SYNOPSIS
Objective
We examined disparities in periodontal disease in U.S. adults according to age, sex, race/ethnicity, country of birth, education, income, and poverty-income ratio within and between the third National Health and Nutrition Examination Survey (NHANES III, 1988–1994) and NHANES 1999–2004.
Methods
We assessed disparities and changes therein using prevalence differences and ratios, as well as the Symmetrized Theil Index (STI). While these measures document disparities between pairs of population subgroups, and changes in relative disparities between surveys, the STI is a summary measure of health disparities that also tracks between-group disparities relative to the total population.
Results
Prevalence differences and ratios for the prevalence of periodontitis, the mean pocket depth (PD), and the mean clinical attachment loss (CAL) suggest that periodontal disease significantly decreased between NHANES III and NHANES 1999–2004 (p<0.01). However, the STI for the prevalence of periodontitis suggests that disparities significantly increased within categories of race/ethnicity, country of birth, and education in NHANES 1999–2004 compared with NHANES III. These findings were corroborated for mean PD and mean CAL (p<0.001): the overall STI significantly increased for mean PD from 4.53% in NHANES III to 11.02% in NHANES 1999–2004 and for mean CAL for teeth with CAL >0 from 31.73% in NHANES III to 43.36% in NHANES 1999–2004.
Conclusions
Our findings suggest that inequalities in periodontal disease significantly decreased between NHANES III and NHANES 1999–2004 in the total population and across selected characteristics of the population. However, these inequalities increased within groups of the population in NHANES 1999–2004 compared with NHANES III. These findings call attention to the absolute and relative differences not only between population groups across surveys, but also within population groups within and between surveys.
Disparities in the prevalence of periodontitis in the United States are pervasive.–19 These disparities have been documented according to age, sex, race/ethnicity, country of birth, education, and income, as well as over time.3,5,15–17,19–25 For example, a higher prevalence of periodontal disease is found in older adults, men, African Americans, those with fewer years of education, and those with lower incomes.15,16,19,24,25 In fact, the Surgeon General's 2000 report on oral health, Oral Health in America,24 not only underscored the importance of oral health, but also called attention to disparities in the oral health status of the American population. Such health disparities have provided the impetus for an extensive body of research to focus on measurement issues across groups of the population as well as over time.26–35
While traditional measures such as prevalence differences and ratios are useful, other methods to measure health disparities provide additional insight into these disparities. For instance, the prevalence differences and ratios improve our understanding of health inequalities between the overall (or a reference) population and categories of selected characteristics of the population at one point in time and/or over time. However, these measures tell us little or nothing regarding how these inequalities are affected by the distribution of disease in the population and/or the size of the population groups. Summary measures of health disparities such the Theil Index (TI) and Mean Log Deviation (MLD)36 help account for these issues, though the TI and MLD require a value judgment as to whether pairwise disparities—for example, between each population subgroup and the “best-off” group—should be weighted by the groups' shares of the adverse health outcome under investigation (TI) or by the groups' population shares (MLD).37 To integrate these two summary measures into a single index, a recent study has proposed the Symmetrized Theil Index (STI), representing the average of TI and MLD.38 Unlike the TI and MLD, the STI is symmetric and avoids the aforementioned value judgment from which the TI and MLD suffer, while accounting for both groups' share of the disease and their population size.39
Because the third National Health and Nutrition Examination Survey (NHANES III, 1988–1994) and NHANES 1999–2004 used the same periodontal examination protocol, the availability of these data affords the opportunity to compare the prevalence of periodontitis between NHANES III and NHANES 1999–2004. Thus, we examined disparities in periodontal disease in U.S. adults according to age, sex, race/ethnicity, country of birth, education, income, and poverty-income ratio (PIR) within and between surveys using prevalence differences and ratios, as well as the STI. Specifically, the disparities in the prevalence of periodontitis, the mean pocket depth (PD), and mean clinical attachment loss (CAL) were examined and discussed in the context of these measures.
METHODS
Data for this analysis came from public-use data files from the NHANES III (Adult and Examination files) and the NHANES 1999–2004 (Demographic, Questionnaire, and Examination files). NHANES III, conducted from 1988 to 1994, represents the seventh in a series of national examination studies in the U.S. NHANES 1999–2004 represents the ongoing collection of the NHANES from March 1999 to December 2004. Both surveys assessed the health status of a nationally representative sample of the civilian noninstitutionalized U.S. population, selected through a stratified multistage probability sampling design. Full descriptions of the sample design and methodology for NHANES III40,41 and NHANES 1999–200442 have been reported elsewhere.
NHANES III yielded 18,825 records for adults aged 20 years and older, of whom 11,917 had a complete periodontal examination. NHANES 1999–2004 yielded 15,332 records for adults aged 20 years and older, of whom 10,044 had a complete periodontal examination. However, 118 records did not have information on PD and/or CAL, yielding an analytical sample of 9,926.
Dentists trained according to the NHANES examination protocol conducted the periodontal examinations.43–45 Briefly, the periodontal examination is conducted in two sites, midbuccal and mesiobuccal for each tooth, in two randomly chosen quadrants, one maxillary and one mandibular, on the assumption that conditions in these two quadrants would represent the mouth. Third molars are excluded because of their frequent extraction in young adulthood, so a maximum of 14 teeth and 28 sites per individual are examined. Previous studies used several combinations of CAL and PD to establish periodontitis case definitions.18,19,46,47 Consistent with a previous study examining trends in oral health in the U.S.,25 we defined periodontitis as having at least one site with PD ≥4 millimeters (mm) and at least one site with CAL ≥3 mm. However, these conditions did not have to be present in the same tooth. In addition, we examined PD and CAL as continuous variables to ascertain inequalities in the severity of periodontal disease in U.S. adults.
