The 2009 H1N1 influenza pandemic was first identified in April 20091 and rapidly spread worldwide.2 In the northern hemisphere, a first wave began in April 2009, peaking in June, followed by relatively low activity during July and August. By September, H1N1 activity began increasing once again, at higher rates than in June, suggesting a larger wave of influenza activity had begun.3 Minnesota clinics reported experiencing very high numbers of patients seeking care, including those with influenza symptoms and the worried-well, as in other parts of the United States and the world.4–6 As more ill patients sought in-person health care, there were more opportunities for influenza transmissions to occur within the crowded health-care system (HCS). Additionally, some facilities reported spot shortages and low inventories of personal protective equipment, such as N95 masks and surgical masks.
Rapid access to H1N1 antiviral treatment became increasingly problematic in September 2009. Given the high number of people seeking care, patients were encountering delays in reaching health-care providers, including patients at increased risk for severe disease who were advised to receive an antiviral prescription (e.g., those with underlying health conditions, young children, and pregnant women). The uninsured and underinsured encountered barriers due to the cost of a health-care provider visit in addition to the cost of an antiviral if indicated. Complicating these concerns was the possibility that overuse and misuse of antivirals may lead to oseltamivir resistance, as was observed in the 2008–2009 circulating seasonal H1N1 influenza strain.
The Minnesota Department of Health (MDH) developed multiple tools to support health-care providers. Information and fact sheets on H1N1 disease activity, vaccine availability, preventing illness, and describing people at risk for more severe disease were developed and distributed through a unique MDH website.7 Specific guidance was created for HCSs on the use of antiviral medications, vaccine distribution and utilization, and infection control in conjunction with the U.S. Centers for Disease Control and Prevention (CDC). Additionally, MDH prioritized the use of Minnesota cache antiviral medications for uninsured or underinsured patients, and for instances when there was a disruption in the market supply. In September 2009, as influenza activity was increasing in Minnesota, an HCS sought guidance from MDH to assist with options for the anticipated surge of people seeking health care.
Nurse triage lines (NTLs) and information lines have been utilized by HCSs for routine patient care, with some jurisdictions utilizing information lines during the H1N1 pandemic.8–11 It was determined that an NTL would be the most effective, rapidly deployed method of meeting the needs of the H1N1-associated health-care surge. A coordinated statewide NTL system called the MN FluLine (Minnesota FluLine) was created to address the following objectives: (1) decrease public confusion by providing accurate information, –consistent messaging, and assistance, including use of antiviral medications; (2) decrease the spread of disease by reducing the volume of sick individuals gathering in health-care settings; (3) reduce medical surge on the HCS to ensure that other priority medical needs would continue to be met; and (4) meet the needs of uninsured or underinsured patients, and those without easy access to health care.
PROJECT DESCRIPTION
MDH was approached by an HCS with the idea of establishing a coordinated, statewide NTL system with a single toll-free number for Minnesotans in September 2009. All HCSs with operations in Minnesota that had an NTL were contacted to participate in this public-private partnership. During a series of teleconferences with 14 Minnesota-based public and private health organization partners—including the Minnesota Hospital Association and the Minnesota Council of Health Plans—and one face-to-face meeting, the structure and functions of the MN FluLine were established. MDH contracted an NTL vendor to operate the MN FluLine toll-free number 24 hours per day, seven days per week. All nurses performing triage services by the vendor were licensed registered nurses (RNs).
MDH created a single clinical evaluation algorithm and a protocol for standing orders based on CDC treatment and prevention guidelines targeting people with symptoms of influenza-like illness (ILI) and those with exposure to someone with ILI. ILI was defined as a fever >100.0°F and cough or sore throat. A draft version of the protocol was provided to the medical directors of partner NTLs for feedback. The edited protocol was adopted by all participating HCS partners and administered uniformly. Adaptation of the protocol to make it compatible with the NTL's own electronic health-care record system was allowed.
