Abstract
Background
Women who participate in high-risk sports suffer anterior cruciate ligament injury at a 4- to 6-fold greater rate than men.
Purpose
To prospectively determine if female athletes with decreased passive knee joint restraint (greater joint laxity) and greater side-to-side differences in knee laxity would be at increased risk of anterior cruciate ligament injury.
Study Design
Case control study; Level of evidence, 3.
Methods
From 1558 female soccer and basketball players who were prospectively screened, 19 went on to tear their anterior cruciate ligaments. Four height- and mass-matched control subjects were selected from the uninjured screened athletes for comparison with each of the 19 injured subjects, making a total of 95 subjects (19 injured; 76 uninjured). Generalized joint-laxity tests and anterior-posterior tibiofemoral translation were quantified using the CompuKT knee arthrometer. A multivariable logistic regression model was constructed to determine predictors of anterior cruciate ligament injury status from recorded laxity measures.
Results
A multivariable logistic regression model (chi-square = 18.6; P = .002) used the independent variables laxity measures of knee hyperextension (P = .02), wrist and thumb to forearm opposition (P = .80), fifth-finger hyperextension >90° (P = .71), side-to-side differences in anterior-posterior tibiofemoral translation (P = .002), and prior knee injury (P = .22) to predict anterior cruciate ligament–injury status. The validated C statistic, or validated area under the receiver operating characteristic curve, was 0.72. For every 1.3-mm increase in side-to-side differences in anterior-posterior knee displacement, the odds of anterior cruciate ligament–injured status increased 4-fold (95% confidence interval, 1.68–9.69). A positive measure of knee hyperextension increased the odds of anterior cruciate ligament–injured status 5-fold (95% confidence interval, 1.24–18.44).
Conclusion
The current results indicate that increased knee-laxity measures may contribute to increased risk of anterior cruciate ligament injury. The methods to quantify knee joint laxity in this report may be used in conjunction with measures of neuromuscular control of the knee joint to identify high-risk female athletes with high accuracy. Once high-risk female athletes are identified, they may be targeted to the appropriate interventions to reduce injury risk.
Keywords: neuromuscular control, dynamic valgus, knee joint load, ACL injury, injury prevention, gender differences
Women who participate in high-risk sports suffer ACL injury at a 4- to 6-fold greater rate than men.1,4 Prior investigations indicate that greater knee laxity38,65,68 and increased generalized joint laxity16,39,44,62,66 are more prevalent in adolescent girls than in their male counterparts. Uhorchak et al74 reported that female athletes with greater passive joint restraint, indicated by generalized joint laxity greater than one standard deviation of the mean, had increased risk of ACL injury. Similarly, Ramesh and colleagues63 found that ACL injury was more frequent in those patients with greater overall joint laxity, specifically those with increased knee joint laxity.
Dynamic knee stability is affected by both passive (ligamentous) and active (neuromuscular) joint restraints.65,67 Female athletes at a high risk of ACL injury exhibit increased knee abduction motion and torque during dynamic landing tasks, which may relate to decreased dynamic knee stability and neuromuscular control of the knee joint.33,34,53 In addition, female athletes with side-to-side differences in knee abduction measures also have increased risk of ACL injury.33 However, it is not yet known which passive and active measures are most contributory to dynamic knee stability and most predictive of increased ACL injury risk. Excessive passive knee laxity may result in decreased dynamic knee stability during athletic maneuvers and may be related to previously identified ACL injury risk factors.34 Most knee ligamentous injuries in women’s sports occur by noncontact mechanisms (deceleration, lateral pivoting, or landing).58 Increased risk of ACL injury may occur in the absence of sufficiently taut ligaments and tendons that traverse and surround the lower extremity to stabilize the knee joint and absorb ground-reaction forces. Anterior cruciate ligament–injury risk factors are likely multifactorial; however, passive joint laxity may be an important contributor to dynamic knee stability and risk of ACL injury.
While strong evidence exists to show that there is a gender difference in rates of ACL injury in postpubertal athletes, there is minimal evidence to suggest that this trend is found in prepubescent athletes.3,10,14,24 After the onset of puberty, both girls and boys experience rapid increases in height and mass and changes in hormonal concentrations. Coinciding with these changes are gender-specific changes in general ligamentous and knee ligament laxity. Female and male generalized joint-laxity patterns diverge during and after puberty, as boys demonstrate a decrease in joint flexibility and ligament laxity with chronological age and maturational stage, while girls demonstrate an increase.9,60,62,69 In addition to gender differences in generalized joint laxity after puberty, anterior-posterior (AP) knee laxity also changes. Boys demonstrate a decrease in AP knee laxity, unlike their female counterparts.72 The joint-laxity differences in adolescent male and female athletes previously reported in the literature are likely a result of the changes that accompany puberty.62 These developmental differences may also contribute to the postpubertal gender gap in decreased dynamic knee stability and increased ACL injury rate.32,33,36,79
There is a trend toward an increase in ACL injuries during the preovulatory phase of the menstrual cycle in female athletes.36 Therefore, fluctuation of female hormones may be involved in increased female ACL injury rates.26,80 Specifically, fluctuations in daily hormone levels during the menstrual cycle may influence AP knee laxity.79 Hence, growth and development and hormonal fluctuations after puberty may be contributors to alterations in joint laxity and increased ACL injury risk in female athletes.
The purpose of the current study was to prospectively determine if female athletes with decreased passive knee joint restraint (greater joint laxity) and greater side-to-side differences in knee laxity would be at increased risk of ACL injury. The prospective coupled biomechanical-epidemiological cohort design of this study allowed us to directly test the hypothesis that greater passive joint laxity and greater side-to-side differences in knee stability would predict ACL injury risk in high-risk female athletes.
MATERIALS AND METHODS
Subjects
The participants included in the present study represent a subset of a cohort of subjects who were prospectively screened (N = 1558) before sports participation during the period from 2002 until 2006. Nineteen female athletes went on to have ACL injuries (15 during soccer and 4 during basketball play). Anterior cruciate ligament ruptures were confirmed by arthroscopic surgery (n = 18) or magnetic resonance image (n = 1). Prior published critiques of similar epidemiological designs to determine risk factors for ACL injury have expressed concern about the confounding effects of sport, height, and mass.33,59 To better control for the confounding variance between individual sport teams and individual anthropometrics, the current investigation used matched investigational subjects with 4 teammates of the nearest height and mass to serve as uninjured control subjects. The nested case control study design yielded 95 female high school and collegiate soccer and basketball players who were all prospectively screened for laxity measures before their recorded ACL injury. The ACL-injured population was similar in age (16.3 ± 1.7 years vs 15.6 ± 1.4 years, P = .08), height (166.4 ± 6.8 cm vs 165.5 ± 6.2 cm, P = .59), and mass (60.3 ± 7.3 kg vs 59.1 ± 7.8 kg, P = .54) to uninjured teammates matched for control comparisons.
