Abstract
Background
Pelvic organ prolapse is the down ward descent of female organs including the bladder, small and large bowel resulting in protrusion of the vagina, uterus or both. It is a disorder exclusive to women and one of the most common indications for gynecologic surgery.
Methods
This hospital based retrospective descriptive study was conducted to assess the magnitude of pelvic organ prolapse and risk factors for it. All cases of pelvic organ prolapse admitted and treated in Jimma University Specialized Hospital from July 1, 2008 to June 30, 2011 were included. The collected data were analyzed using SPSS computer software version 16.0. Chi-square test was used and was considered to be significant when p<0.05.
Results
Pelvic organ prolapse accounted for 40.7% of major gynecologic operations. Mean age of patients was 42.43 ± 10.4 years and there was a significant association between prolapse and age of patients (p <0.05). Mean parity of patients was 6.5± 2.64 with a significant association between prolapse and parity (p < 0.05). Majority of them (80.6%) lived in rural area and there was a significant association between prolapse and residence area. Farmers accounted for 68.2% of the patients and there was a significant association between prolapse and occupation (p < 0.05). Risk factors identified were chronic cough (20.9%), constipation (30.2%) with some having more than one risk factor while none was identified in 59.7%.
Conclusion
Prolapse is common among rural, farmer, parous and older women where most of them delivered at home with prolonged labor. Age, parity and occupation were associated with the stage of prolapse. Awareness creation on risk factors of pelvic organ prolapse and use of contraception to reduce parity is recommended. Health institution delivery should be advocated to minimize the rate of home deliveries and hence of prolonged labor.
Keywords: Pelvic organ prolapse, uterovaginal prolapse, vaginal hysterectomy
Introduction
Pelvic organ prolapse (POP) also called urogenital prolapse is down ward descent of the female pelvic organs including the bladder, post hysterectomy vaginal cuff and the small or large bowel resulting in protrusion of the vagina, uterus or both. Cystocele is the anterior vaginal wall prolapse accompanied by prolapse of the bladder wall. Rectocele is the prolapse of the lower posterior vaginal wall with the rectum. Sometimes, there can be a prolapse of the posterior fornix into the vagina which usually contains the intestine and this is known as enterocele. POP is the third most common indication for hysterectomy. Loss of vaginal or uterine support in women presenting for a routine gynecologic care is seen in up to 43–76% of patients with 3–6% having descent beyond the hymen (1).
Completely prolapsed uterus can undergo ulceration and become infected where the patient may complain of frequency of micturition, stress incontinence, difficulty of passing urine, low back pain, a feeling of something down and chronic discharge. Usually symptomatic women living in more developed countries who actively seek medical help are studied and reported as case control series of hospital population. But few studies from less developed countries suggest that POP in African women may occur at younger age. Loss of vaginal or uterine support in women presenting for routine gynecological checkup is seen in up to 43.8% of patients with a life time risk of 11.1% for prolapse or incontinence surgery by the age of 80 years for women in high income countries (1, 2).
POP can severely affect a woman's quality of life by limiting physical, social, psychological and sexual function. It is estimated that 50% of parous women lose pelvic floor support and subsequently develop a prolapse. However, only 20% of these women are symptomatic (3, 4).
High parity is the single most important risk factor for prolapse in rich and poor women in both more and less developed countries. Not only the number of vaginal deliveries but also other obstetric factors related to the individual delivery such as prolonged second stage or poor surgical repair of perineal injury, improper orientation towards labor process, inappropriate fundal pressure, delivering in squatting position, mismanagement of third stage of labor with excessive traction contributing for the weakening of the supporting structure have been implicated. Other factors such as low levels of estrogen in post menopausal women, obesity, smoking and constipation also contribute to the development of POP (2).
In 1996, International Continence Society defined a system of pelvic organ prolapse quantification (POP-Q) demonstrating high inter and intra observer reliability. It allows researchers to report findings in standardized, easily reproducible fashion. Prolapse in each segment is measured relative to the hymen, which is a fixed anatomic landmark that can be identified consistently. Accordingly, it is stage one when the leading prolapsed part is more than one centimeters above the hymenal ring; stage two when it is between one centimeter above and one centimeter below the hymenal ring; stage three when it is more than one centimeter below the hymenal ring but less than total vaginal length (TVL) minus two centimeters, and stage four if it is more than (TVL-2) cm below the hymenal ring (5).
