Abstract
Objective
To determine whether ethnic group differences in glycated haemoglobin (HbA1c) changed over a 5-year period in people on medication for type 2 diabetes.
Design
Open cohort in 2004–9.
Setting
Electronic records of 100 of the 101 general practices in two inner London boroughs.
Participants
People aged 35 to 74 years on medication for type 2 diabetes.
Main outcome measures
Mean HbA1c and proportion with HbA1c controlled to ≤7.5%.
Results
In this cohort of 24,111 people, 22% were White, 58% South Asian and 17% Black African/Caribbean. From 2004 to 2009 mean HbA1c improved from 8.2% to 7.8% for White, from 8.5% to 8.0% for Black African/Caribbean and from 8.5% to 8.0% for South Asian people. The proportion with HbA1c controlled to 7.5% or less, increased from 44% to 56% in White, 38% to 53% in Black African/Caribbean and 34% to 48% in South Asian people. Ethnic group and social deprivation were independently associated with HbA1c. South Asian and Black African/Caribbean people were treated more intensively than White people.
Conclusion
HbA1c control improved for all ethnic groups between 2004–9. However, South Asian and Black African/Caribbean people had persistently worse control despite more intensive treatment and significantly more improvement than White people. Higher social deprivation was independently associated with worse control.
Introduction
Type 2 diabetes currently affects 2 million people, 4% of the UK population and reduces life expectancy by 10 years with concomitant social inequalities in mortality.1 Among those under 55 years, the poorest 20% of the UK population have twice the prevalence of the richest 20%.2 Type 2 diabetes develops a decade earlier and is four times more prevalent in South Asian people, who have more complications and increased mortality compared with White people.3–5 These social differences are associated with obesity and raised HbA1c.2 National strategy aims to reduce health inequalities by improved diabetes care including target HbA1c levels.6
In 2004, two major UK initiatives were introduced to improve quality of care. The most deprived areas were designated as ‘spearhead’ boroughs for additional support and the Quality and Outcomes Framework (QoF) provided financial incentives for general practitioners to improve clinical management, including a diabetes target HbA1c of 7.5% (58 mmol/mol) or less.7,8 Since 2004, the QoF has reported national reductions in HbA1c in association with increasing numbers of people with diabetes and increasing intensity of treatment.9–12 However, the disparity between higher levels of HbA1c in South Asian and Black African/Caribbeans compared to White people showed no improvement over time either in the UK or among Black and ethnic minority groups in the USA.13–16 In addition, there have been local financial and organizational incentives in the study area to improve diabetes care over the last 5 years. Practices in socially deprived areas or serving South Asian and Black African/Caribbean communities will find it more difficult to achieve QoF targets and these ethnic and social disparities will impact on health outcomes.17
This is the first UK study to describe the independent influence of both ethnic and social group on HbA1c levels in people with type 2 diabetes routinely cared for by general practitioners over five years.
Methods
This study was located in Tower Hamlets and Newham, two inner London ‘spearhead’ boroughs whose 440,000 residents are the most ethnically diverse and socially deprived in England and Wales. Some 350 general practitioners in 101 practices are contracted to provide care for this population by Tower Hamlets and Newham NHS primary care trusts (PCTs). Nationally, these PCTs rank in the top 10% for cardiovascular mortality and diabetes prevalence and are in the lowest 10% of HbA1c control.18 In these areas, 40% of the population are Bangladeshi, Indian or Pakistani and 10% are Black African/Caribbean.
The sample was drawn from all general practices in the two PCTs, all of whom use the same web-enabled computer system (EMIS Web) for their electronic medical records and pre-specified codes for recording data from which anonymized data was accessed (www.emis-online.com). All prescribed diabetes medication for patients in the community is recorded by general practitioners.
We used an open cohort, including both those who left or joined the practice or newly developed diabetes in the period. Patients registered with the practice from 2004–9 were included if they had a Read code for type 2 diabetes and had been prescribed at least one diabetes treatment during this period and were aged 35 to 69 years in 2004. Thus people with type 2 diabetes aged 36–70 yrs were included in 2005, with a sequentially ageing cohort so that people with type 2 diabetes were included if aged 40–74 years in 2009. People under 35 years were excluded to reduce misclassification with type 1 diabetes,19 and the over 75's because more intensive treatment is often precluded by polypharmacy and other considerations.20
Patients only contributed information each year that they received a treatment prescription. For years without a diabetes treatment we could not ascertain whether they were on diet alone, or were on treatment but had not been issued a treatment prescription or whether they had in fact left the practice.
