Abstract
Background
Prospective measures of high knee abduction moment (KAM) during landing identify female athletes at high risk for anterior cruciate ligament injury. Laboratory-based measurements demonstrate 90% accuracy in prediction of high KAM. Clinic-based prediction algorithms that employ correlates derived from laboratory-based measurements also demonstrate high accuracy for prediction of high KAM mechanics during landing.
Hypotheses
Clinic-based measures derived from highly predictive laboratory-based models are valid for the accurate prediction of high KAM status, and simultaneous measurements using laboratory-based and clinic-based techniques highly correlate.
Study Design
Cohort study (diagnosis); Level of evidence, 2.
Methods
One hundred female athletes (basketball, soccer, volleyball players) were tested using laboratory-based measures to confirm the validity of identified laboratory-based correlate variables to clinic-based measures included in a prediction algorithm to determine high KAM status. To analyze selected clinic-based surrogate predictors, another cohort of 20 female athletes was simultaneously tested with both clinic-based and laboratory-based measures.
Results
The prediction model (odds ratio: 95% confidence interval), derived from laboratory-based surrogates including (1) knee valgus motion (1.59: 1.17-2.16 cm), (2) knee flexion range of motion (0.94: 0.89°-1.00°), (3) body mass (0.98: 0.94-1.03 kg), (4) tibia length (1.55: 1.20-2.07 cm), and (5) quadriceps-to-hamstrings ratio (1.70: 0.48%-6.0%), predicted high KAM status with 84% sensitivity and 67% specificity (P < .001). Clinic-based techniques that used a calibrated physician’s scale, a standard measuring tape, standard camcorder, ImageJ software, and an isokinetic dynamometer showed high correlation (knee valgus motion, r = .87; knee flexion range of motion, r = .95; and tibia length, r = .98) to simultaneous laboratory-based measurements. Body mass and quadriceps-to-hamstrings ratio were included in both methodologies and therefore had r values of 1.0.
Conclusion
Clinically obtainable measures of increased knee valgus, knee flexion range of motion, body mass, tibia length, and quadriceps-to-hamstrings ratio predict high KAM status in female athletes with high sensitivity and specificity. Female athletes who demonstrate high KAM landing mechanics are at increased risk for anterior cruciate ligament injury and are more likely to benefit from neuromuscular training targeted to this risk factor. Use of the developed clinic-based assessment tool may facilitate high-risk athletes’ entry into appropriate interventions that will have greater potential to reduce their injury risk.
Keywords: high-risk biomechanics, ACL injury risk factors, targeted neuromuscular training, ACL injury prevention, assessment tools, clinician-friendly
Prospective measures of high knee abduction moment (KAM) during landing predict anterior cruciate ligament (ACL) injury risk in young female athletes.17 In addition, a large-scale prospective study found that military cadets who sustained ACL injury demonstrated knee landing mechanics related to high KAM (D.A. Padua, unpublished data, 2009). Several investigations have demonstrated that female athletes more often exhibit high KAM-related landing mechanics compared with males during landing and pivoting movements.** In validation of these laboratory findings, female athletes often demonstrate knee landing alignments associated with high KAM at the time of injury (Figure 1).4,20,35
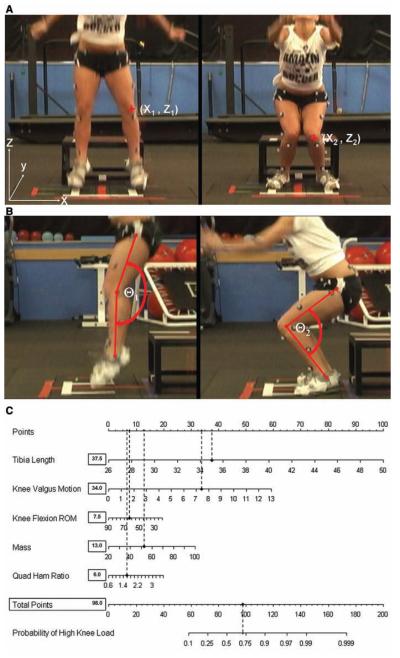
Figure 1.
Videographic depiction of athlete with kinematic pattern that is likely to demonstrate high knee abduction moment (KAM).
Previous reports indicate that increased knee abduction angle, increased relative quadriceps recruitment, and decreased knee flexion range of motion (ROM), concomitant with increased tibia length and body mass normalized to body height that accompanies growth, contribute to approximately 80% of the measured variance in KAM during landing.30 However, expensive biomechanical laboratories, with costly measurement tools that are labor-intensive to test individual athletes, are required to ascertain the measurements. These factors may limit the potential to perform athlete risk assessments on a large scale, further limiting the potential to target high injury–risk athletes with the appropriate intervention strategies. If simpler assessment tools are developed that can be administered in a clinic-based testing environment and are validated by the highly accurate laboratory-based assessment, screening for ACL injury risk could be performed on a more widespread basis. The development of clinic-based assessment tools will improve the potential to identify and target training to female athletes with increased KAM.
The purpose of the current study was to validate a clinic-based landing assessment tool (Figure 2) derived from measures shown to predict KAM with high accuracy.30 We hypothesized that clinic-based measurements would significantly correlate with laboratory-based measurements and that these clinic-based correlates would accurately predict athletes with increased propensity to demonstrate high KAM during landing.
Figure 2.