Informed written consent was obtained from all subjects and their parents and approved by the Institutional Review Board. After the informed consent was obtained, height (in centimeters) and mass (in kilograms) were measured and recorded. A form that included the question “Have you ever injured your knee while playing a sport?” was used to determine history of knee injury. General ligamentous and AP knee–laxity measures were recorded during the laboratory evaluation during each athlete’s visit for their prospective screening.
Test Protocol
Each subject was tested for generalized joint laxity using tests depicted in Figures 1 through 4. Generalized joint-laxity tests consisted of fifth-finger hyperextension >90°, elbow hyperextension beyond neutral, wrist and thumb to forearm opposition, and knee hyperextension beyond neutral.61 Anterior-posterior tibiofemoral translation was quantified using the CompuKT knee arthrometer (Medmetric Corp, San Diego, Calif) to measure total AP displacement of the tibia relative to the secured femur. During the measurement, each leg was placed on the adjustable thigh support with the knee stabilized at 20° to 35° of knee flexion. The arthrometer was secured to the shank such that the patellar sensor pad rested on the patella with the knee joint line reference mark on the CompuKT aligned with the subject’s joint line. The ankle and foot were stabilized to limit leg rotation. The tester provided a posterior and anterior (±134 N) pressure on an axis perpendicular to the tibia. Total displacement (mm) was plotted on the computer and recorded (Figure 5). Side-to-side differences (per 1.3-mm difference; represents the 25th vs 75th interquartile range coefficients) in knee laxity were calculated from the absolute difference in total AP tibial translation between the dominant and nondominant knee. The dominant leg was determined for each subject by asking which leg they would use to kick a ball as far as possible.21,27 CompuKT measurements of anterior knee laxity demonstrated reliability with intraclass correlation coefficients (ICCs) between testers that ranged from 0.81 to 0.86 and within-tester correlations that ranged from 0.92 to 0.95.57 All testing for this study was performed by 2 investigators who demonstrated good to excellent intrarater reliability for CompuKT and joint-laxity scores, respectively, during pilot testing (ICC range, 0.891–0.972). In addition, general joint-laxity classifications, similar to those used in the current investigation, also demonstrate good to excellent interrater reliability.7
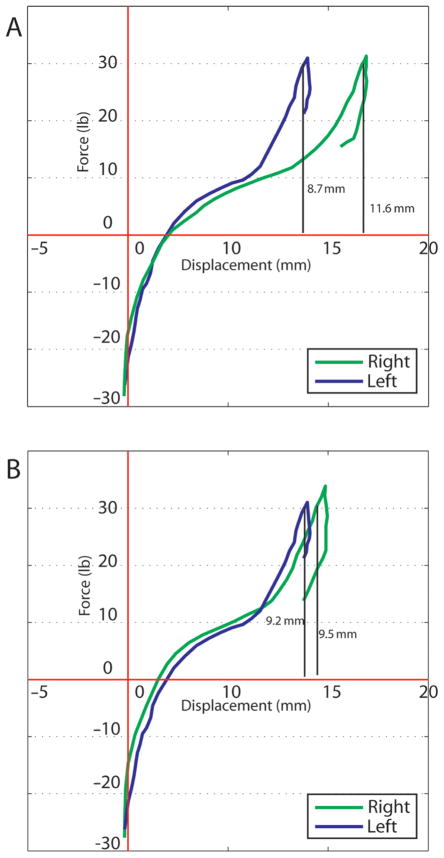
Figure 1.
Knee hyperextension test. Each subject was placed in a supine position with a box placed under both ankles. The axis of the goniometer was aligned with the lateral epicondyle of the femur. The distal arm was positioned with the lateral malleolus, and the proximal arm was aligned with the greater trochanter. Hyperextension of the knee beyond neutral resulted in a positive indication for the knee hyperextension test.
Figure 4.
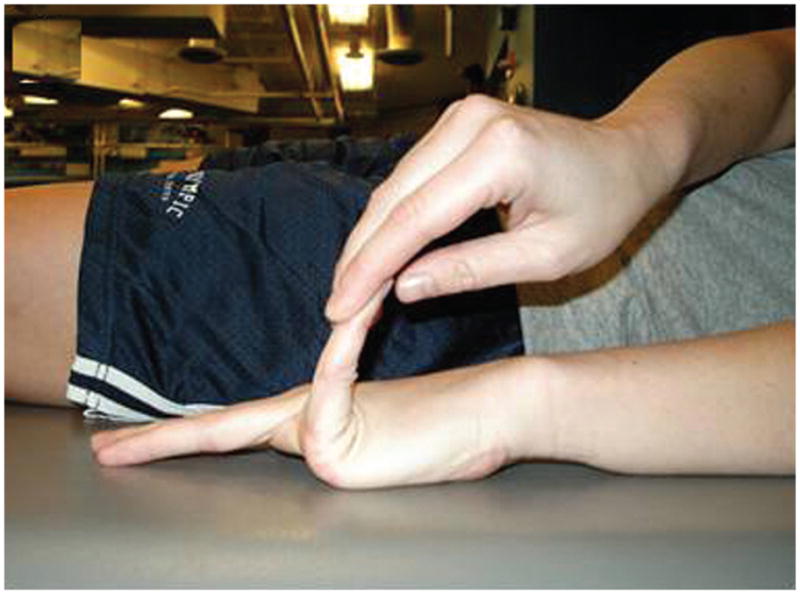
Fifth-finger hyperextension >90° test. Each subject’s forearm, wrist, and fingers were stabilized on a flat table. The tester passively extended the subject’s fifth finger as far as possible without pain. Hyperextension of 90° or greater resulted in a positive indication for the fifth-finger hyperextension >90° test.
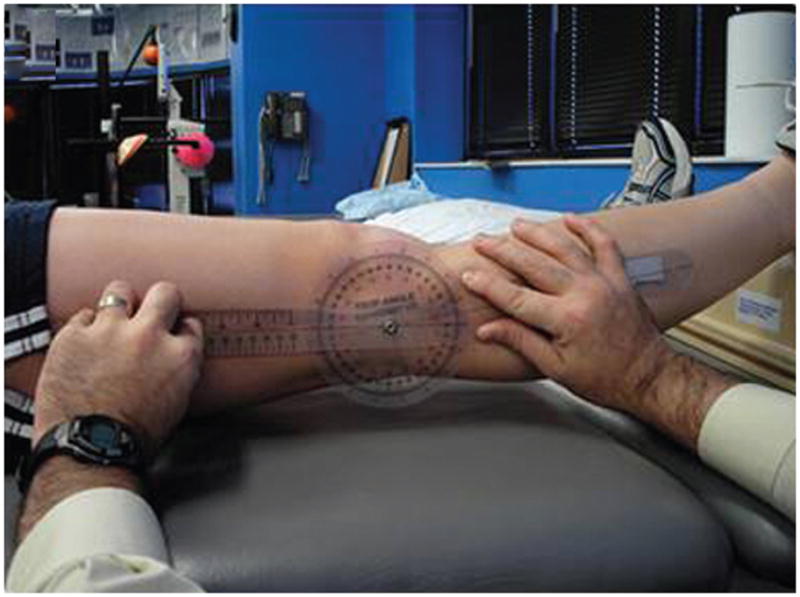
Figure 5.
