SYNOPSIS
Objectives
Unintentional, non-fire-related (UNFR) carbon monoxide (CO) poisoning is a leading cause of poisoning in the United States. A comprehensive national CO poisoning surveillance framework is needed to obtain accurate estimates of CO poisoning burden and guide prevention efforts. This article describes the current national CO poisoning surveillance framework and reports the most recent national estimates.
Methods
We analyzed mortality data from the National Vital Statistics System multiple cause-of-death file, emergency department (ED) and hospitalization data from the Healthcare Cost and Utilization Project's Nationwide Emergency Department Sample and Nationwide Inpatient Sample, hyperbaric oxygen treatment (HBOT) data from HBOT facilities, exposure data from the National Poison Data System, and CO alarm prevalence data from the American Housing Survey and the National Health Interview Survey.
Results
In the United States, 2,631 UNFR CO deaths occurred from 1999 to 2004, an average of 439 deaths annually. In 2007, there were 21,304 (71 per one million population) ED visits and 2,302 (eight per one million population) hospitalizations for confirmed cases of CO poisoning. In 2009, 552 patients received HBOT, and from 2000 to 2009, 68,316 UNFR CO exposures were reported to poison centers. Most nonfatal poisonings were among children (<18 years of age) and females; hospitalizations and deaths occurred more frequently among males and elderly people (>65 years of age). More poisonings occurred during winter months and in the Midwest and Northeast.
Conclusions
UNFR CO poisoning poses a significant public health burden. Systematic evaluation of data sources coupled with modification and expansion of the surveillance framework might assist in developing effective prevention strategies.
Unintentional, non-fire-related (UNFR) carbon monoxide (CO) poisoning is a leading cause of poisoning in the United States.1 Exposure to CO results in nearly 450 deaths, more than 2,000 hospitalizations, and more than 20,000 emergency department (ED) visits annually.1–3 CO is a colorless and odorless gas that is produced due to the incomplete combustion of hydrocarbons. Major nonoccupational sources include poorly maintained and poorly ventilated home heating systems and cooking appliances, motor vehicle exhaust, and fuel-powered equipment (e.g., generators and space heaters).4 Low-level CO exposure can cause flu-like symptoms, such as fatigue, headache, dizziness, nausea, vomiting, and confusion. High-level exposure can cause more severe effects, such as disorientation, collapse, coma, cardiorespiratory failure, and death.5,6 Approximately 15%–49% of CO poisoning cases develop neurocognitive sequelae, including impaired memory and executive functions.7–10 However, the nonspecificity of symptoms often leads to mis- or underdiagnosis of CO poisoning.11,12
Most CO exposures occur in residential settings and are preventable.1,11 Installation of a battery-powered or battery-backup CO alarm, as well as proper maintenance of home heating systems and cooking appliances, can prevent CO poisonings.11,13
Conducting CO poisoning surveillance is an integral part of prevention efforts. Surveillance data are critical in characterizing the populations at risk and developing effective public health interventions and prevention messages. A comprehensive national CO poisoning surveillance framework is needed for accurate estimation of the public health burden and to develop sustainable, evidence-based standards for data collection and integration of scientifically valid data on exposure, health outcome, and interventions.14 This article describes the current framework under which CO poisoning surveillance is conducted and reports the most recent published estimates from these nationwide surveillance data.
METHODS
Conceptual framework
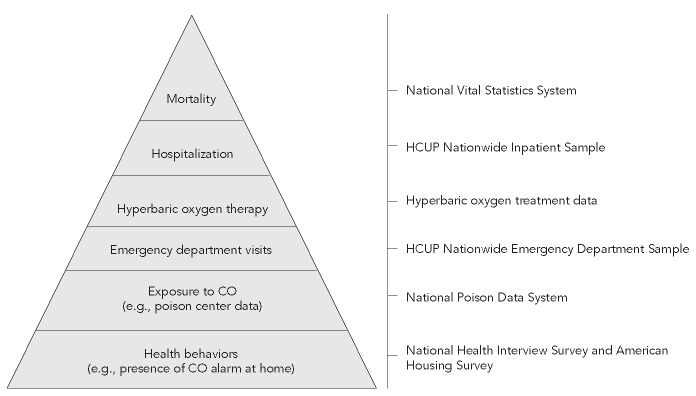
Conducting and prioritizing surveillance of a specific health outcome are guided by factors that include frequency of events, severity of outcome, preventability of exposures, and effectiveness of simple preventive measures.14 Surveillance of UNFR CO poisoning is important and appropriate as it poses a substantial public health burden (e.g., 71 ED visits and eight hospital stays per one million population [hereafter, per million]) and economic burden (e.g., direct health-care cost of hospitalization for confirmed cases of CO poisoning was more than $26 million in 2007).1–3 As stated previously, exposure to CO can cause death and long-term disability.2,7–10 Prevention messages are fairly simple and can be communicated to the public easily. CO alarms can prevent many CO poisoning cases and typically cost $25–$50.11,13 In comparison, the average cost of hospitalization for CO poisoning is more than $11,000.3 The public health importance of CO poisoning is highlighted in Healthy People 2020; CO poisoning surveillance is included as one of the environmental health priority areas (Objective EH-22.7).15 Figure 1 illustrates the parameters by which CO poisoning can be considered a critical health issue for public health surveillance.
Figure 1.
Parameters to assess the public health importance of CO poisoning surveillance
aModified from: Teutsch SM, Churchill RE. Principles and practice of public health surveillance. 2nd ed. New York: Oxford University Press, Inc.; 2000.
