05) status, such that participants with (vs. without) these disorders reported more frequent DSH. Surprisingly, however, there were no significant differences in DSH frequency as a function of BPD status (despite some overlap between a BPD diagnosis and DSH, in the form of one BPD criterion encompassing a history of suicidal and/or DSH behavior; t [59] = -0.09, d = 0.02, p > 0.10).
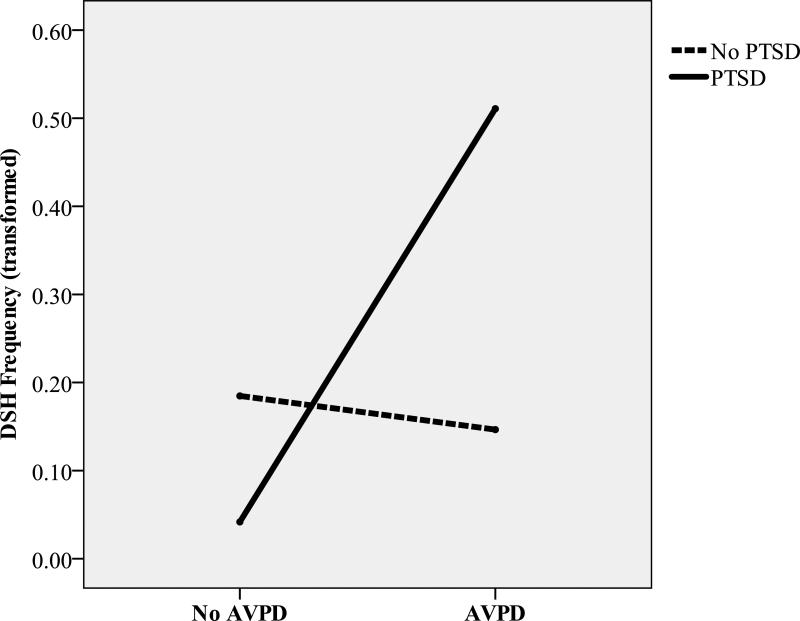
Next, to explore the interactive effect of PTSD, BPD, and AVPD on DSH frequency, we conducted a 2 (PTSD vs. no PTSD) × 2 (BPD vs. no BPD) × 2 (AVPD vs. no AVPD) ANCOVA (controlling for gender and anxiety symptom severity) with DSH frequency serving as the dependent variable (see Table 1). Power analyses revealed power of 0.48 to detect a mediumsized effect within this model (α = 0.05). Although no significant main effects were found for PTSD, BPD, or AVPD status (when controlling for the other variables in the model), results did reveal a significant interaction between PTSD and AVPD (see Table 1 and Figure 1). Post-hoc independent t-tests (using adjusted means) were conducted to explore the nature of the interaction. Results demonstrated that participants with co-occurring PTSD and AVPD reported significantly more frequent DSH than all other groups of participants, ts (dfs range from 19 to 36) > 1.80, ps < 0.05. No other interactions were significant3.
Table 1.
ANCOVA Examining the Interactive Effect of PTSD, AVPD, and BPD on Frequency of DSH.
| F (1, 51) | p | Partial η2 | Observed Power | |
|---|---|---|---|---|
| Gender | 1.95 | 0.17 | 0.04 | 0.28 |
| Anxiety Symptom Severity | 6.08* | 0.02 | 0.11 | 0.68 |
| PTSD | 0.72 | 0.40 | 0.01 | 0.13 |
| AVPD | 3.12† | 0.08 | 0.06 | 0.41 |
| BPD | 3.14† | 0.08 | 0.06 | 0.41 |
| PTSD × AVPD | 4.49* | 0.04 | 0.08 | 0.55 |
| PTSD × BPD | 0.01 | 0.95 | 0.00 | 0.05 |
| AVPD × BPD | 0.28 | 0.60 | 0.01 | 0.08 |
| PTSD × AVPD × BPD | 0.60 | 0.44 | 0.01 | 0.12 |
p < 0.05.
p < 0.10.
Figure 1.
Interactive Effect of PTSD and AVPD on Lifetime DSH Frequency.