Example of CompuKT2000 plots from 2 (A and B) study subjects. Anterior-posterior tibiofemoral translation was measured at ±134 N. Subject A presents greater side-to-side differences in AP knee laxity.
Statistical Analysis
A multivariable logistic regression model was constructed to determine predictors of ACL injury status from the laxity measures taken at the fifth metacarpal, elbow, thumb, knee, and tibiofemoral total translation, including from side-to-side differences in AP tibiofemoral translation. Previous knee injury was also included into the model for adjustment purposes, as it is a potential confounding effect on AP knee–laxity measures. One indicator variable was created for each dichotomous independent variable (fifth metacarpal hyperextension, elbow hyperextension, thumb to forearm, and knee hyperextension). A “1” was used to indicate the presence of positive laxity, and “0” indicated negative laxity.
In addition to the multivariable model, individual simple binary logistic regression models were constructed (1) to select variables for the final prediction model, and (2) to compare unadjusted models to the adjusted models to determine potential confounding effects. If the P value of the chi-square statistics for a specific variable was greater than a liberal value of .50, then the variable was eliminated. Variables that we considered to have high clinical value were included in the model regardless of significance. The multivariable model is considered the primary statistical analysis because it provides (1) adjusted effects controlling for the other predictors in the model, (2) removes the effects of confounding, and (3) provides accurate estimates of model accuracy using the C statistic, which is equivalent to the area under the receiver operating characteristic (ROC) curve. Since overfitting remained likely, given the ratio of the number of events (19 knee injuries) to degrees of freedom (df) of the regression model (df = 5), we validated the C statistic using 200 bootstrap samples. Each of the 200 bootstrap samples had 95 subjects, and these samples were only used to validate the C statistic of the regression model. This is referred to as internal validation and involves fitting and validating the model by carefully using a series of subjects of the same sample size as the study sample. By doing this, one estimates the “likely performance of the final model on new subjects, which, after all, is often of most interest.”29 The validated C statistic provides an estimate that subtracts the average amount of bias from the originally estimated statistics. A perfect model would have a validated C statistic of 1.0. A C statistic of 0.80 or above has excellent utility, and between 0.70 and 0.80 has acceptable utility in predicting the outcomes of individual patients.37
RESULTS
Table 1 presents the frequency distribution for positive laxity measures, and Table 2 presents the means and standard deviations (SDs) for AP knee motion measured on a CompuKT (Medmetric Corp) arthrometer. In the ACL-injured group, 7 of 19 (37%) reported a prior knee injury on their questionnaire. In the control group, 22 of the 76 (29%) athletes reported a history of knee injury.
TABLE 1.
Frequency Distribution for Positive Laxity Measures and Self-Reported Prior Knee Injury
| Positive Laxity Measure | Controls
|
Injured
|
||
|---|---|---|---|---|
| Frequency (n = 76) | % | Frequency (n = 19) | % | |
| Fifth metacarpal | 18 | 24 | 6 | 32 |
| Elbow | 29 | 38 | 7 | 37 |
| Thumb | 42 | 55 | 13 | 68 |
| Knee | 18 | 24 | 8 | 42 |
TABLE 2.
Means and Standard Deviations for Anterior-Posterior Knee Motion Measured on CompuKT Arthrometera,b
| Knee Arthrometer Measurement | Dom
|
Nondom
|
Difference
|
|||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | |
| Control (n = 76) | 8.4 | 2.47 | 8.3 | 2.30 | 1.0 | 0.82 |
| Injured (n = 19) | 9.4 | 2.65 | 9.0 | 2.64 | 2.0 | 1.61 |
Dom, dominant; Nondom, nondominant; SD, standard deviation.
Results of simple binary logistic regression analyses examining prediction of ACL injury from the independent variables are presented in Table 3 under the univariable, or unadjusted, results. Side-to-side differences in knee laxity showed a simple (unadjusted) effect on ACL injury. Subjects with side-to-side differences (per 1.3-mm difference, represents the 25th vs 75th interquartile range coefficients) had more than a 3-fold greater odds of ACL injury than subjects without differences (95% confidence interval [CI], 1.47–7.08). Unadjusted odds ratios (ORs) for the other variables ranged from 0.57 to 2.34 and did not significantly differ from the null hypothesis of an OR of 1.0.
TABLE 3.
Results of Univariate and Multivariate Analysesa
| Factor | Univariable
|
Multivariable
|
||
|---|---|---|---|---|
| OR (95% CI) | P Value | OR (95% CI) | P Value | |
| Side-to-side differences in knee laxityb | 3.23 (1.47–7.08) | .003 | 4.03 (1.68–9.69) | .002 |
| Fifth-finger hyperextension >90° | 1.49 (0.49–4.48) | .48 | 1.27 (0.36–4.48) | .71 |
| Wrist and thumb to forearm opposition | 1.75 (0.60–5.10) | .30 | 1.17 (0.35–4.00) | .80 |
| Knee hyperextension beyond neutral | 2.34 (0.82–6.72) | .11 | 4.78 (1.24–18.44) | .02 |
| Previous knee injury | 1.43 (0.50–4.12) | .51 | 2.27 (0.62–8.33) | .22 |
| Elbow hyperextension beyond neutral | 1.06 (0.37–2.99) | .92 | ||
OR, odds ratio; CI, confidence interval.
Per 1.3-mm difference; represents the 25th vs 75th interquartile range coefficients.