CO = carbon monoxide
In the absence of an active national surveillance system for CO poisoning, national estimates and surveillance activities rely on secondary data sources. The National Vital Statistics System, the National Electronic Injury Surveillance System—All Injury Program, and reports from hyperbaric oxygen treatment (HBOT) facilities have all previously been used for national surveillance of CO-related mortality and morbidity.1–3,16 None of these data sources was primarily designed for CO poisoning surveillance, and data collected for purposes other than surveillance of the health outcome in question may not be sufficient and may suffer limitations in timeliness, availability, completeness, quality, and representation.17–19
In addition to collecting health outcome data, an ideal environmental health surveillance system includes components that enable us to develop a more complete picture of population health status in terms of hazards, exposure, health effects, and intervention;20 surveillance of environmental public health issues has often been described in this “hazard-exposure-outcome” axis context.17 The development of a national CO poisoning surveillance framework was based on a similar public health paradigm but modified to focus on health behavior, exposure, and health outcome. This modification was warranted by the significant role of individual-level high-risk behaviors that often lead to CO-related morbidity and mortality (e.g., no CO alarms at home or improper generator use). As surveillance efforts are expected to couple with specific public health action,14 it is important to identify all opportunities for intervention while developing a comprehensive surveillance framework that captures a range of data including high-risk health behaviors, morbidity, and mortality. Intervention opportunities might focus on areas such as modification of health behavior, education and awareness, improved medical management, or reduction in health-care cost.
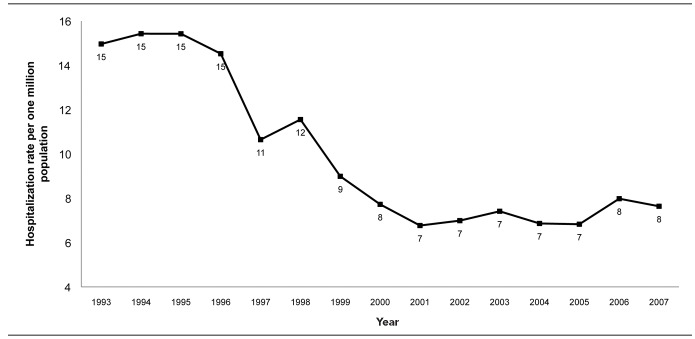
For the purpose of this article, “CO surveillance framework” is defined as a framework that guides the overall approach to surveillance, including the selection of data sources and surveillance components (e.g., health outcome, mortality, and health behavior), of a particular public health topic—in this case, CO poisoning. Development of a framework is important for comprehensive burden estimates, identification of high-risk groups, and guiding public health efforts. Development of the CO poisoning surveillance framework included (1) selecting surveillance components, (2) identifying appropriate data sources, (3) establishing/identifying a standard case definition for each component, (4) generating national estimates, and (5) disseminating findings. Surveillance components were chosen according to a classical “disease pyramid” structure, where the burden is measurable, a routine national data source for the component is available, and surveillance could guide or spur public health action for reduction of risk or health burden. When multiple data sources were available, the selection of the most appropriate data source for surveillance was based on factors including sample size, data validity and reliability, and representativeness.2 Strengths and limitations of the data sources have been described elsewhere.1–3 It was not always possible to use a standard case definition for each surveillance component, as they either did not exist or did not fit the variable definitions or parameters provided by the data sources. Sometimes the standard case definition was modified or established by subject-matter experts. The case definitions for each of the components are described in the article. Age-specific population denominator data from the U.S. Census were used to generate national rates. The surveillance framework described in this article focuses only on UNFR CO poisonings, because the approaches to preventing intentional and fire-related CO exposures greatly differ. Figure 2 illustrates the surveillance components of the framework, along with the respective data sources currently in use for national CO poisoning surveillance.
Figure 2.
National surveillance framework for unintentional, non-fire-related CO poisoning in the United States
CO = carbon monoxide
HCUP = Healthcare Cost and Utilization Project
Case definition
There is no standard clinical case definition for CO poisoning, owing to the wide array of presenting symptoms, varying correlation between carboxyhemoglobin (COHb) levels and health effects, and qualitative differences in data sources (e.g., exposure data from poison centers and administrative coded data from hospitals). In 1998, the Centers for Disease Control and Prevention (CDC)-sponsored national CO Surveillance Workgroup developed the Council of State and Territorial Epidemiologists' (CSTE) “Surveillance Case Definition for Acute Carbon Monoxide Poisoning” to create a nationally consistent measure for CO poisoning and exposure. It was updated in 2007 to be more inclusive and expansive and is widely used for surveillance.2,3,21,22 This case definition was based on International Classification of Diseases (ICD) codes (ICD, ninth revision [ICD-9] and 10th revision [ICD-10] codes used in clinical diagnoses, hospital discharge, death certificates, or clinical procedures), clinical signs and symptoms, laboratory results for COHb, exposure history, and information collected by poison centers and HBOT facilities. According to this definition, acute CO poisoning cases can be categorized into three types: confirmed, probable, and suspected. This case definition includes intentional and fire-related CO exposures. Figure 3 summarizes the CSTE case definition for acute CO poisoning,21 which has been used for UNFR CO-related mortality, ED visits, and hospitalization surveillance.2,3 It has also been used with poison center and HBOT data for CO poisoning surveillance after disasters.22 A more conservative case definition (i.e., only including principal diagnosis of ICD-9 code 986 without any classification of case types) by the State and Territorial Injury Prevention Directors Association has also been recommended for CO poisoning surveillance but has not been used widely.20
Figure 3.
