Abstract
Supratentorial hemangioblastoma is a rare form of hemangioblastoma; little information is available regarding prognosis, treatment, and clinical characteristics, because the available literature is primarily composed of case reports and small case series. Therefore, we performed a systematic review of the literature to analyze clinical characteristics, disease progression, and surgical outcomes with respect to survival for supratentorial hemangioblastomas. The rate of progression-free survival (PFS) was determined using Kaplan-Meier analysis. Differences in categorical factors, including location of tumor and diagnosis of von Hippel-Lindau (VHL) disease, were analyzed using the Pearson χ2 test. A total of 106 articles met the search criteria, which combined for a total of 132 patients. Of the patients with supratentorial tumors, 60% had VHL disease, and 31 (84%) of 37 patients with tumors in the sellar/suprasellar region had associated VHL (χ2, P < .001). Five-year PFS for gross-total resection and subtotal resection were 100% and 53%, respectively (Log rank, P < .01). On the basis of our analysis of the literature on published cases of supratentorial hemangioblastoma, gross-total resection appears to be superior to other treatment modalities in extending PFS. Von Hippel–Lindau disease is positively correlated with supratentorial hemangioblastoma when compared with non-supratentorial CNS hemangioblastomas, particularly when present in the sellar/suprasellar region.
Keywords: hemangioblastoma, supratentorial, von Hippel-Lindau
Hemangioblastomas are uncommon tumors of the central nervous system (CNS) that were first described by von Hippel in 1895.1 They are benign, vascular tumors of uncertain origin principally composed of stromal and endothelial cell components and comprise 1.1%–2.4% of all intracranial space-occupying lesions.2–4 Hemangioblastomas typically occur in the cerebellum, brainstem, and spinal cord and are often associated with von Hippel-Lindau (VHL) disease.5,6 Approximately one-third of hemangioblastomas are associated with VHL, whereas remaining cases occur sporadically.5,7–9
Supratentorial hemangioblastomas are exceedingly rare. Because of the rarity of hemangioblastomas in this location, the literature is primarily composed of case reports and small series. Little information is available regarding the clinical features of these tumors, particularly in comparison with lesions found in other locations. No consensus is currently available regarding appropriate management approaches for supratentorial hemangioblastomas or whether supratentorial hemangioblastoma is part of the stigmata of VHL.
To supplement the current understanding of the clinical significance and management of supratentorial hemangioblastoma, we systematically reviewed the published literature to determine what is known about the presentation and clinical course in patients with this disease. Where possible, we performed statistical analysis to determine the efficacy of various treatment approaches using the existing body of published patient data.
Materials and Methods
Article Selection
A comprehensive systematic review of the English-language literature was performed. Articles were identified via PubMed search using the key words “hemangioblastoma” and “haemangioblastoma” alone and in combination with the key words “capillary” and “supratentorial.” All references of these articles were then searched to extract data on patients who underwent surgery for supratentorial hemangioblastoma. A total of 1052 articles was identified, of which 106 had patient data regarding supratentorial hemangioblastomas.
All references that contained individual patient data or purely supratentorial aggregated data sets of either histologically confirmed tumors or tumors presenting in the context of confirmed diagnosis of VHL disease were included in our analysis. Patients with tumors unrelated to hemangioblastoma or VHL disease were excluded from all analyses.
Data Extraction
Data from individual and aggregated case series were extracted from each article. The median largest tumor dimension and median tumor volume were not reportable or analyzable in our analysis, because studies did not consistently report either value. Patients were considered to have VHL disease if the study reported that they met clinical diagnostic criteria or genetic testing requirements. A clinical diagnosis was made if patients met either of the following 2 criteria: (1) a family history of VHL disease in conjunction with a CNS hemangioblastoma, pheochromocytoma, or clear cell renal carcinoma or (2) ≥2 CNS hemangioblastomas or 1 CNS hemangioblastoma and a visceral tumor, excluding epididymal and renal cysts.10
Statistical Analysis
Pearson' χ2 test was used to analyze differences in preoperative categorical factors. Fisher's exact test was used if there were <five values per cell. Kaplan-Meier analysis was used to generate time to progression curves. Differences in time to progression were analyzed using the log-rank test. Analyses were performed using the statistical software package PASW Statistics 18 (IBM).
Results
Clinical Characteristics
The literature search yielded a total of 106 references2,4,6,11–112 meeting the inclusion criteria, containing data on 132 patients with supratentorial hemangioblastomas (Table 1). There was a slight male preponderance (53%), and the median age was 35 years. The most common presenting symptom was headache (39%), followed by visual changes (28%) and paresis (21%). Most patients with supratentorial hemangioblastoma reported in the literature (60%) received a diagnosis of VHL disease.
Table 1.
Patient, tumor, and treatment characteristics
| Characteristic | n/total (%) |
|---|---|
| Sex | |
| Male | 69/129 (53) |
| Female | 60/129 (47) |
| Median age in years (range) | 35 (0.1–85) |
| Symptom | |
| Headache | 48/122 (39) |
| Nausea | 34/122 (28) |
| Visual | 26/122 (21) |
| Gait | 22/122 (18) |
| Mental status | 22/122 (18) |
| Seizures | 22/122 (18) |
| Abnormal Gait | 15/122 (12) |
| Cystic | 35/105 (33) |
| Solid | 67/105 (67) |
| VHL disease | 59/99 (35) |
| Solitary tumor | 88/125 (70) |
| Surgery | |
| Biopsy | 3/79 (4) |
| Subtotal | 15/79 (19) |
| Gross total | 61/79 (77) |
| Radiation therapy | |
| Yes | 11/133 (8) |
| No | 116/133 (87) |
| Radiosurgery/Gamma knife | 6/133 (5) |
Of the 131 patients with available tumor location data, 147 supratentorial tumors were identified (Table 2). Eighty-five tumors (58%) were found in the cerebrum, 38 (26%) were found in the sellar/suprasellar region, 15 (10%) were intraventricular, and 9 (6%) were in other locations. One-third of the tumors (33%) were found to be cystic, whereas the majority were solid (67%).