We selected age, sex, race/ethnicity, country of birth, education, income, and PIR as characteristics for analysis because, in the U.S., oral health disparities have already been documented for these characteristics over time.3,5,15–17,20–25 In NHANES III, race/ethnicity was self-reported by the survey participants and recoded as non-Hispanic white, non-Hispanic black or African American, Mexican American, and other. In NHANES 1999–2004, the “other” category included multiracial and an additional category of “other Hispanic.” (Hereafter, non-Hispanic black and non-Hispanic white are referred to as black and white, respectively.) For our analysis, we recoded country of birth as U.S.-born (born in the 50 U.S. states or Washington, D.C.) and foreign-born (born in Mexico or elsewhere).
In NHANES III, education was collected as a numerical variable (number of years of education) from zero to 17 years. We categorized education as follows: <12 years, 12 years, and >12 years. In NHANES 1999–2004, this variable was recoded with the same categories as the ones created for NHANES III. In NHANES III, the total 12-month family income was recorded using increments of $1,000 until the last category of ≥$50,000. In NHANES 1999–2004, this variable was recorded using increments of $5,000 until the last category of ≥$75,000. In our analysis, we adjusted income for inflation using the Consumer Price Index48 and then categorized it as low, medium, or high. While not exact, this procedure provided us with a comparison between the categories <$14,999, $15,000–$24,999, and ≥$25,000 (respectively) in NHANES III and the categories <$19,999, $20,000–$44,999, and ≥$45,000 (respectively) in NHANES 1999–2004.
In addition to income, we also examined the PIR, which was calculated as a continuous variable in both surveys using eligibility in the U.S. Department of Agriculture food assistance program (i.e., Special Supplemental Nutrition Program for Women, Infants and Children [WIC]; Food Stamp Program; and school lunch and breakfast programs).49,50 For our analysis, we recoded PIR as follows: 0.000–1.850 (low), 1.851–3.500 (medium), and ≥3.501 (high). Survey respondents without information on education, income, or PIR were included in the analysis as a separate category. Finally, although these variables were coded as ordinal, they were treated as nominal in our analyses.
Statistical analysis
For each survey (NHANES III and NHANES 1999–2004), prevalence of periodontitis, mean PD and CAL, and group-specific as well as between-group STI values and their standard errors for selected sociodemographic characteristics are presented for U.S. adults. Disparities in periodontitis were assessed using prevalence differences and ratios within and between surveys for each characteristic's categories using t-tests as well as Pearson's and Cochran-Mantel-Haenszel Chi-square statistics. In addition, we assessed statistical differences for between-group STI (STIB) values, as well as differences over time, using simple t-tests, with a Bonferroni adjustment for multiple comparisons when necessary. For dichotomous data, such as prevalence of periodontal disease, STIB behaves in a similar way to the Pearson's Chi-square statistic (χ2) for testing the independence of an individual's disease status and that individual's characteristic or group. For continuous data, such as severity of periodontal disease (i.e., mean PD and mean CAL), STIB can be interpreted in a manner akin to the between-group sum-of-squares (SSB) in an analysis-of-variance decomposition, which examines the difference of each group from the population mean. Yet, STIB is more sensitive than either χ2 or SSB in detecting disparities relative to the population prevalence or mean.38
We used SAS® version 9.2 for data management procedures.51 The statistical analyses were conducted in R,52 using the “survey” package,53,54 and in SUDAAN.55 Both statistical software programs take into account the complex sampling design. R code for computing the STI, their group-specific and between-group components in grouped data, and their design-based standard errors can be accessed at http://stat.hunter.cuny.edu/talih. This code can be used in R or in SAS through the SAS/IML® Studio 3.2.51
RESULTS
The overall prevalence of periodontal disease significantly decreased by 7.1% (or an actual percentage decrease of 44.0%) between NHANES III (16.1%) and NHANES 1999–2004 (9.0%; p<0.01; Table 1). Moreover, while the prevalence of periodontal disease decreased across all covariates between surveys, periodontal disease remained most common within survey among those aged 35 years and older, men, black people, Mexican American people, those with <12 years of education, those with low incomes, and those with a PIR <1.85 (p<0.01 for all Chi-square tests of independence).
Table 1.
Prevalence of periodontal disease,a prevalence difference, and prevalence ratio estimates for selected sociodemographic characteristics in U.S. adults 20 years of age and older within and between surveys: NHANES III (1988–1994) and NHANES 1999–2004
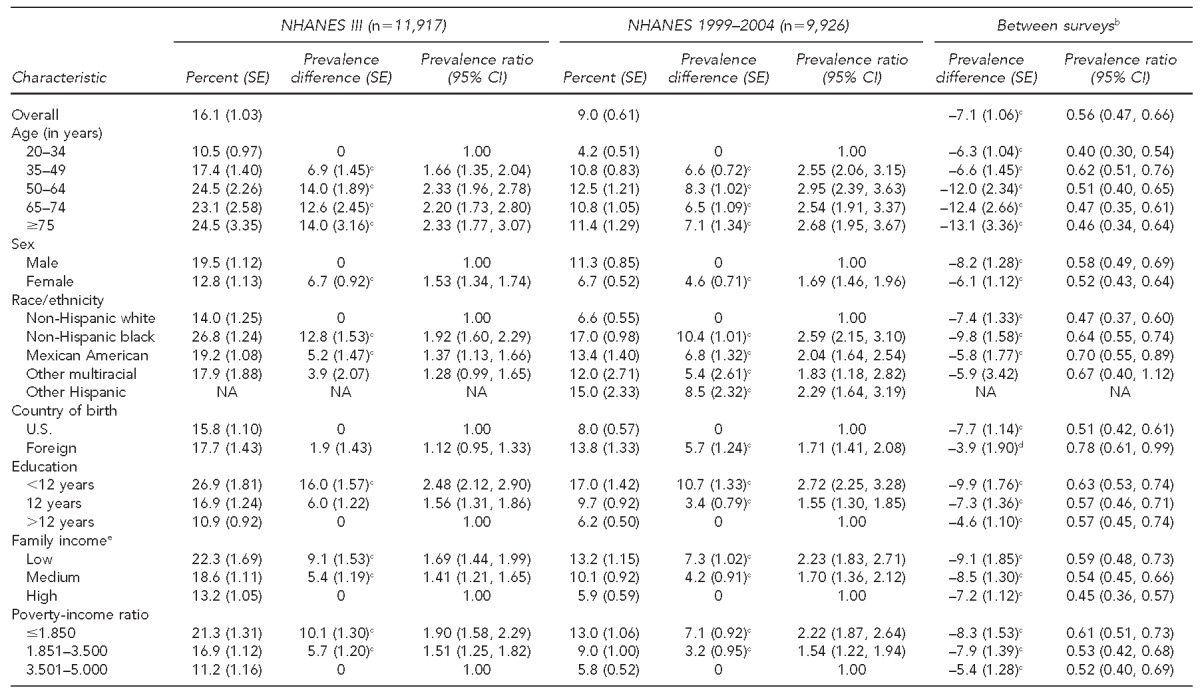
aPrevalence (SEs) of periodontal disease (defined as at least one site with pocket depth ≥4 millimeters [mm] and at least one site with clinical attachment loss ≥3 mm) for adults 20 years of age and older. All p-values for Chi-square tests within and between surveys were <0.01 except for nativity status in NHANES III.