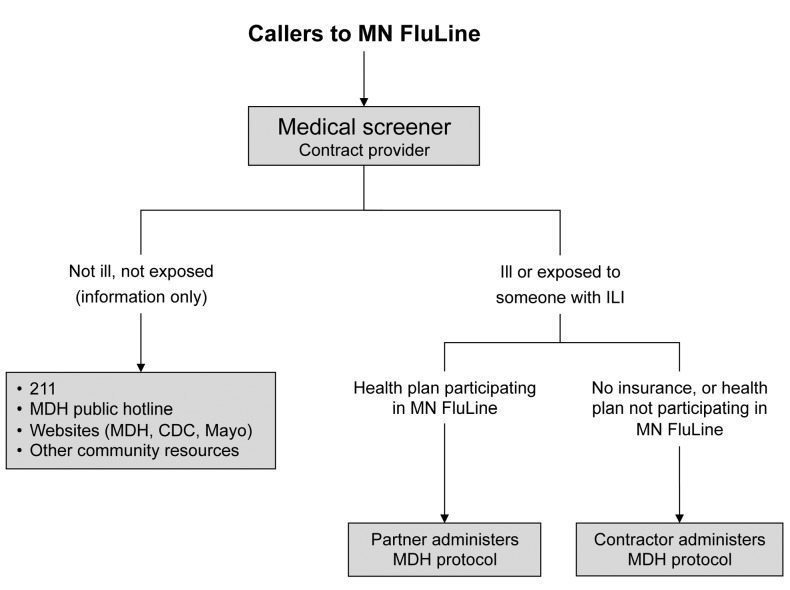
Upon first calling the MN FluLine, all callers received a standard message with information on influenza. If the caller remained on the line to speak with the medical screener but had no symptoms, he or she was referred to influenza information resources, such as general information hotlines, United Way 211, and websites. To maintain continuity of care, once screened, all callers associated with an HCS that operated a participating NTL were transferred from the toll-free number to their HCS NTL where the standardized protocol was administered. If the caller was affiliated with a health organization without an NTL, or if the caller reported not having insurance, the call was maintained by the contract vendor of the MN FluLine, who administered the standardized protocol. For all calls managed by the contract NTL, contact information was recorded by the medical screener, and the caller was placed in a queue for a nurse to return the call (Figure 1).
Figure 1.
MN FluLinea system design
aA statewide nurse triage line responding to 2009 H1N1 influenza in Minnesota providing clinical evaluation, referral to appropriate level of care based on symptoms, infection prevention recommendations, and an antiviral prescription when indicated
MN = Minnesota
MDH = Minnesota Department of Health
CDC = Centers for Disease Control and Prevention
Mayo = Mayo Clinic
ILI = influenza-like illness
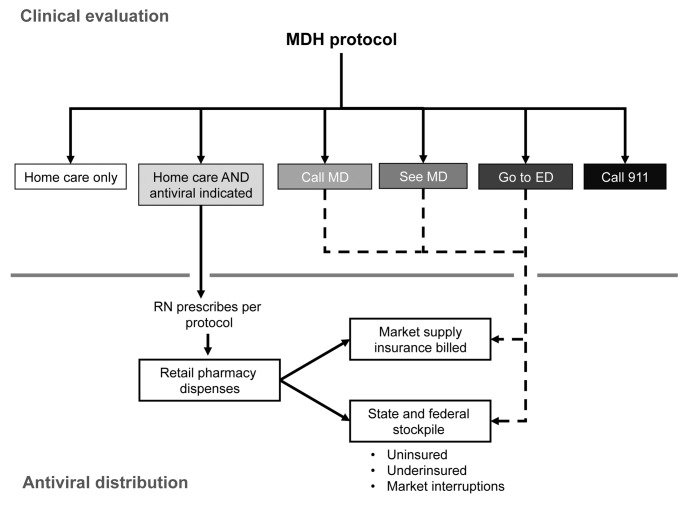
Based on the standardized triage protocol administered by the contract NTL and all other participating NTLs, callers with symptoms were recommended to one of the following dispositions: (1) continue care at home, (2) contact a health-care provider, (3) see a health-care provider, (4) go to the emergency department, or (5) call 911 (Figure 2). If callers were recommended to remain at home but were determined to be at increased risk for severe ILI based on CDC treatment guidelines for treating patients with health conditions that increase the risk for severe complications of influenza, an antiviral (oseltamivir) was prescribed by the contract NTL nurse. Prescriptions were phoned in to the caller's pharmacy of choice for people currently in Minnesota. Before the call was completed, all callers (except those who were recommended to go to the emergency department or call 911) were provided in-depth home care information, infection prevention instructions, information on oseltamivir and side effects if appropriate, and information about when to seek future care for the illness.