Table 2.
Tumor locations
| Location | n/total (%) |
|---|---|
| Cerebral | 85/147 (58) |
| Sellar/suprasellar | 38/147 (26) |
| Intraventricular | 15/147 (10) |
| All other locations | 9/147 (6) |
Of the 79 patients with data describing extent of resection, 3 (4%) underwent a biopsy procedure, 15 (19%) underwent subtotal resection (STR), and 61 (77%) underwent gross-total resection (GTR). Five percent of patients underwent postsurgical treatment with fractionated radiotherapy. Follow-up ranged from 0 to 276 months in these studies.
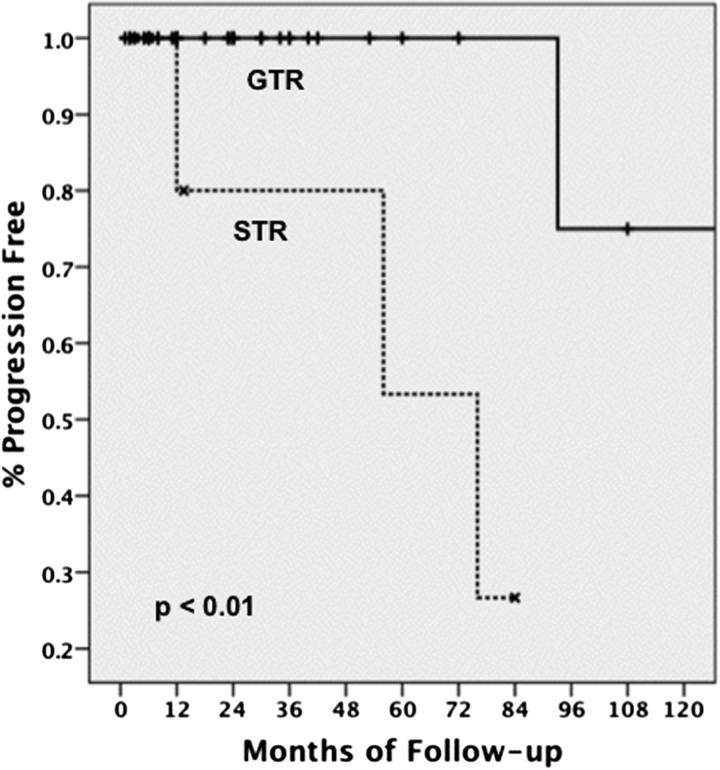
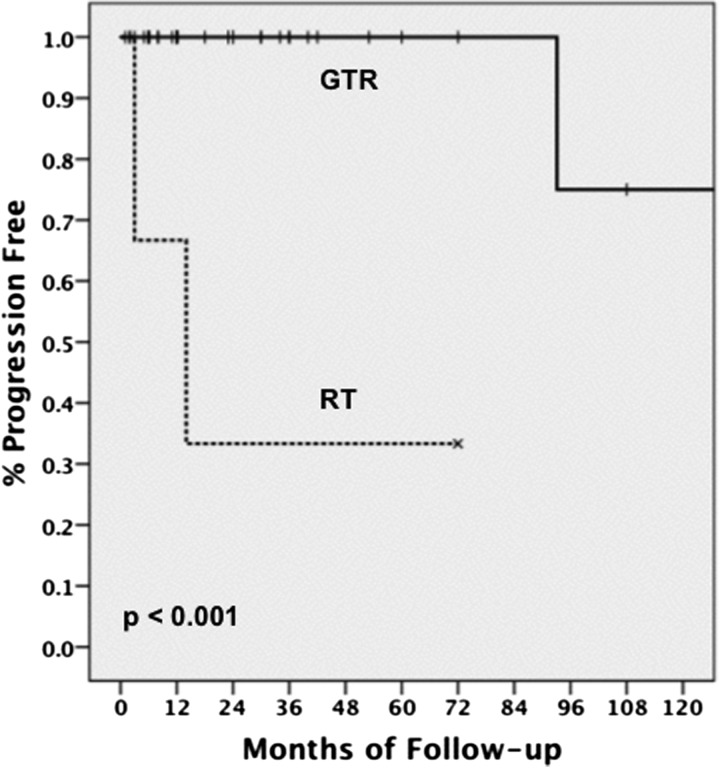
GTR Provides Optimal Progression-Free Survival
Of the 79 cases that reported extent of resection, 61 (77%) achieved GTR. Of the 15 tumors that had STR, only 2 (13%) were in noneloquent locations and 1 (7%) in an unknown location. All other tumors were in eloquent or hazardous locations (Table 3). Analysis suggested that patients undergoing GTR experienced a significant improvement in progression-free survival (PFS), compared with those receiving STR (5-year PFS: GTR 100% vs STR 53%; log rank, P < .01) (Fig. 1). Further analysis suggested that patients undergoing GTR experienced a significant improvement in PFS, compared with those receiving fractionated radiotherapy (RT) alone (5-year PFS: GTR 100% vs RT 33%; log rank, P < .001) (Fig. 2). All patients receiving fractionated RT as the only treatment modality had presumed hemangioblastoma based on diagnosis of VHL disease.
