Abstract
Objective
To describe and evaluate a technique to optimize scan centering during the Stratus optical coherence tomography (OCT) image acquisition process using currently available scan tracking coordinates.
Design
Observational clinical study.
Participants
Twelve eyes of six normal subjects were examined using the Fast retinal nerve fiber layer (RNFL) thickness and the Fast Optic Disc acquisition protocols.
Methods
At visit 1, 3 consecutive measurements (trials) were taken by 2 different operators with the scan subjectively centered on the optic disc for the Fast RNFL thickness protocol and Fast Optic Disc protocol. At visit 2, 3 consecutive measurements were taken by positioning the scan using scan tracking coordinates. The scan coordinates were recorded twice by each operator and the limits of agreement and Bland-Altman plots were used to estimate agreement. The within subjects standard deviation (Sw) and the coefficient of variation (CV) were calculated for RNFL and optic disc parameters for each operator separately and differences by scan positioning method were evaluated using a 3-way (trial x operator x visit) analysis of variance for repeated measures.
Results
The Sw and CV for the RNFL thickness parameters were generally higher when the scan was subjectively centered on the disc compared to when using the newly described coordinate system (eg, for operator 2, temporal sector Sw was 1.60 ± 0.78 and 4.09 ± 0.99 and CV was 2.2% and 5.7% with and without coordinate use, respectively). For the Fast RNFL protocol, the use of scan tracking coordinates resulted in significantly less variability than subjective placement of the scan circle using the landmark feature (currently recommended technique) in the temporal sectors only. No significant difference was found for any of the optic disc parameters. Bland-Altman plots showed good agreement within each operator for calculating scan coordinates suggesting this technique is reproducible.
Conclusions
Reproducibility of RNFL thickness measurements generally improves with the use of scan tracking coordinates, particularly in the temporal sector. However, small changes in the position of the scan do not significantly affect the reproducibility of optic disc parameters.
Keywords: imaging, Stratus optical coherence tomography, retinal nerve fiber layer thickness, reproducibility
The Stratus optical coherence tomography (OCT) has the ability to detect glaucomatous structural damage.1–14 The reproducibility of Stratus OCT measurements has been evaluated in normal and glaucomatous eyes,15–17 with measurements in the nasal quadrant reportedly the most variable.15 Variability in the scan position over time could be one possible component16 affecting intervisit reproducibility but this has not been systematically evaluated.
Stratus OCT lacks a scan registration feature to ensure that the scan and subsequent measurements are obtained at the same location during follow-up examinations. Rather, the operator must consistently position the scan during each follow-up visit with the help of a landmark feature. In a recent study, we demonstrated that changes in the position of the scan at follow-up visits may increase the variability of retinal nerve fiber layer (RNFL) thickness measurements. In particular, clock hour measurements and other sectoral measurements may be affected by scan location.18 This variability due to scan positioning could limit the theoretical ability of the Stratus OCT to detect true structural changes over time.19 In clinical practice, an objective method to center the scan on the optic disc could help to ensure consistent placement of the scan circle during follow-up examinations.
The main goal of this study was to describe and evaluate a new method, the use of scan tracking coordinates, to optimize the scan position during the Stratus OCT image acquisition process, and to evaluate the influence of scan position on the reproducibility of optic disc and RNFL thickness measurements.
METHODS
Twelve eyes of six normal subjects (mean age 40.3 ± 7.9 y; 4 females) were evaluated. All participants in this observational clinical study were evaluated at the Hamilton Glaucoma Center, University of California, San Diego (UCSD). Informed consent was obtained from each participant and the UCSD Human Subjects Committee approved all methodology. All methods adhered to the Declaration of Helsinki for research involving human subjects and the Health Insurance Portability and Account-ability Act.
All subjects underwent a complete ophthalmologic examination including review of medical history, slit-lamp biomicroscopy, intraocular pressure (IOP) measurement, dilated stereoscopic fundus examination using a 78-D lens, stereoscopic optic disc photography, and standard automated perimetry using the 24-2 Swedish Interactive Threshold Algorithm (Humphrey visual field analyzer, Carl Zeiss Meditec) as part of the Diagnostic Innovations in Glaucoma Study, a prospective longitudinal study designed to evaluate optic nerve structure and visual function in glaucoma. All eyes had best-corrected visual acuity of 20/40 or better, sphere within ± 5.0 D and cylinder within ± 3.0 D, a normal fundus examination with a healthy appearance of the optic disc and RNFL, open angle at gonioscopy with IOPs of 22 mm Hg or less, no history of increased IOP, and a normal visual field result. A normal visual field was defined as a mean deviation and a pattern standard deviation within the 95% normal confidence limits and Glaucoma Hemifield Test results within normal limits. The horizontal and vertical cup/disc ratios were not a selection criterion for the study population.