Figure 2.
MN FluLinea disposition design
aA statewide nurse triage line responding to 2009 H1N1 influenza in Minnesota providing clinical evaluation, referral to appropriate level of care based on symptoms, infection prevention recommendations, and an antiviral prescription when indicated
MN = Minnesota
MDH = Minnesota Department of Health
MD = medical doctor
ED = emergency department
RN = registered nurse
At the designated local pharmacy, if the patient had insurance and there was no market interruption in the supply, a treatment course of oseltamivir was dispensed, and insurance was billed. If the patient was uninsured or underinsured, oseltamivir from pre-positioned state cache antivirals was dispensed at no cost to the patient or with an option of a low-cost fee.
MDH created a legal assessment that, along with the algorithm and protocol, explained the legal framework of the MN FluLine. The order to dispense antivirals via protocol was executed by the State Epidemiologist under authority delegated by the Commissioner of Health. As the contract vendor for the MN FluLine was acting on behalf of the state of Minnesota, per Minnesota Statutes 13.04,12 all callers were provided a privacy statement before private health data were collected. Prescribing via protocol by RNs is allowed under MN Statute 151.37.13
Five weeks after planning was initiated, the MN FluLine began operations on October 21, 2009. MDH held a press conference announcing its launch, which was highly attended by local media, and provided subsequent regular interviews based on inquiries from statewide media outlets. Paid advertisements were placed in specific language media outlets, and MDH's influenza website7 had information on the MN FluLine positioned prominently on its main page. The MN FluLine discontinued service on March 31, 2010.
The total number of calls to the toll-free number was based on telephone company data. The NTL contract provider collected data on the number of calls evaluated by the medical screener, the number of calls referred to the partner NTL, and the demographics and disposition of calls for callers with ILI or exposed to someone with ILI. Surveillance for hospitalized cases of laboratory-confirmed influenza was conducted statewide by MDH during the time frame of the MN FluLine's implementation.3 Minnesota county population data used to calculate call rates were based on the U.S. Census Bureau's 2009 intercensal estimates.14