Table 3.
Location of subtotally resected tumors
| Location | n/total (%) |
|---|---|
| Sub-total resection | |
| Eloquent cerebral | 5/15 (33) |
| Non-eloquent cerebral | 2/15 (13) |
| Suprasellar | 3/15 (20) |
| Intrasellar | 2/15 (13) |
| Intraventricular | 2/15 (13) |
| Unknown | 1/15 (7) |
Fig. 1.
Rate of progression-free survival among patients with gross-total resection (GTR) and subtotal resection (STR) of tumors.
Fig. 2.
Rate of progression-free survival among patients with gross-total resection (GTR) and radiation therapy (RT) of tumors.
Because of limitations of the available data on survival, survival analysis provided no significant results for specific treatment modalities. Overall 5-year survival was 88%, with all 8 total deaths occurring within the first 2 years after diagnosis.
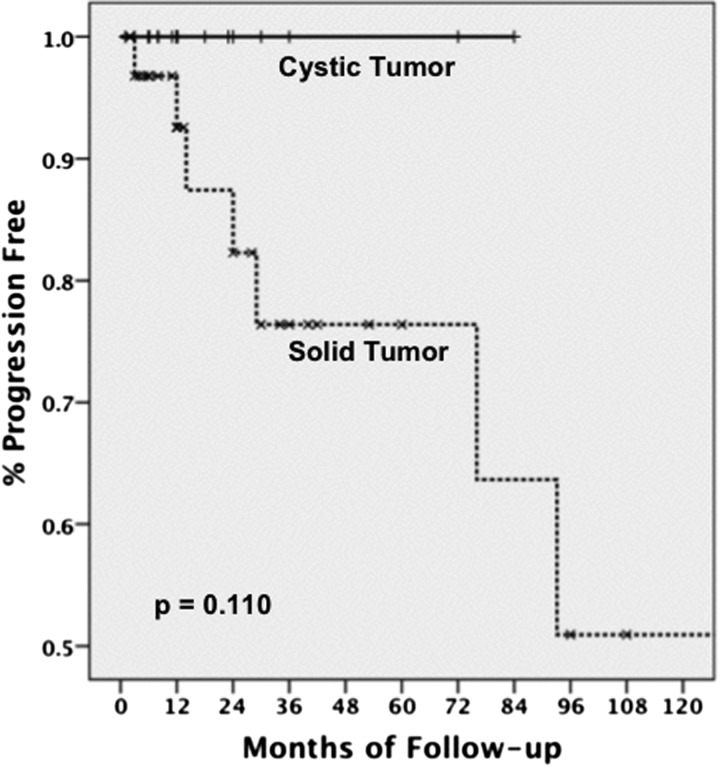
Solid Tumors Are Associated with Earlier Recurrence
Of the 105 cases that reported tumor composition, 35 tumors (33%) were reported to have a cystic component. There was a trend toward significance in the association between presence of cysts and PFS; patients with cystic tumors were less likely to present with progression than were those with solid tumors (5-year PFS: cystic 100% vs solid 76%; Log rank, P = .110) (Fig. 3). Analysis revealed no significance in the association between cystic tumors and extent of resection (χ2, P = .973).
Fig. 3.
Rate of progression-free survival among patients with cystic tumors and solid tumors.
Suprasellar Hemangioblastomas Are Associated with VHL Disease
To determine whether location was an indicator of VHL disease, we compared tumor location with VHL status. A significant association was found between tumors found in the sellar/suprasellar location and diagnosis of VHL disease (χ2, P < .001). When stratified by age, sex, and cystic composition, the association remained significant. No other significant association was found between tumor location and VHL disease.
Discussion
CNS hemangioblastomas, especially multiple hemangioblastomas, are the most common manifestation of VHL disease. Approximately 80% of all patients with VHL develop CNS hemangioblastomas.10 Although most VHL-associated hemangioblastomas are found in the cerebellum, brainstem, or spinal cord,113–115 supratentorial hemangioblastomas are rare,6,8,67,115 with little information in the literature to guide management. Our principle goal was to identify features of these tumors that would not be immediately obvious by reading isolated case reports.
Supratentorial hemangioblastomas are rare and have been reported to comprise only 1%–6% of all hemangioblastomas associated with VHL disease.8,10,116 Peyre et al. screened 409 patients with VHL disease in the French-speaking VHL Study Group database from 1981 through 2008 and only found 13 patients (3.2%) harboring 18 supratentorial tumors, where 4 patients had multiple tumors.8 Six (33.3%) of 18 patients presented with symptoms, with the main symptom being increased intracranial pressure. Of more importance, among 14 tumors with documented serial imaging, 13 tumors showed growth, suggesting that these tumors show high propensity for growth.8 By comparison, a large series reported by Wanebo et al. consisting of 373 hemangioblastomas located primarily in the cerebellum, brainstem, and spinal cord (nonsupratentorial locations) reported only 44% tumor growth.115 Thus, a higher percentage of supratentorial hemangioblastomas (92.9%) seems to grow during follow-up, compared with infratentorial and spinal cord hemangioblastomas (44%), based on the small number of supratentorial hemangioblastomas reported by Peyre et al.8
Hemangioblastoma is currently considered to be a grade I meningeal neoplasm of uncertain origin according to the latest World Health Organization classification of CNS tumors.117 Despite its benign histology, hemangioblastomas can cause symptoms because of mass effect on the surrounding structures by tumor growth, cyst formation/growth, and peritumoral edema. Thus, surgery has been the mainstay treatment for CNS hemangioblastomas with good outcomes. In series by Jagannathan et al., 98% of patients with VHL disease who underwent resection of cerebellar hemangioblastomas had improved or stabilized symptoms 3 months after surgery.5 Consistent with this finding, our analysis of the available data suggests that GTR alone provides excellent tumor control rates, particularly if the tumor lacks a cystic component. Solid tumors seem to have a higher rate of recurrence. Because of insufficient data, we were unable to statistically analyze the efficacy of STR plus adjuvant RT in extending PFS, especially when GTR cannot be achieved safely.