bPrevalence difference and ratio compare NHANES 1999–2004 with NHANES III (1988–1994).
cp<0.01 for t-test assessing the difference between the prevalence of each level of the characteristic and the level assigned as the reference
dp<0.05 for t-test assessing the difference between the prevalence of each level of the characteristic and the level assigned as the reference
eLow, medium, and high categories for income were <$14,999, $15,000–$24,999, and ≥$25,000 in NHANES III and <$19,999, $20,000–$44,999, and ≥$45,000 in NHANES 1999–2004, respectively.
NHANES = National Health and Nutrition Examination Survey
SE = standard error
CI = confidence interval
NA = not applicable
Similarly, the overall mean PD significantly decreased by 0.43 mm between NHANES III (1.45 mm) and NHANES 1999–2004 (1.02 mm; p<0.01 for t-test; Table 2). A decrease in the mean PD between surveys was observed across age, sex, race/ethnicity, country of birth, education, income, and PIR characteristics (p<0.01 for all t-tests). Within survey, the mean PD remained higher among men, racial/ethnic groups other than white, foreign-born individuals, those with <12 years of education, those with low incomes, and those with a PIR <1.85 (p<0.05 for all t-tests). In NHANES 1999–2004, those older than 35 years of age suffered from a higher mean PD than those 20–34 years of age. Finally, the mean CAL significantly decreased by 0.20 mm between NHANES III (0.98 mm) and NHANES 1999–2004 (0.79 mm; p<0.01 for t-test; Table 3). A decrease in mean CAL was observed consistently across all covariates (p<0.05 for all t-tests). In general, the mean CAL remained higher among adults aged 35 years and older, men, black people, other multiracial people, foreign-born individuals, those with at least 12 years of education, those with low incomes, and those with a PIR <1.85 (all p-values <0.01).
Table 2.
Mean pocket depth, mean difference, and mean ratioa estimates for selected sociodemographic characteristics in U.S. adults 20 years of age and older: NHANES III (1988–1994) and NHANES 1999–2004
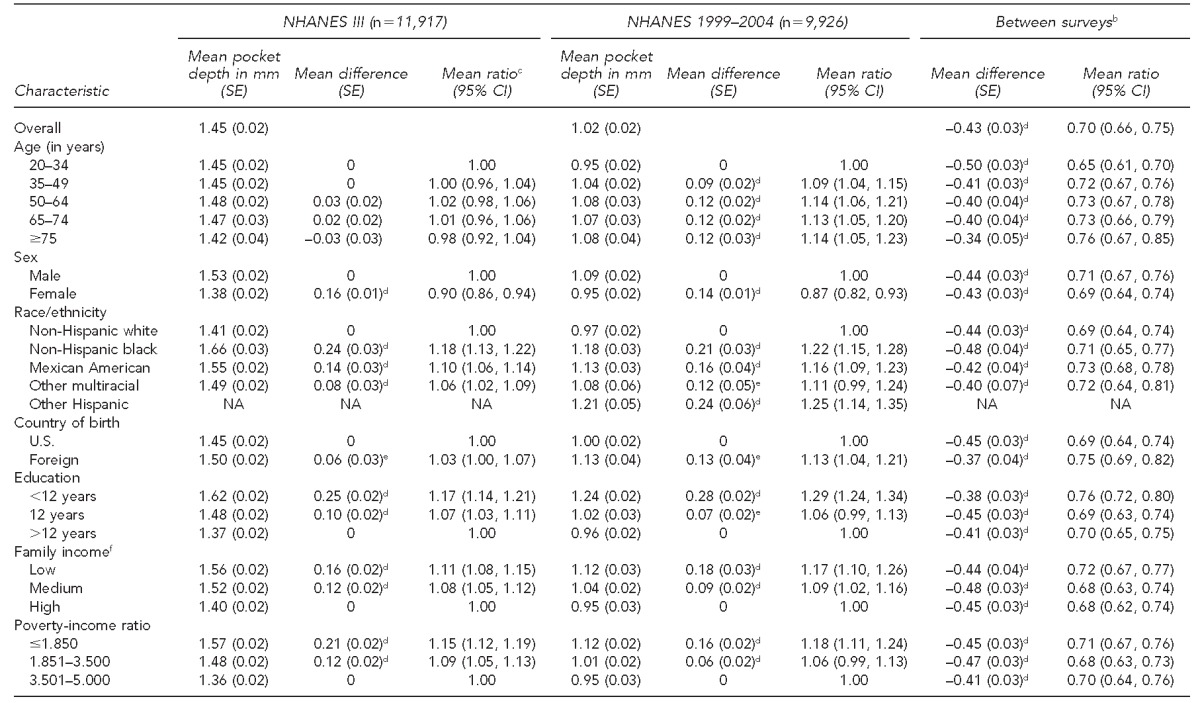
aMeans (SEs) for pocket depth for adults 20 years of age and older
bMean difference and ratio compare NHANES 1999–2004 with NHANES III (1988–1994).
cSEs for ratios calculated using the delta method from estimates obtained from SUDAAN
dp<0.01 for t-test assessing the difference between the prevalence of each level of the characteristic and the level assigned as the reference
ep<0.05 for t-test assessing the difference between the prevalence of each level of the characteristic and the level assigned as the reference
fLow, medium, and high categories for income were <$14,999, $15,000–$24,999, and ≥$25,000 in NHANES III and <$19,999, $20,000–$44,999, and ≥$45,000 in NHANES 1999–2004, respectively.