RESULTS
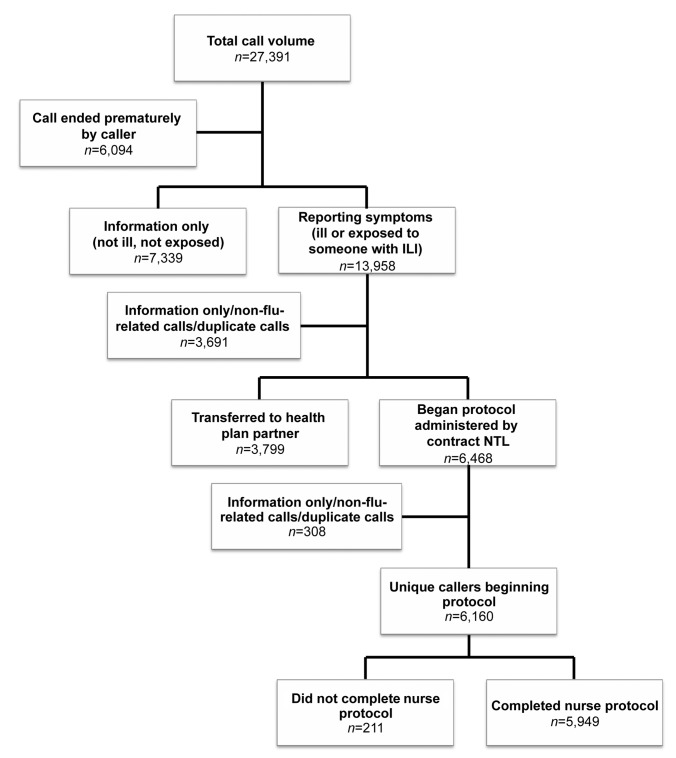
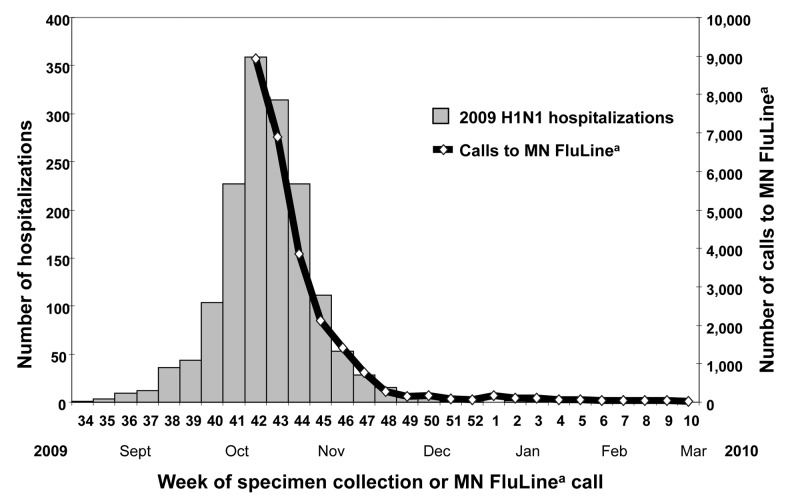
From October 21, 2009, to March 31, 2010, the MN FluLine received 27,391 calls (Figure 3). There was an initial overwhelming response following the launch of the MN FluLine, with more than 9,000 calls in the first 10 days of service. The majority of calls (56%) occurred during the month of October, with demand tapering off during subsequent weeks corresponding to a decreasing number of hospitalizations due to H1N1 (Figure 4). The MN FluLine was initiated the same week the number of hospitalizations peaked in Minnesota.
Figure 3.
Flowchart of all MN FluLinea callers: Minnesota, October 2009–March 2010
aA statewide nurse triage line responding to 2009 H1N1 influenza in Minnesota providing clinical evaluation, referral to appropriate level of care based on symptoms, infection prevention recommendations, and an antiviral prescription when indicated
MN = Minnesota
ILI = influenza-like illness
NTL = nurse triage line
Figure 4.
Hospitalized, PCR-confirmed 2009 H1N1 cases and calls to the MN FluLinea: Minnesota, September 2009–February 2010
aA statewide nurse triage line responding to 2009 H1N1 influenza in Minnesota providing clinical evaluation, referral to appropriate level of care based on symptoms, infection prevention recommendations, and an antiviral prescription when indicated
PCR = polymerase chain reaction
MN = Minnesota
Of the callers, 6,094 voluntarily ended their call after hearing the standard message with information on H1N1 and related resources, leaving a total of 21,297 callers evaluated by the medical screener. Of those callers, 13,958 (66%) reported ILI symptoms or exposure to someone with ILI, and 7,339 (34%) reported not having ILI or exposure to someone with ILI and were referred to general H1N1 information resources. Of those reporting ILI symptoms or exposure to someone with ILI symptoms based on the medical screener data, 3,691 were information-only, non-flu-related, or duplicate calls; 3,799 were transferred to a partner HCS with an NTL for protocol administration; and 6,468 were managed by the MN FluLine contract provider. After excluding additional duplicates, non-flu-related, and information-only calls based on NTL nurse data, a total of 6,160 unique callers (22% of all callers) were triaged by the NTL contract provider. Of those callers, 5,949 (97%) completed the MN FluLine nurse protocol (Figure 3).