Instrumentation
The Stratus OCT obtains cross-sectional images of ocular microstructures.1–17 For this study, the Fast RNFL thickness and the Fast Optic Disc acquisition protocols (Stratus OCT software version 4.0.7; Carl Zeiss Meditec) were used. All recruited subjects had pupil diameters of at least 3 mm in both eyes and OCT images of adequate quality (see below) were obtained without pupil dilation.16,20
Fast RNFL
A total of 3 scans, each composed of 256 A-scans, are acquired consecutively using a circle with a standardized diameter of 3.4 mm. An automated computer algorithm delineates the anterior and posterior margins of the RNFL. The RNFL thickness parameters listed in Table 1 are measured with the Stratus OCT by assessing a total of 768 data points between the anterior and posterior RNFL borders.
TABLE 1.
Between Subjects Mean, Sw ± 1.96SE in Microns and the CV (% in Parenthesis) for the Fast RNFL Parameters for the 2 Operators at Visits 1 and 2
| Operator 1 |
Operator 2 |
|||
|---|---|---|---|---|
| Visit 1 | Visit 2 | Visit 1 | Visit 2 | |
| Average RNFL thickness | 102.8, 1.60 ± 0.50 (1.6) | 103.2, 1.58 ± 0.50 (1.6) | 103, 1.31 ± 0.58 (1.3) | 103.1, 1.17 ± 0.41 (1.1) |
| Superior RNFL thickness | 125.7, 5.68 ± 1.64 (4.5) | 124.4, 4.10 ± 2.13 (3.3) | 123.4, 5.16 ± 1.82 (4.3) | 124, 3.27 ± 0.93 (2.6) |
| Inferior RNFL thickness | 134.1, 4.63 ± 1.54 (3.4) | 132.8, 3.27 ± 0.91 (2.5) | 135.4, 4.02 ± 1.13 (3) | 134.3, 2.89 ± 0.65 (2.1) |
| Nasal RNFL thickness | 81.2, 5.27 ± 1.96 (6.6) | 76.3, 3.91 ± 1.29 (5.1) | 83, 4.77 ± 1.15 (5.9) | 76.7, 3.02 ± 1.01 (3.9) |
| Temporal RNFL thickness* | 73.5, 4.52 ± 1.72 (6.2) | 69.8, 2.41 ± 0.86 (3.5) | 77.6, 4.09 ± 0.99 (5.7) | 71.6, 1.60 ± 0.78 (2.2) |
| RNFL thickness 1-o' clock hour | 111.4, 7.58 ± 2.93 (7.2) | 107.2, 6.03 ± 2.84 (6) | 107.9, 6.91 ± 2.09 (6.5) | 105.5, 5.06 ± 1.65 (4.8) |
| RNFL thickness 2-o' clock hour | 99.2, 9.25 ± 3.66 (9.9) | 92.5, 5.27 ± 2.43 (5.7) | 102.3, 7.16 ± 2.45 (7.3) | 94.4, 4.91 ± 1.26 (5.1) |
| RNFL thickness 3-o' clock hour | 67.2, 6.04 ± 1.89 (9.6) | 62.1, 3.75 ± 1.54 (6) | 69.3, 5.20 ± 0.94 (7.7) | 63.8, 3.42 ± 1.04 (5.5) |
| RNFL thickness 4-o' clock hour | 76.1, 6.13 ± 2.70 (8.1) | 73.9, 4.49 ± 1.18 (6.4) | 76.8, 4.86 ± 1.47 (6.5) | 72, 3.28 ± 1.05 (4.7) |
| RNFL thickness 5-o' clock hour | 107.2, 5.78 ± 2.76 (5.2) | 103.8, 5.29 ± 1.68 (5.3) | 109, 5.75 ± 1.72 (5.1) | 104.1, 3.61 ± 0.91 (3.5) |
| RNFL thickness 6-o' clock hour | 143.3, 8.36 ± 2.60 (5.7) | 140.2, 3.96 ± 1.3 (2.8) | 146.8, 8.38 ± 2.52 (5.6) | 142.2, 5.42 ± 1.56 (3.8) |
| RNFL thickness 7-o' clock hour | 151.8, 7.48 ± 2.14 (5.2) | 154.5, 3.76 ± 1.78 (2.6) | 150, 5.40 ± 2.43 (3.6) | 156.5, 3.26 ± 1.23 (2.1) |
| RNFL thickness 8-o' clock hour* | 77.4, 5.75 ± 1.57 (7.7) | 83.1, 3.72 ± 0.70 (4.7) | 74.8, 5.09 ± 1.53 (6.9) | 84.1, 3.11 ± 1.59 (3.7) |
| RNFL thickness 9-o' clock hour | 55.7, 4.29 ± 1.54 (7.7) | 56.6, 2.48 ± 1.03 (4.4) | 54.4, 2.81 ± 1.06 (5.1) | 57.7, 2.27 ± 0.89 (3.9) |
| RNFL thickness 10-o' clock hour* | 81.1, 6.57 ± 2.53 (8.1) | 79.8, 2.46 ± 1.32 (3.1) | 84.5, 4.74 ± 1.66 (5.6) | 80.7, 2.18 ± 0.87 (2.7) |
| RNFL thickness 11-o' clock hour | 126.8, 6.44 ± 2.74 (5.1) | 136.2, 3.53 ± 1.63 (2.6) | 130.5, 4.69 ± 1.19 (3.6) | 139.1, 3.07 ± 0.70 (2.2) |
| RNFL thickness 12-o' clock hour | 132, 9.34 ± 2.56 (7.1) | 131.1, 6.92 ± 2.55 (5.3) | 126.3, 8.93 ± 3.15 (7.1) | 129.1, 5.01 ± 1.61 (3.9) |
P < 0.05 after ANOVA for repeated measures for Sw for visit 1 vs visit 2.
