Abstract
Background/Study Context
Musculoskeletal pain after motor vehicle collision is a substantial public health problem. The number of elderly individuals experiencing motor vehicle collision is increasing. We conducted analyses of data collected as part of a prospective observational study of outcomes after motor vehicle collision to estimates rates of persistent pain, pain interference, and change in physical function in patients 65 or older.
Methods
Adults presenting to one of four emergency departments following motor vehicle collision without severe or life-threatening injury were recruited. Outcomes were assessed using one month follow-up surveys.
Results
The frequencies of persistent moderate or severe pain resulting from the motor vehicle collision were similar among elderly and non-elderly participants, both in the neck region (27% vs. 30%) and in any region (60% vs. 56%). For both elderly and non-elderly patients, persistent pain was associated with high levels of interference with physical activity and mood.
Conclusion
Further studies of this vulnerable and rapidly increasing injury population are needed.
INTRODUCTION
Approximately 3.5 million people present to United States Emergency Departments (EDs) annually for evaluation following motor vehicle collision (MVC) (Zhao, Lucado et al. 2010). The great majority of adult patients do not have severe or life-threatening injury and are discharged to home after ED evaluation (McCaig 2009). However, North American studies indicate that 10–20% of these adults develop persistent musculoskeletal pain (Hartling, Brison et al. 2001; Suissa, Harder et al. 2001). While studies of post-MVC pain commonly focus on persistent post-MVC neck pain only, recent studies have shown that pain in other body regions is also common (Hincapie, Cassidy et al. 2010). The economic cost of persistent post-MVC musculoskeletal pain and associated disability has been estimated at $29 billion in the United States alone (Freeman, Croft et al. 1999).
By 2025, people 65 and older will account for 25% of U.S. drivers, up from 15% in 2005 (Safety 2008). Because of increases in the number of elderly, as well as increases in licensure rates and annual miles driven, the number of elderly individuals involved in police-reported crashes is projected to increase by 178% from 1999 to 2030 (Lyman, Ferguson et al. 2002). By 2030, over 2 million police reported collisions are expected to involve elderly drivers (Lyman, Ferguson et al. 2002). As with younger adults evaluated in the ED after MVC, more than 80% of elderly individuals experiencing MVC do not have severe or life-threatening injury and are discharged to home after ED evaluation (McCaig 2009). However, no prospective studies have examined the incidence and impact of persistent post-MVC pain in the elderly.
The purpose of this prospective pilot study was to develop preliminary estimates of rates of persistent pain and pain interference burden among elderly individuals presenting to the ED for evaluation after MVC and to compare these outcomes with those of non-elderly individuals. To accurately represent the most common patient group, only patients without severe or life-threatening injury who were discharged to home after ED evaluation were enrolled. In addition, to provide a relatively comprehensive assessment of pain outcomes, post-MVC overall body pain and back pain were assessed in addition to post-MVC neck pain. Based on data from non-injured populations and from retrospective studies of outcomes after MVC which included older adults (Rossignol, Suissa et al. 1988; Harder, Veilleux et al. 1998; Scudds and Mc 1998; Andersson 1999; Kendig, Browning et al. 2000; Jung, Johnson et al. 2004; Edwards 2006; Holm, Carroll et al. 2008; Ziegler, Rathmann et al. 2009), we hypothesized that persistent post-MVC pain would develop at similar rates in elderly and non-elderly individuals and that persistent pain in elderly patients would exact a substantial functional toll.
MATERIALS AND METHODS
Study Population
We analyzed data collected as part of a prospective observational study of patients evaluated at one of four EDs following MVC. All EDs were located in the state of Michigan, a “no fault” insurance state where litigation related to minor MVC is rare. A no-fault insurance state was chosen to avoid a societal environment where financial incentives promote symptom persistence (Cassidy, Carroll et al. 2000). Eligible patients included those who presented to the ED within 24 hours of MVC and were ≥ 18 years of age, English speaking, non-pregnant, and discharged to home after evaluation. Excluded patients included those who were clinically unstable, had potentially life-threatening or severe injuries (including patients with spinal fracture or dislocation, patients with neurologic abnormalities including decreased/absent deep tendon reflexes or weakness, skull fracture, facial fracture, intracranial injury, long bone fracture or laceration with significant hemorrhage), prisoners, and patients chronically using opioids. Additionally, any patient whom the treating provider anticipated would require admission to the hospital was excluded. Institutional review board approval was obtained at each of the four study sites, and written informed consent was obtained from all study patients.