Clinician-friendly nomogram that was developed from the regression analysis can be used to predict outcome based on tibia length (cm), knee valgus motion (cm), knee flexion range of motion (deg), body mass (kg), and quadriceps-to-hamstring ratio. To use the nomogram, one should place a straight edge vertically so that it touches the designated variable on the axis for each predictor, and record the value that each of the 5 predictors provides on the “points” axis at the top of the diagram. All of the recorded points are then summed and this value is located on the “total points” line with a straight edge. A vertical line drawn down from the total points line to the “probability” line will identify the probability that the athlete will demonstrate high knee abduction moment (KAM) during the drop vertical jump based on the utilized predictive variables. Reprinted from Myer et al31 with permission from Elsevier.
METHODS
Participants
Female basketball and soccer players (N = 5 100; age, 14.0 ± 2.5 years; height, 159.1 ± 9.0 cm; body mass, 53.7.0 ± 12.5 kg) were tested using laboratory-based measurement to confirm the validity of the previously identified correlates to be employed in the clinic-based prediction algorithm to determine high KAM status. To further support the selected surrogate predictors, female basketball, soccer, and volleyball players (N 5 20; age, 15.9 ± 1.3 years; height, 163.6 ± 9.9 cm; body mass, 57.0 ± 12.1 kg) were tested using both laboratory-based and clinic-based techniques simultaneously.
Procedures
The Cincinnati Children’s Hospital Medical Center and Rocky Mountain University of Health Professionals Institutional Review Boards approved the data collection procedures and consent forms. Parental consent and athlete assent were received before data collection. Participants were tested before the start of their competitive basketball or soccer season. The testing consisted of a knee examination, medical history, maturational estimates, dynamic strength, and biomechanical landing analysis.
Anthropometrics and Dynamic Strength
Body mass was measured on a calibrated physician scale. Clinic-based tibia length was measured with a standard measuring tape and was equal to the distance between the lateral knee joint line to the lateral malleous (Figure 3). Isokinetic knee extension/flexion (concentric/concentric muscleaction) strength was measured on a Biodex System II (Biodex Medical Systems, Shirley, New York) and consisted of 10 knee flexion/extension repetitions for each leg at 300 deg/s.26 Quadriceps-to-hamstrings ratio (Quad-Ham) was calculated from hamstrings and quadriceps peak isokinetic torque.
Figure 3.
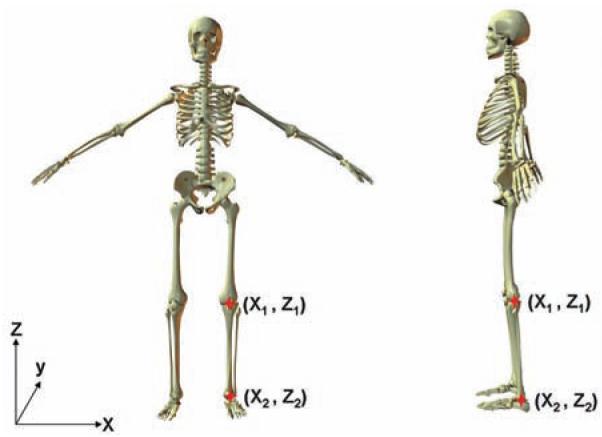
Tibia length was calculated/measured as the distance between knee joint center and ankle joint center (Z2 – Z1). Representative figure created in Poser 6.0 (Smith Micro Software, Watsonville, California).
Laboratory-Based Landing Biomechanics
Three-dimensional (3D) hip, knee, and ankle kinematic and kinetic data were quantified for the contact phase of 3 drop vertical jump (DVJ) tasks. Each participant was instrumented by a single investigator with 37 retroreflective markers placed on the sacrum, left posterior superior iliac spine, sternum, and bilaterally on the shoulder, elbow, wrist, anterior superior iliac spine, greater trochanter, midthigh, medial and lateral knee, tibial tubercle, mid-shank, distal shank, medial and lateral ankle, heel, dorsal surface of the midfoot, lateral foot (fifth metatarsal), and toe (between second and third metatarsals). First, a static trial was conducted in which the participant was instructed to stand still with foot placement standardized to the laboratory coordinate system. This static measurement was used as each participant’s neutral (0) alignment; subsequent kinematic measures were referenced in relation to this position.7 The static standing trial was also used to calculate segment lengths as the estimated distance between the proximal and distal joint center (eg, tibia segment distance was equal to the distance between the knee joint center to ankle joint center [Figure 3]). The DVJ involved the participants standing on top of a box (31 cm high) with their feet positioned 35 cm apart. They were instructed to drop directly down off the box and immediately perform a maximum vertical jump, raising both arms while jumping for a basketball rebound.8
The 3D knee joint angles were calculated according to the Cardan/Euler rotation sequence.6 Ground-reaction force and kinematic data were filtered through a low-pass fourth-order Butterworth filter at a cutoff frequency of 12 Hz to minimize possible impact peak errors.3 Kinematic data were combined with force data to calculate knee joint moments using inverse dynamics.2,40 Net external knee moments are reported in this article and represent the external load on the joint. Knee abduction angle and external abduction moment are represented as negative values based on the analysis convention. The kinematic and kinetic data were exported to MATLAB (MathWorks, Natick, Massachusetts), and the peak knee abduction angle and moment (negative) were identified during the deceleration phase of the initial stance phase of the DVJ. The deceleration phase was operationally defined from initial contact (vertical ground-reaction force first exceeded 10 N) to the lowest vertical position of the body center of mass. Knee valgus motion was calculated as the frontal plane displacement of the knee from initial contact to the end of the deceleration phase of the drop jump landing task (Figure 4). Knee flexion ROM was calculated as the angular displacement of the knee during stance phase of the DVJ (Figure 5). The left-side data were used for statistical analysis. The cut-point used to classify the dependent variable status (high KAM) was .21.74 N ·m of KAM, which was based on published prediction modeling of ACL injury risk prediction and the goal to achieve sensitive prediction of high KAM. Using this classification, participants were dichotomized into high KAM (“yes” or “no”) as the dependent variable.