The degree of prolapse has traditionally been the main determinant in the management of POP with less attention given to symptom severity and its impact on quality of life. However, these are important considerations in the management of women with POP. Many women with POP are asymptomatic and don't need treatment. When prolapse is symptomatic options include conservative management and surgery. Surgical strategies for prolapse can be categorized broadly by reconstructive and obliterative techniques (6, 7, 8).
A cross sectional study conducted in Ejura-Sekyidumasi, Ashanti region in rural Ghana showed that POP was observed in 21 (12.1%) women and 17 (81%) of these women were symptomatic. The mean age of the women was 45.5± 18.5 years (range 24–80) and the mean parity of the women was 5.2± 2.4. The categories of POP observed in the women were 8 (38.1%) with anterior vaginal wall prolapse, 2 (9.5%) with posterior vaginal wall prolapse, 3 (14.3%) women with both anterior and posterior vaginal wall prolapse, 8 (38.5%) women with anterior, posterior and uterine prolapse. Five (23.8%) of the women were with stage-I, 7 (33.3%) with stage-II, 5 (23.8%) with stage-III and 4 (19%) with stage-IV. The most common symptom reported by the women was “something falling out of the vagina” (9).
Community based reproductive health survey was conducted in Farafenni town, Gambia between January and July 1999 where uterovaginal prolapse (UVP) was present in 46% of the women. The types of genital prolapse include anterior only (47%), anterior and posterior (20%), posterior only (16%), anterior and uterine (7%), anterior, posterior and uterine (6%), posterior and uterine (4%). Fifteen percent of the women were found to have symptomatic POP warranting surgical intervention (10).
In Ethiopia data concerning prevalence and associated risk factors of POP are not available as to the best knowledge of the authors except the one conducted 16 years ago where a three years retrospective study from June 12, 1989 to June 12, 1993 was conducted in Gandhi memorial hospital, Addis Ababa and Gondar hospital, Ethiopia which showed that UVP accounted for 19.9 % in Gondar as compared to 17.2% at Gandhi memorial hospital. The mean ages for Gondar and Gandhi memorial hospital subjects were 38.09 ±11.52 and 42.17±13.16 years, respectively. Mean parity of 5.6 ±2.7 children and 5.4 ± 2.6 children have been reported for Gondar and Gandhi Memorial groups, respectively. Of the 125 housewives from the Gondar group, 114 (92.2%) were from the rural area where as the Gandhi memorial group revealed that 143 (90.5%) out of 158 subjects were rural housewives. The symptoms and signs of both centers were various and dependent on degrees of prolapse and the mean durations were 2.8 years ± 2.9 years for Gondar and 2.4 years ± 2.4 years for Gandhi memorial hospital, respectively. The Gondar population was homogenous and the bulk is made of Amharas (88.5 %) followed by Tigreans (10.9%). In contrast the Gandhi memorial hospital study population was heterogeneous and made up of Guraghes (33.3%), Amharas (32.2%), and Oromos (27.2%). The preoperative and post-operative hospital stays for Gondar were 7.7 days ± 4.9 days and 10.9 days ± 3.4 days, respectively while for Gandhi memorial hospital they were 12.4 days ± 6.1 days and 11.2 days ± 3.7 days. Average operation time for the Gondar study was 72.73 minutes ± 13.17 minutes as compared to the Gandhi memorial hospital which was 91.67 minutes ± 30.56 minutes (2).
There is gap of up to date information on POP in our country. As the only already existing study was done long time ago, there is a need to update information on the problem. The aim of this study is to assess the magnitude of POP and common risk factors for it in Jimma University Specialized Hospital (JUSH).
Patients and Methods
This hospital-based retrospective descriptive study was conducted in Jimma university specialized hospital (JUSH). Data were collected from cases managed between July 1, 2008-June 30, 2011. JUSH is located in Jimma city, south west of Ethiopia. The hospital serves as a referral hospital for the south-western sub-region of the country and is a training center for different cadres of health professionals and it has different departments and follow-up clinics for chronic illnesses. The department of obstetrics and gynecology is one of the departments in the hospital giving services at different areas. The service delivery sites are outpatient department, gynecology ward, maternity and labor ward, and operation rooms (OR). Gynecology ward is divided into three main divisions: septic ward where patients with infection are treated; aseptic ward where elective cases are admitted, and fistula ward where fistula patients are admitted and treated. The gynecology ward is run by clinical nurses, medical and health officer interns, obstetrics and gynecology residents, and obstetrics and gynecology consultants.