Individual self-reported ethnicity was recorded in the electronic medical record using the 2001 UK Census categories. These groups were collapsed into four ethnic groups; White (British, Irish, other White), South Asian (Bangladeshi, Indian, Pakistani, other Asian, mixed Asian), Black African/Caribbean (African, Caribbean, Black British, mixed Black), and Other (any other recorded ethnic group). We acknowledge that broad categorization limits further identification of ethnic differences but is used to enable comparison with existing studies. Social deprivation was measured using the Townsend score which includes unemployment, car and home ownership and household overcrowding derived from the UK Census by linkage of geographic lower level superoutput area (approximately 150 households) to the patients postcode at their home address.21
Body Mass Index (BMI) and serum cholesterol were estimated using the latest recording between 2007 and 2009. Smoking status (smoker/non-smoker) was the latest recording at any time. The latest HbA1c value within each annual 12-month period was recorded. Variables were marked as missing if omitted or the value was outside a pre-specified inclusion boundary. Patients were grouped into three exclusive treatment categories each year, based upon the diabetes medication they were prescribed during the year; ‘Metformin only’ if only Metformin was prescribed during the year; ‘Combined oral’ if during the year the patient was prescribed any other hypoglycaemic medication except insulin, either alone or in combination with Metformin, or ‘Insulin’ if prescribed only insulin or insulin in combination with any other medication during the year.
Two outcome measures were used, based upon the latest HbA1c value recorded in each year; mean HbA1c and the proportion of patients with HbA1c ‘controlled’ to ≤7.5% (58 mmol/mol). Data were accessed in August 2010.
Statistical Analysis
Analysis was performed using Stata 11.2 (StatCorp www.stata.com). Demographic statistics were calculated for each ethnic group and social deprivation categorized using Townsend score quintile.
Data were structured with variation at four levels; the lowest level was year, level 2 was patient, level 3 was practice, level 4 was PCT. A linear multilevel model using the first three levels was used to estimate HbA1c to generate unbiased hypothesis tests and confidence intervals.22 Variables were selected for inclusion using a 5% significance level and Collett's variable selection method.23 Models were compared using likelihood ratio tests.22 Townsend score was a continuous measure in the model. An ethnicity*year interaction variable was added to the model to indicate whether the difference in HbA1c between ethnic groups changed over time. An ethnicity*Townsend interaction assessed the relationship between ethnicity and social deprivation. To estimate the proportion with controlled HbA1c, an adjusted logistic multilevel model was constructed using the same combination of variables as the linear HbA1c model. “Other” ethnic groups were not included as they were few and heterogeneous.
Results
Data were obtained from 100 of the 101 general practices. One practice declined access. Diabetes age-standardized prevalence (European standard population) in 2004 was 5.9/100 and in 2009 7.3/100. Between 2004 and 2009 there were 37,297 people with a Read code for type 2 diabetes. Diabetes treatment was recorded in one or more years in 31,697, (85%) and the final sample consisted of 24,111, (76%) who satisfied the age inclusion criteria. Self-reported ethnicity was recorded in 23,483, (97%) of whom 5,206, (22%) were White, 13,633, (58%) South Asian, 3,923, (17%) Black African/Caribbean and 721, (3%) other ethnic groups.
Townsend score was recorded in 23,995, (>99% patients), higher scores indicating more deprivation. Only 2% of patients fell in the two least deprived Townsend groups and the three least deprived groups were combined. Patients were categorized as; ‘Least deprivation’ if their Townsend score was less than 3.93 (N = 4,900, 20%), ‘High deprivation’ if their score was above 6.75 (N = 7,341, 31%) and ‘Medium deprivation’ (11,754, 49%) otherwise. There was a higher proportion of South Asians in the ‘High deprivation’ group. Blood pressure was recorded in 98% of the cohort, BMI 95% and cholesterol 95%. The proportion of patients with HbA1c recorded increased every year; 79% of patients had an HbA1c value recorded in 2004 and 87% of patients had an HbA1c record in 2009.