Measures
After consent was obtained in the ED, all patients received an in-person ED interview followed by a one month telephone follow-up call. All interviews were conducted by trained research assistants using standardized questionnaires with explicit definitions of study variables. Training included completion of a mock patient interview and an online course of the protection of human research subjects. Over the 2 year period of data collection, research assistants met with the project investigators on a monthly basis to review procedures and address questions related to data collection. On average, there were two part-time research assistants available at each study site with most research assistants working for at least one year on the project. The ED and follow-up interviews used a previously validated 0–10 numeric rating scale for pain (Bijur, Latimer et al. 2003) to assess for new neck, back, and total pain symptom presence and intensity since the MVC. The assessment of pain in various body regions was not mutually exclusive. Consistent with previously established cut points (Fejer, Jordan et al. 2005) and clinical practice (Krebs, Carey et al. 2007), pain rated as ≥ 4 was defined as moderate or severe. The ED interview also included an assessment of patient demographic characteristics. Injury characteristics were determined from information in the medical record. The patient’s highest abbreviated injury severity score was also used to describe injury severity, with a score of 1 indicating mild injury and 2 indicating moderate injury (AAAM 1998). This scale was originally developed to characterize trauma patients with multiple injuries; we use the scale here to further characterize the study sample as one without severe or life-threatening injuries. At one month follow-up, pain interference with role-specific function was assessed using the pain interference questions from the Brief Pain Inventory (Daut RL, Cleeland CS et al. 1983). This questionnaire has been previously found to provide a valid and reliable measure of noncancer pain (Keller, Bann et al. 2004). The pain interference questions examine the interference of pain with seven different activities over the past week with responses provided on a 0 to 10 numeric rating scale. Physical function was measured in the ED and at one month follow-up using the Short Form (SF) 36 physical component summary score (Ware JE 1994). The ED assessment of physical function asked patients to provide answers based on their health during the 4 weeks prior to the accident. The physical component summary score uses responses to 22 questions to generate norm-based scoring for which the mean score for the U.S. population is 50 and the standard deviation is 10 (Ware JE 1994). This score was developed as part of an effort to determine the cost-effectiveness of health treatment but is widely used as a measure of various components of health (Ware and Sherbourne 1992). The scale is publicly available from the Research and Development Corporation (Santa Monica, CA). Health services utilization in the month following MVC was assessed using a standard questions.
Statistical Analysis
Adults ≥ 65 years old were categorized as elderly. Sociodemographic characteristics for elderly vs. non-elderly patients are described. The percentages of patients with moderate or severe pain in any location and in the neck and back along with 95% confidence intervals are calculated for elderly and non-elderly patients. Mean pain interference scores and SF-36 physical component summary scores for patients with and without moderate/severe pain are presented by age group. Physical component summary scores were converted to norm-based scores using a published scoring algorithm (Ware JE 1994; Ware JE 2000). Health-care-utilization during the month following the collision is also presented for elderly and non-elderly individuals. Calculations of means and standard errors were performed using PASW 17.0 software (SPSS Inc., Chicago, IL).
RESULTS
A convenience sample of 156 participants completed the ED evaluation. Nine patients were not reached for one month follow-up; all nine were less than age 65. Elderly participants (n=15) were similar to non-elderly participants (n=141) with regard to gender, race, education, and household income (Table 1). Elderly participants were more likely to be neither working nor in school (50% vs. 11%). Most patients in each age group had only musculoskeletal pain. Moderate or severe pain at the time of ED evaluation in any body region was common in both elderly (11 of 15, 73%) and non-elderly (106 of 141, 80%) (Table 2). At one month, persistent MVC-related moderate or severe pain in any body region was also common in both elderly participants (9 of 15, 60%) and younger participants (74 of 132, 56%). Rates of persistent post-MVC back and neck pain were also similar for elderly and non-elderly participants.
Table 1.