All the patients who were admitted and operated in gynecology ward during the study period were used as the source population. All the patients with POP who were admitted and treated during the study period were included and no sampling technique was employed.
Card numbers of patients with POP admitted to gynecology ward for treatment were retrieved from log books at gynecology outpatient department, admission office, discharge book and operation room book. The card numbers were given to record officers and the charts were retrieved and data were collected. Data collectors (medical interns working in the department of obstetrics and gynecology during the data collection time) were trained on each item included in the questionnaire, its meaning and how to retrieve data from records. Data on socio-demographic variables, past reproductive performances, presenting complaints, associated symptoms and signs, risk factors, investigations before surgery, surgeries done, and complications were collected. During data collection the completeness was checked on the spot and corrected by cross checking the card. Data were cleaned, entered and analyzed using computer software SPSS version 16.O and Chi-square test was used and was considered to be significant when p<0.05. Prior to the data retrieval from individual records permission was obtained from JUSH. Confidentiality was kept throughout the study by using code numbers for each chart retrieved to avoid using names of patients from charts and charts were returned back to the record office after the research was completed. As the study was done on review of records some records were incomplete, some missing, and some hand writings were ineligible.
Results
From the total of 143 POP patient cards, complete data were retrieved from 129 cards which was 90.2% retrieval rate. The magnitude of POP out of the major gynecologic operations done in JUSH during the study period was 40.7%. The study population was composed of Oromos (72.9%), Keffa (14%), Amhara (4.7%) and 11 patients' ethnicities were not documented. Ninety nine (82.5%) of them were married, 14.2% were widowed and 3.3% were divorced (Table 1).
Table 1.
Socio-demographic characteristics of patients with UVP in JUSH, Jimma, Ethiopia from July 1, 2008– June 30, 2011.
| Sociodemographic variables |
Number | % |
| Age (years) | ||
| 15–24 | 5 | 3.9 |
| 25–34 | 22 | 17.1 |
| 35–44 | 41 | 31.8 |
| 45–55 | 43 | 33.3 |
| >55 | 18 | 14 |
| Total | 129 | 100 |
| Ethnicity | ||
| Oromo | 94 | 79.7 |
| Keffa | 18 | 15.3 |
| Amhara | 6 | 5 |
| Total | 118 | 100 |
| Occupation | ||
| Farmer | 88 | 68.2 |
| House wife | 33 | 25.6 |
| Merchant | 6 | 4.7 |
| Employed | 2 | 1.6 |
| Total | 129 | 100 |
| Marital status | ||
| Married | 99 | 82.5 |
| Divorced | 4 | 3.3 |
| Widowed | 17 | 14.2 |
| Total | 120 | 100 |
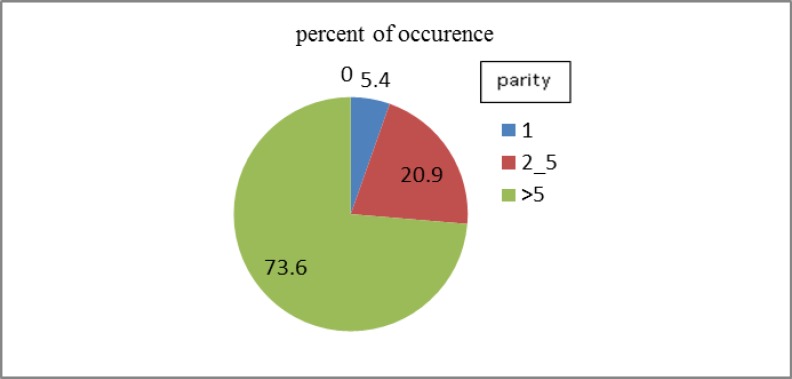
The mean age of women with POP was found to be 42.43 ± 10.4 years (range 22–72) and there was statistically significant association between stage of UVP and age of patients (p < 0.05) (Table 2). Majority (73.6%) of patients with UVP were of parity > 5 (Fig. 1) with mean parity of 6.5 ± 2.64 (range 1–14) and there was statistically significant association between the stage of UVP and parity (p<0.05) (Table 3). Eighty point six percent of UVP patients live outside Jimma city and there was statistically significant association between the stage of UVP and residence area of the patients. Most (97.7%) of the cases delivered their babies at home. Farmers, house wives, merchants, and employed ones account for 68.2%, 25.6%, 4.7% and 1.6%, respectively (Table 1). There was a significant association between UVP and occupation of the patients (p < 0.05) (Table 4).