NHANES = National Health and Nutrition Examination Survey
mm = millimeters
SE = standard error
CI = confidence interval
NA = not applicable
Table 3.
Mean clinical attachment loss, mean difference, and mean ratioa estimates for selected sociodemographic characteristics in U.S. adults 20 years of age and older: NHANES III (1988–1994) and NHANES 1999–2004
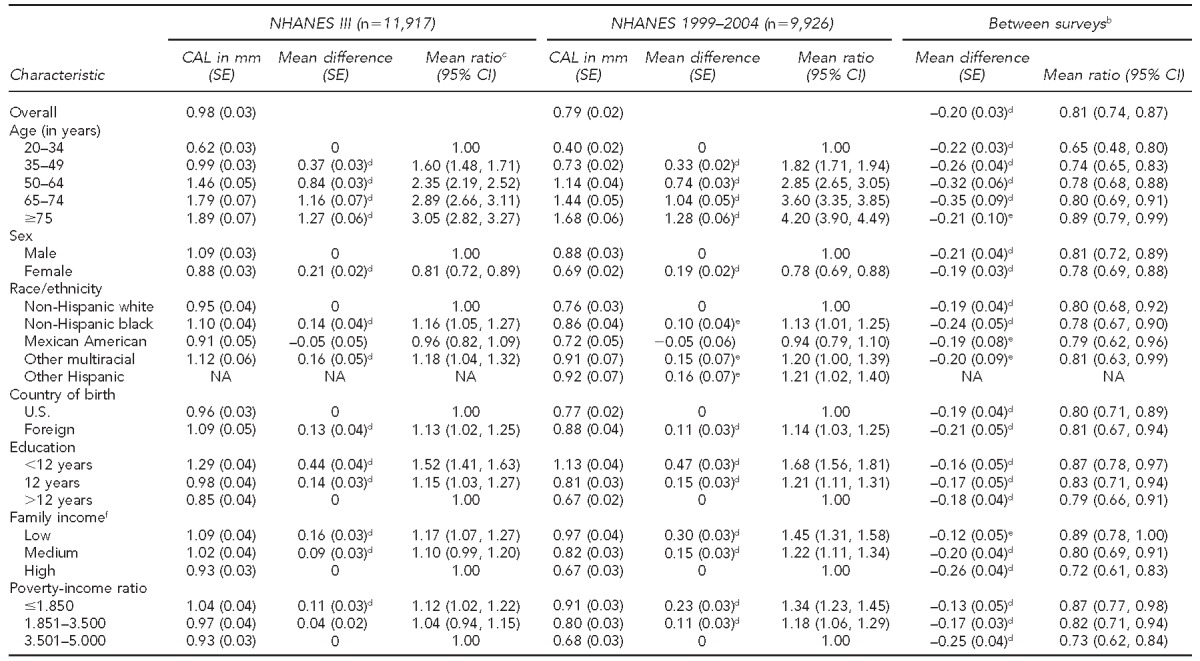
aMeans (SEs) for CAL for adults 20 years of age and older
bMean difference and ratio compare NHANES 1999–2004 with NHANES III (1988–1994).
cSEs for ratios calculated using the delta method from estimates obtained from SUDAAN
dp<0.01 for t-test assessing the difference between the prevalence of each level of the characteristic and the level assigned as the reference
ep<0.05 for t-test assessing the difference between the prevalence of each level of the characteristic and the level assigned as the reference
fLow, medium, and high categories for income were <$14,999, $15,000–$24,999, and ≥$25,000 in NHANES III and <$19,999, $20,000–$44,999, and ≥$45,000 in NHANES 1999–2004, respectively.
NHANES = National Health and Nutrition Examination Survey
CAL = clinical attachment loss
mm = millimeters
SE = standard error
CI = confidence interval
NA = not applicable
Consistent with the findings reported in Table 1, the between-group STI (STIB) for the prevalence of periodontal disease suggests statistically significant differences for comparison among groups of age, sex, race/ethnicity, education, income, and PIR within survey, with values ranging from 2.21% for sex to 6.47% for education in NHANES III, and 3.41% for sex to 8.94% for age in NHANES 1999–2004 (Table 4). This finding was also true for country of birth in NHANES 1999–2004, with a statistically significant STIB of 2.36%. Further, while the prevalence of periodontal disease appeared to decrease between surveys and between groups of the population (Table 1), the comparisons of STIB between surveys (Table 4) were statistically significant for race/ethnicity, country of birth, and income (all p-values <0.05), suggesting that inequalities across groups within these characteristics have increased in NHANES 1999–2004 compared with NHANES III.
Table 4.