Of note, findings remain the same when controlling for depression symptom severity (in addition to gender and anxiety symptom severity), as well as when controlling for anxiety symptom severity only, with only the PTSD × AVPD interaction emerging as significant in these analyses, Fs > 4.16, ηp2s > 0.07, ps < 0.05.
4. Discussion
Despite emerging evidence for an association between PTSD and DSH (Sacks et al., 2008; Bornovalova et al., 2011), few studies have examined the factors that moderate this association or the impact of co-occurring personality disorders among individuals with PTSD on DSH frequency. Given the high rates of co-occurrence between PTSD and two personality disorders of particular relevance to DSH (BPD and AVPD), this study sought to examine the moderating role of these personality disorders in the association between PTSD and DSH frequency among a sample of SUD patients. The results of this study add to the literature on the association between PTSD and DSH, providing evidence for more frequent DSH among patients with versus without PTSD. These results are consistent with past findings of elevated rates of DSH among individuals with PTSD (Zlotnick et al., 1999; Sacks et al., 2008) and extend the research in this area to a particularly relevant at-risk population of SUD patients.
Our results also extend this area of research by highlighting a particular subset of PTSD patients at-risk for DSH. Specifically, findings of more frequent DSH only among PTSD patients with AVPD suggest that PTSD is associated with greater DSH only in the context of cooccurring AVPD. These findings are consistent with, and expand upon, past research demonstrating that the presence of AVPD among patients with other Axis I and II conditions is associated with greater dysfunction and worse outcomes (Feske et al., 1996; Zanarini et al., 2005), and suggest that the co-occurrence of this disorder with PTSD in particular may increase the risk for maladaptive emotion regulation strategies such as DSH (Linehan, 1993). Specifically, given the centrality of emotional avoidance and nonacceptance to AVPD (Taylor et al., 2004), the co-occurrence of this disorder among patients with PTSD could exacerbate the avoidant tendencies already present within PTSD (Morina et al., 2008) and increase the reliance on avoidant emotion regulation strategies. Findings of the relevance of co-occurring AVPD-PTSD to DSH are also consistent with literature emphasizing the centrality of AVPD features to complex PTSD (Cloitre et al., 2002).
Interestingly, we did not find support for an association between BPD and DSH frequency among the participants in this sample. Although this finding is contrary to past findings of a robust association between BPD and DSH (Chapman et al., 2006; Gratz et al., 2010), it is not without support in the literature, as past studies have likewise failed to find a significant association between DSH and co-occurring BPD among patients with Axis I disorders (Joyce et al., 2010). It is possible that BPD may be less relevant to DSH among populations already characterized by high levels of emotion dysregulation, such as SUD patients (Fox et al., 2007). Within such populations, other factors may emerge as more relevant to DSH, such as a tendency toward avoidance or emotional nonacceptance in particular. Findings of the relative relevance of AVPD versus BPD to DSH within this sample are also consistent with recent findings that BPD is not associated with DSH when controlling for harm avoidance (the primary temperament dimension underlying AVPD; Joyce et al., 2003, 2010).
Several limitations warrant consideration. First, given our unique sample of primarily low-SES, African-American SUD patients, findings from this study may not generalize to other clinical populations, particularly non-SUD populations. Indeed, the interrelations examined here may differ in unknown ways between patients with and without SUD, and it is possible that our findings are specific to PTSD-SUD patients in particular. Thus, findings require replication across a more diverse group of PTSD patients. Additionally, our relatively small sample size may have limited our statistical power and ability to detect between-group differences. Although findings that all differences accompanied by medium-to-large effect sizes in this sample were statistically significant suggest that we were not underpowered to detect meaningful differences, replication of these findings in larger PTSD samples with and without co-occurring AVPD and BPD is needed. Furthermore, although we examined the moderating roles of BPD and AVPD in the association between PTSD and DSH, we did not assess for other co-occurring Axis I and II disorders. However, evidence suggests that mood, anxiety, and antisocial personality disorders co-occur at relatively high rates with PTSD (Kessler et al., 1995; Goodwin and Hamilton, 2003) and are associated with DSH (Garrison et al., 1993; Zlotnick et al., 1999; Gollust et al., 2008; Joyce et al., 2010). Thus, future research should examine the influence of these disorders on the relationships examined here. Nonetheless, findings that the interaction between PTSD and AVPD on DSH frequency remained significant when controlling for depression and anxiety symptoms provide some support for the specificity of our findings above and beyond depression and anxiety in general.