Baseline characteristics of study participants (n = 156).
| Characteristic | Age ≥65 (n=15) |
Age 18–64 (n=141) |
|---|---|---|
| Age (mean, range) | 73 (65–84) | 38 (18–64) |
| Female Gender (n, %) | 10 (67) | 81 (57) |
| Race (n, %) | ||
| White | 11 (73) | 91 (65) |
| Black | 3 (20) | 19 (13) |
| Other | 0 | 27 (19) |
| Missing | 1 (7) | 4 (3) |
| Education (n, %) | ||
| Less than High School | 2 (13) | 5 (4) |
| High School | 3 (20) | 30 (22) |
| Post-High School | 4 (27) | 61 (43) |
| College | 0 | 33 (23) |
| Post-Graduate Degree | 5 (33) | 11 (8) |
| Missing | 1 (7) | 1 (1) |
| Employment (n, %) | ||
| Work Full Time | 1 (13.6) | 79 (56) |
| Work Part Time | 3 (27.3) | 22 (16) |
| No Work Outside Home | 9 (50) | 15 (11) |
| Student | 0 | 12 (9) |
| Disabled | 2 (9.1) | 10 (7) |
| Missing | 0 | 3 (2) |
| Annual Income (n, %) | ||
| Below $20,000 | 6 (40) | 52 (38) |
| $20,000–$50,000 | 4 (27) | 43 (31) |
| > $50,000 | 5 (33) | 42 (31) |
| Missing | 0 | 4 (3) |
| Marital Status (n, %) | ||
| Married or with partner | 10 (67) | 72 (51) |
| Single | 0 | 45 (32) |
| Divorced | 2 (13) | 18 (13) |
| Separated | 1 (7) | 2 (1) |
| Widowed | 2 (13) | 3 (2) |
| Missing | 0 | 1 (1) |
| Injury Type (n, %) | ||
| Musculoskeletal Strain only | 13 (87) | 119 (84) |
| Fracture | 2 (13) | 10 (7) |
| Laceration | 1 (7) | 12 (9) |
| Highest AIS* Score (n, %) | ||
| AIS Severity 1 | 6 (40) | 95 (67) |
| AIS Severity 2 | 4 (27) | 12 (9) |
| Missing/Unknown | 5 (33) | 34 (24) |
Abbreviated Injury Severity
Table 2.
Presence of moderate/severe pain by age group in the ED and at one month.
| Pain Type | Age ≥65 | Age 18–64 |
|---|---|---|
| ED Pain | n=15 | n=141 |
| Neck, n (%, 95% CI) | 6 (40, 15–65) | 71 (50, 42–58) |
| Back, n (%, 95% CI) | 7 (47, 21–71) | 60 (42, 34–50) |
| Any Region, n(%, 95% CI) | 11 (73, 51–95) | 106 (75, 68–82) |
| One Month Pain | n=15 | n=132 |
| Neck, n (%, 95% CI) | 4 (27, 4–48) | 39 (29, 21–37) |
| Back, n (%, 95% CI) | 5 (33, 9–57) | 45 (34, 26–42) |
| Any Region, n (%, 95% CI) | 9 (60, 35–85) | 74 (56, 48–64) |
Both elderly and younger participants with persistent MVC-related moderate or severe pain in any body region experienced substantial pain interference (Table 3). In the elderly, the highest scores of pain interference were for walking (5.1) and general activity (4.0). Pain interference scores of 10, indicating that pain completely interferes with that item, were reported for at least one of the seven items in 3 of 15 (20%) elderly and 18 of 132 (14%) non-elderly patients.
Table 3.
Pain interference one month following MVC in elderly vs. non-elderly patients with moderate or severe pain vs. mild or no pain in any body region. Values are mean pain interference scores (standard error), which have a scale of 0 to 10.