There was an approximately even distribution of calls by day, with 24% of calls occurring on Saturday or Sunday. The mean length of call to the MN FluLine was 13 minutes, with a range of 0–70 minutes. MN FluLine patients ranged in age from 26 days to 96 years; 35% of patients were younger than 10 years of age, and the average age was 26 years. The majority of patients were female (58%). The majority of callers were calling on behalf of someone else (56%). Among the 88% of callers who reported their insurance status, 14% reported no insurance coverage (data not shown in Figures).
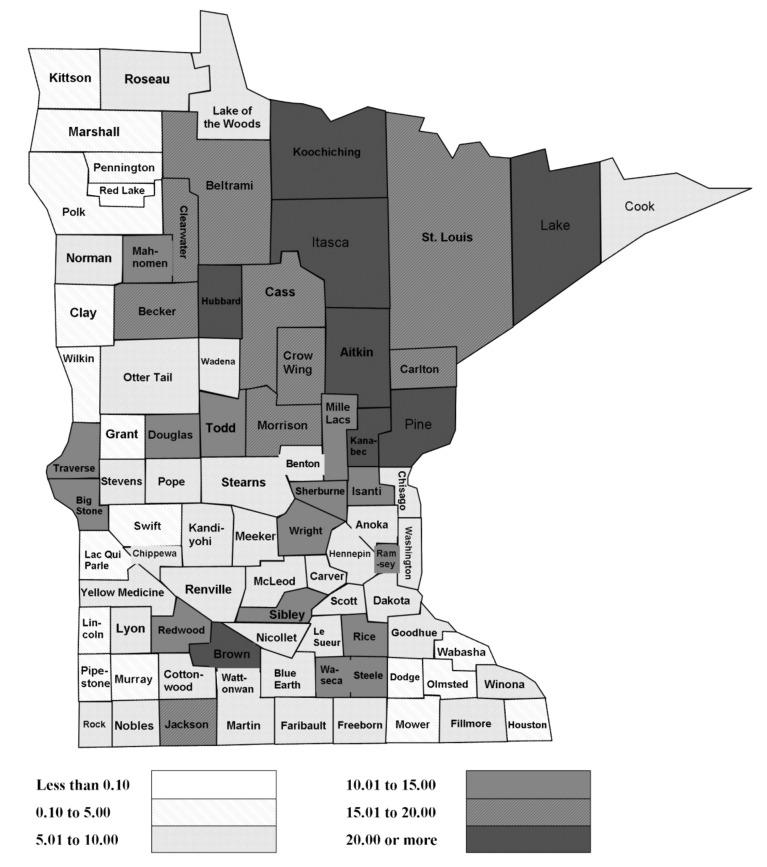
Eighty-eight percent (n=5,445) of callers reported they were currently located in Minnesota. Calls were received from 86 of Minnesota's 87 counties, and a map of call rates by county shows that the highest call rates per capita were from rural areas (Figure 5). Based on 5,445 Minnesotans calling the MN FluLine, approximately one of every 1,000 Minnesotans utilized the service.
Figure 5.
MN FluLinea call rates per 10,000 population, by county: Minnesota, October 2009–March 2010
aA statewide nurse triage line responding to 2009 H1N1 influenza in Minnesota providing clinical evaluation, referral to appropriate level of care based on symptoms, infection prevention recommendations, and an antiviral prescription when indicated
MN = Minnesota
Of the 5,949 callers who received a disposition from the NTL contract provider, 2,666 (45%) were recommended to self/home care, 1,292 (22%) were instructed to see a health-care provider, 875 (15%) were instructed to visit an emergency department, 497 (8%) were instructed to call their health-care provider, 488 (8%) were provided information or advice only, 122 (2%) were instructed to call 911, and eight (<1%) were given an “other” disposition. Six percent (n=374) were prescribed oseltamivir by the NTL contract provider based on the protocol, of which 161 received adult dosing and 213 received pediatric dosing. Oseltamivir prescription rates for Minnesotans were highest in rural counties, similar to MN FluLine call rates by county (data not shown in Figures).