CSTE case definition for acute CO poisoninga
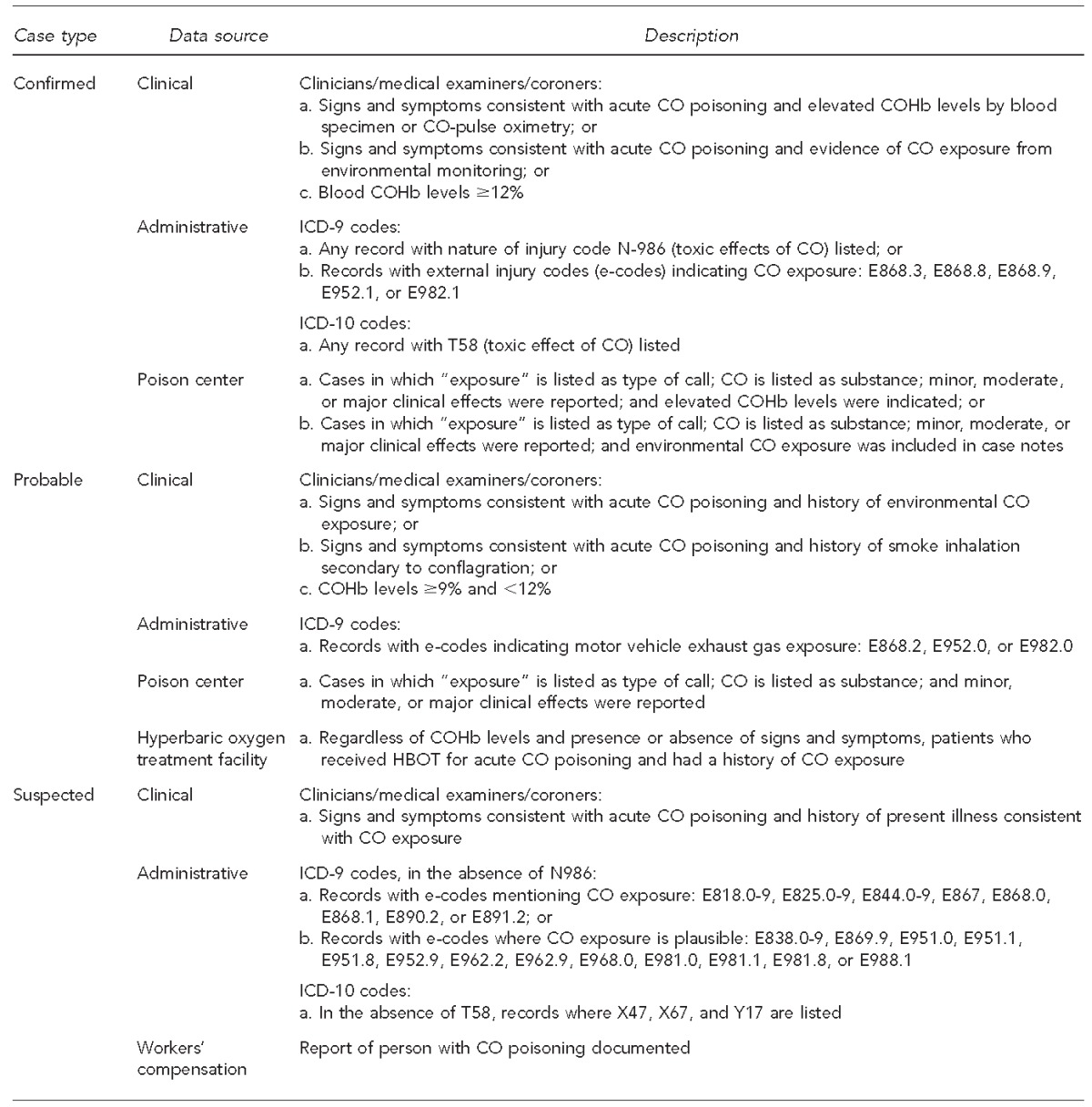
aAdapted from: Council of State and Territorial Epidemiologists. Updates to 1998 case definition for acute carbon monoxide poisoning surveillance [cited 2011 Aug 8]. Available from: URL: http://www.cste.org/PS/2007ps/2007psfinal/EH/07-EH-03.pdf
CSTE = Council of State and Territorial Epidemiologists
CO = carbon monoxide
COHb = carboxyhemoglobin
ICD-9 = International Classification of Diseases, Ninth Revision
ICD-10 = International Classification of Diseases, 10th Revision
Data sources
National Vital Statistics System (NVSS).
The NVSS is the official source of vital statistics (e.g., birth and death) data in the U.S. and was developed through a partnership among CDC's National Center for Health Statistics (NCHS) and vital registration systems in 50 states, two cities (Washington and New York), and five territories (Puerto Rico, the Virgin Islands, Guam, American Samoa, and the Commonwealth of the Northern Mariana Islands).23 The mortality rates for UNFR CO poisoning were calculated from death certificate data obtained from the NVSS using the record axis fields from the multiple cause-of-death files compiled by the NCHS.2,24 Records were searched for all deaths occurring among residents of 50 states and the District of Columbia during 1999–2004 that contained the ICD-10 code T58 (toxic effect of CO) as a contributing cause of death.25
A modified CSTE definition was used to determine UNFR CO poisoning mortality cases.21 A case of unintentional CO-related mortality was defined as one for which both poisoning by accidental exposure to gases or vapors (ICD-10 code X47) and toxic effect of CO (ICD-10 code T58) were listed as causes of death. All records of deaths caused by intentional exposure, exposure of undetermined intent, or fire-related exposure to CO (ICD-10 codes X00–X09, X76, X97, Y26, and Y17) were excluded. Deaths that occurred among foreign residents in the U.S. and deaths among U.S. residents who died abroad were also excluded.
Healthcare Cost and Utilization Project (HCUP).
The HCUP is a nationwide resource for patient-care data developed through federal-state partnerships and sponsored by the Agency for Healthcare Research and Quality (AHRQ). The basis of HCUP data is all-payer discharge information from community hospitals in partner states. Community hospitals are defined as nonfederal, short-term general hospitals, and other specialty hospitals (e.g., obstetrics and gynecology, orthopedic, pediatric, and academic medical centers). Excluded are federal, psychiatric, rehabilitation, long-term, tuberculosis, prison, and institutional hospitals such as college infirmaries.26 Hospitals in participating states send billing information and additional data elements to their respective data organizations, which perform quality checks. State-level data are sent to AHRQ where they undergo further standardization and internal consistency checks before being stored in state-specific databases. Data on hospital stays and ED visits are stored in separate databases.26
The Nationwide Inpatient Sample (NIS) is a stratified probability sample of hospitals drawn from a combined pool of the HCUP state-specific inpatient databases. The NIS approximates a 20% sample of all U.S. hospitals; all discharges from each hospital are included. The 2007 NIS contains data from more than 1,000 hospitals from 40 participating states and eight million unweighted discharge records, or 39 million weighted discharges.27 First made available in 2006, the Nationwide Emergency Department Sample (NEDS) is a stratified probability sample of U.S. EDs approximating a 20% sample of hospital-based EDs. The NEDS uses records from both the HCUP state-specific ED databases—which include ED visits that are “treat-and-release” (i.e., do not result in admission to the hospital in which the ED visit occurred)—and the inpatient databases, which include records for patients initially seen in the ED and then admitted to the same hospital. The 2007 NEDS contains more than 950 EDs from 27 participating states and approximately 26 million unweighted records, or more than 122 million weighted ED visits.28
The HCUP case definition was a modified version of the CSTE case definition that included confirmed, probable, or suspected UNFR CO poisoning cases. ICD-9 codes in the CSTE definition that represented intentional (e.g., E952.0 and E952.1) or fire-related (e.g., E890.2) cases were excluded. In cases where multiple CO poisoning-related ICD-9 codes were listed as diagnosis, the case was counted once to avoid duplicate counts.