| Age ≥65 (n=15) | Age 18–64 (n=132) | |||
|---|---|---|---|---|
| Moderate or Severe Pain (n=9) |
Mild or No Pain (n=6) |
Moderate or Severe Pain (n=74) |
Mild or No Pain (n=58) |
|
| General activity | 4.0 (1.4) | 0.3 (0.2) | 5.1 (0.4) | 0.9 (0.2) |
| Mood | 3.8 (1.3) | 0.7 (0.5) | 5.1 (0.4) | 1.0 (0.2) |
| Walking | 5.1 (1.2) | 0.2 (0.2) | 3.6 (0.4) | 0.5 (0.1) |
| Normal Work | 3.5 (1.5) | 0.7 (0.5) | 5.2 (0.5) | 0.7 (0.2) |
| Relationships | 2.4 (1.2) | 0.2 (0.2) | 3.0 (0.4) | 0.4 (0.1) |
| Sleep | 3.6 (1.1) | 0.2 (0.2) | 5.1 (0.4) | 1.1 (0.2) |
| Enjoyment of Life | 3.1 (1.3) | 0.1 (0.2) | 4.6 (0.4) | 0.6 (0.2) |
To put the change in functional status associated with persistent pain in context, we also examined the change in functional status as measured by the SF-36 physical component summary score from the ED visit to one month, in the groups that did and did not continue to have pain (Figure 1). In both the young and old, those that had continued pain had fairly marked decreases in physical function. For elderly patients with persistent pain, the magnitude of the decrease was nearly a standard deviation worsening in functional status (Ware JE 2001).
Figure 1.
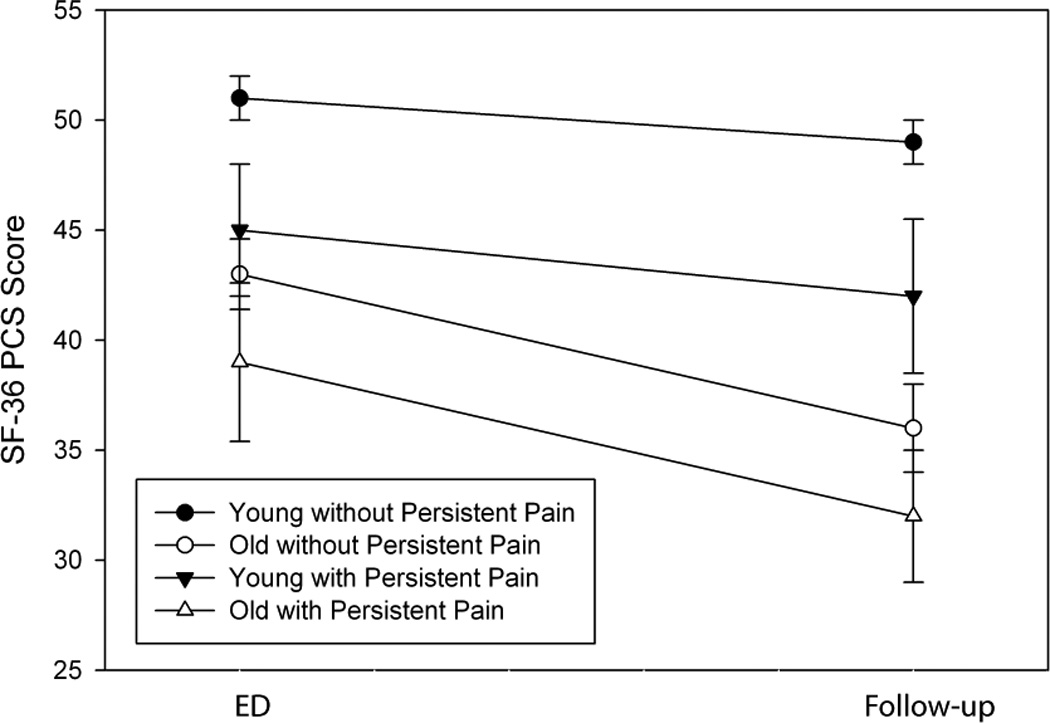
Mean SF 36 Physical Component Summary scores at the time of ED evaluation and at one month follow-up for elderly and non-elderly patients with and without persistent pain. Bars show mean +SEM.
During the month following their ED visit, 67% of elderly participants made physician visits related to the MVC vs. 60% of younger participants (Table 4). For both age groups, this visit was most commonly to a primary care physician. Among participants with moderate or severe pain in any body region at one month, 29% of elderly adults and 41% of younger adults had not seen a primary medical doctor (PMD) in the month following injury (data not shown). Forty seven percent of elderly adults and 32% of younger adults reported additional x-rays, computed tomography scans, or blood work related to the MVC during the month after their ED visit. Rates of physical therapy, chiropractor visits, and alternative medicine visits were low and similar in the two age groups.
Table 4.