ANOVA indicates analysis of variance; CV, coefficient of variation; RNFL, retinal nerve fiber layer.
Fast Optic Disc Analysis
Six radial linear scans each of 4 mm in length are positioned over the optic disc. After the scans are acquired, an automated computer algorithm detects the edges of the optic nerve head and places reference points on the basis of the change in reflectivity determined by the termination point of the retinal pigment epithelium (RPE) layer. For each radial scan, a straight line traced between the 2 reference points defines the disc diameter. By using a reference line located 150 μm anterior to the disc line, the optic cup, and the neuroretinal rim are defined for each radial scan and disc parameters for the Fast Optic Disc analysis are automatically provided (Table 2).
TABLE 2.
Between Subjects Mean, Sw ± 1.96SE in Microns and the CV (% in Parenthesis) for the Fast Optic Disc Parameters for the 2 Operators at Visits 1 and 2
| Operator 1 |
Operator 2 |
|||
|---|---|---|---|---|
| Visit 1 | Visit 2 | Visit 1 | Visit 2 | |
| Vertical integrated rim area | 0.35, 0.04 ± 0.02 (10.4) | 0.31, 0.04 ± 0.02 (12.9) | 0.37, 0.05 ± 0.03 (12.9) | 0.33, 0.03 ± 0.02 (10) |
| Horizontal integrated rim width | 1.70, 0.07 ± 0.01 (3.9) | 1.65, 0.08 ± 0.02 (5) | 1.74, 0.09 ± 0.03 (5.3) | 1.69, 0.07 ± 0.02 (3.8) |
| Disc area | 2.41, 0.12 ± 0.03 (5.4) | 2.38, 0.15 ± 0.05 (6.4) | 2.52, 0.17 ± 0.07 (7.3) | 2.41, 0.15 ± 0.05 (6.6) |
| Cup area | 0.87, 0.05 ± 0.01 (7.6) | 0.90, 0.04 ± 0.02 (5.8) | 0.89, 0.07 ± 0.02 (10.2) | 0.88, 0.05 ± 0.02 (6.7) |
| Rim area | 1.54, 0.10 ± 0.03 (6.9) | 1.48, 0.16 ± 0.06 (10.3) | 1.64, 0.18 ± 0.08 (10.7) | 1.53, 0.11 ± 0.05 (7.3) |
| Cup/disc area ratio | 0.34, 0.02 ± 0.01 (6.3) | 0.36, 0.03 ± 0.01 (7.1) | 0.33, 0.03 ± 0.01 (11.3) | 0.34, 0.02 ± 0.01 (5.6) |
| Horizontal cup/disc ratio | 0.64, 0.03 ± 0.01 (4.9) | 0.63, 0.03 ± 0.01 (5.5) | 0.62, 0.04 ± 0.01 (6.3) | 0.62, 0.02 ± 0.01 (3.6) |
| Vertical cup/disc ratio | 0.52, 0.03 ± 0.01 (5.6) | 0.54, 0.02 ± 0.01 (4.5) | 0.51, 0.03 ± 0.01 (7.5) | 0.53, 0.03 ± 0.01 (6) |
No statistically significant differences were found for any of the parameters after ANOVA for repeated measures.
ANOVA indicates analysis of variance; CV, coefficient of variation.
All scans included in this study had signal strength of at least 8. In addition, criteria for determining scan quality as reported in previous studies were followed.15 The fundus image was clear enough for the optic disc and the scan circle to be seen before and during imaging. Color saturation was even and dense throughout all retinal layers with red color visible in the RPE and the RNFL was visible with no missing or blank areas within the scan pattern (ie, no algorithm failure). For the optic nerve head analysis, each radial scan was evaluated for the presence of artifacts such as failure to detect the edges of the RPE or improper identification of retinal boundaries. In the studied subjects, no such events occurred. Subjects were allowed to blink freely but were asked to keep their head in position during each series of 3 scans.
Each subject included in this study was imaged at 2 visits within a 3-month period. Internal fixation was used at all times. At visit 1, each eye was scanned 3 times by 2 different operators using the Fast Optic Disc followed by the Fast RNFL protocol for a total of 12 scans. The same 2 operators tested all subjects. Both operators were UCSD Imaging Data Evaluation and Analysis Center certified for taking OCT images and are highly experienced with the use of the Stratus OCT, having performed scans on many glaucoma patients before being involved in this study. Specifically, each operator had been previously trained on properly positioning the scan circle centered on the optic disc using a landmark placed on a branching vessel and was asked to do so for both the Fast RNFL and Fast Optic Disc scans. At visit 1, the operators were unaware of the purpose of the study.
Scan Coordinate System for Optimizing Scan Position
At visit 2, the same protocol was applied to acquire a total of 12 scans but each operator used the scan tracking coordinates (see below) to center the scan.