In our analysis of PFS for fractionated RT as the sole treatment modality for supratentorial hemangioblastomas, RT was found to be inferior to GTR. Reported rates of 5-year PFS for fractionated RT for all CNS hemangioblastomas (combined primary treatment modality and adjuvant therapy) range from 33% to 90.5%.118–120 Evidence suggests that high-dose RT provides greater PFS; Smalley et al. reported 57% 5-year PFS for patients receiving ≥50 Gy external beam RT, compared with 33% for patients receiving <50 Gy, whereas Sung et al. reported 90.5% 5-year PFS for patients receiving 40–55 Gy, compared with 54.5% for those receiving 20–36 Gy.
Although not enough data were available to analyze the effectiveness of stereotactic radiosurgery on supratentorial hemangioblastomas, reported rates of 5-year PFS for all CNS hemangioblastomas for both VHL and sporadic cases ranges from 63% to 85%.118,121–125 Evidence suggests that GTR should be the primary goal for the treatment of supratentorial hemangioblastomas; however, in cases in which lesions occur in eloquent, inoperable locations or only STR can be achieved, stereotactic radiosurgery or high-dose adjuvant RT should be considered as alternate treatment modalities.
Among all patients with CNS hemangioblastomas, 33%–38% concurrently receive a diagnosis of VHL disease.5,7–9 Patients with VHL tend to form CNS hemangioblastomas at a younger age, have multiple tumors, and develop new tumors throughout their lifetime, compared with those with sporadic hemangioblastomas.7,75 One study by Conway et al. reported that 53% of patients with VHL harbor multiple hemangioblastomas and have more prevalent spinal hemangioblastomas.7 Moreover, 67% of VHL patients developed new CNS hemangioblastomas during the follow-up at a rate of new tumor every 2.1 years.7 Surgical outcomes were similarly favorable in both groups, with a low complication rate of 15%, which was similar for the VHL-associated supratentorial hemangioblastomas.8 Because patients with VHL are at a high risk for new tumor formation and surgery provides good outcomes at a relatively low risk, a close follow-up with serial imaging is recommended in patients with VHL with CNS hemangioblastomas. Moreover, hemangioblastomas in patients with VHL have high propensity for tumor growth (92.9%),8 compared with sporadic cases (44%).115 Thus, those patients with supratentorial hemangioblastomas should be followed up closely, because our results indicate high incidence of VHL disease in patients harboring tumors at this location.
Asymptomatic lesions should be carefully followed up with a low threshold for surgical resection with development of new symptoms given low risks involved with surgery.7,8 For example, Peyre et al. reported postoperative focal neurological deficits in 15% of patients after supratentorial hemangioblastoma resection, all of which ultimately improved.8 Although the primary objective of surgery is to resect the symptomatic tumor, other lesions can be considered for resection if they are easily accessible with the same approach. In one study by Jagannathan et al., a total of 164 cerebellar hemangioblastomas were resected during 126 operations, in which 136 tumors were symptomatic (83%) and 28 tumors were asymptomatic (17%) tumors that were easily accessible during the same surgery.5 Because of the high propensity for tumor growth for VHL-associated hemangioblastomas,8 careful preoperative planning should be conducted, especially in patients with VHL with multiple tumors.
In our study, we found that the rate of occurrence of VHL disease is significantly greater in patients with supratentorial hemangioblastoma, with 60% of patients receiving a diagnosis of VHL disease. Tumors located in the sellar/suprasellar region are even more likely to be associated with VHL disease, with 84% of patients with tumors in this location having associated VHL disease. Considering the high rate of occurrence of VHL disease in association with hemangioblastomas in the sellar/suprasellar region, we suggest that sellar/suprasellar hemangioblastomas be considered part of the stigmata of VHL disease, and the clinical suspicion of VHL disease should be raised in patients with supratentorial hemangioblastomas in the sellar/suprasellar region.
Study Limitations
As a retrospective study, this review is limited by the data available and may reflect source study biases. The diverse range of available data limits the number of variables that can be analyzed and controlled. Variables of possible interest, such as tumor volume and histological variants, were reported inconsistently and could not be analyzed.
Conclusion
In conclusion, we report patient, tumor, and treatment characteristics for previously published cases of supratentorial hemangioblastomas. GTR appears to be superior, compared with other treatment modalities, in extending PFS. VHL disease is positively correlated with supratentorial hemangioblastoma, compared with nonsupratentorial CNS hemangioblastomas, particularly when present in the sellar/suprasellar region. Because of the relative rarity of this tumor, this study aims to accurately describe outcome and tumor location characteristics using a data set that would be difficult to accumulate at a single center treating this tumor.
Funding
This work was supported by the National Institutes of Health (National Research Service Award to F32NS073326-01 to M.O., F32NS066719-01 to M.S.), the Doris Duke Charitable Foundation (to M.R.), and the Reza and Georgianna Khatib Endowed Chair in Skull Base Tumor Surgery (A.T.P.).
Acknowledgments
Conflict of interest statement. None declared.