HBOT data.
Patients receiving HBOT for CO poisoning have not been characterized extensively. The Undersea and Hyperbaric Medical Society (UHMS) recommends that patients with severe CO poisoning receive HBOT.29,30 In 2007, an estimated 0.3% of patients diagnosed with CO poisoning in EDs and 21.6% of those who were hospitalized received HBOT.3 Severe CO poisoning cases are defined by presenting signs and symptoms (e.g., transient or prolonged unconsciousness, abnormal neurologic signs or cardiovascular findings, or severe acidosis), severity of exposure (patients ≥36 years of age with CO exposure history ≥24 hours including intermittent exposure), or elevated (≥25%) COHb levels.29,31
The CSTE case definition for probable CO poisoning cases was used as the HBOT case definition in conjunction with reports from the facilities to ascertain the cases. UHMS and CDC collaboratively developed an online reporting system for HBOT facilities in the U.S. that treat patients with CO poisoning. Participating UHMS physicians voluntarily respond to a panel of 38 questions on the patient receiving treatment, which includes de-identified information regarding patient demographics, treatment regimens, and circumstances surrounding the poisonings. In 2009, patient-level data were reported by 36 HBOT facilities in 36 states.32 Cases were excluded from analysis if there was any indication of fire-relatedness or intentional exposure in the CO source, hospital service, intent of exposure, or activity fields.
National Poison Data System (NPDS).
The NPDS is a near real-time comprehensive poisoning surveillance system resulting from calls placed to any of the U.S. poison centers regarding poison exposure. This data source is owned and managed by the American Association of Poison Control Centers. CDC's National Center for Environmental Health uses the NPDS to receive, analyze, and display data from poison center calls. Calls to poison centers come from health-care professionals or the general public voluntarily reporting a poison exposure. The information provided by the caller may pertain to themselves and/or others and is used by the poison center to create a record of the call with details such as the date, poison substance, and symptoms. If the report concerns someone receiving treatment at a health-care facility, poison center staff will contact the facility throughout the course of treatment to obtain pertinent clinical information. Details from poison center records are uploaded to the NPDS.
Data were extracted from the NPDS for the years 2000–2009 where CO was identified in the substance data field and the reason for exposure was recorded as “unintentional.” If “fire” or “smoke” were in the substance data field, these exposures were excluded to restrict our analysis to UNFR CO exposures. Data were then stratified according to “management site” (i.e., health-care facility or site of exposure). Rates were calculated using reports of CO exposures to the poison centers and U.S. Census data from 2000–2009.33,34 This case definition is similar to the CSTE case definition, but while the CSTE case definition focuses on poisoning cases that resulted in adverse health effects from CO exposure, CO cases identified via poison center data included cases that identified CO exposure with or without apparent health effects (e.g., symptoms).
American Housing Survey (AHS) and the National Health Interview Survey (NHIS).
The AHS is a representative household survey designed to collect information on the quality of housing in the U.S. It is conducted by the U.S. Census Bureau every other year via telephone interviews or in-person visits of approximately 60,000 housing units.35 The AHS routinely collects data on the presence of a working CO alarm at home.
A representative cross-sectional national health survey conducted by CDC in collaboration with the U.S. Census Bureau, the NHIS also provides information on the presence of a CO alarm at home. On an annual basis, NHIS completes interviews of approximately 35,000 households containing 87,500 people.36 In 2009, NHIS included a supplemental question to the family file about the presence of a CO alarm in the home.37
RESULTS
The most recent estimates obtained from each of the surveillance components (e.g., mortality and ED visits) of the framework are illustrated in the Table. According to the NVSS multiple cause-of-death file, 2,631 UNFR CO deaths occurred in the U.S. during 1999–2004, an average of 439 deaths each year.2 Men and adults aged ≥65 years were more likely to die from CO exposures compared with women and younger individuals, respectively. The annual average age-adjusted death rate in the U.S. was 1.53 deaths per million. Age-adjusted death rates were higher among non-Hispanic black and non-Hispanic white people than other racial/ethnic subgroups; however, the difference between the rates for non-Hispanic black and white people was not statistically significant. The average daily number of CO-related deaths was greatest during the months of January (2.07 deaths per million) and December (1.97 deaths per million) and lowest during the months of July (0.67 deaths per million) and August (0.67 deaths per million) (data not shown).
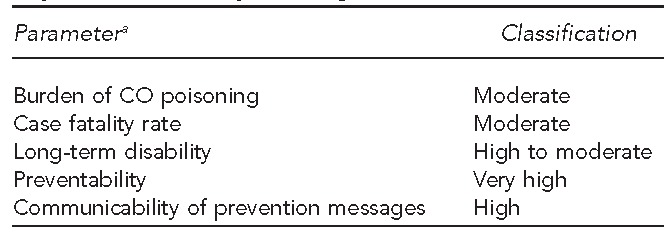
In 2007, there were 22,718 UNFR CO-related hospitalizations nationwide using the CSTE case definition; of these, 2,302 (eight cases per million) were confirmed cases of CO poisoning.3 The rate of hospitalization increased with age among the confirmed cases, and, similar to CO poisoning mortality trends, the highest rates were observed among the elderly (18 cases per million among those ≥65 years of age). Men had higher rates (nine cases per million) of hospitalization resulting from CO exposure than women (seven cases per million) (data not shown). There was a decline in CO-related hospitalizations from 1993 to 2001 (Figure 4). The rate plateaus during 2001–2005, with a slightly upward trend in 2006 and 2007. A total of 232,875 (772 ED visits per million) UNFR CO-related ED visits occurred in 2007, of which 21,304 (71 ED visits per million) were confirmed cases.3 Among these confirmed cases, the highest rates were observed among those 18–44 years of age (87 ED visits per million), followed by those 0–17 years of age (76 ED visits per million). Women frequented EDs at a higher rate than men (75 vs. 67 ED visits per million). The Midwestern and Northeastern regions had higher rates of ED visits and hospitalization (data not shown).