Health services utilization by elderly and non-elderly patients following minor injury after MVC.
| Type of Health Care | Age ≥65 (n=15) |
Age 18–64 (n=132) |
|---|---|---|
| Physician visit | 10 (67%) | 79 (60%) |
| Primary Physician visit | 9 (60%) | 60 (45%) |
| Specialist Physician visit | 4 (27%) | 25 (19%) |
| x-rays, CT scans, or blood work | 7 (47%) | 42 (32%) |
| Physical therapy | 2 (13%) | 19 (14%) |
| Chiropractor visit | 1 (7%) | 15 (11%) |
| Alternative medicine* | 0 | 10 (8%) |
Alternative medicine is defined as acupuncture, herbal medicines, or dietary supplements specifically intended to address the pain thought due to injury from the MVC.
DISCUSSION
Persistent pain after minor MVC is recognized as an international public health problem (Freeman, Croft et al. 1999; Holm, Carroll et al. 2008). Despite the projected growth in the number of elderly individuals involved in MVC, no prospective cohort studies of pain outcomes among elderly adults experiencing MVC have been performed. In elderly adults, persistent pain has been associated with functional impairment (Morrison, Magaziner et al. 2003), decreased balance (Poole, Treleaven et al. 2008), falls (Leveille, Jones et al. 2009), and mortality (Zhu, Devine et al. 2007), making efforts to prevent the development of chronic pain in elderly adults a particularly important challenge. Interventional studies to prevent persistent post-operative pain, including a study of opioids in elderly adults (Morrison, Flanagan et al. 2009), support the hypothesis that secondary prevention of persistent post-MVC pain in the elderly is possible. However, prior to the development of interventions to improve outcomes for elderly adults after minor MVC, more information is needed regarding the frequency of and risk factors for persistent pain in this population. The occurrence of functional impairment and posttraumatic stress disorder symptoms, which are present in approximately 20% of non-elderly patients 6 months after MVC (Ursano, Fullerton et al. 1999), should also be examined.
The results of this pilot study suggest that elderly adults who experience MVC develop persistent pain with a similar incidence as younger adults and that both pain interference and a loss of physical function occur frequently in this population. Health services utilization by elderly adults was substantial in the month following the collision, with almost half of elderly adults receiving additional testing. However, in our sample 29% of elderly patients with persistent moderate or severe post-MVC pain did not see a primary medical doctor during the month following injury. If this estimate is representative, then the ED may be the optimal setting for implementing secondary preventive interventions for high risk individuals. The potential importance of developing effective interventions for elderly patients is underscored by our finding that persistent post-MVC pain had a substantial effect on physical function (e.g., general activity and walking). This finding is consistent with the results of studies assessing the burden of chronic pain in elderly community-dwelling adults (Scudds and McD Robertson 1998; Thomas, Peat et al. 2004; Zhu, Devine et al. 2007).
Studies of persistent pain in non-elderly patients after MVC suggest a number of candidate predictor variables for a model of persistent post-MVC pain in the elderly. Candidate predictors would likely include demographic characteristics; ED pain symptoms, in particular axial (i.e. neck and back) pain; acute psychological symptoms such as peritraumatic distress and pain catastrophizing; depression; baseline physical function; social support; and socioeconomic status. The strengths of these predictors might suggest a conceptual framework for the development of persistent pain in the elderly. There is empirical evidence from studies of chronic pain in non-elderly adults to support both the biopsychosocial model (Gatchel, Peng et al. 2007) and the fear avoidance model (Gheldof, Crombez et al.). Assuming 60% of patients would have persistent pain at one month, a study of 150 patients total with 90 patients with the outcome of interest would be needed to support a derivation model with 10 predictor variables.
Limitations
This preliminary study has several limitations which should be considered when reviewing our results. The small sample size leaves us with broad confidence intervals around our estimates of persistent pain and does not allow for assessment of predictors of persistent pain. We defined elderly as age 65 or older. The optimal age cutoff for defining a group of patients at increased risk of adverse outcomes after MVC is not known, and additional analyses looking at alternative age groups may be of value using a larger sample. Emergency physicians probably have a lower threshold for admitting elderly MVC patients than for admitting younger MVC patients. Since we studied only non-admitted patients, this difference in admission criteria may produce an elderly group who are less injured than younger patients. In comparing injury types and highest AIS, we did not see evidence of lower injury rates in elderly patients in our sample, but it may be appropriate to adjust for injury severity in analyses which compare rates of pain and persistent pain across age groups. Nine of the non-elderly patients were lost to follow-up. In a larger study, loss to follow-up of elderly patients, which might result in some cases from a decline in health leading to a change in living situation, may be an important threat to internal validity. Procedures to maximize retention of study subjects during the follow-up will be essential for a successful larger study.