Figure 4.
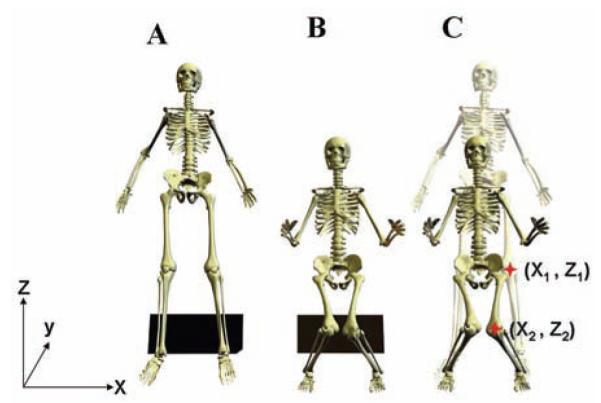
A, example of initial measure of frontal plane knee alignment in participant performing the drop vertical jump. B, example of frontal plane knee alignment taken at maximum knee flexion during landing. C, the calibrated displacement measure between the 2 marked knee alignments (X2 – X1) is representative of the amount of knee valgus motion during the drop vertical jump. Representative figure created in Poser 6.0.
Figure 5.

A, example of initial measure of sagittal plane knee flexion (ϴ1) angle while the participant performs the drop vertical jump. B, example of sagittal plane knee flexion angle taken at maximum knee flexion (ϴ2) during landing. The displacement of knee flexion is found by calculating the differences in knee flexion position between positions (ϴ1 – ϴ2). Representative figure created in Poser 6.0.
Clinic-Based Landing Biomechanics
Clinic-based landing biomechanics were obtained simultaneously with standard video equipment (Panasonic DV camcorder PV-DV601D and PV-GS250, Panasonic, Secaucus, New Jersey) during the 5 recorded trials of DVJ. Landing sequence images were captured from recorded video with Virtual-Dub freeware (www.virtualdub.org) and clinic-based kinematic coordinate data were compiled using ImageJ software (National Institutes of Health, Bethesda, Maryland [http://rsb.info.nih.gov/ij/]). Specifically, ImageJ provided the knee joint center coordinate data in the x-axis. The frontal plane knee coordinate data were assessed at both initial contact and at maximum knee valgus position. These kinematic coordinates were exported to MATLAB, where the difference between coordinate position (x-axis; Figure 4) recorded from the video frame just before initial contact and the coordinate of maximum medial displacement was calculated. The difference measurement between these 2 coordinate data points was calibrated to known distance and used to represent knee valgus motion (medial knee displacement) (Figure 4). The sagittal plane video camcorder view was used to capture knee flexion angles with the ImageJ angle measurement tool. Knee flexion angles were measured in the video frame just before initial contact and maximum knee flexion. Knee flexion range of motion was calculated as the differences in knee flexion between the 2 positions (Y1 – Y2; Figure 5).
Statistical Analyses
Data were exported to SPSS for Windows version 16.0 (SPSS, Chicago, Illinois) and SAS version 9.1 (SAS Institute, Cary, North Carolina) for statistical analyses. Multivariate logistic regression was employed to validate the prediction of high KAM status from the surrogate clinic-based variables. The logistic regression model was estimated using a logit link. The predictive accuracy of the multivariable regression model was quantified with the use of the C statistic, which measures the area under the receiver operating characteristic curve. A P value of <.05 was used as a cut-off for keeping in the model; all variables associated with the outcome bivariately were considered for inclusion in the initial model.
RESULTS
Means and 95% confidence intervals (CIs) for independent variables used in the confirmatory dataset (N = 100 participants) model development are presented in Table 1. The initial prediction of high KAM was performed using logistic regression analysis in a training dataset (N = 598). The prediction model, which included (1) knee valgus motion (odds ratio [OR], 1.59; 95% CI, 1.17-2.16 cm), (2) knee flexion range of motion (OR, 0.94; 95% CI, 0.890°-1.00°), (3) body mass (OR, 0.98; 95% CI, 0.94-1.03 kg), (4) tibia length (OR, 1.55; 95% CI, 1.20-2.07 cm), and (5) quadriceps to hamstrings ratio (1.70: 0.48%-6.0%), predicted high KAM status with 84% sensitivity and 67% specificity (P < .001). This model was predictive of high KAM status with a C statistic of 0.85.
TABLE 1.