For the multivariable logistic regression model, the variable elbow hyperextension exceeded the minimum predetermined alpha cutoff and was eliminated. Prior knee injury exceeded the alpha cutoff but was considered clinically relevant and was included in the final model. The remaining 5 variables were then examined together in a multivariable model. The multivariable logistic regression model (chi-square, 18.6; P = .002) used the independent variables of laxity measures of knee hyperextension (P = .02), wrist and thumb-to-forearm opposition (P = .80), fifth-finger hyperextension >90° (P = .71), side-to-side differences in AP tibiofemoral translation (P = .002), and prior knee injury (P = .22) to predict ACL injury status. The model has a C statistic of 0.78. Upon validation of the model, the validated C statistic was 0.72. Therefore, the amount of overfitting, or overoptimism, was approximately 8%. For every 1.3-mm increase in side-to-side differences in AP knee displacement, the odds of ACL-injured status increased 4-fold (95% CI, 1.68–9.69). Interestingly, only 47% of the knees with increased AP knee displacement were the actual knees that went on to ACL-injured status. A positive measure of knee hyperextension increased the odds of ACL-injured status 5-fold (95% CI, 1.24–18.44). Prior knee injury did not change the odds of ACL-injured status (OR = 2.27; 95% CI, 0.62–8.33). Comparing the results of the adjusted multivariable models with the unadjusted univariable models indicated potential confounding effects, as regression coefficients changed at least 10%. Therefore, we recommend the estimates from the multivariable model be used because adjustment removes the effect of confounding.
DISCUSSION
The purpose of this study was to identify prospectively measured laxity measures related to the future risk of ACL injury in young, female athletes. A logistic regression model that included knee hyperextension and side-to-side differences in AP tibiofemoral translation was predictive of future ACL-injury status. These findings indicate that knee-laxity measures are potential measures that may be related to increased risk of ACL injury. Previous authors have reported that excessive generalized joint laxity and knee joint laxity also increased risk.65,74 In addition to knee hyperextension, side-to-side differences in measures of total AP tibiofemoral translation also increased the risk of ACL injury in the current study. Hewett and colleagues33 demonstrated that greater side-to-side differences and total dynamic coronal plane knee stability, evidenced by greater knee abduction moments and angles during a drop vertical jump, were related to increased risk of ACL injury. Collectively, these data indicate that joint stabilization provided by both active (dynamic knee alignment) and passive (ligament and tendon laxity) restraints is needed to provide protection against joint injury. Ligaments provide passive joint restraint, while musculotendinous units contribute to both passive and active joint restraint. Ligaments, joint capsules, joint surface contacts, passive or reflexive muscle tensions, and soft tissues all provide contributions to dynamic joint stability and end-range of motion.71
Prior investigations indicate that greater knee laxity38,65,68 and increased generalized joint laxity16,39,44,62,66 are more prevalent in adolescent girls than in their male counterparts. Uhorchak et al74 reported that female athletes with greater passive joint restraint, indicated by generalized joint laxity greater than 1 standard deviation of the mean, had increased risk of ACL injury. Similarly, Ramesh and colleagues63 found ACL injury was more frequent in those patients with greater overall joint laxity and specifically those with increased knee joint laxity. In general, the passive joint restraints are not readily modifiable by nature. Flexibility training may offer some potential for modification to the passive restraints system. However, in 1997, Ford20 compared soccer athletes who had greater hamstring flexibility with those with average flexibility while performing a 180° cutting technique. Using a relatively small sample size (N = 19), the greater hamstring flexibility group revealed trends of decreased knee flexion angle (P = .070) at initial contact of the cut with concomitantly slower onset of hamstrings activation (P = .098). Increased flexibility may be related to a period of greater delay of effective cocontraction of the hamstring and quadriceps.20 The delay may predispose athletes with increased knee flexor laxity and knee hyperextension to perform dynamic sports-related activities with decreased sagittal plane knee flexion.6 Sagittal plane movement and load patterns during dynamic tasks may also contribute to the current gender disparity in noncontact ACL injury rates.11,46 Specifically, the relative decreases in knee flexion typically observed in female athletes at initial contact and throughout stance during sports movements are proposed to elicit anterior tibial shear loads large enough to injure the ACL.17,47 Therefore, improved lower extremity movement strategies during high-risk sports movements—in particular those that address high-risk movements that contribute to decreased sagittal plane motion and increased coronal plane motions and load—may reduce risk and possibly prevent ACL injuries in female athletes.6,33,58 In addition, the current data may indicate that increased joint mobility through active and passive flexibility training may be contraindicated for ACL injury–prevention programs. Recent meta-analysis and review of the literature also indicate that flexibility training does not provide protective effects from injury, as has been previously purported in the literature.73 The cumulative evidence indicates that static stretching immediately prior to play may decrease performance8,13,78 and does not reduce injury risk in athletes.2,30,73,76
There is strong evidence that neuromuscular training programs are effective for improving measures of performance. The benefits of a program designed for performance enhancement often include greater power, agility, and speed.41,42,77 Female athletes may especially benefit from multicomponent neuromuscular training, as they often display decreased baseline levels of strength and power compared with their male counterparts. Comprehensive neuromuscular training programs designed for young women may significantly increase power, strength, and neuromuscular control and decrease gender differences in these measures.42,43 Dynamic neuromuscular training can reduce gender-related differences in force absorption, active joint stabilization, muscle imbalances, and functional biomechanics while increasing strength of bones, ligaments, and tendons.18,19,35,64 In addition, neuromuscular training may increase active knee stability in the coronal plane.35,52,54,55 Concomitantly, neuromuscular training also likely reduces the risk of ACL injury in female athletes.31
Myer et al attempted to address the prevention of ACL injuries by examining the effects of well-established training strategies on lower limb mechanical parameters that predict ACL injury risk.33,51 Specifically, they evaluated the most effective and efficient means of increasing dynamic knee stability in female athletes.51 A linear regression analysis was employed to determine the potential association between the pretest measures of coronal-plane knee laxity and change in this variable with training. In the trained group, pretest coronal-plane knee laxity predicted 40% of the variance in the reduction of coronal-plane knee laxity measured after training. In contrast, the control group showed no similar causal relationship between pretest knee abduction measures and change in posttest measures.51 This analysis indicated that athletes with normal levels of coronal plane knee stability will have little if any benefit from targeted neuromuscular training. However, athletes who demonstrate decreased levels of dynamic knee stability appear to have a greater potential to change their outcome. This association between decreased symptom and decreased effect of intervention has been previously demonstrated40 but is often ignored in clinical investigations.28
There is limited potential to modify the passive knee-laxity measures obtained in the current study. However, passive knee laxity may be used in combination with dynamic coronal-plane knee measures to more effectively identify female athletes at risk of ACL injury. Once identified, these athletes may be targeted for neuromuscular training designed to increase dynamic coronal-plane knee stability. These screening methods may work synergistically to provide the greatest potential to selectively identify high-risk active and passive knee stability profiles that indicate female athletes who would benefit from targeted neuromuscular training.33,51 Prevention of these injuries would allow tens of thousands of young female athletes to continue the health benefits of sports participation into adulthood and avoid the long-term disability and osteoarthritis that occur with an estimated 10-fold or greater incidence after knee ligament injury.15,25,45,75
The absence of passive and/or dynamic knee joint stability may be responsible for the increased rates of knee injury in female athletes,35,38 but it is not normally examined in athletes before participation. Standard preparticipation physical examinations rarely assess joint stability. Huston and Wojtys38 reported greater knee laxity in mature female athletes relative to males, while Cheng et al12 showed no differences in prepubescent children. Few if any measures are assessed during preparticipation examinations, and plans for intervention are rarely implemented. Although musculoskeletal disorders are observed during preparticipation examination in approximately 10% of examined athletes,48 intervention occurs in only 1% to 3%.70 Addressing these deficiencies in current screening protocols may allow the targeting of specific athletes to potential prophylactic treatments that reduce ACL injury risk. In addition, proper rehabilitation of athletes after a knee injury may be crucial to help reduce the potential for an ACL injury.56 The current investigation reported that 37% of the subjects indicated a prior knee injury on their questionnaire. While this factor did not significantly contribute to the current regression model’s prediction of ACL-injured status, previous authors have demonstrated prior lower extremity injury may lead to increased risk of injury.5,49,50 For this reason, prior knee injury was included in the final regression analyses based on its potential confounding effect on the other significant risk factors. Future investigations should continue to determine the relationship of prior knee injury to the subsequent ACL injury.