References
- 1.Toyoda H, Seki M, Nakamura H, Inoue Y, Yamano Y, Takaoka K. Intradural extramedullary hemangioblastoma differentiated by MR images in the cervical spine: a case report and review of the literature. J Spinal Disord Tech. 2004;17(4):343–347. doi: 10.1097/01.bsd.0000083630.91606.af. doi:10.1097/01.bsd.0000083630.91606.af. [DOI] [PubMed] [Google Scholar]
- 2.Acikalin MF, Oner U, Tel N, Pasaoglu O, Altinel F. Supratentorial hemangioblastoma: a case report and review of the literature. Arch Pathol Lab Med. 2003;127(9):e382–e384. doi: 10.5858/2003-127-e382-SHACRA. [DOI] [PubMed] [Google Scholar]
- 3.Hussein MR. Central nervous system capillary haemangioblastoma: the pathologist's viewpoint. Int J Exp Pathol. 2007;88(5):311–324. doi: 10.1111/j.1365-2613.2007.00535.x. doi:10.1111/j.1365-2613.2007.00535.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wasenko JJ, Rodziewicz GS. Suprasellar hemangioblastoma in Von Hippel-Lindau disease: a case report. Clin Imaging. 2003;27(1):18–22. doi: 10.1016/s0899-7071(02)00537-5. doi:10.1016/S0899-7071(02)00537-5. [DOI] [PubMed] [Google Scholar]
- 5.Jagannathan J, Lonser RR, Smith R, DeVroom HL, Oldfield EH. Surgical management of cerebellar hemangioblastomas in patients with von Hippel-Lindau disease. J Neurosurg. 2008;108(2):210–222. doi: 10.3171/JNS/2008/108/2/0210. doi:10.3171/JNS/2008/108/2/0210. [DOI] [PubMed] [Google Scholar]
- 6.Lonser RR, Butman JA, Kiringoda R, Song D, Oldfield EH. Pituitary stalk hemangioblastomas in von Hippel-Lindau disease. J Neurosurg. 2009;110(2):350–353. doi: 10.3171/2008.4.17532. doi:10.3171/2008.4.17532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Conway JE, Chou D, Clatterbuck RE, Brem H, Long DM, Rigamonti D. Hemangioblastomas of the central nervous system in von Hippel-Lindau syndrome and sporadic disease. Neurosurgery. 2001;48(1):55–62. doi: 10.1097/00006123-200101000-00009. discussion -3. [DOI] [PubMed] [Google Scholar]
- 8.Peyre M, David P, Van Effenterre R, et al. Natural history of supratentorial hemangioblastomas in von Hippel-Lindau disease. Neurosurgery. 2010;67(3):577–587. doi: 10.1227/01.NEU.0000374846.86409.A7. discussion 87 doi:10.1227/01.NEU.0000374846.86409.A7. [DOI] [PubMed] [Google Scholar]
- 9.Richard S, Graff J, Lindau J, Resche F. Von Hippel-Lindau disease. Lancet. 2004;363(9416):1231–1234. doi: 10.1016/S0140-6736(04)15957-6. doi:10.1016/S0140-6736(04)15957-6. [DOI] [PubMed] [Google Scholar]
- 10.Lonser RR, Glenn GM, Walther M, et al. von Hippel-Lindau disease. Lancet. 2003;361(9374):2059–2067. doi: 10.1016/S0140-6736(03)13643-4. doi:10.1016/S0140-6736(03)13643-4. [DOI] [PubMed] [Google Scholar]
- 11.Adegbite AB, Rozdilsky B, Varughese G. Supratentorial capillary hemangioblastoma presenting with fatal spontaneous intracerebral hemorrhage. Neurosurgery. 1983;12(3):327–330. doi: 10.1227/00006123-198303000-00015. doi:10.1227/00006123-198303000-00015. [DOI] [PubMed] [Google Scholar]
- 12.Agostinelli C, Roncaroli F, Galassi E, Bernardi B, Acciarri N, Tani G. Leptomeningeal hemangioblastoma. Case illustration. J Neurosurg. 2004;101(suppl 1):122. doi: 10.3171/ped.2004.101.2.0122. [DOI] [PubMed] [Google Scholar]
- 13.Albrechtsen R. Supratentorial haemangioblastoma. Dan Med Bull. 1971;18(4):73–75. [PubMed] [Google Scholar]
- 14.Bachmann K, Markwalder R, Seiler RW. Supratentorial haemangioblastoma. Case report. Acta Neurochir (Wien) 1978;44(3–4):173–177. doi: 10.1007/BF01402059. doi:10.1007/BF01402059. [DOI] [PubMed] [Google Scholar]
- 15.Baggenstos M, Chew E, Butman JA, Oldfield EH, Lonser RR. Progressive peritumoral edema defining the optic fibers and resulting in reversible visual loss. J Neurosurg. 2008;109(2):313–317. doi: 10.3171/JNS/2008/109/8/0313. doi:10.3171/JNS/2008/109/8/0313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Balcer LJ, Galetta SL, Curtis M, Maguire A, Judy K. von Hippel-Lindau disease manifesting as a chiasmal syndrome. Surv Ophthalmol. 1995;39(4):302–306. doi: 10.1016/s0039-6257(05)80107-9. doi:10.1016/S0039-6257(05)80107-9. [DOI] [PubMed] [Google Scholar]
- 17.Black ML, Tien RD, Hesselink JR. Third ventricular hemangioblastoma: MR appearance. AJNR Am J Neuroradiol. 1991;12(3):553. [PMC free article] [PubMed] [Google Scholar]