Means, 95% Confidence Intervals, and Correlation Coefficients for Independent Predictor Variables Used in the Validation Dataset (N = 100) Model Developmenta
| 95% Confidence Interval for Mean |
||||
|---|---|---|---|---|
| Mean | Lower Bound |
Upper Bound |
Surrogate Predictor Variable Correlation to Primary Predictorb |
|
| Peak knee abduction angle, deg | 11.24 | 10.08 | 12.40 | .40b |
| Knee valgus motion, cmc | 4.15 | 3.74 | 4.55 | |
| Knee flexion ROM, degd | 59.93 | 57.77 | 62.09 | N/A |
| BMI Z-score, no. of SD | 0.34 | 0.17 | 0.52 | .78b |
| Body mass, kgc | 53.66 | 51.18 | 56.14 | |
| Tibia length, cmd | 35.91 | 35.41 | 36.41 | N/A |
| Peak knee extensor moment, N ·m | 97.38 | 90.94 | 103.82 | .26b |
| QuadHam ratioc | 1.54 | 1.45 | 1.62 | |
ROM, range of motion; BMI, body mass index; SD, standard deviations; QuadHam, quadriceps to hamstrings; N/A, not applicable.
Correlation is significant at the .01 level (2-tailed).
Surrogate to laboratory-based predictors employed in clinic-based regression model.
Predictor variables were included in both laboratory-based and clinic-based regression models.
Simultaneous measurement of independent variables using the clinic-based and laboratory-based techniques demonstrated high correlation that ranged from .87 to .98 (P < .001). The correlation between simultaneously captured knee valgus motion captured with a standard video camera in the frontal plane and with laboratory-based motion analysis techniques was r = .87 (Figure 6; P < .001). Figure 7 presents the correlation plot between simultaneously captured knee flexion range of motion captured with a standard video camera in the sagittal plane and with laboratory-based motion analysis techniques, which was r = .95 (P < .001). The plot of clinician-measured tibia length to the tibia length quantified during the static standing trial with laboratory-based motion analysis is shown in Figure 8 (r = .98; P < .001).
Figure 6.
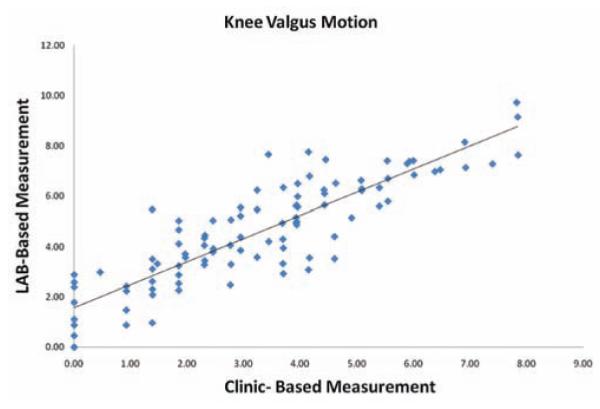
Correlation plot between simultaneously captured knee valgus motion captured with a standard video camera in the frontal plane and with laboratory-based motion analysis techniques.
Figure 7.
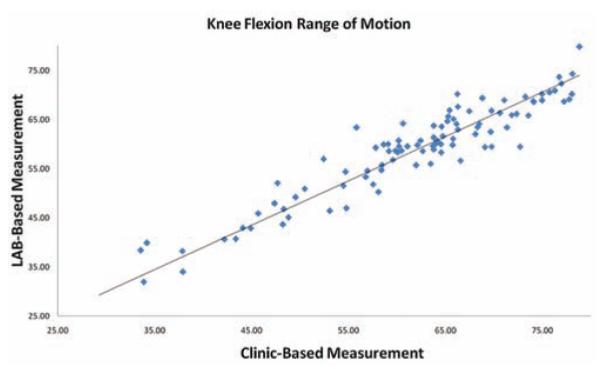
Correlation plot between simultaneously captured knee flexion range of motion captured with a standard video camera in the sagittal plane and with laboratory-based motion analysis techniques during the drop vertical jump.
Figure 8.
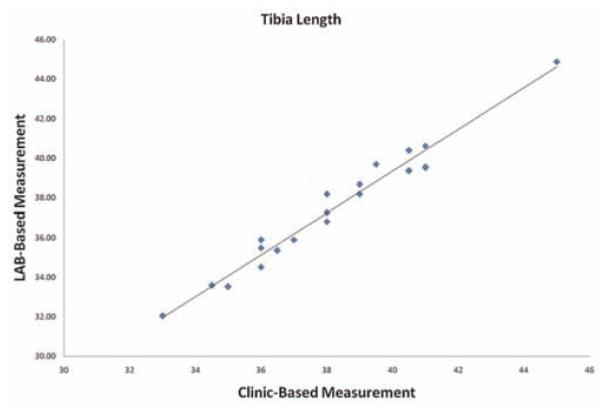
The relationship plot of clinician-measured tibia length to the tibia length quantified during the static standing trial with laboratory-based motion analysis.
DISCUSSION
Use of the laboratory-based measures of high KAM during landing predict ACL injury risk with high sensitivity and specificity in young female athletes.17 Additive to this evidence, a large-scale prospective study of nearly 5700 military cadets found that those who sustained ACL injury demonstrated increased laboratory-based measures related to high KAM at initial contact during the landing phase of a DVJ (D.A. Padua, unpublished data, 2009). Several investigations have demonstrated that female athletes demonstrate a propensity for increased lower extremity alignments related to high KAM compared with males during landing and pivoting movements, which are suggested to be the underlying mechanisms that lead to their increased risk of ACL injury.** Accordingly, associated high KAM alignments are often the reported mechanism associated with ACL injury.4,20,35 Cumulatively, the existing literature indicates that identification and treatment of this modifiable risk factor may ultimately yield the desired reduction of ACL injury incidence in competitive female athletes. However, the procurement of these predictive measures requires cost- and labor-intensive biomechanical laboratory-based measurements that can often only be used to test individual athletes. The current study validates a “clinician-friendly” landing assessment tool (clinic-based) derived from the highly predictive laboratory-based measurements that would be easy to use and would facilitate the potential for widespread use in clinical and field settings.