Limitations
Injury to the ACL in female athletes likely has a multifactorial origin, with several potential elements that determine injury outcome. Prior epidemiologic data demonstrate that many physical and psychological parameters may contribute to ACL injury rates in female athletes. There are several possible contributing and confounding variables that were not controlled for in the current study design, which included school, team/sport, age/grade, aggressiveness, foot pronation, quadriceps angle, femoral notch width, biomechanical and neuromuscular parameters, reliable menstrual status reporting, blood hormone levels, previous lower extremity injury other than the knee, and prior knee injury classification. Without the inclusion of these measures in the regression analysis, their potential confounding effects of knee laxity and ACL-injury risk cannot be controlled for, thus limiting the generalizability of the current results. To better define the mechanism of increased risk of ACL injury in female athletes, future investigations with larger samples size should aim to develop more robust ACL injury prediction models that include all contributing parameters. However, the significant effects of general joint-laxity measures on ACL-injury status in female athletes were observed in this study. The observed differences were of a magnitude outside the protocol’s measurement error and should be considered a potential contributing mechanism to increased ACL-injury risk in female athletes.
CONCLUSION
It is well known that ACL-injury risk in the athletic population is greater in female athletes compared with male athletes. Prior studies indicate that decreased dynamic knee stability, evidenced from decreased coronal-plane knee stability, provides a mechanism that underlies this gender disparity in ACL-injury risk.21–23,32,33 The current results indicate that passive anteroposterior tibiofemoral laxity and passive knee hyperextension may contribute to increased ACL injury risk. Future research is warranted to determine the relationships between active and passive knee stability and to determine their relationship to one another or determine if they independently increase risk of injury in female athletes. Female athletes who demonstrate decreased active and passive knee stability may be indicated for targeted neuromuscular training.51 No validated method for the screening and identification of athletes at greater risk of ACL injury based on joint laxity has previously been available. Further research into the proposed theories relating to this musculoskeletal problem is warranted for intervention and possible prevention of ACL injuries in female athletes.
Figure 2.
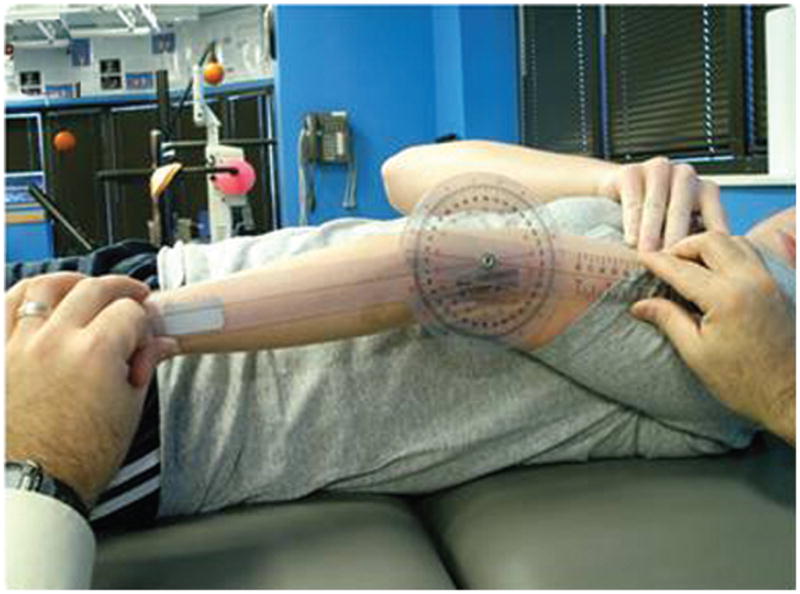
Elbow hyperextension test. Each subject’s shoulder was abducted to approximately 80°, with the forearm supinated. The axis of the goniometer was placed over the lateral epicondyle of the humerus, with the distal end aligned with the radial styloid process, and the proximal arm aligned along the lateral midline of the subject’s humerus. Hyperextension beyond neutral resulted in a positive indication for the elbow hyperextension test.
Figure 3.

Thumb to forearm test. Each subject flexed the wrist and pulled the thumb toward the forearm using the opposite hand. If the thumb could be abducted to touch the forearm, a positive indicator was given for the thumb to forearm test. Inability to touch the forearm resulted in a negative indication.
Acknowledgments
The authors acknowledge funding support from National Institutes of Health Grant R01-AR049735. The authors thank Carmen Quatman for her critical input into the article content.
Footnotes
No potential conflict of interest declared.