Of those who received a disposition, 3,659 callers (13% of all total callers) received a recommendation that did not involve seeking in-person health care. Including the 7,339 callers who contacted the MN FluLine but did not have symptoms of influenza (Figure 3), up to 10,998 in-person health-care encounters may have been prevented by the MN FluLine.
DISCUSSION
The pandemic due to 2009 H1N1 had a significant impact on our society, with years of life lost comparable with pandemics in 1957 and 1968.15 During the H1N1 pandemic, CDC recommended that health-care providers consider using telephone contact to reduce delays in treatment access16 and later published a report describing how to develop and implement an NTL as a means of addressing population needs during a pandemic.17 The MN FluLine was a statewide NTL that was developed in five weeks and began service at the peak of 2009 H1N1 activity during late October in Minnesota, mitigating some of the pandemic's impact on the health-care community.
Although other organizations utilized telephone lines during the 2009 H1N1 pandemic,8–10 the MN FluLine was, to our knowledge, the only statewide NTL implemented specifically to respond to the public health threat of 2009 H1N1 and to offer a prescription for an antiviral if indicated. It had a major impact on the Minnesota population and the health-care community, with one in every 1,000 Minnesotans accessing the MN FluLine during its operation. Many patients were children and were from rural areas with more limited health-care access. The frequency of callers who were uninsured (14%) was about 1.5 times the percentage of uninsured Minnesotans in 2009 (9.1%).18 The even distribution of calls by day emphasizes the importance of having services such as the MN FluLine available seven days per week.
Many of the challenges that occurred during the 2009 H1N1 pandemic were solved by creating a public-private partnership that included MDH, an existing highly experienced telephone nurse triage call center, and the state's largest health-care plans with NTLs. Prior to this process, there was no coordination or formal communication between HCS triage lines, and very few provided antiviral medication per a nurse protocol. This intervention was specifically designed to reduce the burden on medical providers by triaging patients and providing advice or antivirals as indicated. Critical to this intervention was its design and implementation in only five weeks. While other areas of the country also had NTL in response to H1N1,10 the MN FluLine was staffed by nurses utilizing a standardized protocol, who were able to prescribe antivirals and reach a large percentage of people living in the state.
There are many benefits to the use of telephone consultations as a response to a public health threat. They offer the ability to quickly standardize and update information, provide a safety net for uninsured and underinsured populations, decrease the exposure rate both for ill people and worried-well people seeking in-person care, and provide information and emotional support to people who are concerned about illness. NTLs are also beneficial in that they reduce strain on the HCS, offer high levels of patient satisfaction, and serve as a safe, efficient, and cost-effective method of information dissemination.19–24 Benefits can also be seen in reduced travel costs, reduced time away from school/work, and reduced childcare expenses.17
Limitations
There were several limitations in the design and implementation of the MN FluLine. The service was so overwhelmingly busy in the first week that additional infrastructure, including phone lines and automated systems, were needed to meet the demand. Initially, there was also some confusion in communication about the MN FluLine as to whether or not a person needed insurance to be able to call. Although this confusion was quickly clarified in MDH communications, it is possible that some people without insurance did not attempt to access the MN FluLine. Because callers could repeatedly access this service and were not assigned a unique identifier when they called, it is possible that there were repeat callers in our data. However, repeat callers may represent a change in the status of the patient. In this regard, each change in status could represent an instance where the caller would have sought in-person health care. It is also possible that people used the line for non-flu-related calls, therefore incurring costs that should not have been covered by this MDH service. Finally, an a priori collection of performance measures would likely have improved the types of data collected and would have provided greater clarity to our estimation of the MN FluLine's impact.
It was our experience that using a currently operating, experienced NTL was vital to the rapid implementation of the MN FluLine. Utilizing direct transfers from the contract NTL to other participating NTLs was also important in maintaining communication between the NTL and the caller's health-care provider. Additionally, accurate anticipation of caller volume could optimize the initial success but, as we experienced, can be difficult to predict. NTLs can be powerful tools in responding to public health emergencies, and future preparedness planning should include their use.