The Stratus OCT scan tracking coordinate system used for this study is available for viewing on the screen during image acquisition process. Figure 1 illustrates how the coordinates are shown on the screen. The position of the fixation point, landmark, and circle scan visible on the acquisition screen representing the fundus image of the eye is given in x/y coordinates. The x-axis represents horizontal shifts (temporal-nasal) and the y-axis represents vertical shifts (superior-inferior). For each approximately 10-μm shift of the circle scan along the x-y axis, new x-y coordinates are generated and provided on the screen corresponding to x and/or y shifts of 0.01 pixels.
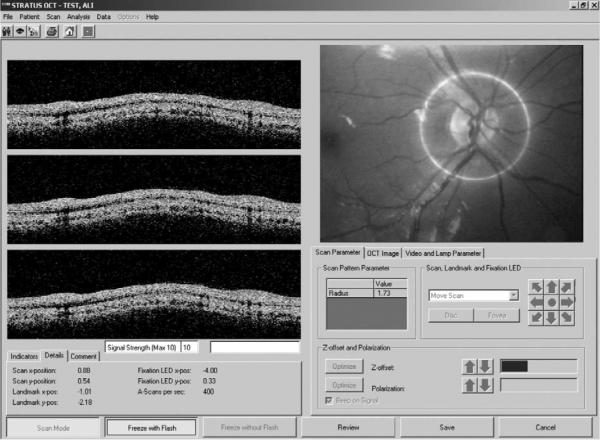
FIGURE 1.
Image capture of the Stratus OCT screen during acquisition process. The x-y coordinates for the scan, the landmark, and the fixation point are shown under the “Details” menu in the bottom left corner of the screen. OCT indicates optical coherence tomography.
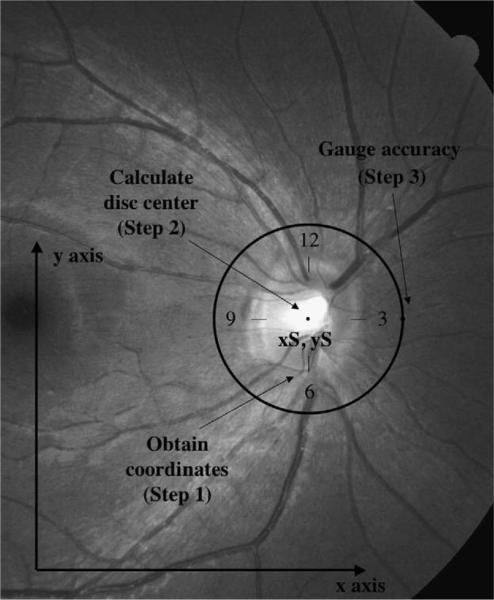
Objectively identifying the center of the disc optimizes the operator's placement of the scan. To calculate the center of the disc, the following steps were followed. First, the landmark was placed at the 12, 3, 6, and 9-o'clock hour positions along the optic disc margin. This provided x/y coordinates for each position (step 1).
Second, the x/y coordinates for each position were averaged, giving the center x/y coordinates, relative to the scan circle (step 2). These relative scan coordinates can be used to define the placement of the scan circle (and of the radial lines) in follow-up images.
For the Fast RNFL protocol, to assess accuracy of the x/y coordinates describing the center of the disc, the process was repeated and the landmark was placed 1.73 mm from the center of the disc (radius of the 3.4-mm scan circle) in the x (horizontal) direction at the 3-o'clock position (step 3). If this calculation is completed correctly, the landmark should lie on the scan circle at 3-o'clock position (Fig. 2). For this study, in the event that the landmark did not overlap the scan circle, the x/y coordinates were recalculated until visual verification of the proper position of the scan circle was obtained.
FIGURE 2.
Schematic representation of the Fast RNFL thickness scan taken around the optic nerve head in OD at visit 2. After obtaining x/y coordinates at 12, 6, 3, and 9 (step 1), the scan tracking coordinates xS, yS are derived from averaging x/y coordinates at the 4 locations (step 2). After repeating the process, the landmark is positioned 1.73mm from the center of the disc in the x direction at 3-o'clock to gauge accuracy (step 3). RNFL indicates retinal nerve fiber layer.
Statistical Analyses
Scan tracking coordinates were recorded twice by each operator for each of the 2 protocols of analysis (Fast Optic Disc and Fast RNFL). The agreement for scan tracking coordinates measurements within each operator was evaluated using Bland-Altman plots and the Spearman rank correlation coefficient.21 To determine the intratest variability of each method, the within subjects standard deviation (Sw) and the coefficient of variation (CV) were calculated for the 2 operators at each visit for all RNFL and optic disc parameters. Sw is defined as the square root of the within-subjects variance (defined as the within-subjects sum of squares divided by its degrees of freedom). For each parameter, a 3-way analysis of variance (ANOVA) (trial x operator x visit) for repeated measures was used to compare RNFL and optic disc measurements performed by the 2 operators at different visits. For post hoc analysis of pairwise comparisons, the Dunn-Sidak method was used.22
In addition, differences in RNFL thickness variability by sectors and optic disc parameters were evaluated in 1-way ANOVA with post hoc analysis to test the hypothesis that the nasal sector had the largest CV as previously suggested.15
The analyses were performed using JMP version 6.1 software (SAS Institute, Cary, NC) and SPSS version 15.0 software. A P value less than 0.05 was considered statistically significant.