The clinic-based surrogates provided strong correlation to their laboratory-based parent variables that ranged from .87 to .98. This strong relationship will allow clini-cians to confidently obtain clinic-based measurements and easily employ the provided ACL injury risk algorithm to identify an athlete who will likely demonstrate high KAM and an increased risk for ACL injury (Figure 2).31 The clinician-friendly nomogram that was developed from the regression analysis can be used to predict probability to demonstrate high KAM landing mechanics based on the described clinic-based measures of tibia length (Figure 3), knee valgus motion (Figure 4), knee flexion range of motion (Figure 5), body mass, and QuadHam.
Use of the Prediction Algorithm
To use the prediction nomogram, one should place a straight edge vertically so that it touches the designated variable on the axis for each predictor, and record the value that each of the 5 predictors provides on the “points” axis at the top of the diagram. All of the recorded points are then summed and this value is located on the “total points” line with a straight edge. A vertical line drawn down from the total points line to the “probability” line will identify the probability that the athlete will demonstrate high KAM during the DVJ based on the utilized predictive variables. Figure 9 provides a completed nomogram for the representative participant with the following measurements: tibia length, 35.0 cm; knee valgus motion, 7.4 cm [Figure 9A]; knee flexion ROM, 65.8° [Figure 9B]; body mass, 52.2 kg; QuadHam, 1.55%). On the basis of her demonstrated measurements, this participant would have a 73% chance (98 total points from nomogram scoring) to demonstrate high KAM during the DVJ. Her actual KAM measure for the presented DVJ that was quantified simultaneously with 3D motion analysis was 24.2 N ·m of knee abduction load.
Figure 9.
Example prediction of probability for high knee abduction moment (KAM) from a representative participant’s landing mechanics measured during the performance of a drop vertical jump. A, knee valgus motion during the drop vertical jump is calculated as the displacement measure between the 2 marked knee alignments in the X plane measured at the frame prior to initial contact and the frame with maximum knee flexion (X2 – X1). B, knee flexion range of motion during the drop vertical jump is calculated as the difference in knee flexion angle between initial contact and maximum knee flexion positions (ϴ1 – ϴ2). C, completed nomogram for the representative participant (tibia length, 35.0 cm; knee valgus motion, 7.4 cm; knee flexion range of motion, 65.8°; body mass, 52.2 kg; quadriceps-to-hamstrings ratio, 1.55%). Based on her demonstrated measurements, this athlete would have a 73% chance (98 points) to demonstrate high KAM during the drop vertical jump. Her actual KAM measure for the presented drop vertical jump that was quantified simultaneously with 3D motion analysis was 24.2 N ·m of knee abduction load.
Some clinical settings may not have an isokinetic testing device that is readily available. In this case a surrogate measure of QuadHam can be employed that was defined using linear regression analysis to predict QuadHam based on the athlete’s body mass. The surrogate QuadHam measure can be obtained by multiplying the female athlete’s mass by 0.01 and the resultant value added to 1.10. If further simplicity is desired, the mean value of 1.53 can be substituted into the prediction algorithm for QuadHam.
Algorithmic Approach to Target Neuromuscular Training to High-Risk Athletes
Investigation into the results that relate the underlying mechanics to high KAM have led to the development of specific neuromuscular training interventions designed to reduce risk factors, particularly in female athletes.16,21,28,32,33,38 Initial evidence indicates that these programs are likely to reduce the potential for ACL injury in female athletes.12 However, recent findings also indicate that despite widespread education and institution of ACL injury interventions over the recent years, female athletes who participate in the high-risk sports have not decreased their incidence of injury.1 The disparity between positive laboratory-based results and actual effects on injury outcomes in high-risk female populations suggests a missing link between current research evidence and the appropriate clinical application of interventions. The current investigation provides the critical next step to merge this gap between research findings and clinical practices with the presented clinic-based assessment tool. The simplicity and lessened equipment and labor cost (relative to laboratory-based assessments that may exceed $1000 per athlete) associated with use of this tool may facilitate the identification of high ACL injury–risk athletes on a more widespread basis in clinical and field settings.
Another potential reason for the disparity between the positive laboratory-based reductions in risk factors (eg, reduced KAM) and actual reduced ACL injury incidence outcomes may be related to the difficulty in implementation of the techniques previously found to be successful in altering biomechanics and/or injury risk. Interventions currently used in ACL injury prevention approaches often involve team-based training, which requires large time and space commitments and may be perceived by coaches or players to detract from sport-specific skill training. Such constraints may deter coaches from instituting ACL injury interventions into their preseason or in-season conditioning programs.14,23,34 However, if preseason clinicbased assessment methods as employed in the current study (Figure 9) could identify an athlete who is at high risk for an ACL injury, coaches may be more likely to institute and remain committed to injury prevention programs for the identified high-risk athletes.