Table 1 describes the characteristics of people with and without HbA1c records for the entire five year cohort in whom recording by ethnic and social group was similar. Table 2 shows the demographic variables for the entire five year cohort. Of the total sample over the 5-year period 27% were on ‘Metformin Only’, 50% on ‘Combined oral’ and 23% on ‘Insulin’. In the least deprivation group 51% had HbA1c controlled, compared to 45% in the high deprivation group.
Table 1.
Proportion of each category with an HbA1c value recorded 2004–9
| Variable | Category | Proportion with HbA1c value | Mean with HbA1c record | Mean without HbA1c record |
|---|---|---|---|---|
| Age in years | – | – | 53.4 | 53.0 |
| Serum cholesterol | – | – | 4.1 | 4.3 |
| BMI | – | – | 29.6 | 29.7 |
| Ethnicity | White | 85% | – | – |
| S Asian | 88% | – | – | |
| Black | 87% | – | – | |
| Social deprivation | Least | 88% | – | – |
| Medium | 87% | – | – | |
| High | 86% | – | – | |
| Treatment | Metformin Only | 85% | – | – |
| Other hypoglycaemic | 88% | – | – | |
| Insulin | 86% | – | – | |
| Sex | Female | 87% | – | – |
| Male | 86% | – | – | |
| Overall | – | 87% | – | – |
Table 2.
Demographic and clinical characteristics by ethnicity and Townsend category 2004–9
| Variable | Category | All | Ethnicity | Townsend category | |||||
|---|---|---|---|---|---|---|---|---|---|
| White | S Asian | Black | Least | Medium | High | ||||
| N | – | – | 24,111 | 5,206 | 13,633 | 3,923 | 4,900 | 11,754 | 7,341 |
| Demographic variables | Age | – | 52.6 | 54.7 | 51.7 | 53.1 | 52.4 | 52.7 | 52.6 |
| Male | – | 53% | 58% | 52% | 49% | 56% | 53% | 51% | |
| Townsend score | – | 5.5 | 5.5 | 5.5 | 5.5 | 2.7 | 5.3 | 7.6 | |
| Townsend category | Least | 20% | 20% | 20% | 20% | – | – | – | |
| Medium | 49% | 51% | 47% | 52% | – | – | – | ||
| High | 31% | 29% | 33% | 28% | – | – | – | ||
| Clinical variables | HbA1c% | – | 8.1 | 7.9 | 8.1 | 8.1 | 8.0 | 8.1 | 8.1 |
| Controlled HbA1c | HbA1c ≤ 7.5% ≤58mmol/mol | 47% | 52% | 45% | 49% | 51% | 47% | 45% | |
| BMI | – | 29.5 | 33.3 | 27.8 | 30.8 | 29.6 | 29.7 | 29.1 | |
| Serum cholesterol | – | 4.2 | 4.3 | 4.1 | 4.4 | 4.3 | 4.2 | 4.1 | |
| Smoker | 15% | 26% | 13% | 9% | 11% | 15% | 18% | ||
| Treatment | Metformin only | 27% | 30% | 25% | 27% | 29% | 26% | 26% | |
| Combined oral | 50% | 42% | 54% | 48% | 49% | 50% | 51% | ||
| Insulin | 23% | 27% | 21% | 25% | 21% | 24% | 23% | ||
From 2004 to 2009 there was little change in the proportion of patients on each treatment; 26% of patients were on ‘Metformin Only’ in 2004, compared to 29% in 2009. 52% of patients were on ‘Combined oral’ in 2004 compared to 48% in 2009. 23% of patients were on Insulin in both 2004 and 2009. White people (69%), were less likely to be on intensive diabetes treatment (either ‘Combined oral’ or ‘Insulin’) than South Asian (75%) and Black African/Caribbean people (73%) but South Asian people were less likely to be on insulin (21%), than White people (27%). A chi-squared test indicated these treatment differences were significant (P < 0.001).
Between 2004 and 2009, unadjusted mean HbA1c for White people declined by 0.4% from 8.2% to 7.8%; for South Asian and Black African/Caribbean people it declined by 0.5% from 8.5% to 8.0%. Similarly, the proportion of people with HbA1c controlled to 7.5% or less, increased by 12% in White people (from 44% in 2004 to 56% in 2009), by 14% in South Asian people (from 34% to 48%) and by 15% in Black African/Caribbean people (from 38% to 53%).