RESULTS
Tables 1 and 2 show the between subjects mean, Sw ± 1.96SE and the CV (% in parenthesis) for the Fast RNFL and the Fast Optic Disc parameters, respectively.
In general, RNFL thickness measured in clock hours showed the greatest variability as shown in Table 1. For example, at visit 1, the CV for operator 1 was 9.9% at 2-clock hour whereas it was 1.6% for the average RNFL thickness. Among sectors, the nasal sector had the largest CV, followed by the temporal sector (ANOVA with post hoc analysis: F = 4.24; P<0.05). When comparing the RNFL measurements obtained by the 2 operators, no significant difference was found for any of the parameters.
For both operators, the CVs calculated at visit 2 (when using the coordinate system) were generally lower compared with visit 1 but these differences reached statistical significance for the temporal RNFL sector (F = 5.78; P<0.05) and for the 8 (F = 5.44; P<0.05) and 10 (F = 6.01; P<0.05) clock hours measurements only. These differences between using the scan coordinate system and landmark were confirmed after post hoc analysis using the Dunn-Sidak method.
Among the Fast Optic Disc parameters, the vertical integrated rim area showed the highest CV followed by rim area, although differences in variability across parameters were not significant (Table 2, ANOVA: F = 1.84; P = 0.09). In addition, there was no significant effect of operator or visit on Sw and CV for any of the optic disc parameters. Therefore, for the Fast Optic Disc protocol, the use of scan coordinates did not improve the repeatability of the measurements.
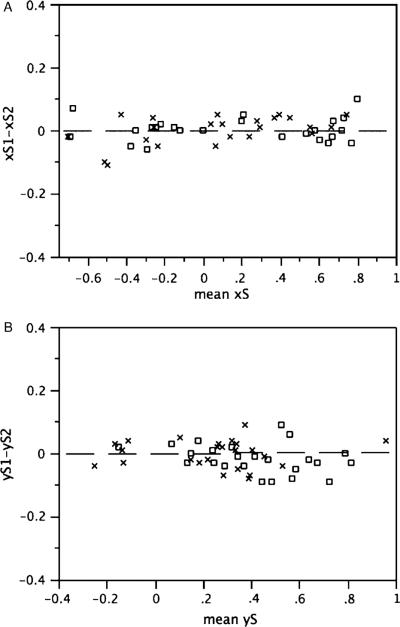
For the x/y scan tracking coordinates, the 95% limits of agreement for x were −0.08 and 0.08 for operator 1 and −0.1 and 0.09 for operator 2, whereas for y they were −0.1 and 0.07 for operator 1 and −0.09 and 0.09 for operator 2 for Fast RNFL and Fast Optic Disc combined. Figures 3A and B show the Bland-Altman plots for the scan tracking coordinates xS and yS for each single operator. In general, good agreement was found in estimating the x-y coordinates within each operator (Spearman rank correlation coefficient rS = 0.25; P = 0.11 for x and rS= −0.20; P = 0.21 for y). For the Fast RNFL thickness protocol, 1 eye required recalculation of coordinates because the landmark was not lying on the scan circle after the first evaluation.
FIGURE 3.
A, Bland-Altman plot of the difference between the first and the second scan tracking coordinates estimate xS1–xS2 versus the mean xS for operator 1 (x) and for operator 2 (□). B, Bland-Altman plot of the difference between the first and the second scan tracking coordinates estimate yS1–yS2 versus the mean yS for operator 1 (x) and for operator 2 (□).
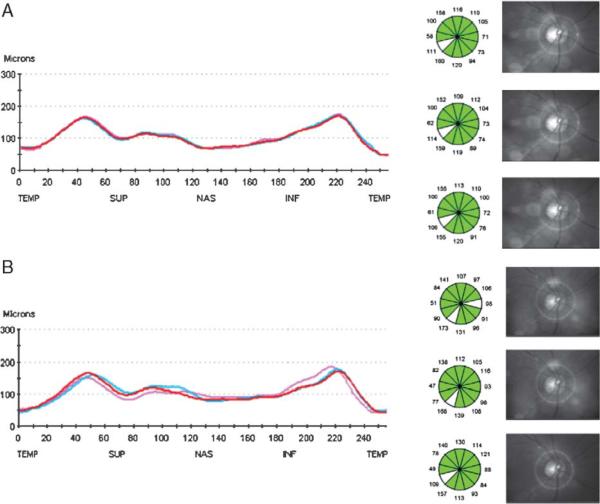
Figures 4A and B show the effect of scan repositioning by the operator at each scan on a serial analysis. Figure 4A shows an example of a series of 3 consecutive Fast RNFL scans with the scan circle held in position using scan tracking coordinates whereas Figure 4B shows a series of 3 consecutive Fast RNFL scans with the scan circle positioned around the optic disc at each single scan by the operator using the landmark feature.