An important step for treatment of a particular injury mechanism is the appropriate application of a treatment targeted to the population at risk. Theoretically, through identification of female athletes at greater risk for ACL injury, the number of athletes who would need to be treated to prevent an ACL injury could be substantially reduced. As mentioned previously, the current nontargeted neuromuscular training programs require application to 89 female athletes to prevent 1 ACL injury.11 The current clinic-based assessment tool may drastically increase the efficiency of neuromuscular training if it were to be targeted to high KAM female athletes. The results of the current investigation may aid in the dissemination of assessment techniques required for the application of targeted neuromuscular training intervention to high-risk populations.
Limitations
Anterior cruciate ligament injury in female athletes likely has a multi-factorial origin. Prior epidemiologic data indicate that altered muscular activation or other intrinsic factors (such as anatomical, hormonal, and potentially psychological parameters) may contribute to ACL injury risk, but are not included in the evaluated prediction models. However, the prediction model incorporates the clinically obtainable measures of knee valgus, knee flexion range of motion, body mass, tibia length, and QuadHam that have all been related to increased risk of ACL injury in previous prospective and retrospective epidemiologic reports.4,17,39
Another limitation to consider is that the developed prediction algorithm was influenced for sensitive prediction of high KAM. Although the treatment (neuromuscular training) for high KAM training has very little physical risk, there is the potential psychological and social risk in falsely identifying certain young athletes as being at high risk for ACL injury. It is possible that in some cases, athletes would be less inclined to maintain participation in their sport once they have been identified as high risk. Accordingly, clinicians who employ the current prediction algorithm should be prepared to counsel athletes with a clear message that neuromuscular training may be most effective in those who are classified as high risk, and that neuromuscular training may also provide beneficial adaptations even to those classified as low risk.18,25,27-29,33,37 In addition, clinicians should counsel athletes classified as high risk with the strong evidence that neuromuscular training can reduce their risk of future injury.10,12 Efforts to further validate the currently investigated clinic-based algorithm to determine its reliability and accuracy to predict risk of ACL injury are warranted. Furthermore, future research is needed to delineate the most efficient training methods to target females who demonstrate high KAM landing mechanics to further improve the potential prophylactic effects.
CONCLUSION
Considering the significant short- and long-term debilitation associated with noncontact ACL injury, prevention of such injuries is crucial. The current study addresses the increased potential to reduce ACL injury and potentially the long-term osteoarthritis risk via identification of simple clinical measures that can be used to assess high KAM landing mechanics. Specifically, we have defined clinic-based techniques that use readily available 2-dimensional camcorders in lieu of laboratory-based motion analysis systems to identify athletes with high KAM landing strategies. The resultant clinic-based assessment techniques, in combination with the presented prediction algorithm, allow for low-cost identification of athletes who demonstrate high KAM and are at increased risk of injury. The combined simplicity and accuracy of the presented clinic-based tool may facilitate its use on a widespread basis that would likely increase both the efficacy and efficiency of prevention strategies for noncontact ACL injury among young female athletes.
ACKNOWLEDGMENT
The authors thank the Boone County, Kentucky school district, especially School Superintendent Randy Poe, for participation in this study. We also thank Mike Blevins, Ed Massey, Dr Brian Blavatt, and the athletes of the Boone County public school district for their participation in this study. The authors also acknowledge the Sports Medicine Biodynamics Team, who worked together to make the large data collection sessions possible. Finally, the authors would like to acknowledge Sam Wordeman for his assistance with the use of R-project software and Dr. Mitch Rauh for his helpful advice throughout this investigation.
The authors acknowledge funding support from National Institutes of Health Grants R01-AR049735, R01-AR055563, and R01-AR056259. The Cincinnati Children’s Hospital Medical Center and Rocky Mountain University of Health Professions Institutional Review Boards approved this study.
Footnotes
REFERENCES
- 1.Agel J, Arendt EA, Bershadsky B. Anterior cruciate ligament injury in national collegiate athletic association basketball and soccer: a 13-year review. Am J Sports Med. 2005;33(4):524–530. doi: 10.1177/0363546504269937. [DOI] [PubMed] [Google Scholar]