Tables 3 and Appendix 1 (available at http://jrsm.rsmjournals.com/lookup/suppl/doi:10.1258/jrsm.2012.110289/-/DC1) show the parameter estimates from the multilevel models used to derive adjusted HbA1c mean and HbA1c control outcomes. PCT was dropped from the model as it was not significant (P = 0.095). There was significant evidence to justify inclusion of age, gender, year, Townsend score, serum cholesterol, smoking status, ethnic group and treatment in both models. BMI did not significantly influence HbA1c (P = 0.227) but was retained in both models as a variable of interest. The ethnicity*year interaction was significant in both models indicating that the difference between ethnicities in mean HbA1c and HbA1c control changed between 2004 and 2009. There was no interaction between ethnicity and social deprivation (P = 0.475). Ethnic group was more strongly associated with HbA1c than social deprivation with regression estimates of 0.36 and 0.32 for South Asian and Black ethnic groups compared to 0.02 for Townsend score.
Table 3.
Predictors of HbA1c using a linear multilevel regression model
| Variable | Category | HbA1c Estimate | 95% CI | Category P value | Variable P value |
|---|---|---|---|---|---|
| Age | – | −0.02 | (−0.02, −0.01) | – | <0.001 |
| Townsend | – | 0.02 | (0.01, 0.03) | – | <0.001 |
| Serum cholesterol | – | 0.23 | (0.22, 0.25) | – | <0.001 |
| BMI | – | −0.002 | (−0.005, 0.001) | – | 0.227 |
| Year | 2004 (ref) | − | − | – | <0.001 |
| 2005 | −0.17 | (−0.25, −0.1) | <0.001 | ||
| 2006 | −0.33 | (−0.4, −0.26) | <0.001 | ||
| 2007 | −0.28 | (−0.35, −0.21) | <0.001 | ||
| 2008 | −0.49 | (−0.56, −0.42) | <0.001 | ||
| 2009 | −0.42 | (−0.49, −0.35) | <0.001 | ||
| Ethnicity | White (ref) | − | − | – | <0.001 |
| S Asian | 0.36 | (0.27, 0.44) | <0.001 | ||
| Black | 0.32 | (0.22, 0.42) | <0.001 | ||
| Treatment | Metformin Only (ref) | − | − | – | <0.001 |
| Combined oral | 0.42 | (0.39, 0.45) | <0.001 | ||
| Insulin | 1.05 | (1.01, 1.09) | <0.001 | ||
| Sex | Female (ref) | − | − | – | <0.001 |
| Male | 0.11 | (0.07, 0.15) | <0.001 | ||
| Smoking status | Non–Smoker (ref) | − | − | – | <0.001 |
| Smoker | 0.18 | (0.13, 0.24) | <0.001 | ||
| Ethnicity*Year | S Asian*2009 | −0.11 | (−0.19, −0.03) | 0.007 | <0.001 |
| Black*2009 | −0.20 | (−0.3, −0.09) | <0.001 |
In this adjusted analysis, men, smokers and those with high deprivation had higher HbA1c and lower odds of controlled HbA1c. Increased treatment intensity ‘Combined oral’ or ‘Insulin’ treatment were associated with a higher mean HbA1c, 0.4% and 1.1% respectively, and lower probability of controlled HbA1c relative to ‘Metformin only’ treatment.
In 2004, mean HbA1c was significantly lower in White people relative to South Asian people; difference = 0.36%, P < 0.001 and Black African/Caribbean people; difference = 0.32%, P < 0.001. Similarly in 2004, HbA1c controlled to 7.5% or less was more likely in White people than South Asian people (OR 2.1, 95% CI: 1.8, 2.5) or Black African/Caribbean people (OR 1.7, 95% CI: 1.4, 2.1).
The ethnicity*year interaction (Table 3) shows that from 2004 to 2009 the difference in mean HbA1c between White and Black African/Caribbean people decreased significantly by 0.2% (P < 0.001) from 0.32% to 0.12%. In addition, the odds of a White person having controlled HbA1c relative to a Black African/Caribbean person was significantly reduced to 1.3. The difference in mean HbA1c between White and South Asian people also decreased significantly by 0.11% (P = 0.007) from 0.36% to 0.25%. However, the odds of a White patient having controlled HbA1c in 2009 relative to a South Asian patient was not significantly different to the odds in 2004 (P = 0.118).