CONCLUSION
This public-private partnership leveraged public health and nurse triage expertise utilizing the existing telecommunications infrastructure to rapidly implement a focused and efficient health-care delivery system based on a standard protocol and statewide antiviral prescribing. The MN FluLine was implemented at the time of greatest need in Minnesota, reached many rural and uninsured Minnesotans, and may have prevented nearly 11,000 in-person health-care encounters. An activity such as the MN FluLine could be rapidly initiated to respond to multiple health-care threats, such as emerging infectious disease outbreaks or bioterrorism threats, or to provide health-care access following a natural disaster.
Acknowledgments
The authors thank Sanne Magnan, Richard Danila, Kristen Ehresmann, Dawn Ginzl, Aggie Leitheiser, Catherine Lexau, Craig Morin, Dave Orren, Kevin Sell, and Megan Thompson, all with the Minnesota Department of Health (MDH); Patsy Stinchfield with Children's Hospitals and Clinics of Minnesota; Alex Kallen and John Jernigan with the Centers for Disease Control and Prevention (CDC); Blue Cross and Blue Shield of Minnesota; Children's Physician Network; Fairview Health Service; HealthPartners; Mayo Clinic; Medica; Metropolitan Health Plan; OptumHealth; Park Nicollet Health Services; Prime West Health; UCare; and United Way 211. Financial support for the operation of the MN FluLine was provided by the CDC Public Health Emergency Response Grant (1H75TP000348).
Footnotes
The views expressed in this article are those of the authors and do not necessarily represent the views of CDC. This work was exempt from Institutional Review Board approval.
REFERENCES
- 1.Swine influenza A (H1N1) infection in two children—Southern California, March-April 2009. MMWR Morb Mortal Wkly Rep. 2009;58(15):400–2. [PubMed] [Google Scholar]
- 2.World Health Organization. Swine flu illness in the United States and Mexico—update 2. 2009. [cited 2010 Jan 11]. Available from: URL: http://www.who.int/csr/don/2009_04_26/en/index.html.
- 3.Minnesota Department of Health. Influenza, 2009. Minnesota Department of Health Disease Control Newsletter 2009. [cited 2011 Jan 11]. Available from: URL: http://www.health.state.mn.us/divs/idepc/newsletters/dcn/sum09/influenza.html.
- 4.Van Cleve WC, Hagan P, Lozano P, Mangione-Smith R. Investigating a pediatric hospital's response to an inpatient census surge during the 2009 H1N1 influenza pandemic. Jt Comm J Qual Patient Saf. 2011;37:376–82. doi: 10.1016/s1553-7250(11)37048-1. [DOI] [PubMed] [Google Scholar]
- 5.Brooks-Pollock E, Tilston N, Edmunds WJ, Eames KT. Using an online survey of healthcare-seeking behaviour to estimate the magnitude and severity of the 2009 H1N1 influenza epidemic in England. BMC Infect Dis. 2011;11:68. doi: 10.1186/1471-2334-11-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hersh AL, Stafford RS. Antiviral prescribing by office-based physicians during the 2009 H1N1 pandemic. Ann Intern Med. 2011;154:74–6. doi: 10.7326/0003-4819-154-1-201101040-00019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Minnesota Department of Health. Influenza (flu) [cited 2011 Feb 7]. Available from: URL: http://www.health.state.mn.us/divs/idepc/diseases/flu/index.html.
- 8.Rubin GJ, Aml̂ot R, Carter H, Large S, Wessely S, Page L. Reassuring and managing patients with concerns about swine flu: qualitative interviews with callers to NHS Direct. BMC Public Health. 2010;10:451. doi: 10.1186/1471-2458-10-451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.North F, Varkey P, Bartel GA, Cox DL, Jensen PL, Stroebel RJ. Can an office practice telephonic response meet the needs of a pandemic? Telemed J E Health. 2010;16:1012–6. doi: 10.1089/tmj.2010.0102. [DOI] [PubMed] [Google Scholar]
- 10.Clancy T, Neuwirth C, Bukowski G. Lessons learned in implementing a 24/7 public health call center in response to H1N1 in the state of New Jersey. Am J Disaster Med. 2009;4:253–60. [PubMed] [Google Scholar]
- 11.Cleary V, Balasegaram S, McCloskey B, Keeling D, Turbitt D. Pandemic (H1N1) 2009: setting up a multi-agency regional response centre—a toolkit for other public health emergencies. J Bus Contin Emer Plan. 2010;4:154–64. [PubMed] [Google Scholar]
- 12.Minnesota Office of the Revisor of Statutes. Minnesota Statutes. 13.04 Rights of subjects of data. [cited 2011 Apr 1]. Available from URL: https://www.revisor.mn.gov/statutes/?id=13.04.