Figure 4.
Trends in hospitalization rates for confirmed cases of unintentional, non-fire-related poisoning: United States, 1993–2007a
aSource: Agency for Healthcare Research and Quality (US). Healthcare Cost and Utilization Project: nationwide inpatient sample, 1993–2007 [cited 2012 Jun 14]. Available from: URL: http://www.hcup-us.ahrq.gov/databases.jsp
In 2009, among the 552 patients reported to receive HBOT for UNFR CO poisoning, most of the patients were non-Hispanic white (57.7%), male (57.1%), and aged 18–44 years (42.7%).32 Consistent with the mortality, hospitalization, and ED data, reported exposures occurred more frequently during the winter (41.9%). Seventy-two percent of patients reported that their exposure location was a residence, and only 9.2% of patients reported the presence of a CO alarm at their exposure location. Sixteen patients (2.9%) reported a prior CO exposure. About half of those treated (55.2%) were discharged after treatment, while 40.8% were hospitalized. Seventy three percent of patients reported being part of an exposure that involved more than one individual (data not shown).
From 2000 to 2009, 68,316 UNFR CO exposures were reported to poison centers. Of these, 30,798 (45.1%) were managed on the site of exposure, and 36,691 (53.7%) were managed at a health-care facility.33 Patients managed on site were predominantly 18–44 years of age (29.8%), female (50.8%), and exposed at a residential setting (80.3%). Similar to the findings from other data sources, CO exposures most frequently occurred between November and February (53.5%) and among people residing in the Midwest (31.2 cases per million) or the Northeast (36.7 cases per million). A greater proportion of CO exposures that were managed on site occurred in the Northeast (35.5%) (data not shown).
In 2007, results from the AHS showed that, nationally, 32.6% of occupied homes reported having a working CO alarm. In 2009, this percentage increased to 36.4%. Data from the AHS also indicated that certain groups reported a lower prevalence of working CO alarms in their housing units. These groups included those living in manufactured housing (22.0%), those of Hispanic ethnicity (24.5%), renters (25.5%), those living below the poverty level (25.8%), and respondents residing in the Southern (23.9%) or Western (22.9%) regions of the U.S. Conversely, several groups, including homeowners (41.5%), those living in housing units constructed within the last four years (38.4%), elderly respondents (35.7%), and those living in the Northeastern (61.0%) or Midwestern (50.0%) regions, reported the presence of a working alarm more frequently.38
In 2009, the NHIS estimated that 40.3% of homes reported the presence of a CO alarm (Table). Further analysis of NHIS data is ongoing.39
DISCUSSION
Public health surveillance is an integral part of prevention that helps assess the public health burden, define public health priorities, evaluate control measures, and guide research efforts. A primary purpose of surveillance is to understand the public health status of a certain health outcome.14 The national UNFR CO poisoning surveillance data identified a substantial number of cases that pose a significant public health burden. Identification and characterization of high-risk groups, exposure site, and regional and seasonal variations provides information on opportunities for effective prevention. This framework attempts to draw together data from multiple sources, otherwise available in sporadic and piecemeal form, for comprehensive understanding of UNFR CO poisoning.
Both nonfatal CO exposures and ED visits were more common among children (<18 years of age) and females, while hospitalization and fatality rates were higher among males and older adults (≥65 years of age). These population subgroups (male, older adults) have consistently been found to be at higher risk for more severe CO poisoning.2,3 As with mortality risk, the higher hospitalization rate among men has been assumedly a result of engaging in high-risk behaviors, such as using fuel-burning tools or -appliances. Also, severe CO exposures among the older adult population could be due to the misidentification of nonspecific CO-related symptoms, such as fatigue or flu-like illnesses.2,40 Biologically, children are more susceptible to CO poisoning because they have higher basal metabolic rates and tissue oxygen demands.41 Women, similar to children, manifest symptoms at lower levels of CO exposure because they have a lower red blood cell count.40,42 These factors might lead to earlier exposure recognition and, therefore, a lower exposure and shorter recovery time.40 Identifying these high-risk subgroups is important because they can help target public health prevention efforts.
Both fatal and nonfatal UNFR CO poisonings follow a seasonal pattern, with more cases occurring during the winter months. These trends are presumably due to the increased use of home heating systems, use of alternative heat sources, improper use of portable generators during power outages caused by winter storms, indoor use of charcoal grills, warming up motor vehicles in an enclosed space (e.g., an attached garage), or exposure to automobile exhaust by motorists stranded in snow or blizzards.1,2 The increased rate observed during winter months is believed to lead to an overall variation in geographic distribution of CO poisonings as a result of differences in length and intensity of winter seasons in different regions. States and regions that experience long and hard winter seasons disproportionately bear the burden of CO poisoning cases. During 1999–2004, the highest rate for CO poisoning fatalities occurred in the states of Alaska, Montana, Wyoming, Nebraska, and North Dakota.2 In 2007, the Northeast and Midwest regions of the United States had the highest rates of ED visits and hospitalizations for confirmed cases of CO poisoning.3 Similar geographic distributions (60% of cases were from the Northeast or Midwestern regions) were observed in the 2000–2009 poison center data.33 Public health prevention efforts can benefit from focused education and awareness campaigns before and during the occurrence of natural disasters.
Measurement of hazard, exposure, and health outcomes; ongoing systematic data collection; and timely and representative estimates for planning, implementation, and evaluation purposes are three major functions of an environmental health surveillance system.17 However, as is often the case with environmental public health surveillance,17 the CO poisoning surveillance framework includes data from multiple secondary sources. Although use of secondary data sources for surveillance might be less expensive and require fewer resources than establishing a large-scale active surveillance system, it has some limitations that might restrict the usability of the data. Because some of these limitations and restrictions are component- or data source-specific, they have been discussed in detail elsewhere.1–3,31,32 As a whole, timely annual surveillance data are important in resource allocation and program planning.17 Acquisition of secondary data can be time consuming and resource intensive, and surveillance systems relying on secondary data sources are restricted by the timing of data release by the specific data authority, resource availability, and methodological implications (e.g., five years of NVSS data are usually compiled together for statistically valid estimates of CO-related mortality).