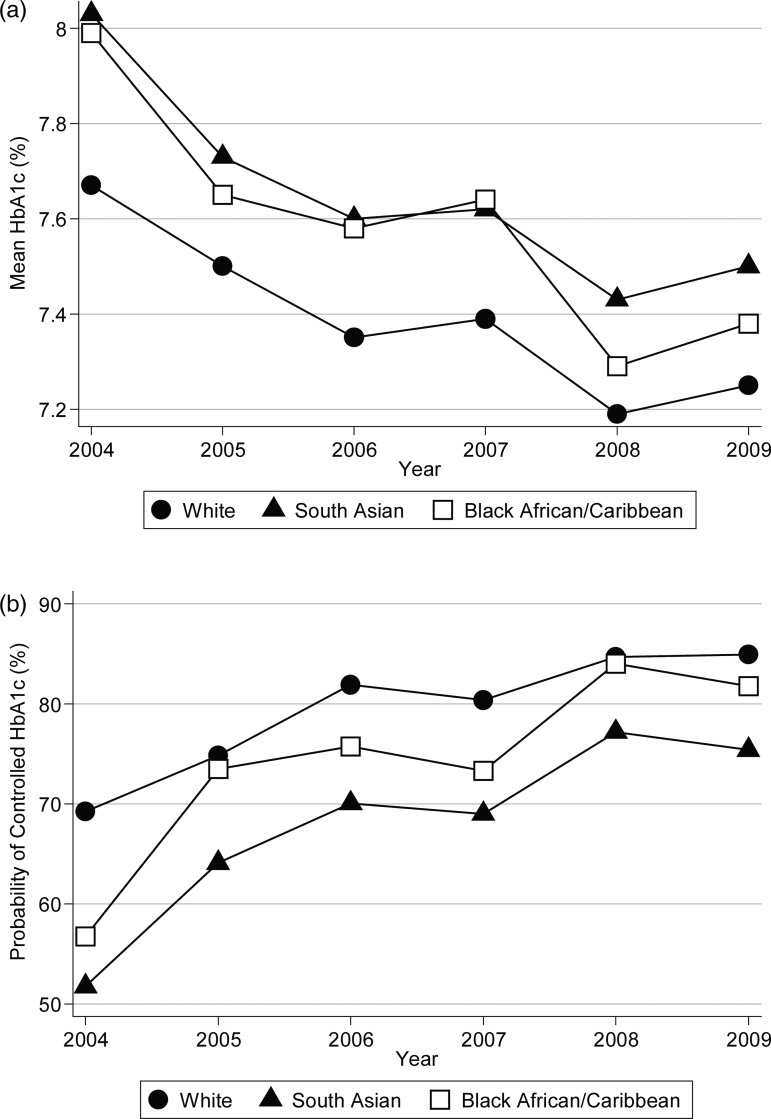
Illustrative graphs in Figure 1 show the expected mean HbA1c and probability of having HbA1c controlled each year by ethnic group (derived for a non-smoking male on ‘Metformin only’ using a mean age of 53 years and serum cholesterol 4mmol/l). The graphs show a reduction in HbA1c for all ethnic groups since 2004, most marked in earlier years, and a small reduction in the difference in mean HbA1c and HbA1c control between White and other ethnic groups.
Figure 1.
Estimated mean HbA1c (a) and probability of controlled HbA1c(b) by ethnic group 2004–9
Social deprivation remained independently associated with HbA1c after adjustment for other factors including ethnic group. As an illustrative example, Table 4A shows the expected mean HbA1c and probability of having controlled HbA1c for a white non-smoking male patient in 2009 on ‘Metformin only’ in the least, medium and high social deprivation groups. The table shows that high social deprivation increases mean HbA1c by 0.1% (1 mmol/mol) and reduces the probability of having controlled HbA1c by 3% relative to being in the least deprivation group. Similarly Table 4B shows the difference in expected mean HbA1c and probability of having HbA1c control between each ethnic group. Table 4C shows the relationship between HbA1c, ethnic and social group. The non-significance of the ethnicity*Townsend interaction means an increase in deprivation effects similar changes in the HbA1c levels of each ethnic group.
Table 4a.
Predicted mean and controlled HbA1c in 2009 for each Townsend category
| Townsend score category | Townsend category mean | Mean HbA1c % | Probability of controlled HbA1c |
|---|---|---|---|
| Least deprivation | 2.7 | 7.19 | 87% |
| Medium deprivation | 5.3 | 7.24 | 85% |
| High deprivation | 7.6 | 7.29 | 84% |
Table 4b.