Our study was conducted in a no-fault insurance state. Tort systems have been shown to be associated with increased rates of persistent pain (Cassidy, Carroll et al. 2000), so our results may represent a lower bound on rates of persistent pain. Some study measures reported here, such as the patient’s SF-36 physical component summary score, ask patients to describe their health prior to the collision. It is unknown whether the recent or immediate experience of an MVC would alter a patient’s description of their health in the preceding month. In future studies, the primary purpose of these measures will likely be to identify predictors of adverse outcomes. If the measures serve as reliable and valid predictors of adverse outcomes, the problem of assessing measures following a collision is of secondary importance.
We obtained information on persistent pain one month following the injury. Prior studies of non-elderly adults have shown that post-MVC pain is present at least a year after the date of injury in a substantial portion of individuals, and a longer follow-up period would allow one to better characterize the evolution and burden of persistent pain over time (Barnsley, Lord et al. 1995; Hartling, Brison et al. 2001; Suissa, Harder et al. 2001; Hill, Lewis et al. 2004; Hendriks, Scholten-Peeters et al. 2005). A study with multiple follow-up time points would lend itself to analyses which would examine the trajectories of pain; such analyses can be used to differentiate between patients who recover from those with chronic disability (Sterling, Hendrikz et al.).
CONCLUSION
Our results suggest that rates of persistent pain in elderly adults experiencing minor MVC are similar to rates for younger patients, and that persistent moderate or severe pain results in substantial functional interference in elderly adults. Further studies to define predictors of long term adverse outcomes among elderly individuals experiencing MVC are needed.
Acknowledgments
Support: Funding for this study was provided by NIH 5KL2RR025746-03 (Platts-Mills), NIH K23 KAR050410A (McLean), and institutional resources
REFERENCES
- Association for the Advancement of Automotive Medicine. The Abbreviated Injury Scale-1990 Revision, Update 1998. Des Plaines, Il: 1998. [Google Scholar]
- Andersson GB. Epidemiological features of chronic low-back pain. The Lancet. 1999;354(9178):581–585. doi: 10.1016/S0140-6736(99)01312-4. [DOI] [PubMed] [Google Scholar]
- Barnsley L, Lord SM, et al. The prevalence of chronic cervical zygapophysial joint pain after whiplash. Spine (Phila Pa 1976) 1995;20(1):20–25. doi: 10.1097/00007632-199501000-00004. discussion 26. [DOI] [PubMed] [Google Scholar]
- Bijur PE, Latimer CT, et al. Validation of a verbally administered numerical rating scale of acute pain for use in the emergency department. Academic Emergency Medicine. 2003;10(4):390–392. doi: 10.1111/j.1553-2712.2003.tb01355.x. [DOI] [PubMed] [Google Scholar]
- Cassidy JD, Carroll LJ, et al. Effect of eliminating compensation for pain and suffering on the outcome of insurance claims for whiplash injury. New England Journal of Medicine. 2000;342(16):1179–1186. doi: 10.1056/NEJM200004203421606. [DOI] [PubMed] [Google Scholar]
- Daut RL, Cleeland CS, et al. Development of the Wisconsin brief pain questionnaire to assess pain in cancer and other diseases. Pain. 1983;(17):197–210. doi: 10.1016/0304-3959(83)90143-4. [DOI] [PubMed] [Google Scholar]
- Edwards RR. Age differences in the correlates of physical functioning in patients with chronic pain. Journal of Aging and Health. 2006;18(1):56–69. doi: 10.1177/0898264305280976. [DOI] [PubMed] [Google Scholar]
- Fejer R, Jordan A, et al. Categorising the severity of neck pain: establishment of cut-points for use in clinical and epidemiological research. Pain. 2005;119(1–3):176–182. doi: 10.1016/j.pain.2005.09.033. [DOI] [PubMed] [Google Scholar]