FIGURE 4.
A, Sample eye arbitrarily chosen showing a series of 3 consecutive Fast RNFL scans taken by operator 1 with the scan circle held in position using scan tracking coordinates at visit 2. Note that the scan circle overlaps the landmark point at 3-o'clock indicating accurate measurements. B, Same eye of A showing a series of 3 consecutive Fast RNFL scans with the scan circle subjectively positioned around the optic disc at each scan by operator 1 at visit 1 using the landmark feature. RNFL indicates retinal nerve fiber layer.
DISCUSSION
In the current study, when attempts were made to optimize the position of the circle scan around the optic disc by using scan tracking coordinates, the reproducibility of the RNFL measurements generally improved, although this difference was statistically significant only for the temporal sector and for the 8 and 10-clock hours. However, no improvements in reproducibility were observed for the optic disc parameters.
At the first visit, estimating the center of the disc by calculating its coordinates can provide a more objective way to center the scan around the disc. This is important because scan misalignment can produce significant changes in sectoral RNFL assessment.18 For follow-up examinations, while it is frequently difficult to visualize a vessel branch to use as reference in the live fundus image (particularly when the eye has not been previously dilated), the optic disc margin often contrasts well against the darker background providing a clearer reference. The use of multiple reference points (ie, 12, 3, 6, and 9-clock hours around the disc) and averaging their position to acquire coordinates relative to the center of the disc as opposed to using only one landmark reference, can help reposition the scan circle more consistently on subsequent images.
This study confirms other reports15,18 that the average RNFL thickness is the most reproducible Stratus OCT RNFL parameter and that the nasal and temporal sectors and their corresponding clock hour measurements provide the greatest variability when variability is described as CV. For the thinner nasal and temporal sectors, the Sw was similar in magnitude to the thicker inferior and superior sectors, resulting in an increased CV (eg, for operator 1, at visit 1, nasal and temporal sectors' Sw were 5.27 and 4.52 compared with 4.63 and 5.68 for the inferior and superior sectors). Perhaps the presence of microsaccades occurring during imaging may be the cause of these findings, as it has been shown that shifts along the horizontal axis (temporal-nasal) may produce a greater variance than shifts along the vertical axis (superior-inferior).18 Attempts have been made by other researchers to correct for the presence of eye movements.23
Alternatively, the results may be due to an intrinsic characteristic of the instrument. These findings are clinically important because when evaluating OCT results over time, one may detect higher percentage changes from baseline in the thinner nasal and temporal sectors that may be due to variability in the measurements and not necessarily because of RNFL thinning. Moreover, it is known that nasal and temporal sectors are the least affected in glaucoma, at least in the early stages of the disease.7
For the disc parameters, the results suggest that repositioning of the scan radial lines over the optic disc has little influence on the overall reproducibility of the parameters. This is not surprising because variations in the location of the optic disc along each radial line should not influence the calculation of the disc parameters as long as the anatomic structures are properly identified. Moreover, there is interpolation of data between the 6 radial scans, so that small centering differences may not result in large differences in parameter values. Other factors, such as the ability of the algorithm to place the reference points and the reference line on the basis of the detectable RPE and to calculate the parameters, may play a more important role in terms of measurement variability.
Both operators involved in this study were trained and experienced with imaging using the Stratus OCT, therefore, it is unlikely that operator learning effects contributed to the findings obtained at the second visit. It is possible that less experienced technicians would be less accurate, when manually centering OCT scans in a fast-paced clinical setting. Calculating the center of the disc helped the operators achieve proper scan position around the disc. The calculation was relatively simple and was made before recording each scan. In addition, for the Fast RNFL protocol, the landmark placed on the scan circle was used for visual verification of the accuracy in estimating scan coordinates. This might have helped in achieving better reproducibility during RNFL assessment, as the operator knew during image acquisition that the scan was centered. However, in the absence of dedicated software, the process does increase the time it takes to complete an OCT examination. For this reason, future software modifications by the instrument manufacturer that allow scan coordinates to be more easily accessible would be helpful.
In this study, there was good agreement for estimating both the x and y coordinates within operators. Because the x/y values collected by each operator for a single eye during a session depend on the relative position of the optic nerve head during image acquisition process, differences in the values between operators are not relevant. Scan coordinates are relative to the scan centered on the optic disc so that head movement is not problematic as long as scan coordinates are calculated at each visit.
This is the first study with OCT designed to evaluate operator variability and the variability for repositioning the scan on the optic disc using the manufacturers' suggested method (the landmark feature) compared with a new scan tracking coordinate method. Previous reproducibility studies do not specify how the scan circle was held in place for retest and scan misalignment can influence RNFL measurements, particularly sectoral and clock hours RNFL thickness measurements.15–17 In addition, the fundus image is not recorded during the actual OCT scan acquisition but only after the OCT scan has been obtained; it is possible that the scan visible in the fundus image may not correspond to the actual location of the acquired scan. Because physicians generally do not perform OCT scans themselves, it is important for the operator to follow any method available to minimize the occurrence of scan misplacement.18 This study suggests that operator variability may not be a problem with Stratus OCT as long as a proper method for positioning the scan is employed. Although using scan tracking coordinates resulted in lower Sw and CV, this was statistically significant only in the temporal sector. In addition, the differences in Sw between the 2 methods may not be clinically important per se, but any increment in Sw may contribute to the increased variability found at follow-up visits. Numerous studies have shown that factors such as age,24 media opacity, pupil dilation,16,20 sampling density,25 type of scan,15,16 and signal strength26,27 might also have important effects on the long-term variability of the OCT measurements.