Predicted mean HbA1c and controlled HbA1c in 2009 for each ethnic group
| Ethnicity | Mean HbA1c % | Probability of controlled HbA1c |
|---|---|---|
| White | 7.25 | 84.9% |
| S Asian | 7.5 | 75.4% |
| Black | 7.38 | 81.8% |
Table 4c.
Predicted mean HbA1c for each ethnic and social group in 2009
| Ethnicity | Least deprivation | Medium deprivation | High deprivation |
|---|---|---|---|
| White | 7.19 | 7.24 | 7.29 |
| S Asian | 7.43 | 7.48 | 7.53 |
| Black | 7.31 | 7.36 | 7.41 |
There was concern that the sample age range selectively excluded more South Asian people with diabetes aged 18-34 years. Therefore the HbA1c model was rerun including all 2612 patients of these ages of whom 11% were White, 76% South Asian, 13% Black African/Caribbean and 17% were least deprivation, 47% medium and 36% high deprivation. The statistical models indicated ethnic group (P < 0.001) and social group (P < 0.001) were still significant predictors of HbA1c and the difference in mean HbA1c between ethnic groups still decreased significantly (P < 0.001) over the study period.
Discussion
Our findings are consistent with those nationally, showing that HbA1c control has improved in all ethnic groups since 2004, with slower improvement in more recent years.12 Our study confirmed that HbA1c control to 7.5% or less is persistently worse in South Asian and Black African/Caribbean people than in White people despite more intensive treatment in these ethnic groups.
Our study is the first to consider both socio-economic status and ethnic group concurrently, and we found both ethnicity and social deprivation had an independent effect on HbA1c, ethnicity having the stronger effect. Our findings support previous reports of social deprivation associated with poor HbA1c control.14,24,25
Treatment
Although other studies have shown improvement in HbA1c, ours is the first study to demonstrate an improvement in the relative difference between ethnic groups. However, in absolute terms these reductions of 0.1% in HbA1c were small and regression to the mean, or changes in case-mix may be responsible. Treatment intensity did not substantially alter during the period, though we were unable to ascertain dose changes which may have increased.
Like other studies, we found a lower proportion of South Asian people (21%) were prescribed insulin, than White people (27%). However, more intensive treatments in the form of either ‘Combined oral’ or ‘Insulin’, were used by a higher proportion of South Asian (75%) and Black African/Caribbean people (73%), than White people (69%). HbA1c values worsen in all treatment groups over time and insulin does not reduce HbA1c more than oral agents in the first three years of treatment.28 Our results do not support the explanation that South Asian people have higher HbA1c because they receive less drug treatment than other groups, though lower insulin use may contribute to poorer control in the longer term.
Case-mix
Our open cohort design is unusual and cross sectional analyses at two points in time have been more commonly used to describe provider performance. Our design, adjusted for age, provides more information than cross-sectional studies about patient experience with type 2 diabetes over time. Person years at risk would have further enhanced the analysis, but accurate dates of leaving the cohort were not available.
Changes in the case-mix of the diabetic population over time are likely to have contributed to reductions and ethnic differentials in HbA1c. The number of people with diabetes increased from 11,080 in 2004 to 20,935 in 2009, and those people with newer onset diabetes are likely to have lower HbA1c and be more susceptible to treatment. However, this may have been offset by worsening HbA1c control over time.28 Though recording of HbA1c increased over time, there is no reason why this should reduce HbA1c in favour of South Asian and Black African/Caribbean patients.
Our study accurately describes changes in HbA1c over time by ethnic group and social deprivation but is unable to elucidate the reasons for these changes or for persistent differences between ethnic groups. This would require experimental designs including diabetes of comparable duration and trials to determine differential treatment efficacy.
Conclusion
In recent years the improvements in HbA1c have levelled off but ethnic group differences have persisted. Similar findings have been reported in the USA.13,26,27 In the UK, these persistent differences may be relevant to clinicians working in socially or ethnically diverse areas, who may find it harder to achieve target levels and the contingent financial rewards.
Strengths of our study include data from 99% of all practices including almost every person aged 35–69 years known to have type 2 diabetes in the two primary care trust areas. Completeness and quality of recording of self-reported ethnicity has been supported by local incentives,29 and the availability of small area Census data for social deprivation has made it possible to consider both variables concurrently with a high degree of accuracy. The ethnic diversity of the population enhanced group comparisons further. For all other confounding variables used, less than 5% of data was missing.