Table 2.
Association of age with stage of UVP in JUSH, Jimma, Ethiopia from July 1, 2008–June 30, 2011.
| Age (years) | Stage of UVP | Total | p-value | |
| 3 | 4 | |||
| 15 –24 | 2 | 3 | 5 | |
| 25–34 | 18 | 4 | 22 | |
| 35–44 | 22 | 19 | 41 | 0.036 |
| 45–55 | 24 | 19 | 43 | |
| >55 | 6 | 12 | 18 | |
| Total | 72 | 57 | 129 | |
Age range (22–72), Mean age = 42.43 ± 10.04, X2 = 10.305, df=4, p < 0.036
Figure 1.
Parity of patients with UVP in JUSH, Jimma, Ethiopia from July 1, 2008 – June 30, 2011.
Table 3.
Parity of women versus stage of UVP in JUSH, Jimma, Ethiopia July 1, 2008– June 30, 2011.
| Stage of UVP | p-value | |||
| Parity | 3 | 4 | Total | |
| I | 4 | 3 | 7 | |
| II–V | 21 | 6 | 27 | 0.033 |
| >V | 47 | 48 | 95 | |
| Total | 72 | 57 | 129 | |
Parity range (1–12), Mean = 6.50 ± 2.64
Table 4.
Address and occupation of women versus stage of UVP in JUSH, Ethiopia from July 1, 2008– June 30, 2011.
| Address | Stage of prolapse | Total | p-value | |
| 3 | 4 | |||
| Address | ||||
| Out of Jimma | 53 | 51 | 104 | 0.024 |
| Jimma | 19 | 6 | 25 | |
| Total | 72 | 57 | 129 | |
| Occupation | ||||
| House wife | 12 | 21 | 33 | |
| Farmer | 53 | 35 | 88 | 0.027 |
| Merchant | 5 | 1 | 6 | |
| Employed | 2 | 0 | 2 | |
| Total | 57 | 52 | 129 | |
All patients with UVP in JUSH came with presenting complaint of mass per vagina. Some of the additional symptoms were urinary incontinence (20.2%), coital difficulty (17.1%), failure to pass feces (14.7%) and ulcer (9.3%). The mean duration of symptoms was 3.11 years ± 3.02 years (range 0.08 – 10 years).
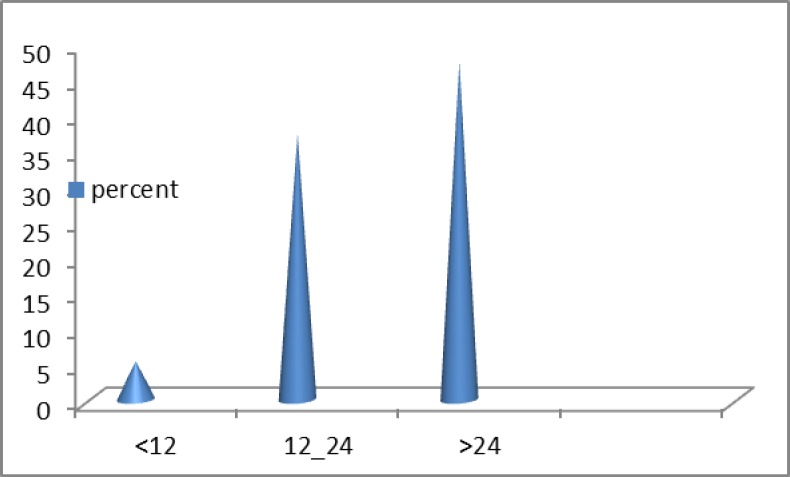
The maximum duration of labor in women with UVP in JUSH was more than 24 hours in 47.3% of the cases (Fig. 2). Other risk factors identified were chronic cough in 20.9% of patients, constipation in 30.2%, while 59.7% of them had no identifiable risk factors. On the other hand 72 (55.8%) had stage three, 57 (44.2%) had stage four UVP while 98.4% had associated cystocele, 16.3% rectocele, 1% urethrocele and 0.8% vaginal vault prolapse. The pre-operative and post-operative haematocrit levels were 39.17± 4.37 (range 24–47) and 33.5± 4.6 (range 19–41), respectively.