Future research is also needed to examine the mechanisms underlying DSH among PTSD patients with AVPD, including emotional avoidance, distress intolerance, thought suppression, and emotion regulation difficulties (all of which are considered relevant to both AVPD and DSH; Taylor et al., 2004; Chapman et al., 2006; Gratz et al., 2010). Indeed, although the relative ease with which co-occurring AVPD can be assessed and identified in both clinical and research settings increases the clinical significance of the present findings, research is needed to examine the specific mechanisms underlying the association between AVPD and DSH, as well as the interactive effect of PTSD and AVPD on DSH. Findings of the relevance of particular emotional or cognitive mechanisms to the association between PTSD-AVPD and DSH would facilitate the development of targeted interventions for this population.
Despite limitations, the results of this study add to the growing literature on DSH in PTSD, providing evidence for heightened levels of DSH only among PTSD patients with AVPD. These findings have important clinical implications, highlighting the clinical utility of assessing for co-occurring personality disorders (particularly AVPD) among PTSD-SUD patients. Incorporating such assessments into standard intake evaluations for SUD treatment programs may facilitate the identification of a subset of PTSD-SUD patients at greater risk for DSH. These findings also suggest potential targets for intervention within this population. Specifically, given the proposed centrality of emotional avoidance and nonacceptance to both AVPD and DSH, findings highlight the potential utility of mindfulness- and acceptance-based interventions for DSH within this population (e.g., Dialectical Behavior Therapy [Linehan, 1993] and Acceptance and Commitment Therapy [Hayes et al., 1999]). Such interventions are considered to be particularly useful for decreasing avoidance and promoting acceptance, facilitating an open and non-evaluative stance toward internal experiences that may enable clients to remain present with their emotions. Likewise, given the role of emotion regulation difficulties in AVPD, findings suggest the benefits of teaching self-harming PTSD-SUD patients more adaptive ways of modulating emotional arousal. In particular, interventions aimed at teaching healthy, nonavoidant strategies for modulating the intensity and/or duration of emotions may decrease the reliance on maladaptive regulation strategies such as DSH.
Acknowledgments
This research was supported by R03 DA023001 from the National Institute on Drug Abuse, awarded to the second author.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errorsmaybe discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The rate of DSH within this sample was previously reported in Gratz and Tull (2010).
Anxiety was selected over depression due to its stronger zero-order correlation with DSH frequency, as well as its greater relevance to PTSD and AVPD.
Comparable findings were obtained when using the non-transformed DSH frequency variable (including a significant PTSD × AVPD interaction, F[1,51] = 8.53, ηp2 = 0.14, p < 0.01), with the exception of significant main effects of both BPD and AVPD on DSH (Fs[1,51]≥ 4.62, ps < 0.05, ηp2s = 0.10 and 0.08, respectively).