In conclusion, this study provides evidence over a five year period that HbA1c improved in all ethnic and social groups, albeit levelling off more recently. Differences between White and other ethnic groups persisted despite a small reduction between them. Ethnic group and, to a lesser extent, social deprivation were both independently associated with HbA1c.
DECLARATIONS
Competing interests
None declared
Funding
The study was funded by The Health Foundation
Ethical approval
was not necessary as the study was based upon routinely extracted anonymised data
Guarantor
JR
Contributorship
G.D. James designed the analysis and undertook data extraction, analysis and interpretation, P. Baker undertook the literature review All authors contributed to the drafting of the paper and development of core ideas J. Robson and S. Hull were principal investigators who initiated and supervised the study. We acknowledge the contribution of S. Shajahan who managed the project and the east London Clinical Effectiveness Group and east London general practitioners for access to data
Reviewer
Mark Ashworth
References
- 1.Morrish NJ, Wang SL, Stevens LK, Fuller JH, Keen H Mortality and causes of death in the WHO multinational study of vascular disease in diabetes. Diabetologia 2001;44 Suppl 2:S14–21 [DOI] [PubMed] [Google Scholar]
- 2.National Clinical Audit Support Programme. National diabetes audit executive summary 2008/9. London: NHS National Information Centre; 2009 [Google Scholar]
- 3.Fischbacher CM, Bhopal R, Steiner M, Morris AD, Chalmers J Is there equity of service delivery and intermediate outcomes in South Asians with type 2 diabetes? Analysis of DARTS database and summary of UK publications. J Public Health (Oxf) 2009;31:239–49 [DOI] [PubMed] [Google Scholar]
- 4.Khaw KT, Wareham N, Luben R, Bingham S, Oakes S, Welch A, et al. Glycated haemoglobin, diabetes, and mortality in men in Norfolk cohort of european prospective investigation of cancer and nutrition (EPIC-Norfolk). BMJ 2001;322:15–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bellary S, O'Hare JP, Raymond NT, Gumber A, Mughal S, Szczepura A, et al. Enhanced diabetes care to patients of south Asian ethnic origin (the United Kingdom Asian Diabetes Study): a cluster randomised controlled trial. Lancet 2008;371:1769–76 [DOI] [PubMed] [Google Scholar]
- 6.NHS Diabetes. 2010. Health equality strands. http://diabetes.flanders.seegreen.eu/our_work_areas/inequalities/health_inequalities_resources/
- 7.Alshamsan R, Majeed A, Ashworth M, Car J, Millett C Impact of pay for performance on inequalities in health care: systematic review. J Health Serv Res Policy 2010;15:178–84 [DOI] [PubMed] [Google Scholar]
- 8.Quality and Outcomes Framework data tables: PCT diabetes 2009/10 The NHS Information Centre 2011. http://www.ic.nhs.uk/statistics-and-data-collections/supporting-information/audits-and-performance/the-quality-and-outcomes-framework/qof-2009-10/data-tables/pct-level-data-tables (last accessed 15 February 2012)
- 9.Millett C, Saxena S, Ng A, Mainous A 3rd, Majeed A Socio-economic status, ethnicity and diabetes management: an analysis of time trends using the health survey for England. J Public Health (Oxf) 2007;29:413–9 [DOI] [PubMed] [Google Scholar]
- 10.Calvert M, Shankar A, McManus RJ, Lester H, Freemantle N Effect of the quality and outcomes framework on diabetes care in the United Kingdom: retrospective cohort study. BMJ 2009;338:b1870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Oluwatowoju I, Abu E, Wild SH, Byrne CD Improvements in glycaemic control and cholesterol concentrations associated with the Quality and Outcomes Framework: a regional 2-year audit of diabetes care in the UK. Diabetic Medicine 2010;27:354–9 [DOI] [PubMed] [Google Scholar]
- 12.Verma A, Birger R, Bhatt H, Murray J, Millett C, Saxena S, et al. Ethnic disparities in diabetes management: a 10-year population-based repeated cross-sectional study in UK primary care. J Public Health (Oxf) 2010;32:250–8 [DOI] [PubMed] [Google Scholar]