This study has several limitations. First, only healthy eyes were evaluated; previous studies have shown that the variability of the parameters generally increases in glaucomatous eyes.15,16 However, similar benefits of using scan tracking coordinates are expected. Second, because the results show that scan registration has small effects on the intratest reproducibility and because of patient's repositioning at follow-up examinations and other factors (such as proper visualization of the live fundus image at each visit), greater variability due to scan misalignment may occur when eyes are evaluated over a longer time for detecting glaucoma or monitoring its progression. The fact that imaging was conducted on 2 separate visits should have little impact on the within subjects variability of the measurements of visit 1 versus visit 2.
In conclusion, temporal RNFL thickness measurement variability significantly decreased when the position of the scan was optimized with the use of tracking coordinates. However, the position of the radial scans over the optic disc during optic disc imaging had little effect on the reproducibility of disc parameters. Scan position, determined by each operator during a single examination, may represent another source of variability of which clinicians should be aware when interpreting RNFL results from the Stratus OCT. Scan location at first visit and scan repositioning at follow-ups might be better achieved by including calculation of the center of the disc in the live fundus image.
Acknowledgments
Supported in part by NEI EY11008.
Footnotes
Disclosure: Gianmarco Vizzeri, none; Christopher Bowd, none; Felipe A. Medeiros, Carl Zeiss (F,R), Heidelberg Engineering (R); Linda M. Zangwill, Heidelberg Engineering (F), Carl Zeiss (F); Robert N. Weinreb, Heidelberg Engineering (F), Carl Zeiss (C).
REFERENCES
- 1.Huang D, Swanson EA, Lin CP, et al. Optical coherence tomography. Science. 1991;254:1178–1181. doi: 10.1126/science.1957169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schuman JS, Hee MR, Puliafito CA, et al. Quantification of nerve fiber layer thickness in normal and glaucomatous eyes using optical coherence tomography. Arch Ophthalmol. 1995;113:586–596. doi: 10.1001/archopht.1995.01100050054031. [DOI] [PubMed] [Google Scholar]
- 3.Bagga H, Greenfield DS. Quantitative assessment of structural damage in eyes with localized visual field abnormalities. Am J Ophthalmol. 2004;137:797–805. doi: 10.1016/j.ajo.2003.11.060. [DOI] [PubMed] [Google Scholar]
- 4.Budenz DL, Michael A, Chang RT, et al. Sensitivity and specificity of the Stratus OCT for perimetric glaucoma. Ophthalmology. 2005;112:3–9. doi: 10.1016/j.ophtha.2004.06.039. [DOI] [PubMed] [Google Scholar]
- 5.Medeiros FA, Zangwill LM, Bowd C, et al. Evaluation of retinal nerve fiber layer, optic nerve head, and macular thickness measurements for glaucoma detection using optical coherence tomography. Am J Ophthalmol. 2005;139:44–55. doi: 10.1016/j.ajo.2004.08.069. [DOI] [PubMed] [Google Scholar]
- 6.Brusini P, Salvetat ML, Zeppieri M, et al. Comparison between GDx VCC scanning laser polarimetry and Stratus OCT optical coherence tomography in the diagnosis of chronic glaucoma. Acta Ophthalmol Scand. 2006;84:650–655. doi: 10.1111/j.1600-0420.2006.00747.x. [DOI] [PubMed] [Google Scholar]
- 7.Sihota R, Sony P, Gupta V, et al. Diagnostic capability of optical coherence tomography in evaluating the degree of glaucomatous retinal nerve fiber damage. Invest Ophthalmol Vis Sci. 2006;47:2006–2010. doi: 10.1167/iovs.05-1102. [DOI] [PubMed] [Google Scholar]
- 8.Cheng HY, Huang ML. Discrimination between normal and glaucomatous eyes using Stratus optical coherence tomography in Taiwan Chinese subjects. Graefes Arch Clin Exp Ophthalmol. 2005;243:894–902. doi: 10.1007/s00417-005-1140-y. [DOI] [PubMed] [Google Scholar]
- 9.Medeiros FA, Zangwill LM, Bowd C, et al. Comparison of the GDx VCC scanning laser polarimeter, HRT II confocal scanning laser ophthalmoscope, and stratus OCT optical coherence tomograph for the detection of glaucoma. Arch Ophthalmol. 2004;122:827–837. doi: 10.1001/archopht.122.6.827. [DOI] [PubMed] [Google Scholar]