References
- Back S, Dansky BS, Coffey SF, Saladin ME, Sonne S, Brady KT. Cocaine dependence with and without posttraumatic stress disorder: A comparison of substance use, trauma history and psychiatric comorbidity. The American Journal on Addictions. 2000;9:51–62. doi: 10.1080/10550490050172227. [DOI] [PubMed] [Google Scholar]
- Blake DD, Weathers FW, Nagy L, Kaloupek DG, Klauminzer G, Charney DS, Keane TM. The Clinician Administered PTSD Scale. Boston VA Health Care System; Boston: 1990. [Google Scholar]
- Bollinger AR, Riggs DS, Blake DD, Ruzek JI. Prevalence of personality disorders among combat veterans with posttraumatic stress disorder. Journal of Traumatic Stress. 2000;13:255–270. doi: 10.1023/A:1007706727869. [DOI] [PubMed] [Google Scholar]
- Bornovalova M, Ouimette P, Crawford AV, Levy R. Testing gender effects on the mechanisms explaining the association between post-traumatic stress symptoms and substance use frequency. Addictive Behaviors. 2009;34:685–692. doi: 10.1016/j.addbeh.2009.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bornovalova MA, Tull MT, Gratz KL, Levy R, Lejuez CW. Extending models of deliberate self-harm and suicide attempts to substance users: Exploring the roles of childhood abuse, posttraumatic stress, and difficulties controlling impulsive behavior when distressed. Psychological Trauma: Theory, Research, Practice, and Policy. 2011;3:349–359. [Google Scholar]
- Brady KT, Back SE, Coffey SF. Substance abuse and posttraumatic stress disorder. Current Directions in Psychological Science. 2004;13:206–209. [Google Scholar]
- Brown TA, Chorpita BF, Korotitsch W, Barlow DH. Psychometric properties of the Depression Anxiety Stress Scales (DASS) in clinical samples. Behaviour Research and Therapy. 1997;35:79–89. doi: 10.1016/s0005-7967(96)00068-x. [DOI] [PubMed] [Google Scholar]
- Cerutti R, Manca M, Presaghi F, Gratz KL. Prevalence and clinical correlates of deliberate self-harm among a community sample of Italian adolescents. Journal of Adolescence. 2011;34:337–347. doi: 10.1016/j.adolescence.2010.04.004. [DOI] [PubMed] [Google Scholar]
- Chapman AL, Gratz KL, Brown MZ. Solving the puzzle of deliberate self-harm: The experiential avoidance model. Behaviour Research and Therapy. 2006;44:371–394. doi: 10.1016/j.brat.2005.03.005. [DOI] [PubMed] [Google Scholar]
- Cloitre M, Koenen KC, Gratz KL, Jakupcak M. Differential diagnosis of PTSD in women. In: Kimerling R, Ouimette PC, Wolfe J, editors. Gender and Posttraumatic Stress Disorder: Clinical, Research, and Program-Level Applications. Guilford Press; New York: 2002. pp. 117–149. [Google Scholar]
- Connor KM, Davidson JRT, Hughes DC, Swartz MS, Blazer DG, George LK. The impact of borderline personality disorder on post-traumatic stress in the community: A study of health status, health utilization, and functioning. Comprehensive Psychiatry. 2002;43:41–48. doi: 10.1053/comp.2002.29846. [DOI] [PubMed] [Google Scholar]
- Dyer KW, Dorahy MJ, Hamilton G, Corry M, Shannon M, MacSherry A, McRobert G, Elder R, McElhill B. Anger, aggression, and self-harm in PTSD and complex PTSD. Journal of Clinical Psychology. 2009;65:1099–1114. doi: 10.1002/jclp.20619. [DOI] [PubMed] [Google Scholar]
- Feske U, Perry KJ, Chambless DL, Renneberg B, Goldstein AJ. Avoidant personality disorder as a predictor for treatment outcome among generalized social phobics. Journal of Personality Disorders. 1996;10:174–184. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders – patient edition (SCID-I/P, Version 2.0) New York State Psychiatric Institute; New York: 1996. [Google Scholar]
- Fliege H, Kocalevent R, Walter OB, Beck S, Gratz KL, Gutierrez P, Klapp BF. Three assessment tools for deliberate self-harm and suicide behavior: Evaluation and psychopathological correlates. Journal of Psychosomatic Research. 2006;61:113–121. doi: 10.1016/j.jpsychores.2005.10.006. [DOI] [PubMed] [Google Scholar]