- 13.Sequist TD, Fitzmaurice GM, Marshall R, Shaykevich S, Safran DG, Ayanian JZ Physician performance and racial disparities in diabetes mellitus care. Arch Intern Med 2008;168:1145–51 [DOI] [PubMed] [Google Scholar]
- 14.Alshamsan R, Millett C, Majeed A, Khunti K Has pay for performance improved the management of diabetes in the United Kingdom? Prim Care Diabetes 2010;4:73–8 [DOI] [PubMed] [Google Scholar]
- 15.Millett C, Gray J, Saxena S, Netuveli G, Khunti K, Majeed A Ethnic disparities in diabetes management and pay-for-performance in the UK: the Wandsworth Prospective Diabetes Study. PLoS Med 2007;4:e191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gray J, Millett C, Saxena S, Netuveli G, Khunti K, Majeed A Ethnicity and quality of diabetes care in a health system with universal coverage: population-based cross-sectional survey in primary care. J Gen Intern Med 2007;22:1317–20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Millett C, Netuveli G, Saxena S, Majeed A Impact of pay for performance on ethnic disparities in intermediate outcomes for diabetes: a longitudinal study. Diabetes Care 2009;32:404–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Quality and Outcomes Framework prevalence data. 2010. NHS Information Centre. http://www.ic.nhs.uk/statistics-and-data-collections/supporting-information/audits-and-performance/the-quality-and-outcomes-framework/qof-2009-10/data-tables/prevalence-data-tables .
- 19.de Lusignan S, Khunti K, Belsey J, Hattersley A, van Vlymen J, Gallagher H, et al. A method of identifying and correcting miscoding, misclassification and misdiagnosis in diabetes: a pilot and validation study of routinely collected data. Diabet Med 2011;27:203–9 [DOI] [PubMed] [Google Scholar]
- 20.Huang ES, Sachs GA, Chin MH Implications of new geriatric diabetes care guidelines for the assessment of quality of care in older patients. Medical Care 2006;44:373–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mathur R, Badrick E, Boomla K, Bremner S, Hull S, Robson J Prescribing in general practice for people with coronary heart disease; equity by age, sex, ethnic group and deprivation. Ethn Health 2011;16:107–23 [DOI] [PubMed] [Google Scholar]
- 22.James G, Zhou Y, Miller S Modeling data with structural and temporal correlation using lower level and higher level multilevel models. Pharm Stat 2011;5:395–406 [DOI] [PubMed] [Google Scholar]
- 23.Collett D Modelling binary data. London: Chapman and Hall/CRC, 2002 [Google Scholar]
- 24.Hamilton FL, Bottle A, Vamos EP, Curcin V, Anthea M, Molokhia M, et al. Impact of a pay-for-performance incentive scheme on age, sex, and socioeconomic disparities in diabetes management in UK primary care. J Ambul Care Manage 2010;33:336–49 [DOI] [PubMed] [Google Scholar]
- 25.O'Kane MJ, McMenamin M, Bunting BP, Moore A, Coates VE The relationship between socioeconomic deprivation and metabolic/cardiovascular risk factors in a cohort of patients with type 2 diabetes mellitus. Prim Care Diabetes 2010;4:241–9 [DOI] [PubMed] [Google Scholar]
- 26.Trivedi AN, Grebla RC, Wright SM, Washington DL Despite improved quality of care in the Veterans Affairs health system, racial disparity persists for important clinical outcomes. Health Aff (Millwood) 2011;30:707–15 [DOI] [PubMed] [Google Scholar]
- 27.Trivedi AN, Zaslavsky AM, Schneider EC, Ayanian JZ Trends in the quality of care and racial disparities in Medicare managed care. N Engl J Med 2005;353:692–700 [DOI] [PubMed] [Google Scholar]
- 28.Turner RC, Cull CA, Frighi V, Holman RR Glycemic control with diet, sulfonylurea, metformin, or insulin in patients with type 2 diabetes mellitus: progressive requirement for multiple therapies (UKPDS 49). UK Prospective Diabetes Study (UKPDS) Group. JAMA 1999;281:2005–12 [DOI] [PubMed] [Google Scholar]
- 29.Hull SA, Mathur R, Badrick E, Robson J, Boomla K Recording ethnicity in primary care: assessing the methods and impact. Br J Gen Pract 2011;61:e290–4 [DOI] [PMC free article] [PubMed] [Google Scholar]