- Freeman MD, Croft AC, et al. A review and methodologic critique of the literature refuting whiplash syndrome. Spine. 1999;24(1):86–96. doi: 10.1097/00007632-199901010-00022. [DOI] [PubMed] [Google Scholar]
- Gatchel RJ, Peng YB, et al. The biopsychosocial approach to chronic pain: scientific advances and future directions. Psychological Bulletin. 2007;133(4):581–624. doi: 10.1037/0033-2909.133.4.581. [DOI] [PubMed] [Google Scholar]
- Gheldof EL, Crombez G, et al. Pain-related fear predicts disability, but not pain severity: a path analytic approach of the fear-avoidance model. European Journal of Pain. 14(8):870 e1–870 e9. doi: 10.1016/j.ejpain.2010.01.003. [DOI] [PubMed] [Google Scholar]
- Harder S, Veilleux M, et al. The effect of socio-demographic and crash-related factors on the prognosis of whiplash. Journal of Clinical Epidemiology. 1998;51(5):377–384. doi: 10.1016/s0895-4356(98)00011-0. [DOI] [PubMed] [Google Scholar]
- Hartling L, Brison RJ, et al. Prognostic value of the Quebec Classification of Whiplash-Associated Disorders. Spine. 2001;26(1):36–41. doi: 10.1097/00007632-200101010-00008. [DOI] [PubMed] [Google Scholar]
- Hendriks EJ, Scholten-Peeters GG, et al. Prognostic factors for poor recovery in acute whiplash patients. Pain. 2005;114(3):408–416. doi: 10.1016/j.pain.2005.01.006. [DOI] [PubMed] [Google Scholar]
- Hill J, Lewis M, et al. Predicting persistent neck pain: a 1-year follow-up of a population cohort. Spine. 2004;29(15):1648–1654. doi: 10.1097/01.brs.0000132307.06321.3c. [DOI] [PubMed] [Google Scholar]
- Hincapie CA, Cassidy JD, et al. Whiplash injury is more than neck pain: a population-based study of pain localization after traffic injury. Journal of Occupational Environmental Medicine. 2010;52(4):434–440. doi: 10.1097/JOM.0b013e3181bb806d. [DOI] [PubMed] [Google Scholar]
- Holm LW, Carroll LJ, et al. The burden and determinants of neck pain in whiplash-associated disorders after traffic collisions: results of the Bone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated Disorders. Spine. 2008;33(4 Suppl):S52–S59. doi: 10.1097/BRS.0b013e3181643ece. [DOI] [PubMed] [Google Scholar]
- Jung BF, Johnson RW, et al. Risk factors for postherpetic neuralgia in patients with herpes zoster. Neurology. 2004;62(9):1545–1551. doi: 10.1212/01.wnl.0000123261.00004.29. [DOI] [PubMed] [Google Scholar]
- Keller S, Bann CM, et al. Validity of the brief pain inventory for use in documenting the outcomes of patients with noncancer pain. Clinical Journal of Pain. 2004;20(5):309–318. doi: 10.1097/00002508-200409000-00005. [DOI] [PubMed] [Google Scholar]
- Kendig H, Browning CJ, et al. Impacts of illness and disability on the well-being of older people. Disability and Rehabilitation. 2000;22(1–2):15–22. doi: 10.1080/096382800297088. [DOI] [PubMed] [Google Scholar]
- Krebs EE, Carey TS, et al. Accuracy of the pain numeric rating scale as a screening test in primary care. Journal of General Internal Medicine. 2007;22(10):1453–1458. doi: 10.1007/s11606-007-0321-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leveille SG, Jones RN, et al. Chronic musculoskeletal pain and the occurrence of falls in an older population. The Journal of the American Medical Association. 2009;302(20):2214–2221. doi: 10.1001/jama.2009.1738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyman S, Ferguson SA, et al. Older driver involvements in police reported crashes and fatal crashes: trends and projections. Injury Prevention. 2002;8(2):116–120. doi: 10.1136/ip.8.2.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCaig LF. National Center for Health Statisitcs. Personal communication. 2009 Nov [Google Scholar]