- Fox HC, Axelrod SR, Paliwal PP, Sleeper JJ, Sinha RR. Difficulties in emotion regulation and impulse control during cocaine abstinence. Drug and Alcohol Dependence. 2007;89:298–301. doi: 10.1016/j.drugalcdep.2006.12.026. [DOI] [PubMed] [Google Scholar]
- Garrison CZ, Addy CL, McKeown RE, Cuffe SP. Nonsuicidal physically self-damaging acts in adolescents. Journal of Child and Family Studies. 1993;2:339–352. [Google Scholar]
- Gollust S, Eisenberg D, Golberstein E. Prevalence and correlates of self-injury among university students. Journal of American College Health. 2008;56:491–498. doi: 10.3200/JACH.56.5.491-498. [DOI] [PubMed] [Google Scholar]
- Goodwin RD, Hamilton SP. Lifetime comorbidity of antisocial personality disorder and anxiety disorders among adults in the community. Psychiatry Research. 2003;117:159–166. doi: 10.1016/s0165-1781(02)00320-7. [DOI] [PubMed] [Google Scholar]
- Gratz KL. Measurement of deliberate self-harm: Preliminary data on the Deliberate Self-Harm Inventory. Journal of Psychopathology and Behavioral Assessment. 2001;23:253–263. [Google Scholar]
- Gratz KL, Breetz A, Tull MT. The moderating role of borderline personality in the relationships between deliberate self-harm and emotion-related factors. Personality and Mental Health. 2010;4:96–107. [Google Scholar]
- Gratz KL, Tull MT. The relationship between emotion dysregulation and deliberate self-harm among inpatients with substance use disorders. Cognitive Therapy and Research. 2010;34:544–553. doi: 10.1007/s10608-009-9268-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gunderson JG. Borderline Personality Disorder: A Clinical Guide. American Psychiatric Association; Washington, D.C.: 2001. [Google Scholar]
- Haines J, Williams CL, Brain KL. The psychopathology of incarcerated self-mutilators. The Canadian Journal of Psychiatry. 1995;40:514–522. doi: 10.1177/070674379504000903. [DOI] [PubMed] [Google Scholar]
- Harned MS, Najavits LM, Weiss RD. Self-harm and suicidal behavior in women with comorbid PTSD and substance dependence. The American Journal on Addictions. 2006;15:392–395. doi: 10.1080/10550490600860387. [DOI] [PubMed] [Google Scholar]
- Hayes SC, Strosahl K, Wilson KG. Acceptance and Commitment Therapy: An Experiential Approach to Behavior Change. Guilford Press; New York: 1999. [Google Scholar]
- Heffernan K, Cloitre M. A comparison of posttraumatic stress disorder with and without borderline personality disorder among women with a history of childhood sexual abuse: Etiological and clinical characteristics. Journal of Nervous and Mental Disease. 2000;188:589–595. doi: 10.1097/00005053-200009000-00005. [DOI] [PubMed] [Google Scholar]
- Herman JL. Complex PTSD: A syndrome in survivors of prolonged and repeated trauma. Journal of Traumatic Stress. 1992;3:377–391. [Google Scholar]
- Joyce PR, Light KJ, Rowe SL, Cloninger CR, Kennedy MA. Self-mutilation and suicide attempts: Relationships to bipolar disorder, borderline personality disorder, temperament and character. Australian and New Zealand Journal of Psychiatry. 2010;44:250–257. doi: 10.3109/00048670903487159. [DOI] [PubMed] [Google Scholar]
- Joyce PR, McKenzie JM, Luty SE, Mulder RT, Carter JD, Sullivan PF, Cloninger CR. Temperament, childhood environment and psychopathology as risk factors for avoidant and borderline personality disorders. Australian and New Zealand Journal of Psychiatry. 2003;37:756–764. doi: 10.1080/j.1440-1614.2003.01263.x. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Frank RG. The impact of psychiatric disorders on work loss days. Psychological Medicine. 1997;27:861–873. doi: 10.1017/s0033291797004807. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry. 1995;52:1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- Klonsky ED, Oltmanns TF, Turkheimer E. Deliberate self-harm in a nonclinical population: Prevalence and psychological correlates. American Journal of Psychiatry. 2003;160:1501–1508. doi: 10.1176/appi.ajp.160.8.1501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lejuez CW, Bornovalova MA, Reynolds EK, Curtin JJ, Daughters SB. Risk factors in the relationship between gender and crack/cocaine. Experimental and Clinical Psychopharmacology. 2007;15:165–175. doi: 10.1037/1064-1297.15.2.165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linehan MM. Cognitive-Behavioral Treatment of Borderline Personality Disorder. Guilford Press; New York: 1993. [Google Scholar]