Symmetrized Theil Index for disparities in the prevalence and severity of periodontal disease among U.S. adults 20 years of age and older for selected sociodemographic characteristics: NHANES III (1988–1994) and NHANES 1999–2004
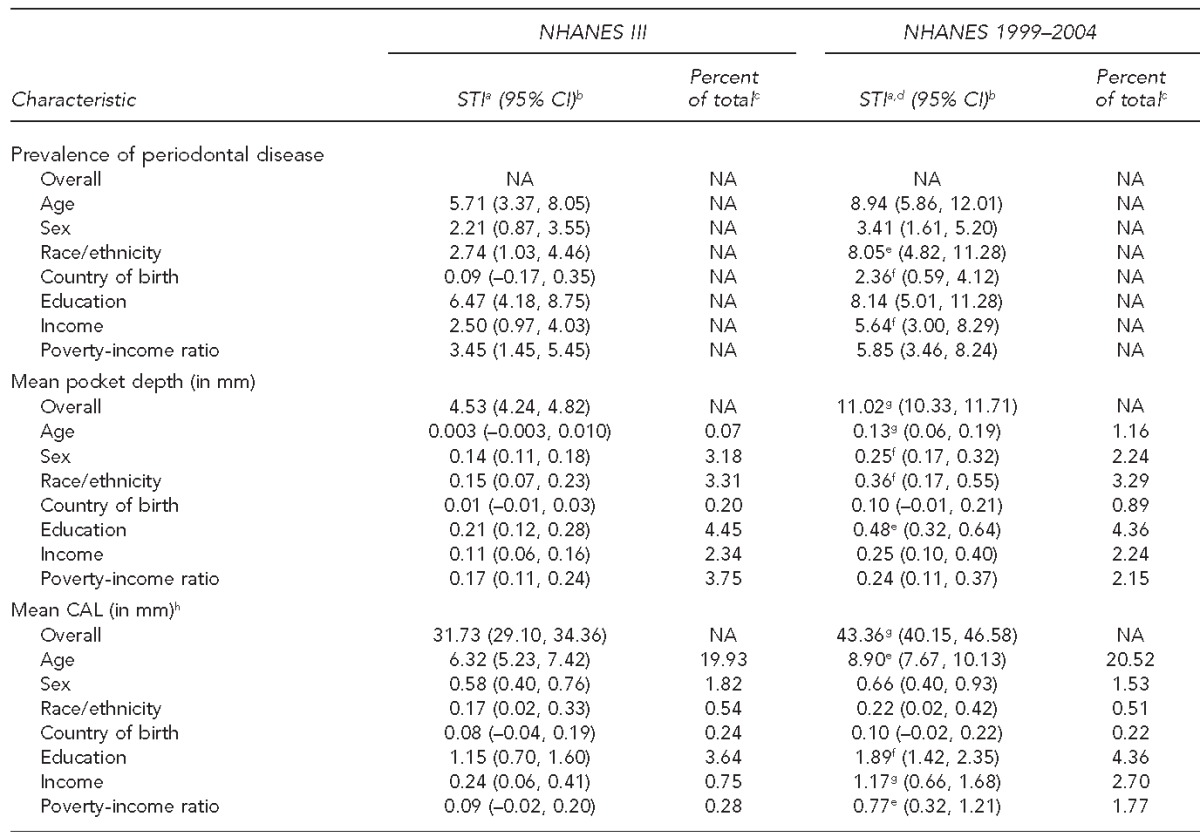
aWith the exception of the overall STI for the mean pocket depth and CAL, the STI is the between-group STI for the characteristics presented.
bDesign-based standard errors computed via Taylor series linearization were used for the CIs.
cThe percent is the proportion of the overall STI corresponding to its between-group component.
dStatistically significant pairwise comparisons of STI between surveys for prevalence of periodontal diseases and mean pocket depth and CAL for the overall and each variable indices
ep<0.01
fp<0.05
gp<0.001
hThe STI calculations for mean CAL are conditional on CAL >0.
NHANES = National Health and Nutrition Examination Survey
STI = Symmetrized Theil Index
CI = confidence interval
NA = not applicable
mm = millimeters
CAL = clinical attachment loss
Table 4 also shows the overall and between-group STI for the mean PD and CAL. The overall STI for PD significantly increased from 4.53% in NHANES III to 11.02% in NHANES 1999–2004 (p<0.001), underscoring an increase in disparities among those with periodontal disease within NHANES 1999–2004. Consistent with findings from Table 2, in both surveys, sex, race/ethnicity, education, income, and PIR explained a significant portion of the overall inequality in PD, with the proportion of the overall STI corresponding to its between-group component STIB ranging from 2.15% of the total for PIR in NHANES 1999–2004 to 4.45% of the total for education in NHANES III. Finally, the comparisons of STIB between surveys for mean PD were statistically significant for age, sex, race/ethnicity, and education (all p-values <0.05), suggesting that inequalities have increased in NHANES 1999–2004 compared with NHANES III for these sociodemographic groups.
Similarly, for the mean CAL for teeth with CAL >0, the overall STI significantly increased from 31.73% in NHANES III to 43.36% in NHANES 1999–2004 (p<0.001). Within surveys, age, sex, race/ethnicity, education, income, and PIR explained a significant portion of the overall inequality, with the proportion of the overall STI corresponding to its between-group component STIB ranging from 0.51% for race/ethnicity to 20.52% for age in NHANES 1999–2004. Finally, inequalities for mean CAL across groups of age, education, income, and PIR have significantly increased between surveys as indicated by the STIB between surveys (all p-values <0.05; Table 4).
DISCUSSION
Our findings suggest that inequalities in periodontal disease significantly decreased between NHANES III and NHANES 1999–2004 in the total population and across selected characteristics of the population when using the prevalence differences and ratios independent of the periodontal measure used—prevalence of periodontitis (a combination of PD and CAL), mean PD, or mean CAL. However, the STIB suggests that these inequalities increased within groups of the population in NHANES 1999–2004 compared with NHANES III. Specifically, statistically significant increases were observed for the prevalence of periodontitis across groups of race/ethnicity, country of birth, and income in NHANES 1999–2004 as compared with NHANES III. This increase was also observed for the overall STI for the mean PD and mean CAL: statistically significant increases were observed for STIB for the mean PD among groups within age, sex, race/ethnicity, and education, whereas the STIB for the mean CAL significantly increased between surveys for age, education, income, and PIR groups.