- 2.Andriacchi TP, Natarajan RN, Hurwitz DE. Musculoskeletal dynamics, locomotion, and clinical applications. In: Mow VC, Hayes WC, editors. Basic Orthopaedic Biomechanics. 2nd ed Lippincott-Raven; Philadelphia, PA: 1997. pp. 37–68. [Google Scholar]
- 3.Bisseling RW, Hof AL. Handling of impact forces in inverse dynamics. J Biomech. 2006;39(13):2438–2444. doi: 10.1016/j.jbiomech.2005.07.021. [DOI] [PubMed] [Google Scholar]
- 4.Boden BP, Dean GS, Feagin JA, Garrett WE. Mechanisms of anterior cruciate ligament injury. Orthopedics. 2000;23(6):573–578. doi: 10.3928/0147-7447-20000601-15. [DOI] [PubMed] [Google Scholar]
- 5.Chappell JD, Yu B, Kirkendall DT, Garrett WE. A comparison of knee kinetics between male and female recreational athletes in stop-jump tasks. Am J Sports Med. 2002;30(2):261–267. doi: 10.1177/03635465020300021901. [DOI] [PubMed] [Google Scholar]
- 6.Cole GK, Nigg BM, Ronsky JL, Yeadon MR. Application of the joint coordinate system to three-dimensional joint attitude and movement representation: a standardization proposal. J Biomech Eng. 1993;115(4A):344–349. doi: 10.1115/1.2895496. [DOI] [PubMed] [Google Scholar]
- 7.Ford KR, Myer GD, Hewett TE. Reliability of landing 3D motion analysis: implications for longitudinal analyses. Med Sci Sports Exerc. 2007;39(11):2021–2028. doi: 10.1249/mss.0b013e318149332d. [DOI] [PubMed] [Google Scholar]
- 8.Ford KR, Myer GD, Hewett TE. Valgus knee motion during landing in high school female and male basketball players. Med Sci Sports Exerc. 2003;35(10):1745–1750. doi: 10.1249/01.MSS.0000089346.85744.D9. [DOI] [PubMed] [Google Scholar]
- 9.Ford KR, Myer GD, Smith RL, Vianello RM, Seiwert SL, Hewett TE. A comparison of dynamic coronal plane excursion between matched male and female athletes when performing single leg landings. Clin Biomech (Bristol, Avon) 2006;21(1):33–40. doi: 10.1016/j.clinbiomech.2005.08.010. [DOI] [PubMed] [Google Scholar]
- 10.Gilchrist J, Mandelbaum BR, Melancon H, et al. A randomized controlled trial to prevent noncontact anterior cruciate ligament injury in female collegiate soccer players. Am J Sports Med. 2008;36(8):1476–1483. doi: 10.1177/0363546508318188. [DOI] [PubMed] [Google Scholar]
- 11.Grindstaff TL, Hammill RR, Tuzson AE, Hertel J. Neuromuscular control training programs and noncontact anterior cruciate ligament injury rates in female athletes: a numbers-needed-to-treat analysis. J Athl Train. 2006;41(4):450–456. [PMC free article] [PubMed] [Google Scholar]
- 12.Hewett TE, Ford KR, Myer GD. Anterior cruciate ligament injuries in female athletes: part 2, a meta-analysis of neuromuscular interventions aimed at injury prevention. Am J Sports Med. 2006;34(3):490–498. doi: 10.1177/0363546505282619. [DOI] [PubMed] [Google Scholar]
- 13.Hewett TE, Ford KR, Myer GD, Wanstrath K, Scheper M. Gender differences in hip adduction motion and torque during a single leg agility maneuver. J Orthop Res. 2006;24(3):416–421. doi: 10.1002/jor.20056. [DOI] [PubMed] [Google Scholar]
- 14.Hewett TE, Lindenfeld TN, Riccobene JV, Noyes FR. The effect of neuromuscular training on the incidence of knee injury in female athletes: a prospective study. Am J Sports Med. 1999;27(6):699–706. doi: 10.1177/03635465990270060301. [DOI] [PubMed] [Google Scholar]
- 15.Hewett TE, Myer GD, Ford KR. Decrease in neuromuscular control about the knee with maturation in female athletes. J Bone Joint Surg Am. 2004;86(8):1601–1608. doi: 10.2106/00004623-200408000-00001. [DOI] [PubMed] [Google Scholar]
- 16.Hewett TE, Myer GD, Ford KR. Reducing knee and anterior cruciate ligament injuries among female athletes: a systematic review of neuromuscular training interventions. J Knee Surg. 2005;18(1):82–88. doi: 10.1055/s-0030-1248163. [DOI] [PubMed] [Google Scholar]
- 17.Hewett TE, Myer GD, Ford KR, et al. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study. Am J Sports Med. 2005;33(4):492–501. doi: 10.1177/0363546504269591. [DOI] [PubMed] [Google Scholar]
- 18.Hewett TE, Stroupe AL, Nance TA, Noyes FR. Plyometric training in female athletes: decreased impact forces and increased hamstring torques. Am J Sports Med. 1996;24(6):765–773. doi: 10.1177/036354659602400611. [DOI] [PubMed] [Google Scholar]
- 19.Kernozek TW, Torry MR, Van Hoof H, Cowley H, Tanner S. Gender differences in frontal and sagittal plane biomechanics during drop landings. Med Sci Sports Exerc. 2005;37(6):1003–1013. [PubMed] [Google Scholar]
- 20.Krosshaug T, Nakamae A, Boden BP, et al. Mechanisms of anterior cruciate ligament injury in basketball: video analysis of 39 cases. Am J Sports Med. 2007;35(3):359–367. doi: 10.1177/0363546506293899. [DOI] [PubMed] [Google Scholar]
- 21.Lephart SM, Abt JP, Ferris CM, et al. Neuromuscular and biomechanical characteristic changes in high school athletes: a plyometric versus basic resistance program. Br J Sports Med. 2005;39(12):932–938. doi: 10.1136/bjsm.2005.019083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Malinzak RA, Colby SM, Kirkendall DT, Yu B, Garrett WE. A comparison of knee joint motion patterns between men and women in selected athletic tasks. Clin Biomech (Bristol, Avon) 2001;16(5):438–445. doi: 10.1016/s0268-0033(01)00019-5. [DOI] [PubMed] [Google Scholar]