Restrictions on the release of certain variables also limit subgroup analysis and identification of high-risk populations. For example, while the mortality data indicate that some racial disparity among CO poisoning cases exists, with non-Hispanic black people having higher rates of mortality, this finding cannot be assessed or replicated with ED visit or hospitalization data, owing to lack of individual-level data on race/ethnicity for these health outcomes. It is important to characterize risk among population subgroups to better understand the health behavior, attitude, and knowledge, and to develop more effective targeted prevention.
Limitations of and reliance on secondary data sources emphasize the need for a continued effort to expand and enhance current surveillance capacity and improve our understanding of CO poisoning. A complete cost analysis of establishing additional surveillance for CO poisoning has not been conducted. Such an analysis might justify allocation of appropriate resources, as there is some indication that the benefits might outweigh the cost.3 The direct hospitalization cost for cases of CO poisonings was more than $26 million in 2007.3 Efforts to include or increase CO-related questions in national surveys such as the AHS, the NHIS, or the Behavioral Risk Factor Surveillance System are ongoing. However, financial and other resource constraints are a major obstacle in developing a more complete and comprehensive national CO poisoning surveillance framework. Also, CDC has recently undertaken a project to monitor the number of states with regulations that mandate having a CO alarm in residential settings. CDC's primary recommendation to prevent CO poisoning is to have a working CO alarm at home. Understanding the regulatory and enforcement issues regarding CO alarm installation has important public health implications because almost 70% of UNFR CO poisonings occur at home.
According to the National Fire Protection Association, fire departments responded to an estimated 61,100 CO exposure incidents in 2005 that were not related to a fire or were due to false activation of a CO alarm.43 Because a single CO exposure event can affect multiple individuals, the current morbidity and mortality estimates suggest that a large number of CO poisoning cases might not have been captured through the current surveillance mechanisms. Due to the overlapping nature and limitations of the data sources, it is difficult to depict a complete picture of the burden of CO poisoning. Some cases could have been counted more than once under this surveillance framework. For example, it is unclear what proportion of CO exposure cases end up in the ED or hospitalized from the ED nationwide. Also, different case definitions used for surveillance of CO exposure and poisoning might have resulted in misclassification of cases. It has been suggested that the CSTE case definition might lack specificity and include cases that are not directly attributable to CO poisoning. For example, only 10% of the hospitalization cases identified using the CSTE definition were confirmed cases of CO poisoning.3,40 It is important that validated and standardized case definitions are used for accuracy and comparison purposes. Additionally, differences in timing of data releases from each source make it difficult to compare trends or evaluate prevention efforts.
Evaluation of surveillance systems is an integral part of surveillance efforts for valid and reliable estimates. CDC has provided recommendations and guidelines to evaluate surveillance systems.44 None of the secondary data sources in this framework have undergone a systematic evaluation. Evaluation of surveillance systems will lead to better understanding and interpretation of data and provide guidelines for expansion and modification of the framework. It is important that efforts are undertaken to continuously evaluate the effectiveness of these data sources for CO poisoning surveillance. However, development of a framework from secondary data sources encourages resource conservation and partnership among key stakeholders.17
There is a dearth of literature on the development of surveillance systems and the challenges surrounding them. This is the first article to describe CO poisoning surveillance framework at the national level. Most of these data sources are also available at state or local levels, and local health authorities could use a similar systematic approach in developing a local-level framework. Monitoring and surveillance of CO poisoning cases at the state level is a public health priority, and the Healthy People 2020 objective EH-22.7 is to have a CO poisoning surveillance system in all 50 states.15 The framework described has already been successfully adopted at the local level for disaster-related CO poisoning surveillance.22 Disaster-related CO poisoning is a common phenomenon and usually results from high-risk health behaviors (e.g., improper placement of generators or indoor use of charcoal grills) during widespread power outages caused by natural disasters.45
CONCLUSIONS
The prevention of CO poisoning depends on source reduction or avoidance and early detection. Public health interventions aimed at modification of health behaviors, such as maintenance of heating and cooking appliances, installation of battery-powered or battery backup CO alarms at home, and proper use of portable sources of CO poisoning (e.g., gasoline-powered generators and charcoal grills), might prevent a large number of CO poisoning cases. Nationwide, it is estimated that only 40% of households have a CO alarm. There is a definite need and opportunity for public education and awareness for the prevention of CO poisoning cases. The current national CO poisoning surveillance framework includes data from a broad spectrum of sources for surveillance on the key areas of the “health behavior-exposure-health outcome” continuum, from which the national burden of CO poisoning could be successfully estimated. It also identified population subgroups that could be at higher risk of CO-related mortality and morbidity and provided valuable information to guide prevention efforts. This framework will continue to be modified and expanded to include new data sources and increase stakeholder involvement for better surveillance both at the national and local levels.
Table.
Estimates from national unintentional, non-fire-related CO poisoning surveillance in the United States
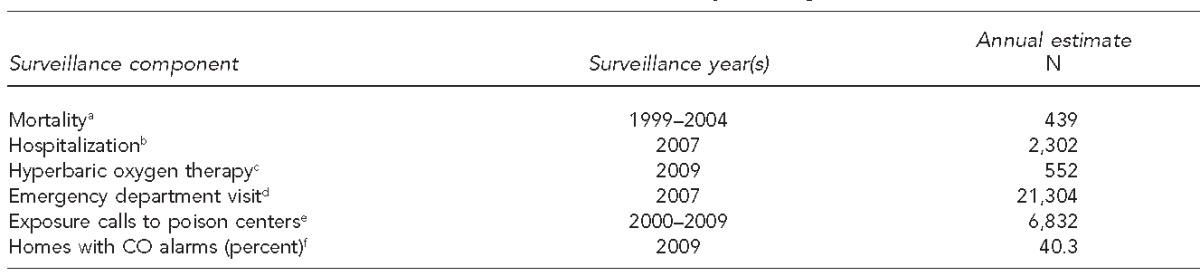
aSource: National Vital Statistics System
bSource: Healthcare Cost and Utilization Project Nationwide Inpatient Sample
cSource: Hyperbaric oxygen treatment facility data
dSource: Healthcare Cost and Utilization Project Nationwide Emergency Department Sample
eSource: National Poison Data System
fSource: National Health Interview Survey 2009
CO = carbon monoxide
Acknowledgments
The authors thank Anne Elixhauser, PhD, Senior Research Scientist, Agency for Healthcare Research and Quality; Neil B. Hampson, MD, Undersea and Hyperbaric Medical Society; and Arthur Chung, MD, Centers for Disease Control and Prevention (CDC), National Center for Environmental Health, Health Studies Branch. This work was exempt from Institutional Review Board approval.