Figure 2.
Maximum duration of labor in patients with UVP in JUSH, Jimma, Ethiopia from July 1, 2008–June 30, 2011.
The major operations performed for patients with UVP in JUSH during the study period were vaginal hysterectomy with anterior colporrhaphy and vaginal hysterectomy with anterior colporrhaphy and posterior colpoperinorrhaphy, 76.7% and 14.3%, respectively while the remaining had vaginal hysterectomy with sacrospinous fixation and Manchester operation. The average operation time for the surgeries was 89.49 minutes ± 22.85 minutes (range 50–160) and the average creatinine value for the study group was 0.86± 0.35 (range 0.3–2.38).
On the other hand one patient had previous operation for UVP and re-operated for vault prolapse and three patients had transfusion with one unit of blood each. Furthermore, one patient developed acute abdomen secondary to adhesion and vaginal cuff cellulites on the fifth and tenth post operation day, respectively. Another patient developed vaginal cuff cellulites on the third post operation day. One patient had associated cervical cancer and no death was reported. The pre-operative and post-operative stay for the study group were 9.5 days± 4.5 days (range 2–29) and 5.23 days ± 1.83 days (range 2–16), respectively.
Discussion
The study revealed that 72.9% of the patients who were operated for UVP in JUSH were Oromo and 76.7% were married as compared to the study in Gondar where 88.5% were Amharas and 90.4% were married while in the Gandhi Hospital the study population were rather heterogenous of Guraghes 33.3% and 32.2 % were Amharas, 27.2 % were Oromos and 84.1% were married. This could be attributed to the study setting.
The mean age of women with UVP is found to be 42.43 ± 10.04 which is consistent with other studies conducted in Gondar and Ghandi memorial hospital with 38.09 ± 11.52 and 42.17 ± 13.16 years, respectively. The mean parity of the study group was 6.50 ± 2.64 children which is comparable to that of Gondar and Ghandi memorial hospital study 4.6 ± 2.5 children and 5.9 ± 2.7 children, respectively. This study also showed that 80.6% of the patients came from areas outside Jimma city and 68.2% were farmers and 97.7 % delivered their babies at home.
The maximum duration of labor in women with UVP in JUSH was more than 24 hours in 47.3%, 12–24 hrs in 37.2% and 5.4 % took less than 12 hours and it appears that most of the patients who had UVP in JUSH have had prolonged labor. This study also demonstrated that UVP affects younger age group of women in Ethiopia than their counter parts in the developed countries and this may be due to various obstetric factors like delivering at home with long duration of labor and high parity.
This study showed that most of the cases were rural women farmers and it is traditionally assumed that assisting in farmland, marketing, wood and water fetching, child rearing and carrying the baby on the back, grinding are some of the physically demanding day to day activities which are assigned to rural women farmers even during pregnancy and puerperium which have detrimental effect for the loss of genitourinary supporting structures. The study also showed that mean duration of symptoms was 3.11±3.02 years, which is comparable with the Gondar and Gandhi study groups 2.8±2.9 years and 2.4±2.2 years, respectively.
The pre-operative hospital stay for the study group were 9.5± 4.5 days which is fairly consistent with the Gondar and Gandhi studies which were 7.7±4.9 days and 12.4±6.1 days, respectively. The post-operative hospital stay for JUSH was 5.23±1.83 days which is relatively lower than the Gondar and Gandhi 10.9±3.4 days and 11.2±3.7 days, respectively. This may be due to the type of operation performed and specific protocol of patient discharge which was used at the different hospitals.
The study also showed the most commonly practiced operation for women with uterovaginal prolapse was vaginal hysterectomy and anterior colporrhaphy with or without posterior colpoperinorrhaphy (91%) which is different from the Gondar study which was 0% and in the Gandhi study VH+AC±PCPR was done in 44.6 %. In Gondar they practiced vaginal hysterectomy with plastic surgery most and this may be due to operators' skill or preference and availability of mesh and tapes.
The study also revealed that the average operation time for the study group was an 89.49±22.85 minute which is comparable with the Gandhi group 91.67±30.56 minutes. There was only one (0.8%) recurrence recorded in JUSH as compared to the Gandhi study, 4(2.1%) and this could be as a result of the operation type performed.