- 10.Jeoung JW, Park KH, Kim TW, et al. Diagnostic ability of optical coherence tomography with a normative database to detect localized retinal nerve fiber layer defects. Ophthalmology. 2005;112:2157–2163. doi: 10.1016/j.ophtha.2005.07.012. [DOI] [PubMed] [Google Scholar]
- 11.Bowd C, Zangwill LM, Medeiros FA, et al. Structure-function relationships using confocal scanning laser ophthalmoscopy, optical coherence tomography, and scanning laser polarimetry. Invest Ophthalmol Vis Sci. 2006;47:2889–2895. doi: 10.1167/iovs.05-1489. [DOI] [PubMed] [Google Scholar]
- 12.Hoffmann EM, Medeiros FA, Sample PA, et al. Relationship between patterns of visual field loss and retinal nerve fiber layer thickness measurements. Am J Ophthalmol. 2006;141:463–471. doi: 10.1016/j.ajo.2005.10.017. [DOI] [PubMed] [Google Scholar]
- 13.Racette L, Boden C, Kleinhandler SL, et al. Differences in visual function and optic nerve structure between healthy eyes of blacks and whites. Arch Ophthalmol. 2005;123:1547–1553. doi: 10.1001/archopht.123.11.1547. [DOI] [PubMed] [Google Scholar]
- 14.Shah NN, Bowd C, Medeiros FA, et al. Combining structural and functional testing for detection of glaucoma. Ophthalmology. 2006;113:1593–1602. doi: 10.1016/j.ophtha.2006.06.004. [DOI] [PubMed] [Google Scholar]
- 15.Budenz DL, Chang RT, Huang X, et al. Reproducibility of retinal nerve fiber thickness measurements using the Stratus OCT in normal and glaucomatous eyes. Invest Ophthalmol Vis Sci. 2005;46:2440–2443. doi: 10.1167/iovs.04-1174. [DOI] [PubMed] [Google Scholar]
- 16.Paunesco LA, Schuman JS, Price LL, et al. Reproducibility of nerve fiber layer thickness, macular thickness, and optic nerve head measurements using Stratus OCT. Invest Ophthalmol Vis Sci. 2004;45:1716–1724. doi: 10.1167/iovs.03-0514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Carpineto P, Ciancaglini M, Aharrh-Gnama A, et al. Custom measurement of retinal nerve fiber layer thickness using Stratus OCT in normal eyes. Eur J Ophthalmol. 2005;15:360–366. doi: 10.1177/112067210501500308. [DOI] [PubMed] [Google Scholar]
- 18.Vizzeri G, Bowd C, Medeiros FA, et al. Effect of improper circle alignment around the optic nerve head on retinal nerve fiber layer thickness measurements using stratus OCT. J Glaucoma. 2008 doi: 10.1097/IJG.0b013e31815c3aeb. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zangwill LM, Bowd C. Retinal nerve fiber layer analysis in the diagnosis of glaucoma. Curr Opin Ophthalmol. 2006;17:120–131. doi: 10.1097/01.icu.0000193079.55240.18. [DOI] [PubMed] [Google Scholar]
- 20.Savini G, Zanini M, Barboni P. Influence of pupil size and cataract on retinal nerve fiber layer thickness measurements by Stratus OCT. J Glaucoma. 2006;15:336–340. doi: 10.1097/01.ijg.0000212244.64584.c2. [DOI] [PubMed] [Google Scholar]
- 21.Bland JM, Altman DG. Measuring agreement in method comparison studies. Stat Methods Med Res. 1999;8:135–160. doi: 10.1177/096228029900800204. [DOI] [PubMed] [Google Scholar]
- 22.Ludbrook J. On making multiple comparisons in clinical and experimental pharmacology and physiology. Clin Exp Pharmacol Physiol. 1991;18:379–392. doi: 10.1111/j.1440-1681.1991.tb01468.x. [DOI] [PubMed] [Google Scholar]
- 23.Hammer DX, Ferguson RD, Magill JC, et al. Active retinal tracker for clinical optical coherence tomography systems. J Biomed Opt. 2005;10:024038. doi: 10.1117/1.1896967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Parikh RS, Parikh SR, Sekhar GC, et al. Normal age related decay of retinal nerve fiber layer thickness. Ophthalmology. 2007;114:921–926. doi: 10.1016/j.ophtha.2007.01.023. [DOI] [PubMed] [Google Scholar]
- 25.Gursen-Ozden R, Ishikawa H, Hoh ST, et al. Increasing sampling density improves reproducibility of optical coherence tomography measurements. J Glaucoma. 1999;8:238–241. [PubMed] [Google Scholar]
- 26.Sadda SR, Wu Z, Walsh AC, et al. Errors in retinal thickness measurements obtained by optical coherence tomography. Ophthalmology. 2006;113:285–293. doi: 10.1016/j.ophtha.2005.10.005. [DOI] [PubMed] [Google Scholar]
- 27.Wu Z, Vazeen M, Varma R, et al. Factors associated with variability in retinal nerve fiber layer thickness measurements obtained by Optical Coherence Tomography. Ophthalmology. 2007;114:1505–1512. doi: 10.1016/j.ophtha.2006.10.061. [DOI] [PubMed] [Google Scholar]