- 18.Boughey AM, Fletcher NA, Harding AE. Central nervous system haemangioblastoma: a clinical and genetic study of 52 cases. J Neurol Neurosurg Psychiatry. 1990;53(8):644–648. doi: 10.1136/jnnp.53.8.644. doi:10.1136/jnnp.53.8.644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chakraborti PR, Chakrabarti KB, Doughty D, Plowman PN. Stereotactic multiple are radiotherapy. IV–Haemangioblastoma. Br J Neurosurg. 1997;11(2):110–115. doi: 10.1080/02688699746447. doi:10.1080/02688699746447. [DOI] [PubMed] [Google Scholar]
- 20.Cosar M, Hatiboglu MA, Iplikcioglu AC, Ozcan D. Parasagittal leptomeningeal hemangioblastoma–case report. Neurol Med Chir (Tokyo) 2006;46(6):294–297. doi: 10.2176/nmc.46.294. doi:10.2176/nmc.46.294. [DOI] [PubMed] [Google Scholar]
- 21.Courcoutsakis NA, Prassopoulos PK, Patronas NJ. Aggressive leptomeningeal hemangioblastomatosis of the central nervous system in a patient with von Hippel-Lindau disease. AJNR Am J Neuroradiol. 2009;30(4):758–760. doi: 10.3174/ajnr.A1360. doi:10.3174/ajnr.A1360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Crivelli G, Dario A, Cerati M, Dorizzi A. Solid supratentorial haemangioblastoma. Case report. J Neurosurg Sci. 1992;36(3):161–166. [PubMed] [Google Scholar]
- 23.D'Aliberti G, Mancuso P, Chiaramonte I, Giuffrida S, Lombardo M, Tropea R. Supratentorial haemangioblastomas. Report of two cases. Acta Neurol (Napoli) 1986;8(6):639–647. [PubMed] [Google Scholar]
- 24.Dan NG, Smith DE. Pituitary hemangioblastoma in a patient with von Hippel-Lindau disease. Case report. J Neurosurg. 1975;42(2):232–235. doi: 10.3171/jns.1975.42.2.0232. doi:10.3171/jns.1975.42.2.0232. [DOI] [PubMed] [Google Scholar]
- 25.Deck JH, Rubinstein LJ. Glial fibrillary acidic protein in stromal cells of some capillary hemangioblastomas: significance and possible implications of an immunoperoxidase study. Acta Neuropathol. 1981;54(3):173–181. doi: 10.1007/BF00687739. doi:10.1007/BF00687739. [DOI] [PubMed] [Google Scholar]
- 26.Di Lorenzo N, Spallone A, Morselli E. Cerebral and cerebellar haemangioblastoma occurring in the same patient. Ital J Neurol Sci. 1983;4(1):99–102. doi: 10.1007/BF02043446. doi:10.1007/BF02043446. [DOI] [PubMed] [Google Scholar]
- 27.Diehl PR, Symon L. Supratentorial intraventricular hemangioblastoma: case report and review of literature. Surg Neurol. 1981;15(6):435–443. doi: 10.1016/s0090-3019(81)80033-x. doi:10.1016/S0090-3019(81)80033-X. [DOI] [PubMed] [Google Scholar]
- 28.Elster AD, Arthur DW. Intracranial hemangioblastomas: CT and MR findings. J Comput Assist Tomogr. 1988;12(5):736–739. doi:10.1097/00004728-198809010-00003. [PubMed] [Google Scholar]
- 29.Ferrante L, Acqui M, Mastronardi L, Fortuna A. Supratentorial hemangioblastoma. Report of a case and review of the literature. Zentralbl Neurochir. 1988;49(3):151–161. [PubMed] [Google Scholar]
- 30.Ferrante L, Celli P, Fraioli B. Supratentorial haemangioblastomas in children. Case report. Acta Neurochir (Wien) 1982;62(3–4):241–246. doi: 10.1007/BF01403629. doi:10.1007/BF01403629. [DOI] [PubMed] [Google Scholar]
- 31.Fomekong E, Hernalsteen D, Godfraind C, D'Haens J, Raftopoulos C. Pituitary stalk hemangioblastoma: the fourth case report and review of the literature. Clin Neurol Neurosurg. 2007;109(3):292–298. doi: 10.1016/j.clineuro.2006.11.007. doi:10.1016/j.clineuro.2006.11.007. [DOI] [PubMed] [Google Scholar]
- 32.Fu Y, Ward J, Young HF. Unusual, rod-shaped cytoplasmic inclusions (Hirano bodies) in a cerebellar hemangioblastoma. Acta Neuropathol. 1975;31(2):129–135. doi: 10.1007/BF00688147. doi:10.1007/BF00688147. [DOI] [PubMed] [Google Scholar]
- 33.Ginzburg BM, Montanera WJ, Tyndel FJ, et al. Diagnosis of von Hippel-Lindau disease in a patient with blindness resulting from bilateral optic nerve hemangioblastomas. AJR Am J Roentgenol. 1992;159(2):403–405. doi: 10.2214/ajr.159.2.1632366. [DOI] [PubMed] [Google Scholar]
- 34.Goto T, Nishi T, Kunitoku N, et al. Suprasellar hemangioblastoma in a patient with von Hippel-Lindau disease confirmed by germline mutation study: case report and review of the literature. Surg Neurol. 2001;56(1):22–26. doi: 10.1016/s0090-3019(01)00482-7. doi:10.1016/S0090-3019(01)00482-7. [DOI] [PubMed] [Google Scholar]