The pre-operative and post-operative hematocrit levels for Jimma patients were 39.17% ± 4.57% and 33.5% ± 4.6% ,respectively which is similar to the Gondar (39.03 ± 4.1 and 33.03% ± 3.8%, respectively) and the Gandhi studies (39.62% ± 4.96% and 33.37% ± 4.57%, respectively).
The study also showed that 20.3% of the women had additional urinary incontinence which is higher than the Gondar population which was 10%. However, it is three times lower than the Gandhi population (57.1%) and this may be due to diagnostic capacity. In this study group 9.3% of the subjects had decubitus ulcer which is much lower than the Gandhi study group (35.7%) and this could be from early presentation for treatment of the cases in Gandhi while the cases in JUSH were coming for treatment after the decubitus ulcer has healed.
In conclusion, UVP is one of the major gynecologic problems in older rural women farmers with high parity where most physical demanding chores are allocated. In addition, most of the women with UVP delivered at home with prolonged labor and stage of UVP has been found to have association with age, parity and occupation. The common presenting complaint of the patients was mass per vaginum. The most commonly performed surgery was vaginal hysterectomy and anterior colporrhaphy with or without posterior colpoperinorrhaphy.
Awareness creation on risk factors of pelvic organ prolapse and use of contraception to reduce parity is recommended. Health institution delivery should be advocated to minimize the rate of home deliveries and hence of prolonged labor. The record keeping in JUSH be improved and simplified.
Acknowledgments
We would like to pass our deepest appreciation to patients whose records were used for the purpose of the study, data collectors, Jimma University for funding, and Professor Lukman Yusuf for providing references and other relevant information.
References
- 1.Jelovsek C Maher, Barber Matthew D. Pelvic organ prolapse. Lancet. 2007;369:1027–1038. doi: 10.1016/S0140-6736(07)60462-0. 2007. [DOI] [PubMed] [Google Scholar]
- 2.Lukman Y. Utero vaginal prolapse a rural disability of the young. East Afr Med journal January. 1995;72(1):1–9. [PubMed] [Google Scholar]
- 3.Mant J, Painter R, Vessey M. Epidemiology of genital prolapse: observations from the Oxford Family Planning Association Study. Br J Obstetrics and Gynecology. 1997;104(5):579–585. doi: 10.1111/j.1471-0528.1997.tb11536.x. [DOI] [PubMed] [Google Scholar]
- 4.Beck RP. Pelvic relaxational prolapse. In: Kase NG, Weingold AB, editors. Principles and Practice of Clinical Gynecology. New York: John Wiley and Sons; 1983. pp. 677–685. [Google Scholar]
- 5.Daneshgari Firouz, Moore Courtney K. Female urology. 3rd ed. Philadelphia: Elsevier Saunders; 2008. Epidemiology of pelvic organ prolapse; pp. 1022–1027. chapter 51. [Google Scholar]
- 6.Schorge John O, Schaffer Joseph I, Halvorson Lisa M, Hoffman Barbara L, Bradshaw Karen D, Cunningham F Gary. Williams gynecology. McGraw-Hill Companies; 2008. Pelvic organ prolapse. chapter 24. [Google Scholar]
- 7.Chiaffarino F, Chatenoud L, Dindelli M, et al. Reproductive factors, family history, occupation and risk of urogenital prolapse. Eur J Obstetrics & Gynecology and Reprod Biol. 1999;82(1):63–67. doi: 10.1016/s0301-2115(98)00175-4. [DOI] [PubMed] [Google Scholar]
- 8.Burrows LJ, Meyn LA, Walters MD, Weber AM. Pelvic symptoms in women with pelvic organ prolapse. Obstetrics and Gynecology. 2004;104(5 Pt 1):982–988. doi: 10.1097/01.AOG.0000142708.61298.be. [DOI] [PubMed] [Google Scholar]
- 9.Wusu-Ansah Osei K, Opare-Addo Henry S. Pelvic organ prolapse in rural Ghana. International journal of Obstetrics and gynecology. 2008;103:121–124. doi: 10.1016/j.ijgo.2008.06.014. [DOI] [PubMed] [Google Scholar]
- 10.Scherf C, Morison L, Fiander A, Ekpo C, Walraven G. Epidemiology of pelvic organ prolapse in rural Gambia, West Africa. BJOG. 2002 Apr;109(4):431–436. doi: 10.1111/j.1471-0528.2002.01109.x. [DOI] [PubMed] [Google Scholar]