While our findings cannot be directly compared with previous studies, the findings for the prevalence differences and ratios are consistent with previous reports of changes in periodontal disease between NHANES III and NHANES 1999–2004.14,16,19,25 For instance, Dye et al.25 reported significant absolute decreases in the prevalence of periodontitis as well as the mean PD and mean CAL between NHANES III and NHANES 1999–2004. These findings were observed across age groups, sex, race/ethnicity, education, and poverty. Consistent with these findings, our study found that the prevalence of periodontal disease, the mean PD, and the mean CAL significantly decreased between surveys for age groups, sex, race/ethnicity, education, income, and PIR (Tables 1–3). Similarly, using data from NHANES III and NHANES 1999–2000 to examine racial/ethnic disparities, Borrell et al.16 found that the overall prevalence of periodontal disease decreased between NHANES III and NHANES 1999–2000. However, the racial/ethnic disparities have remained the same between surveys, with black people exhibiting higher odds of periodontal disease than white people. Moreover, two studies independently examining racial/ethnic and socioeconomic disparities in the prevalence odds of periodontal disease in NHANES III14 and NHANES 1999–200419 suggested that disparities for race/ethnicity increased, while for education, disparities decreased between NHANES III and NHANES 1999–2004. However, disparities across income groups remained nearly unchanged. -Consistent with previous studies,34,35,38 our study assessed inequalities in periodontal disease using new methods. We used the STI for both binary and continuous data and found that racial/ethnic and income inequalities in the prevalence of periodontal disease increased in NHANES 1999–2004 compared with NHANES III. Additionally, when compared with NHANES III, we found statistically significant increases in inequalities in the NHANES 1999–2004 mean PD for age, sex, race/ethnicity, and education and in the mean CAL for age, education, income, and PIR.
Our findings of a decrease in periodontitis from the prevalence differences and ratios between NHANES III and NHANES 1999–2004 and an increase from the STI in NHANES 1999–2004 compared with NHANES III complement each other and may shed light on the examination of health inequalities. For instance, while most studies of inequalities in periodontitis in the U.S.15,16,25 aimed to compare estimates across different points in time (i.e., NHANES I vs. NHANES III) when examining inequalities, the inequalities within the population for a particular point in time are usually neglected or seen as a different research question. Our findings suggest that to reduce and eventually eliminate inequalities in periodontitis and health in general, the between and within inequalities in population groups must be examined. Failure to account for inequalities within populations when examining inequalities over time not only may yield misleading conclusions, but also may ignore the needs of those at the very bottom of the social ladder.
Limitations
Limitations of the study include the cross-sectional nature of the data and the lack of information on the length of time individuals had been disadvantaged, which prevented us from making inferences regarding temporal ordering between exposure and disease. Moreover, a limitation inherent in national surveys collecting periodontal data is the use of partial-mouth examinations of only two sites (mesiobuccal and midfacial) in two randomly selected quadrants of the mouth, and the assumption that these measurements are representative of the full mouth.56,57 In fact, a recent study suggests that the partial-mouth periodontal examination protocols used in NHANES III and NHANES 2001–2004 could underestimate the prevalence of periodontitis by 50% or greater.58 Therefore, our findings could be underestimating the true inequalities in periodontal disease in the U.S.
CONCLUSIONS
This study indicated that inequalities in periodontal disease significantly decreased between NHANES III and NHANES 1999–2004 in the total population and across selected characteristics of the population when using the prevalence differences and ratios. However, the STI suggested that inequalities in periodontal health within age, sex, race/ethnicity, education, and income characteristics increased in NHANES 1999–2004 compared with NHANES III. These findings called attention to the absolute and relative differences not only between population groups over time, but also within population groups at a particular point in time and over time. The latter could provide a better dimension of where we stand on the quest for eliminating health inequalities for all.
Footnotes
This study was supported by the National Institute for Dental and Craniofacial Research (R03DE017901). This study was exempt from Institutional Review Board approval.
REFERENCES
- 1.Nikias MK, Fink R, Sollecito W. Oral health status in relation to socioeconomic and ethnic characteristics of urban adults in the U.S.A. Community Dent Oral Epidemiol. 1977;5:200–6. doi: 10.1111/j.1600-0528.1977.tb01641.x. [DOI] [PubMed] [Google Scholar]
- 2.Oliver RC, Brown LJ, Loe H. Variations in the prevalence and extent of periodontitis. J Am Dent Assoc. 1991;122:43–8. doi: 10.1016/s0002-8177(91)26016-x. [DOI] [PubMed] [Google Scholar]
- 3.Oliver RC, Brown LJ, Loe H. Periodontal diseases in the United States population. J Periodontol. 1998;69:269–78. doi: 10.1902/jop.1998.69.2.269. [DOI] [PubMed] [Google Scholar]
- 4.Elter JR, Beck JD, Slade GD, Offenbacher S. Etiologic models for incident periodontal attachment loss in older adults. J Clin Periodontol. 1999;26:113–23. doi: 10.1034/j.1600-051x.1999.260209.x. [DOI] [PubMed] [Google Scholar]
- 5.White BA, Caplan DJ, Weintraub JA. A quarter century of changes in oral health in the United States. J Dent Educ. 1995;59:19–57. [PubMed] [Google Scholar]
- 6.Caplan DJ, Weintraub JA. The oral health burden in the United States: a summary of recent epidemiologic studies. J Dent Educ. 1993;57:853–62. [PubMed] [Google Scholar]
- 7.Albandar JM. Periodontal diseases in North America. Periodontol 2002. 2000;29:31–69. doi: 10.1034/j.1600-0757.2002.290103.x. [DOI] [PubMed] [Google Scholar]
- 8.Borrell LN, Burt BA, Warren RC, Neighbors HW. The role of individual and neighborhood social factors on periodontitis: the third National Health and Nutrition Examination Survey. J Periodontol. 2006;77:444–53. doi: 10.1902/jop.2006.050158. [DOI] [PubMed] [Google Scholar]
- 9.Borrell LN, Burt BA, Neighbors HW, Taylor GW. Social factors and periodontitis in an older population. Am J Public Health. 2004;94:748–54. doi: 10.2105/ajph.94.5.748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Albandar JM, Brunelle JA, Kingman A. Destructive periodontal disease in adults 30 years of age and older in the United States, 1988-1994. J Periodontol. 1999;70:13–29. doi: 10.1902/jop.1999.70.1.13. [DOI] [PubMed] [Google Scholar]