- 23.Mandelbaum BR, Silvers HJ, Watanabe D, et al. Effectiveness of a neuromuscular and proprioceptive training program in preventing the incidence of ACL injuries in female athletes: two-year follow up. Am J Sport Med. 2005;33(6):1003–1010. doi: 10.1177/0363546504272261. [DOI] [PubMed] [Google Scholar]
- 24.McLean SG, Huang X, Su A, van den Bogert AJ. Sagittal plane biomechanics cannot injure the ACL during sidestep cutting. Clin Biomech (Bristol, Avon) 2004;19:828–838. doi: 10.1016/j.clinbiomech.2004.06.006. [DOI] [PubMed] [Google Scholar]
- 25.Myer GD, Brent JL, Ford KR, Hewett TE. A pilot study to determine the effect of trunk and hip focused neuromuscular training on hip and knee isokinetic strength. Br J Sports Med. 2008;42(7):614–619. doi: 10.1136/bjsm.2007.046086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Myer GD, Ford KR, Foss KD Barber, Liu C, Nick TG, Hewett TE. The relationship of hamstrings and quadriceps strength to anterior cruciate ligament injury in female athletes. Clin J Sport Med. 2009;19(1):3–8. doi: 10.1097/JSM.0b013e318190bddb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Myer GD, Ford KR, Brent JL, Hewett TE. The effects of plyometric versus dynamic balance training on landing force and center of pressure stabilization in female athletes. Br J Sports Med. 2005;39(6):397. [Google Scholar]
- 28.Myer GD, Ford KR, Brent JL, Hewett TE. The effects of plyometric versus dynamic balance training on power, balance and landing force in female athletes. J Strength Cond Res. 2006;20(2):345–353. doi: 10.1519/R-17955.1. [DOI] [PubMed] [Google Scholar]
- 29.Myer GD, Ford KR, Brent JL, Hewett TE. Differential neuromuscular training effects on ACL injury risk factors in “high-risk” versus “low-risk” athletes. BMC Musculoskelet Disord. 2007;8:39. doi: 10.1186/1471-2474-8-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Myer GD, Ford KR, Khoury J, Succop P, Hewett TE. Biomechanics laboratory-based prediction algorithm to identify female athletes with high knee loads that increase risk of ACL injury. Br J Sports Med. 2010 doi: 10.1136/bjsm.2009.069351. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Myer GD, Ford KR, Khoury J, Succop P, Hewett TE. Clinical correlates to laboratory measures for use in non-contact anterior cruciate ligament injury risk prediction algorithm [published online ahead of print June 4, 2010] Clin Biomech. doi: 10.1016/j.clinbiomech.2010.04.016. doi:10.1016/j.clinbiomech.2010.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Myer GD, Ford KR, McLean SG, Hewett TE. The effects of plyometric versus dynamic stabilization and balance training on lower extremity biomechanics. Am J Sports Med. 2006;34(3):445–455. doi: 10.1177/0363546505281241. [DOI] [PubMed] [Google Scholar]
- 33.Myer GD, Ford KR, Palumbo JP, Hewett TE. Neuromuscular training improves performance and lower-extremity biomechanics in female athletes. J Strength Cond Res. 2005;19(1):51–60. doi: 10.1519/13643.1. [DOI] [PubMed] [Google Scholar]
- 34.Myklebust G, Engebretsen L, Braekken IH, Skjolberg A, Olsen OE, Bahr R. Prevention of anterior cruciate ligament injuries in female team handball players: a prospective intervention study over three seasons. Clin J Sport Med. 2003;13(2):71–78. doi: 10.1097/00042752-200303000-00002. [DOI] [PubMed] [Google Scholar]
- 35.Olsen OE, Myklebust G, Engebretsen L, Bahr R. Injury mechanisms for anterior cruciate ligament injuries in team handball: a systematic video analysis. Am J Sports Med. 2004;32(4):1002–1012. doi: 10.1177/0363546503261724. [DOI] [PubMed] [Google Scholar]
- 36.Pappas E, Hagins M, Sheikhzadeh A, Nordin M, Rose D. Biomechanical differences between unilateral and bilateral landings from a jump: gender differences. Clin J Sport Med. 2007;17(4):263–268. doi: 10.1097/JSM.0b013e31811f415b. [DOI] [PubMed] [Google Scholar]
- 37.Paterno MV, Myer GD, Ford KR, Hewett TE. Neuromuscular training improves single-limb stability in young female athletes. J Orthop Sports Phys Ther. 2004;34(6):305–317. doi: 10.2519/jospt.2004.34.6.305. [DOI] [PubMed] [Google Scholar]
- 38.Pollard CD, Sigward SM, Ota S, Langford K, Powers CM. The influence of in-season injury prevention training on lower-extremity kinematics during landing in female soccer players. Clin J Sport Med. 2006;16(3):223–227. doi: 10.1097/00042752-200605000-00006. [DOI] [PubMed] [Google Scholar]
- 39.Uhorchak JM, Scoville CR, Williams GN, Arciero RA, St Pierre P, Taylor DC. Risk factors associated with noncontact injury of the anterior cruciate ligament: a prospective four-year evaluation of 859 West Point cadets. Am J Sports Med. 2003;31(6):831–842. doi: 10.1177/03635465030310061801. [DOI] [PubMed] [Google Scholar]
- 40.Winter DA. Biomechanics and Motor Control of Human Movement. 2nd ed John Wiley & Sons; New York, NY: 1990. pp. 91–95. [Google Scholar]
- 41.Zeller BL, McCrory JL, Kibler WB, Uhl TL. Differences in kinematics and electromyographic activity between men and women during the single-legged squat. Am J Sports Med. 2003;31(3):449–456. doi: 10.1177/03635465030310032101. [DOI] [PubMed] [Google Scholar]