- Morrison RS, Flanagan S, et al. A novel interdisciplinary analgesic program reduces pain and improves function in older adults after orthopedic surgery. Journal of the American Geriatric Society. 2009;57(1):1–10. doi: 10.1111/j.1532-5415.2008.02063.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrison RS, Magaziner J, et al. The impact of post-operative pain on outcomes following hip fracture. Pain. 2003;103(3):303–311. doi: 10.1016/S0304-3959(02)00458-X. [DOI] [PubMed] [Google Scholar]
- Poole E, Treleaven J, et al. The influence of neck pain on balance and gait parameters in community-dwelling elders. Manual Therapy. 2008;13(4):317–324. doi: 10.1016/j.math.2007.02.002. [DOI] [PubMed] [Google Scholar]
- Rossignol M, Suissa S, et al. Working disability due to occupational back pain: three-year follow-up of 2,300 compensated workers in Quebec. Journal of Occupational Medicine. 1988;30(6):502–505. [PubMed] [Google Scholar]
- Safety A F f T. U.S. safety and mobility crisis looms for aging baby boomers, AAA foundation warns. Senior Safety and Mobility. 2008 Retrieved September 8th, 2009, 2009, from http://www.aaafoundation.org/pdf/LPWorkshopRelease.pdf. [Google Scholar]
- Scudds RJ, Mc DRJ. Empirical evidence of the association between the presence of musculoskeletal pain and physical disability in community-dwelling senior citizens. Pain. 1998;75(2–3):229–235. doi: 10.1016/s0304-3959(97)00224-8. [DOI] [PubMed] [Google Scholar]
- Scudds RJ, McD Robertson J. Empirical evidence of the association between the presence of musculoskeletal pain and physical disability in community-dwelling senior citizens. Pain. 1998;75(2–3):229–235. doi: 10.1016/s0304-3959(97)00224-8. [DOI] [PubMed] [Google Scholar]
- Sterling M, Hendrikz J, et al. Similar factors predict disability and posttraumatic stress disorder trajectories after whiplash injury. Pain. doi: 10.1016/j.pain.2011.01.056. [DOI] [PubMed] [Google Scholar]
- Suissa S, Harder S, et al. The relation between initial symptoms and signs and the prognosis of whiplash. European Spine Journal. 2001;10(1):44–49. doi: 10.1007/s005860000220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas E, Peat G, et al. The prevalence of pain and pain interference in a general population of older adults: cross-sectional findings from the North Staffordshire Osteoarthritis Project (NorStOP) Pain. 2004;110(1–2):361–368. doi: 10.1016/j.pain.2004.04.017. [DOI] [PubMed] [Google Scholar]
- Ursano RJ, Fullerton CS, et al. Acute and chronic posttraumatic stress disorder in motor vehicle accident victims. American Journal of Psychiatry. 1999;156(4):589–595. doi: 10.1176/ajp.156.4.589. [DOI] [PubMed] [Google Scholar]
- Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Medical Care. 1992;30(6):473–483. [PubMed] [Google Scholar]
- Ware JEKM. SF-36 Physical and Mental Health Summary Scales: A Manual for Users of Version 1. Second Edition. Lincoln, RI: QualityMetric Incorporated; 2001. [Google Scholar]
- Ware JEKM, Dewey JE. How to score version two of the SF-36 Health Survey. Lincoln, RI: QualityMetric Incorporated; 2000. [Google Scholar]
- Ware JEKM, Keller SK. SF-36 Physical and Mental Health Summary Scales: A User's Manual. Boston, MA: The Health Institute, New England Medical Center; 1994. [Google Scholar]
- Zhao L, Lucado J, et al. Emergency department visits associated with motor vehicle accidents, 2006. 2010 Retrieved October 15th, 2010, from http://www.hcup-us.ahrq.gov/reports/statbriefs/sb84.jsp.
- Zhu K, Devine A, et al. Association of back pain frequency with mortality, coronary heart events, mobility, and quality of life in elderly women. Spine. 2007;32(18):2012–2018. doi: 10.1097/BRS.0b013e318133fb82. [DOI] [PubMed] [Google Scholar]
- Ziegler D, Rathmann W, et al. Neuropathic pain in diabetes, prediabetes and normal glucose tolerance: the MONICA/KORA Augsburg Surveys S2 and S3. Pain Medicine. 2009;10(2):393–400. doi: 10.1111/j.1526-4637.2008.00555.x. [DOI] [PubMed] [Google Scholar]