- 11.Albandar JM, Kingman A, Brown LJ, Loe H. Gingival inflammation and subgingival calculus as determinants of disease progression in early-onset periodontitis. J Clin Periodontol. 1998;25:231–7. doi: 10.1111/j.1600-051x.1998.tb02433.x. [DOI] [PubMed] [Google Scholar]
- 12.Hyman JJ, Reid BC. Epidemiologic risk factors for periodontal attachment loss among adults in the United States. J Clin Periodontol. 2003;30:230–7. doi: 10.1034/j.1600-051x.2003.00157.x. [DOI] [PubMed] [Google Scholar]
- 13.Dye BA, Selwitz RH. The relationship between selected measures of periodontal status and demographic and behavioural risk factors. J Clin Periodontol. 2005;32:798–808. doi: 10.1111/j.1600-051X.2005.00742.x. [DOI] [PubMed] [Google Scholar]
- 14.Borrell LN, Lynch J, Neighbors H, Burt BA, Gillespie BW. Is there homogeneity in periodontal health between African Americans and Mexican Americans? Ethn Dis. 2002;12:97–110. [PubMed] [Google Scholar]
- 15.Borrell LN, Burt BA, Gillespie BW, Lynch J, Neighbors H. Race and periodontitis in the United States: beyond black and white. J Public Health Dent. 2002;62:92–101. doi: 10.1111/j.1752-7325.2002.tb03428.x. [DOI] [PubMed] [Google Scholar]
- 16.Borrell LN, Burt BA, Taylor GW. Prevalence and trends in periodontitis in the USA: the [corrected] NHANES, 1988 to 2000 [published erratum appears in J Dent Res 2006;85:287] J Dent Res. 2005;84:924–30. doi: 10.1177/154405910508401010. [DOI] [PubMed] [Google Scholar]
- 17.Douglass CW, Gillings D, Sollecito W, Gammon M. National trends in the prevalence and severity of the periodontal diseases. J Am Dent Assoc. 1983;107:403–12. doi: 10.14219/jada.archive.1983.0273. [DOI] [PubMed] [Google Scholar]
- 18.Locker D, Leake JL. Risk indicators and risk markers for periodontal disease experience in older adults living independently in Ontario, Canada. J Dent Res. 1993;72:9–17. doi: 10.1177/00220345930720011501. [DOI] [PubMed] [Google Scholar]
- 19.Borrell LN, Crawford ND. Social disparities in periodontitis among United States adults 1999-2004. Community Dent Oral Epidemiol. 2008;36:383–91. doi: 10.1111/j.1600-0528.2007.00406.x. [DOI] [PubMed] [Google Scholar]
- 20.Kelly JE, Van Kirk LE. Periodontal disease in adults. United States, 1960-1962. Vital Health Stat 11. 1965 12. [Google Scholar]
- 21.Kelly JE, Harvey CR. Basic data on dental examination findings of persons 1-74 years. United States, 1971-1974. Vital Health Stat 11. 1979 214. [PubMed] [Google Scholar]
- 22.Capilouto ML, Douglass CW. Trends in the prevalence and severity of periodontal diseases in the US: a public health problem? J Public Health Dent. 1988;48:245–51. doi: 10.1111/j.1752-7325.1988.tb03206.x. [DOI] [PubMed] [Google Scholar]
- 23.Drury TF, Garcia I, Adesanya M. Socioeconomic disparities in adult oral health in the United States. Ann N Y Acad Sci. 1999;896:322–4. doi: 10.1111/j.1749-6632.1999.tb08129.x. [DOI] [PubMed] [Google Scholar]
- 24.Department of Health and Human Services (US), Office of the Surgeon General. Oral health in America: a report of the Surgeon General. Rockville (MD): HHS, National Institute of Dental and Craniofacial Research, National Institutes of Health; 2000. [Google Scholar]
- 25.Dye BA, Tan S, Smith V, Lewis BG, Barker LK, Thornton-Evans G, et al. Trends in oral health status: United States, 1988-1994 and 1999-2004. Vital Health Stat 11. 2007 248. [PubMed] [Google Scholar]
- 26.Wagstaff A, Paci P, van Doorslaer E. On the measurement of inequalities in health. Soc Sci Med. 1991;33:545–57. doi: 10.1016/0277-9536(91)90212-u. [DOI] [PubMed] [Google Scholar]
- 27.Mackenbach JP, Kunst AE. Measuring the magnitude of socio-economic inequalities in health: an overview of available measures illustrated with two examples from Europe. Soc Sci Med. 1997;44:757–71. doi: 10.1016/s0277-9536(96)00073-1. [DOI] [PubMed] [Google Scholar]
- 28.Pearcy JN, Keppel KG. A summary measure of health disparity. Public Health Rep. 2002;117:273–80. doi: 10.1016/S0033-3549(04)50161-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Regidor E. Measures of health inequalities: part 1. J Epidemiol Community Health. 2004;58:858–61. doi: 10.1136/jech.2003.015347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Regidor E. Measures of health inequalities: part 2. J Epidemiol Community Health. 2004;58:900–3. doi: 10.1136/jech.2004.023036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Keppel K, Pamuk E, Lynch J, Carter-Pokras O, Kim Ins un, Mays V, et al. Methodological issues in measuring health disparities. Vital Health Stat 2. 2005 141. [PMC free article] [PubMed] [Google Scholar]
- 32.Harper S, Lynch J. NCI Cancer Surveillance Monograph Series, Number 6. NIH Publication No. 05-5777. Bethesda (MD): National Cancer Institute; 2005. Methods for measuring cancer disparities: a review using data relevant to Healthy People 2010 cancer-related objectives. [Google Scholar]
- 33.Harper S, Lynch J. Measuring health inequalities. In: Oakes JM, Kaufman JS, editors. Methods in social epidemiology. San Francisco: Jossey-Bass; 2006. pp. 134–68. [Google Scholar]
- 34.Cheng NF, Han PZ, Gansky SA. Methods and software for estimating health disparities: the case of children's oral health. Am J Epidemiol. 2008;168:906–14. doi: 10.1093/aje/kwn207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Harper S, Lynch J, Meersman SC, Breen N, Davis WW, Reichman ME. An overview of methods for monitoring social disparities in cancer with an example using trends in lung cancer incidence by area-socioeconomic position and race-ethnicity, 1992-2004. Am J Epidemiol. 2008;167:889–99. doi: 10.1093/aje/kwn016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Theil H. Economics and information theory. Amsterdam (The Netherlands): North-Holland Publishing Co.; 1967. [Google Scholar]
- 37.Firebaugh G. The new geography of global income inequality. Cambridge (MA): Harvard University Press; 2003. [Google Scholar]
- 38.Borrell LN, Talih M. A symmetrized Theil index measure of health disparities: an example using dental caries in U.S. children and adolescents. Stat Med. 2011;30:277–90. doi: 10.1002/sim.4114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Levy JI, Chemerynski SM, Tuchmann JL. Incorporating concepts of inequality and inequity into health benefits analysis. Int J Equity Health. 2006;5:2. doi: 10.1186/1475-9276-5-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.National Center for Health Statistics (US). Plan and operation of the Third National Health and Nutrition Examination Survey, 1988-94. Vital Health Stat 1. 1994 32. [PubMed] [Google Scholar]
- 41.Ezzati TM, Massey JT, Waksberg J, Chu A, Maurer KR. Sample design: Third National Health and Nutrition Examination Survey. Vital Health Stat 2. 1992 113. [PubMed] [Google Scholar]
- 42.Centers for Disease Control and Prevention (US), National Center for Health Statistics. National Health and Nutrition Examination Survey. Questionnaires, datasets and related documentation, 1999-2004. [cited 2009 Jul 3]. Available from: URL: http://www.cdc.gov/nchs/nhanes/nhanes_questionnaires.htm.