References
- 1.Agel J, Arendt EA, Bershadsky B. Anterior cruciate ligament injury in national collegiate athletic association basketball and soccer: a 13-year review. Am J Sports Med. 2005;33:524–530. doi: 10.1177/0363546504269937. [DOI] [PubMed] [Google Scholar]
- 2.Andersen JC. Stretching before and after exercise: effect on muscle soreness and injury risk. J Athl Train. 2005;40:218–220. [PMC free article] [PubMed] [Google Scholar]
- 3.Andrish JT. Anterior cruciate ligament injuries in the skeletally immature patient. Am J Orthop. 2001;30:103–110. [PubMed] [Google Scholar]
- 4.Arendt E, Dick R. Knee injury patterns among men and women in collegiate basketball and soccer. NCAA data and review of literature. Am J Sports Med. 1995;23:694–701. doi: 10.1177/036354659502300611. [DOI] [PubMed] [Google Scholar]
- 5.Bahr R, Bahr IA. Incidence of acute volleyball injuries: a prospective cohort study of injury mechanisms and risk factors. Scand J Med Sci Sports. 1997;7:166–171. doi: 10.1111/j.1600-0838.1997.tb00134.x. [DOI] [PubMed] [Google Scholar]
- 6.Boden BP, Dean GS, Feagin JA, Garrett WE., Jr Mechanisms of anterior cruciate ligament injury. Orthopedics. 2000;23:573–578. doi: 10.3928/0147-7447-20000601-15. [DOI] [PubMed] [Google Scholar]
- 7.Boyle KL, Witt P, Riegger-Krugh C. Intrarater and interrater reliability of the Beighton and Horan Joint Mobility Index. J Athl Train. 2003;38:281–285. [PMC free article] [PubMed] [Google Scholar]
- 8.Bradley PS, Olsen PD, Portas MD. The effect of static, ballistic, and proprioceptive neuromuscular facilitation stretching on vertical jump performance. J Strength Cond Res. 2007;21:223–226. doi: 10.1519/00124278-200702000-00040. [DOI] [PubMed] [Google Scholar]
- 9.Branta C, Haubenstricker J, Seefeldt V. Age changes in motor skills during childhood and adolescence. Exerc Sport Sci Rev. 1984;12:467–520. [PubMed] [Google Scholar]
- 10.Buehler-Yund C. Environmental Health. Cincinnati, Ohio: University of Cincinnati; 1999. A longitudinal study of injury rates and risk factors in 5- to 12-year-old soccer players; p. 161. [Google Scholar]
- 11.Chappell JD, Yu B, Kirkendall DT, Garrett WE. A comparison of knee kinetics between male and female recreational athletes in stop-jump tasks. Am J Sports Med. 2002;30:261–267. doi: 10.1177/03635465020300021901. [DOI] [PubMed] [Google Scholar]
- 12.Cheng JC, Chan PS, Hui PW. Joint laxity in children. J Pediatr Orthop. 1991;11:752–756. doi: 10.1097/01241398-199111000-00010. [DOI] [PubMed] [Google Scholar]
- 13.Church JB, Wiggins MS, Moode FM, Crist R. Effect of warm-up and flexibility treatments on vertical jump performance. J Strength Cond Res. 2001;15:332–336. [PubMed] [Google Scholar]
- 14.Clanton TO, DeLee JC, Sanders B, Neidre A. Knee ligament injuries in children. J Bone Joint Surg Am. 1979;61:1195–1201. [PubMed] [Google Scholar]
- 15.Deacon A, Bennell K, Kiss ZS, Crossley K, Brukner P. Osteoarthritis of the knee in retired, elite Australian Rules footballers. Med J Aust. 1997;166:187–190. doi: 10.5694/j.1326-5377.1997.tb140072.x. [DOI] [PubMed] [Google Scholar]
- 16.Decoster LC, Vailas JC, Lindsay RH, Williams GR. Prevalence and features of joint hypermobility among adolescent athletes. Arch Pediatr Adolesc Med. 1997;151:989–992. doi: 10.1001/archpedi.1997.02170470023005. [DOI] [PubMed] [Google Scholar]
- 17.DeMorat G, Weinhold P, Blackburn T, Chudik S, Garrett W. Aggressive quadriceps loading can induce noncontact anterior cruciate ligament injury. Am J Sports Med. 2004;32:477–483. doi: 10.1177/0363546503258928. [DOI] [PubMed] [Google Scholar]
- 18.Faigenbaum AD, Kraemer WJ, Cahill B, et al. Youth resistance training: position statement paper and literature review. Strength and Conditioning. 1996;18:62–75. [Google Scholar]
- 19.Fleck SJ, Falkel JE. Value of resistance training for the reduction of sports injuries. Sports Med. 1986;3:61–68. doi: 10.2165/00007256-198603010-00006. [DOI] [PubMed] [Google Scholar]
- 20.Ford KR. Kinesiology and Health Promotion. Lexington, Ky: University of Kentucky; 1997. A comparison of knee joint kinematics and related muscle onset patterns observed during a 180° cutting maneuver executed by male and female soccer players; p. 83. [Google Scholar]
- 21.Ford KR, Myer GD, Hewett TE. Valgus knee motion during landing in high school female and male basketball players. Med Sci Sports Exerc. 2003;35:1745–1750. doi: 10.1249/01.MSS.0000089346.85744.D9. [DOI] [PubMed] [Google Scholar]
- 22.Ford KR, Myer GD, Smith RL, Vianello RM, Seiwert SL, Hewett TE. A comparison of dynamic coronal plane excursion between matched male and female athletes when performing single leg landings. Clin Biomech. 2006;21:33–40. doi: 10.1016/j.clinbiomech.2005.08.010. [DOI] [PubMed] [Google Scholar]
- 23.Ford KR, Myer GD, Toms HE, Hewett TE. Gender differences in the kinematics of unanticipated cutting in young athletes. Med Sci Sports Exerc. 2005;37:124–129. [PubMed] [Google Scholar]
- 24.Gallagher SS, Finison K, Guyer B, Goodenough S. The incidence of injuries among 87 000 Massachusetts children and adolescents: results of the 1980–81 Statewide Childhood Injury Prevention Program Surveillance System. Am J Public Health. 1984;74:1340–1347. doi: 10.2105/ajph.74.12.1340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gillquist J, Messner K. Anterior cruciate ligament reconstruction and the long-term incidence of gonarthrosis. Sports Med. 1999;27:143–156. doi: 10.2165/00007256-199927030-00001. [DOI] [PubMed] [Google Scholar]
- 26.Gray J, Taunton JE, McKenzie DC, Clement DB, McConkey JP, Davidson RG. A survey of injuries to the anterior cruciate ligament of the knee in female basketball players. Int J Sports Med. 1985;6:314–316. doi: 10.1055/s-2008-1025861. [DOI] [PubMed] [Google Scholar]
- 27.Greenberger HB, Paterno MV. Relationship of knee extensor strength and hopping test performance in the assessment of lower extremity function. J Orthop Sports Phys Ther. 1995;22:202–206. doi: 10.2519/jospt.1995.22.5.202. [DOI] [PubMed] [Google Scholar]
- 28.Harrell FE. Regression Modeling Statistics. New York, NY: Springer-Verlag New York Inc; 2001. [Google Scholar]