- 35.Grisoli F, Gambarelli D, Raybaud C, Guibout M, Leclercq T. Suprasellar hemangioblastoma. Surg Neurol. 1984;22(3):257–262. doi: 10.1016/0090-3019(84)90010-7. doi:10.1016/0090-3019(84)90010-7. [DOI] [PubMed] [Google Scholar]
- 36.Hande AM, Nagpal RD. Cerebellar haemangioblastoma with extensive dissemination. Br J Neurosurg. 1996;10(5):507–511. doi: 10.1080/02688699647186. doi:10.1080/02688699647186. [DOI] [PubMed] [Google Scholar]
- 37.Hankey GJ, Davies L, Gubbay SS. Long term survival with early childhood intracerebral tumours. J Neurol Neurosurg Psychiatry. 1989;52(6):778–781. doi: 10.1136/jnnp.52.6.778. doi:10.1136/jnnp.52.6.778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ho YS, Plets C, Goffin J, Dom R. Hemangioblastoma of the lateral ventricle. Surg Neurol. 1990;33(6):407–412. doi: 10.1016/0090-3019(90)90154-h. doi:10.1016/0090-3019(90)90154-H. [DOI] [PubMed] [Google Scholar]
- 39.Hoang MP, Amirkhan RH. Inhibin alpha distinguishes hemangioblastoma from clear cell renal cell carcinoma. Am J Surg Pathol. 2003;27(8):1152–1156. doi: 10.1097/00000478-200308000-00014. doi:10.1097/00000478-200308000-00014. [DOI] [PubMed] [Google Scholar]
- 40.Hoff JT, Ray BS. Cerebral hemangioblastoma occurring in a patient with von Hippel-Lindau disease. Case report. J Neurosurg. 1968;28(4):365–368. doi: 10.3171/jns.1968.28.4.0365. doi:10.3171/jns.1968.28.4.0365. [DOI] [PubMed] [Google Scholar]
- 41.Ikeda M, Asada M, Yamashita H, Ishikawa A, Tamaki N. [A case of suprasellar hemangioblastoma with thoracic meningioma] No Shinkei Geka. 2001;29(7):679–683. [PubMed] [Google Scholar]
- 42.Iplikcioglu AC, Yaradanakul V, Trakya U. Supratentorial haemangioblastoma: appearances on MR imaging. Br J Neurosurg. 1997;11(6):576–578. doi: 10.1080/02688699745772. doi:10.1080/02688699745772. [DOI] [PubMed] [Google Scholar]
- 43.Isaka T, Horibe K, Nakatani S, Maruno M, Yoshimine T. Hemangioblastoma of the third ventricle. Neurosurg Rev. 1999;22(2–3):140–144. doi: 10.1007/s101430050050. [DOI] [PubMed] [Google Scholar]
- 44.Ishwar S, Taniguchi RM, Vogel FS. Multiple supratentorial hemangioblastomas. Case study and ultrastructural characteristics. J Neurosurg. 1971;35(4):396–405. doi: 10.3171/jns.1971.35.4.0396. doi:10.3171/jns.1971.35.4.0396. [DOI] [PubMed] [Google Scholar]
- 45.Isolan GR, Krayenbuhl N, Mahmoud M, Al-Mefty O. A hemangioblastoma in the pineal region: case report. Neurosurgery. 2007;61(2):E423. doi: 10.1227/01.NEU.0000255516.12085.BB. discussion E doi:10.1227/01.NEU.0000255516.12085.BB. [DOI] [PubMed] [Google Scholar]
- 46.Jang H. Supratentorial leptomeningeal hemangioblastoma: case report. Yeungnam University J of Med. [Case Report] 2007;24(suppl 2):S770–S774. [Google Scholar]
- 47.Jeffreys RV. Supratentorial haemangioblastoma. Acta Neurochirurgica. 1974;31(1–2):55–65. doi:10.1007/BF01432781. [Google Scholar]
- 48.Johnson MD, Mitchell AR, Troup EC, et al. Congenital cystic hemangioblastomas of the cerebral hemisphere in a neonate without alteration in the VHL gene. Pediatr Neurosurg. 2004;40(3):124–127. doi: 10.1159/000079854. doi:10.1159/000079854. [DOI] [PubMed] [Google Scholar]
- 49.Jung SM, Kuo TT. Immunoreactivity of CD10 and inhibin alpha in differentiating hemangioblastoma of central nervous system from metastatic clear cell renal cell carcinoma. Mod Pathol. 2005;18(6):788–794. doi: 10.1038/modpathol.3800351. doi:10.1038/modpathol.3800351. [DOI] [PubMed] [Google Scholar]
- 50.Jyotsna VP, Singh SK, Chaturvedi R, et al. Cranial irradiation–an unusual cause for diabetes insipidus. J Assoc Physicians India. 2000;48(11):1107–1108. [PubMed] [Google Scholar]
- 51.Kachhara R, Nair S, Radhakrishnan VV. Sellar-sphenoid sinus hemangioblastoma: case report. Surg Neurol. 1998;50(5):461–463. doi: 10.1016/s0090-3019(97)00197-3. discussion 3–4 doi:10.1016/S0090-3019(97)00197-3. [DOI] [PubMed] [Google Scholar]
- 52.Karabagli H, Karabagli P, Alpman A, Durmaz B. Congenital supratentorial cystic hemangioblastoma. Case report and review of the literature. J Neurosurg. 2007;107(suppl 6):515–518. doi: 10.3171/PED-07/12/515. [DOI] [PubMed] [Google Scholar]