- 43.Winn DM, Johnson CL, Kingman A. Periodontal disease estimates in NHANES III: clinical measurement and complex sample design issues. J Public Health Dent. 1999;59:73–8. doi: 10.1111/j.1752-7325.1999.tb03238.x. [DOI] [PubMed] [Google Scholar]
- 44.Dye BA, Barker LK, Selwitz RH, Lewis BG, Wu T, Fryar CD, et al. Overview and quality assurance for the National Health and Nutrition Examination Survey (NHANES) oral health component, 1999-2002. Community Dent Oral Epidemiol. 2007;35:140–51. doi: 10.1111/j.1600-0528.2007.00310.x. [DOI] [PubMed] [Google Scholar]
- 45.Dye BA, Nowjack-Raymer R, Barker LK, Nunn JH, Steele JG, Tan S, et al. Overview and quality assurance for the oral health component of the National Health and Nutrition Examination Survey (NHANES), 2003-04. J Public Health Dent. 2008;68:218–26. doi: 10.1111/j.1752-7325.2007.00076.x. [DOI] [PubMed] [Google Scholar]
- 46.Beck JD, Koch GG, Rozier RG, Tudor GE. Prevalence and risk indicators for periodontal attachment loss in a population of older community-dwelling blacks and whites. J Periodontol. 1990;61:521–8. doi: 10.1902/jop.1990.61.8.521. [DOI] [PubMed] [Google Scholar]
- 47.Machtei EE, Christersson LA, Grossi SG, Dunford R, Zambon JJ, Genco RJ. Clinical criteria for the definition of “established periodontitis”. J Periodontol. 1992;63:206–14. doi: 10.1902/jop.1992.63.3.206. [DOI] [PubMed] [Google Scholar]
- 48.Department of Labor (US), Bureau of Labor Statistics. Databases, tables and calculators by subject. Consumer Price Index inflation calculator. [cited 2009 Aug 12]. Available from: URL: http://www.bls.gov/data/inflation_calculator.htm.
- 49.Centers for Disease Control and Prevention (US), National Center for Health Statistics. Hyattsville (MD): CDC, NCHS; 1996. NHANES III reference nanual and reports [CD-ROM] [Google Scholar]
- 50.Centers for Disease Control and Prevention (US), National Center for Health Statistics. National Health and Nutrition Examination Survey. Questionnaires, datasets and related documentation, 1999-2004. NHANES 1999-2000 addendum to the NHANES III analytic guidelines. Updated August 30, 2002. [cited 2009 Aug 4]. Available from: URL: http://www.cdc.gov/nchs/data/nhanes/guidelines1.pdf.
- 51.SAS Institute, Inc. SAS®. Version 9.2. Cary (NC): SAS Institute, Inc.; 2009. [Google Scholar]
- 52.R Development Core Team. R: a language and environment for statistical computing [ISBN 3-900051-07-0] Vienna (Austria): R Foundation for Statistical Computing; 2010. [Google Scholar]
- 53.Lumley T. Analysis of complex survey samples. J Stat Software. 2004;9:1–19. [Google Scholar]
- 54.Lumley T. Analysis of complex survey samples. R package version 3.16. 2009. [cited 2011 Jan 8]. Available from: URL: http://cran.fhcrc.org/web/packages/survey/index.html.
- 55.Research Triangle Institute. SUDAAN®: Release 10.0. Research Triangle Park (NC): Research Triangle Institute; 2008. [Google Scholar]
- 56.Kingman A, Albandar JM. Methodological aspects of epidemiological studies of periodontal diseases. Periodontol 2000. 2000;29:11–30. doi: 10.1034/j.1600-0757.2002.290102.x. [DOI] [PubMed] [Google Scholar]
- 57.Susin C, Kingman A, Albandar JM. Effect of partial recording protocols on estimates of prevalence of periodontal disease. J Periodontol. 2005;76:262–7. doi: 10.1902/jop.2005.76.2.262. [DOI] [PubMed] [Google Scholar]
- 58.Eke PI, Thornton-Evans GO, Wei L, Borgnakke WS, Dye BA. Accuracy of NHANES periodontal examination protocols. J Dent Res. 2010;89:1208–13. doi: 10.1177/0022034510377793. [DOI] [PubMed] [Google Scholar]