- 29.Harrell FE, Lee KL, Mark DB. Multivariable prognostic models: issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat Med. 1996;15:361–387. doi: 10.1002/(SICI)1097-0258(19960229)15:4<361::AID-SIM168>3.0.CO;2-4. [DOI] [PubMed] [Google Scholar]
- 30.Herbert RD, Gabriel M. Effects of stretching before and after exercising on muscle soreness and risk of injury: systematic review. BMJ. 2002;325:468. doi: 10.1136/bmj.325.7362.468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hewett TE, Ford KR, Myer GD. Anterior cruciate ligament injuries in female athletes: part 2. A meta-analysis of neuromuscular interventions aimed at injury prevention. Am J Sports Med. 2006;34(3):490–498. doi: 10.1177/0363546505282619. [DOI] [PubMed] [Google Scholar]
- 32.Hewett TE, Myer GD, Ford KR. Decrease in neuromuscular control about the knee with maturation in female athletes. J Bone Joint Surg Am. 2004;86:1601–1608. doi: 10.2106/00004623-200408000-00001. [DOI] [PubMed] [Google Scholar]
- 33.Hewett TE, Myer GD, Ford KR, et al. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study. Am J Sports Med. 2005;33:492–501. doi: 10.1177/0363546504269591. [DOI] [PubMed] [Google Scholar]
- 34.Hewett TE, Myer GD, Ford KR, Succop P. Passive and dynamic knee restraints determine risk of ACL injury in female athletes. Trans Orthop Res Soc. 2006;31:1125. [Google Scholar]
- 35.Hewett TE, Stroupe AL, Nance TA, Noyes FR. Plyometric training in female athletes. Decreased impact forces and increased hamstring torques. Am J Sports Med. 1996;24:765–773. doi: 10.1177/036354659602400611. [DOI] [PubMed] [Google Scholar]
- 36.Hewett TE, Zazulak BT, Myer GD. The effects of the menstrual cycle on ACL injury risk: a systematic review. Am J Sports Med. 2007;35(4):659–668. doi: 10.1177/0363546506295699. [DOI] [PubMed] [Google Scholar]
- 37.Hosmer DW, Lomeshow S. Applied Logistic Regression. New York, NY: J Wiley; 2000. [Google Scholar]
- 38.Huston LJ, Wojtys EM. Neuromuscular performance characteristics in elite female athletes. Am J Sports Med. 1996;24:427–436. doi: 10.1177/036354659602400405. [DOI] [PubMed] [Google Scholar]
- 39.Jansson A, Saartok T, Werner S, Renstrom P. General joint laxity in 1845 Swedish school children of different ages: age- and gender-specific distributions. Acta Paediatr. 2004;93:1202–1206. doi: 10.1080/08035250410023971. [DOI] [PubMed] [Google Scholar]
- 40.Knaus WA, Harrell FE, Fisher CJ, Jr, et al. The clinical evaluation of new drugs for sepsis. A prospective study design based on survival analysis. JAMA. 1993;270:1233–1241. [PubMed] [Google Scholar]
- 41.Kraemer WJ, Duncan ND, Volek JS. Resistance training and elite athletes: adaptations and program considerations. J Orthop Sports Phys Ther. 1998;28:110–119. doi: 10.2519/jospt.1998.28.2.110. [DOI] [PubMed] [Google Scholar]
- 42.Kraemer WJ, Hakkinen K, Triplett-Mcbride NT, et al. Physiological changes with periodized resistance training in women tennis players. Med Sci Sports Exerc. 2003;35:157–168. doi: 10.1097/00005768-200301000-00024. [DOI] [PubMed] [Google Scholar]
- 43.Kraemer WJ, Mazzetti SA, Nindl BC, et al. Effect of resistance training on women’s strength/power and occupational performances. Med Sci Sports Exerc. 2001;33:1011–1025. doi: 10.1097/00005768-200106000-00022. [DOI] [PubMed] [Google Scholar]
- 44.Larsson LG, Baum J, Mudholkar GS. Hypermobility: features and differential incidence between the sexes. Arthritis Rheum. 1987;30:1426–1430. doi: 10.1002/art.1780301216. [DOI] [PubMed] [Google Scholar]
- 45.Lohmander LS, Ostenberg A, Englund M, Roos H. High prevalence of knee osteoarthritis, pain, and functional limitations in female soccer players 12 years after anterior cruciate ligament injury. Arthritis Rheum. 2004;50:3145–3152. doi: 10.1002/art.20589. [DOI] [PubMed] [Google Scholar]
- 46.Malinzak RA, Colby SM, Kirkendall DT, Yu B, Garrett WE. A comparison of knee joint motion patterns between men and women in selected athletic tasks. Clin Biomech. 2001;16:438–445. doi: 10.1016/s0268-0033(01)00019-5. [DOI] [PubMed] [Google Scholar]
- 47.Markolf KL, Burchfield DM, Shapiro MM, Shepard MF, Finerman GA, Slauterbeck JL. Combined knee-loading states that generate high anterior cruciate ligament forces. J Orthop Res. 1995;13:930–935. doi: 10.1002/jor.1100130618. [DOI] [PubMed] [Google Scholar]
- 48.McKeag DB. Preseason physical examination for the prevention of sports injuries. Sports Med. 1985;2:413–431. doi: 10.2165/00007256-198502060-00003. [DOI] [PubMed] [Google Scholar]
- 49.Messina DF, Farney WC, DeLee JC. The incidence of injury in Texas high school basketball. A prospective study among male and female athletes. Am J Sports Med. 1999;27:294–299. doi: 10.1177/03635465990270030401. [DOI] [PubMed] [Google Scholar]
- 50.Milgrom C, Shlamkovitch N, Finestone A, et al. Risk factors for lateral ankle sprain: a prospective study among military recruits. Foot Ankle. 1991;12:26–30. doi: 10.1177/107110079101200105. [DOI] [PubMed] [Google Scholar]
- 51.Myer GD, Ford KR, Brent JL, Hewett TE. Differential neuromuscular training effects on ACL injury risk factors in “high-risk” versus “low-risk” athletes. BMC Musculoskelet Disord. 2007;8:39. doi: 10.1186/1471-2474-8-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Myer GD, Ford KR, Brent JL, Hewett TE. The effects of plyometric versus dynamic balance training on power, balance, and landing force in female athletes. J Strength Cond Res. 2006;20:345–353. doi: 10.1519/R-17955.1. [DOI] [PubMed] [Google Scholar]
- 53.Myer GD, Ford KR, Hewett TE. Rationale and clinical techniques for anterior cruciate ligament injury prevention among female athletes. J Athl Train. 2004;39:352–364. [PMC free article] [PubMed] [Google Scholar]
- 54.Myer GD, Ford KR, McLean SG, Hewett TE. The effects of plyometric versus dynamic stabilization and balance training on lower extremity biomechanics. Am J Sports Med. 2006;34:445–455. doi: 10.1177/0363546505281241. [DOI] [PubMed] [Google Scholar]