- 13.Minnesota Office of the Revisor of Statutes. Minnesota Statutes. 151.37 Legend drugs, who may prescribe, possess. [cited 2011 Apr 1]. Available from: URL: https://www.revisor.mn.gov/statutes/?id=151.37.
- 14.Census Bureau (US) State and county quick facts. Minnesota. [cited 2010 Nov 1]. Available from: URL: http://quickfacts.census.gov/qfd/states/27000.html.
- 15.Viboud C, Miller M, Olson D, Osterholm M, Simonsen L. Preliminary estimates of mortality and years of life lost associated with the 2009 A/H1N1 pandemic in the U. PLoS Curr. 2010:RRN1153. doi: 10.1371/currents.RRN1153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Centers for Disease Control and Prevention (US) Updated interim recommendations for the use of antiviral medications in the treatment and prevention of influenza for the 2009-2010 season. 2009. [cited 2011 Jan 3]. Available from: URL: http://www.cdc.gov/h1n1flu/recommendations.htm.
- 17.Centers for Disease Control and Prevention (US) Coordinating call centers for responding to pandemic influenza and other public health emergencies. 2009. [cited 2010 Feb 22]; Available from: URL: http://emergency.cdc.gov/healthcare/pdf/FinalCallCenter WorkbookForWeb.pdf. [Google Scholar]
- 18.Minnesota Department of Health. Minnesota Health Access Survey. [cited 2010 Aug 2]; Available from: URL: https://pqc.health.state .mn.us/mnha/Welcome.action. [Google Scholar]
- 19.Lattimer V, George S, Thompson F, Thomas E, Mullee M, Turnbull J, et al. Safety and effectiveness of nurse telephone consultation in out of hours primary care: randomised controlled trial The South Wiltshire Out of Hours Project (SWOOP) Group. BMJ. 1998;317:1054–9. doi: 10.1136/bmj.317.7165.1054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Keatinge D, Rawlings K. Outcomes of a nurse-led telephone triage service in Australia. Int J Nurs Pract. 2005;11:5–12. doi: 10.1111/j.1440-172X.2005.00495.x. [DOI] [PubMed] [Google Scholar]
- 21.Venn MJ, Darling E, Dickens C, Quine L, Rutter DR, Slevin ML. The experience and impact of contacting a cancer information service. Eur J Cancer Care (Engl) 1996;5:38–42. doi: 10.1111/j.1365-2354.1996.tb00204.x. [DOI] [PubMed] [Google Scholar]
- 22.Marklund B, Str̈om M, Månsson J, Borgquist L, Baigi A, Fridlund B. Computer-supported telephone nurse triage: an evaluation of medical quality and costs. J Nurs Manag. 2007;15:180–7. doi: 10.1111/j.1365-2834.2007.00659.x. [DOI] [PubMed] [Google Scholar]
- 23.Cariello FP. Computerized telephone nurse triage An evaluation of service quality and cost. J Ambul Care Manage. 2003;26:124–37. doi: 10.1097/00004479-200304000-00005. [DOI] [PubMed] [Google Scholar]
- 24.Bunn F, Byrne G, Kendall S. Telephone consultation and triage: effects on health care use and patient satisfaction. Cochrane Database Syst Rev. 2004;(4):CD004180. doi: 10.1002/14651858.CD004180.pub2. [DOI] [PubMed] [Google Scholar]