Footnotes
The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of CDC.
REFERENCES
- 1.Nonfatal, unintentional, non-fire-related carbon monoxide exposures—United States, 2004-2006. MMWR Morb Mortal Wkly Rep. 2008;57(33):896–9. [PubMed] [Google Scholar]
- 2.Carbon monoxide-related deaths—United States, 1999-2004. MMWR Morb Mortal Wkly Rep. 2007;56(50):1309–12. [PubMed] [Google Scholar]
- 3.Iqbal S, Law HZ, Clower JH, Yip FY, Elixhauser A. Hospital burden of unintentional carbon monoxide poisoning in the United States, 2007. Am J Emerg Med. 2012;30:657–64. doi: 10.1016/j.ajem.2011.03.003. [DOI] [PubMed] [Google Scholar]
- 4.Environmental Protection Agency (US) Indoor air quality. Carbon monoxide (CO) [cited 2011 Aug 11]. Available from: URL: http://www.epa.gov/iaq/co.html.
- 5.National Workgroup on Carbon Monoxide Surveillance. Carbon monoxide: a model environmental public health indicator. 2006. Apr, [cited 2008 Sep 17]. Available from: URL: http://www.myfloridaeh.com/programs/Environmental_Public_Health_-Tracking/PDFs/CO_A_Model_Public_Health_Indicator.pdf.
- 6.Raub JA, Mathieu-Nolf M, Hampson NB, Thom SR. Carbon monoxide poisoning—a public health perspective. Toxicology. 2000;145:1–14. doi: 10.1016/s0300-483x(99)00217-6. [DOI] [PubMed] [Google Scholar]
- 7.Myers RA, DeFazio A, Kelly MP. Chronic carbon monoxide exposure: a clinical syndrome detected by neuropsychological tests. J Clin Psychol. 1998;54:555–67. doi: 10.1002/(sici)1097-4679(199808)54:5<555::aid-jclp1>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- 8.Hopkins RO, Weaver LK, Kesner RP. Long-term memory impairments and hippocampal magnetic resonance imaging in carbon monoxide-poisoned subjects. Undersea Hyperb Med. 1993;20:15. [Google Scholar]
- 9.Hopkins RO, Woon FL. Neuroimaging, cognitive, and neurobehavioral outcomes following carbon monoxide poisoning. Behav Cogn Neurosci Rev. 2006;5:141–55. doi: 10.1177/1534582306289730. [DOI] [PubMed] [Google Scholar]
- 10.Gale SD, Hopkins RO. Effects of hypoxia on the brain: neuroimaging and neuropsychological findings following carbon monoxide poisoning and obstructive sleep apnea. J Int Neuropsychol Soc. 2004;10:60–71. doi: 10.1017/S1355617704101082. [DOI] [PubMed] [Google Scholar]
- 11.Unintentional, non-fire-related carbon monoxide exposures—United States, 2001-2003. MMWR Morb Mortal Wkly Rep. 2005;54(2):36–9. [PubMed] [Google Scholar]
- 12.Wright J. Chronic and occult carbon monoxide poisoning: we don't know what we're missing. Emerg Med J. 2002;19:386–90. doi: 10.1136/emj.19.5.386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Use of carbon monoxide alarms to prevent poisonings during a power outage—North Carolina December 2002. MMWR Morb Mortal Wkly Rep. 2004;53(9):189–92. [PubMed] [Google Scholar]
- 14.Lee LM, Teutsch SM, Thacker SB, St. Louis ME. 3rd ed. New York: Oxford University Press, Inc.; 2010. Principles and practice of public health surveillance. [Google Scholar]
- 15.Department of Health and Human Services (US) Healthy People 2020. [cited 2011 Aug 10];Topics and objectives. Available from: URL: http://www.healthypeople.gov/2020/topicsobjectives2020/default.aspx. [Google Scholar]
- 16.Graber JM, Macdonald SC, Kass DE, Smith AE, Anderson HA. Carbon monoxide: the case for environmental public health surveillance. Public Health Rep. 2007;122:138–44. doi: 10.1177/003335490712200202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Thacker SB, Stroup DF, Parrish RG, Anderson HA. Surveillance in environmental public health: issues, systems, and sources. Am J Public Health. 1996;86:633–8. doi: 10.2105/ajph.86.5.633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Goldman LR, Gomez M, Greenfield S, Hall L, Hulka BS, Kaye WE, et al. Use of exposure databases for status and trends analysis. Arch Environ Health. 1992;47:430–8. doi: 10.1080/00039896.1992.9938384. [DOI] [PubMed] [Google Scholar]
- 19.Holzner CL, Hirsh RB, Perper JB. Managing workplace exposure information. Am Ind Hyg Assoc J. 1993;54:15–21. doi: 10.1080/15298669391354252. [DOI] [PubMed] [Google Scholar]
- 20.Hampson NB. Emergency department visits for carbon monoxide poisoning in the Pacific Northwest. J Emerg Med. 1998;16:695–8. doi: 10.1016/s0736-4679(98)00080-8. [DOI] [PubMed] [Google Scholar]
- 21.Council of State and Territorial Epidemiologists. Updates to 1998 case definition for acute carbon monoxide poisoning surveillance. [cited 2011 Aug 8]. Available from: URL: http://www.cste.org/PS/2007ps/2007psfinal/EH/07-EH-03.pdf.