- Lovibond SH, Lovibond PF. Manual for the Depression Anxiety Stress Scales. 2nd Edition The Psychology Foundation of Australia; Sydney: 1995. [Google Scholar]
- Miller MW, Resick PA. Internalizing and externalizing subtypes in female sexual assault survivors: Implications for the understanding of complex PTSD. Behavior Therapy. 2007;38:58–71. doi: 10.1016/j.beth.2006.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morina N, Stangier U, Risch A. Experiential avoidance in civilian war survivors with current versus recovered posttraumatic stress disorder: A pilot study. Behaviour Change. 2008;25:15–22. [Google Scholar]
- Najavits LM, Weiss RD, Shaw SR. A clinical profile of women with posttraumatic stress disorder and substance dependence. Psychology of Addictive Behaviors. 1999;13:98–104. [Google Scholar]
- Nepon J, Belik S, Bolton J, Sareen J. The relationship between anxiety disorders and suicide attempts: Findings from the National Epidemiologic Survey on Alcohol and Related Conditions. Depression and Anxiety. 2010;27:791–798. doi: 10.1002/da.20674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sacks MB, Flood AM, Dennis MF, Hertzberg MA, Beckham JC. Self-mutilative behaviors in male veterans with posttraumatic stress disorder. Journal of Psychiatric Research. 2008;42:487–494. doi: 10.1016/j.jpsychires.2007.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, De la Fuente JR, Grant M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on early detection of persons with harmful alcohol consumption. Addiction. 1993;88:791–803. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- Southwick SM, Yehuda R, Giller EL. Personality disorders in treatment-seeking combat veterans with posttraumatic stress disorder. American Journal of Psychiatry. 1993;150:1020–1023. doi: 10.1176/ajp.150.7.1020. [DOI] [PubMed] [Google Scholar]
- Tabachnick BG, Fidell LS. Using Multivariate Statistics. 5th ed. Allyn and Bacon; Boston: 2007. [Google Scholar]
- Taylor CT, Laposa JM, Alden LE. Is avoidant personality disorder more than just social avoidance? Journal of Personality Disorders. 2004;18:571–594. doi: 10.1521/pedi.18.6.571.54792. [DOI] [PubMed] [Google Scholar]
- Trull TJ, Sher KJ, Minks-Brown C, Durbin J, Burr R. Borderline personality disorder and substance use disorders: A review and integration. Clinical Psychology Review. 2000;20:235–253. doi: 10.1016/s0272-7358(99)00028-8. [DOI] [PubMed] [Google Scholar]
- Weathers FW, Keane TM, Davidson JRT. Clinician-administered PTSD scale: A review of the first ten years of research. Depression and Anxiety. 2001;13:132–156. doi: 10.1002/da.1029. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR, Hennen J, Reich B, Silk KR. The McLean Study of Adult Development (MSAD): Overview and implications of the first six years of prospective follow-up. Journal of Personality Disorders. 2005;19:505–523. doi: 10.1521/pedi.2005.19.5.505. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR, Sickel AE, Young L. Diagnostic Interview for DSM-IV Personality Disorders. McLean Hospital; Boston: 1996. Unpublished measure. [Google Scholar]
- Zanarini MC, Skodol AE, Bender D, Dolan R, Sanislow CA, Schaefer E, Morey LC, Grilo CM, Shea MT, McGlashan TH, Gunderson JG. The Collaborative Longitudinal Personality Disorders Study II: Reliability of axis I and axis II diagnosis. Journal of Personality Disorders. 2000;14:291–299. doi: 10.1521/pedi.2000.14.4.291. [DOI] [PubMed] [Google Scholar]
- Zlotnick C, Mattia JI, Zimmerman M. Clinical correlates of self-mutilation in a sample of general psychiatric patients. Journal of Nervous and Mental Disease. 1999;187:296–301. doi: 10.1097/00005053-199905000-00005. [DOI] [PubMed] [Google Scholar]