- 55.Myer GD, Ford KR, Palumbo JP, Hewett TE. Neuromuscular training improves performance and lower-extremity biomechanics in female athletes. J Strength Cond Res. 2005;19:51–60. doi: 10.1519/13643.1. [DOI] [PubMed] [Google Scholar]
- 56.Myer GD, Paterno MV, Ford KR, Quatman CE, Hewett TE. Rehabilitation after anterior cruciate ligament reconstruction: criteria-based progression through the return to sport phase. J Orthop Sports Phys Ther. 2006;36:385–402. doi: 10.2519/jospt.2006.2222. [DOI] [PubMed] [Google Scholar]
- 57.Myrer JW, Schulthies SS, Fellingham GW. Relative and absolute reliability of the KT-2000 arthrometer for uninjured knees. Testing at 67, 89, 134, and 178 N and manual maximum forces. Am J Sports Med. 1996;24:104–108. doi: 10.1177/036354659602400119. [DOI] [PubMed] [Google Scholar]
- 58.Olsen OE, Myklebust G, Engebretsen L, Bahr R. Injury mechanisms for anterior cruciate ligament injuries in team handball: a systematic video analysis. Am J Sports Med. 2004;32:1002–1012. doi: 10.1177/0363546503261724. [DOI] [PubMed] [Google Scholar]
- 59.Orchard JW. Potential to reduce the risk of noncontact anterior cruciate ligament (ACL) injuries. Am J Sports Med. 2005;33:1930–1931. doi: 10.1177/0363546505278707. [DOI] [PubMed] [Google Scholar]
- 60.Ostyn M, Simons J, Beunen G, et al. Somatic and Motor Development of Belgian Secondary School Boys. Leuven, Belgium: Catholic University of Leuven Press; 1980. [Google Scholar]
- 61.Pasque CB, Hewett TE. A prospective study of high school wrestling injuries. Am J Sports Med. 2000;28:509–515. doi: 10.1177/03635465000280041101. [DOI] [PubMed] [Google Scholar]
- 62.Quatman CE, Ford KR, Myer GD, Paterno MV, Hewett TE. The effects of gender and pubertal status on generalized joint laxity in young athletes [published online ahead of print June 25, 2007] J Sci Med Sport. doi: 10.1016/j.jsams.2007.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ramesh R, Von Arx O, Azzopardi T, Schranz PJ. The risk of anterior cruciate ligament rupture with generalized joint laxity. J Bone Joint Surg Br. 2005;87:800–803. doi: 10.1302/0301-620X.87B6.15833. [DOI] [PubMed] [Google Scholar]
- 64.Rooks DS, Micheli LJ. Musculoskeletal assessment and training: the young athlete. Clin Sports Med. 1988;7:641–677. [PubMed] [Google Scholar]
- 65.Rozzi SL, Lephart SM, Gear WS, Fu FH. Knee joint laxity and neuromuscular characteristics of male and female soccer and basketball players. Am J Sports Med. 1999;27:312–319. doi: 10.1177/03635465990270030801. [DOI] [PubMed] [Google Scholar]
- 66.Seckin U, Tur BS, Yilmaz O, Yaqci I, Bodur H, Arasil T. The prevalence of joint hypermobility among high school students. Rheumatol Int. 2005;25:260–263. doi: 10.1007/s00296-003-0434-9. [DOI] [PubMed] [Google Scholar]
- 67.Shultz SJ, Carcia CR, Perrin DH. Knee joint laxity affects muscle activation patterns in the healthy knee. J Electromyogr Kinesiol. 2004;14:475–483. doi: 10.1016/j.jelekin.2003.11.001. [DOI] [PubMed] [Google Scholar]
- 68.Shultz SJ, Shimokochi Y, Nguyen AD, et al. Measurement of varus-valgus and internal-external rotational knee laxities in vivo. Part II: relationship with anterior-posterior and general joint laxity in males and females. J Orthop Res. 2007;25:981–988. doi: 10.1002/jor.20398. [DOI] [PubMed] [Google Scholar]
- 69.Simons J. Growth and Fitness of Flemish Girls: the Leuven Growth Study. Champaign, Ill: Human Kinetics; 1990. [Google Scholar]
- 70.Smith J, Laskowski E. The preparticipation physical examination: Mayo Clinic experience with 2739 examinations. Mayo Clin Proc. 1998;73:419–429. doi: 10.1016/S0025-6196(11)63723-3. [DOI] [PubMed] [Google Scholar]
- 71.Solomonow M, Krogsgaard M. Sensorimotor control of knee stability. A review. Scand J Med Sci Sports. 2001;11:64–80. doi: 10.1034/j.1600-0838.2001.011002064.x. [DOI] [PubMed] [Google Scholar]
- 72.Sports Physical Therapy Section Abstracts: Platform Presentations SPL1–SPL28. Abstract of Paterno MV, Ford KR, Myer GD, et al. A prospective, longitudinal analysis of sex differences in knee laxity during growth and development in adolescents. J Orthop Sports Phys Ther. 2007;37(1):A67–A78. [Google Scholar]
- 73.Thacker SB, Gilchrist J, Stroup DF, Kimsey CD., Jr The impact of stretching on sports injury risk: a systematic review of the literature. Med Sci Sports Exerc. 2004;36:371–378. doi: 10.1249/01.mss.0000117134.83018.f7. [DOI] [PubMed] [Google Scholar]
- 74.Uhorchak JM, Scoville CR, Williams GN, Arciero RA, St Pierre P, Taylor DC. Risk factors associated with noncontact injury of the anterior cruciate ligament: a prospective 4-year evaluation of 859 West Point cadets. Am J Sports Med. 2003;31:831–842. doi: 10.1177/03635465030310061801. [DOI] [PubMed] [Google Scholar]
- 75.von Porat A, Roos EM, Roos H. High prevalence of osteoarthritis 14 years after an anterior cruciate ligament tear in male soccer players: a study of radiographic and patient relevant outcomes. Ann Rheum Dis. 2004;63:269–273. doi: 10.1136/ard.2003.008136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Weldon SM, Hill RH. The efficacy of stretching for prevention of exercise-related injury: a systematic review of the literature. Man Ther. 2003;8:141–150. doi: 10.1016/s1356-689x(03)00010-9. [DOI] [PubMed] [Google Scholar]
- 77.Wroble RR, Moxley DR. The effect of winter sports participation on high school football players: strength, power, agility, and body composition. J Strength Cond Res. 2001;15:132–135. [PubMed] [Google Scholar]
- 78.Young WB, Behm DG. Effects of running, static stretching, and practice jumps on explosive force production and jumping performance. J Sports Med Phys Fitness. 2003;43:21–27. [PubMed] [Google Scholar]
- 79.Zazulak BT, Paterno MV, Myer GD, Romani WA, Hewett TE. A systematic review of the effects of the menstrual cycle on anterior knee laxity in females. Sports Med. 2006;36:847–862. doi: 10.2165/00007256-200636100-00004. [DOI] [PubMed] [Google Scholar]
- 80.Zelisko JA, Noble HB, Porter M. A comparison of men’s and women’s professional basketball injuries. Am J Sports Med. 1982;10:297–299. doi: 10.1177/036354658201000507. [DOI] [PubMed] [Google Scholar]