- 22.Lutterloh EC, Iqbal S, Clower JH, Spiller HA, Riggs MA, Sugg TJ, et al. Carbon monoxide poisoning after an ice storm in Kentucky, 2009. Public Health Rep. 2011;126(Suppl 1):108–15. doi: 10.1177/00333549111260S114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Centers for Disease Control and Prevention (US), National Center for Health Statistics. About the National Vital Statistics System. [cited 2011 Aug 10]. Available from: URL: http://www.cdc.gov/nchs/nvss/about_nvss.htm.
- 24.Centers for Disease Control and Prevention (US), National Center for Health Statistics. Vital statistics data available online. Mortality multiple cause files. [cited 2011 Aug 10]. Available from: URL: http://www.cdc.gov/nchs/data_access/Vitalstatsonline.htm.
- 25.World Health Organization. International statistical classification of diseases and related health problems, 10th revision. Geneva: WHO; 1992. [Google Scholar]
- 26.Agency for Healthcare Research and Quality (US) Healthcare Cost and Utilization Project (HCUP) [cited 2011 Aug 10]. Available from: URL: http://www.ahrq.gov/data/hcup/#hcup. [PubMed]
- 27.Agency for Healthcare Research and Quality (US) Introduction to the HCUP Nationwide Inpatient Sample (NIS) 2007. [cited 2011 Aug 10]. Available from: URL: http://hcup-us.ahrq.gov/db/nation/nis/NIS_Introduction_2007.jsp.
- 28.Agency for Healthcare Research and Quality (US) Introduction to the HCUP Nationwide Emergency Department Sample (NEDS) 2007. [cited 2011 Aug 10]. Available from: URL: http://www.hcup-us.ahrq.gov/db/nation/neds/NEDS_2007_Introduction_v5.pdf.
- 29.Weaver LK. Clinical practice. Carbon monoxide poisoning. N Engl J Med. 2009;360:1217–25. doi: 10.1056/NEJMcp0808891. [DOI] [PubMed] [Google Scholar]
- 30.Weaver LK, Hopkins RO, Chan KJ, Churchill S, Elliott CG, Clemmer TP, et al. Hyperbaric oxygen for acute carbon monoxide poisoning. N Engl J Med. 2002;347:1057–67. doi: 10.1056/NEJMoa013121. [DOI] [PubMed] [Google Scholar]
- 31.Gesell LB, editor. 12th ed. Durham (NC): Undersea and Hyperbaric Medical Society; 2008. The Hyperbaric Oxygen Therapy Committee report: indications and results. [Google Scholar]
- 32.Clower JH, Hampson NB, Iqbal S, Yip FY. Recipients of hyperbaric oxygen treatment for carbon monoxide poisoning and exposure circumstances. Am J Emerg Med. 2011. Aug 18, [epub ahead of print]. [DOI] [PubMed]
- 33.Carbon monoxide exposures—United States, 2000-2009. MMWR Morb Mortal Wkly Rep. 2011;60(30):1014–7. [PubMed] [Google Scholar]
- 34.Census Bureau (US) Annual estimates of the resident population by sex and five-year age groups for the United States: April 1, 2000, to July 1, 2009. Washington: Census Bureau, Population Division; 2010. [cited 2011 Jul 29]. Also available from: URL: http://www.census.gov/popest/data/national/asrh/2009/index.html. [Google Scholar]
- 35.Census Bureau (US). American Housing Survey (AHS) Methodology. [cited 2011 Jul 14]. Available from: URL: http://www.census.gov/housing/ahs/methodology.
- 36.Centers for Disease Control and Prevention (US), National Center for Health Statistics. About the National Health Interview Survey. [cited 2011 Jul 10]. Available from: URL: http://www.cdc.gov/nchs/nhis/about_nhis.htm.
- 37.Centers for Disease Control and Prevention (US), National Center for Health Statistics. 2009 National Health Interview Survey (NHIS) public use data release. [cited 2011 Aug 10]. Available from: URL: ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_-Documentation/NHIS/2009/readme.pdf.
- 38.Census Bureau (US) American Housing Survey national tables: 2009 using Census 2000-based weighting. [cited 2011 Jul 20]. Available from: URL: http://www.census.gov/housing/ahs/data/ahs2009.html.
- 39.Census Bureau (US) American Housing Survey national tables: 2007 using Census 2000-based weighting. [cited 2011 Jul 20]. Available from: URL: http://www.census.gov/housing/ahs/data/ahs2007.html.
- 40.Iqbal S, Clower JH, Boehmer TK, Yip FY, Garbe P. Carbon monoxide-related hospitalizations in the U.S.: evaluation of a web-based query system for public health surveillance. Public Health Rep. 2010;125:423–32. doi: 10.1177/003335491012500311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Liebelt EL. Hyperbaric oxygen therapy in childhood carbon monoxide poisoning. Curr Opin Pediatr. 1999;11:259–64. doi: 10.1097/00008480-199906000-00017. [DOI] [PubMed] [Google Scholar]
- 42.WebMD. First aid and emergencies. Carbon monoxide poisoning treatment. [cited 2011 Jul 20]. Available from: URL: http://firstaid.webmd.com/carbon-monoxide-co.
- 43.Flynn JD. National Fire Protection Association, Fire Analysis and Research Division. Non-fire carbon monoxide incidents reported in 2005. 2007. Jun, [cited 2011 Jul 13]. revised April 2008. Available from: URL: http://www.nfpa.org/assets/files//PDF/OS.CarbonMonoxide.pdf.
- 44.German RR, Lee LM, Horan JM, Milstein RL, Pertowski CA, Waller MN Guidelines Working Group. Updated guidelines for evaluating public health surveillance systems: recommendations from the Guidelines Working Group. MMWR Recomm Rep. 2001;50(RR-13):1–35. [PubMed] [Google Scholar]
- 45.Iqbal S, Clower JH, Hernandez SA, Damon SA, Yip FY. A review of disaster-related carbon monoxide poisoning: surveillance, epidemiology, and opportunities for prevention. Am J Public Health. 2012 doi: 10.2105/AJPH.2012.300674. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]