- 53.Katayama Y, Tsubokawa T, Miyagi A, Goto T, Miyagami M, Suzuki K. Solitary hemangioblastoma within the third ventricle. Surg Neurol. 1987;27(2):157–162. doi: 10.1016/0090-3019(87)90288-6. doi:10.1016/0090-3019(87)90288-6. [DOI] [PubMed] [Google Scholar]
- 54.Keith J, Ang LC, Megyesi J. Cytodiagnosis of supratentorial hemangioblastoma. Acta Cytol. 2008;52(2):260–263. doi: 10.1159/000325496. doi:10.1159/000325496. [DOI] [PubMed] [Google Scholar]
- 55.Kepes JJ, Rengachary SS, Lee SH. Astrocytes in hemangioblastomas of the central nervous system and their relationship to stromal cells. Acta Neuropathol. 1979;47(2):99–104. doi: 10.1007/BF00717031. doi:10.1007/BF00717031. [DOI] [PubMed] [Google Scholar]
- 56.Kerr DJ, Scheithauer BW, Miller GM, Ebersold MJ, McPhee TJ. Hemangioblastoma of the optic nerve: case report. Neurosurgery. 1995;36(3):573–580. doi: 10.1227/00006123-199503000-00017. discussion 80–81 doi:10.1227/00006123-199503000-00017. [DOI] [PubMed] [Google Scholar]
- 57.Kim JM, Cheong JH, Bak KH, Kim CH, Park DW, Oh YH. Congenital supratentorial hemangioblastoma as an unusual cause of simultaneous supra- and infratentorial intracranial hemorrhage: case report. J Neurooncol. 2006;77(1):59–63. doi: 10.1007/s11060-005-9002-3. doi:10.1007/s11060-005-9002-3. [DOI] [PubMed] [Google Scholar]
- 58.Kouri JG, Chen MY, Watson JC, Oldfield EH. Resection of suprasellar tumors by using a modified transsphenoidal approach. Report of four cases. J Neurosurg. 2000;92(6):1028–1035. doi: 10.3171/jns.2000.92.6.1028. doi:10.3171/jns.2000.92.6.1028. [DOI] [PubMed] [Google Scholar]
- 59.Lee KR, Kishore PR, Wulfsberg E, Kepes JJ. Supratentorial leptomeningeal hemangioblastoma. Neurology. 1978;28(7):727–730. doi: 10.1212/wnl.28.7.727. [DOI] [PubMed] [Google Scholar]
- 60.Leibner IW. Brain tumors in infancy; a report of seven cases. Pediatrics. 1948;1(3):346–363. [PubMed] [Google Scholar]
- 61.Leung SY, Chan AS, Wong MP, Yuen ST, Fan YW, Chung LP. Expression of vascular endothelial growth factor in von Hippel-Lindau syndrome-associated papillary cystadenoma of the epididymis. Hum Pathol. 1998;29(11):1322–1324. doi: 10.1016/s0046-8177(98)90265-9. doi:10.1016/S0046-8177(98)90265-9. [DOI] [PubMed] [Google Scholar]
- 62.Liang L, Korogi Y, Sugahara T, et al. Dynamic MR imaging of neurohypophyseal germ cell tumors for differential diagnosis of infundibular diseases. Acta Radiol. 2000;41(6):562–566. doi: 10.1080/028418500127345901. doi:10.1080/028418500127345901. [DOI] [PubMed] [Google Scholar]
- 63.Lindvall P, Brannstrom T. Spontaneous regression of two putative supratentorial haemangioblastomas in one patient. Acta Neurochir (Wien) 2008;150(1):73–76. doi: 10.1007/s00701-007-1453-1. discussion 6 doi:10.1007/s00701-007-1453-1. [DOI] [PubMed] [Google Scholar]
- 64.Loftus CM, Marquardt MD, Stein BM. Hemangioblastoma of the third ventricle. Neurosurgery. 1984;15(1):67–72. doi: 10.1227/00006123-198407000-00012. doi:10.1227/00006123-198407000-00012. [DOI] [PubMed] [Google Scholar]
- 65.Maiuri F. Cysts with mural tumor nodules in the cerebral hemispheres. Neurosurgery. 1988;22(4):703–706. doi: 10.1227/00006123-198804000-00014. doi:10.1227/00006123-198804000-00014. [DOI] [PubMed] [Google Scholar]
- 66.McDonnell DE, Pollock P. Cerebral cystic hemangioblastoma. Surg Neurol. 1978;10(3):195–199. [PubMed] [Google Scholar]
- 67.Meyerle CB, Dahr SS, Wetjen NM, et al. Clinical course of retrobulbar hemangioblastomas in von Hippel-Lindau disease. Ophthalmology. 2008;115(8):1382–1389. doi: 10.1016/j.ophtha.2008.01.027. doi:10.1016/j.ophtha.2008.01.027. [DOI] [PubMed] [Google Scholar]
- 68.Miller MH, Tucker WS, Bilbao JM. Supratentorial hemangioblastoma associated with Von Hippel Lindau disease: case report and review of the literature. Can Assoc Radiol J. 1986;37(1):35–37. [PubMed] [Google Scholar]
- 69.Miyagami M, Katayama Y. Long-term prognosis of hemangioblastomas of the central nervous system: clinical and immunohistochemical study in relation to recurrence. Brain Tumor Pathol. 2004;21(2):75–82. doi: 10.1007/BF02484514. doi:10.1007/BF02484514. [DOI] [PubMed] [Google Scholar]
- 70.Miyata S, Mikami T, Minamida Y, Akiyama Y, Houkin K. Suprasellar hemangioblastoma. J Neuroophthalmol. 2008;28(4):325–326. doi: 10.1097/WNO.0b013e318183c633. doi:10.1097/WNO.0b013e318183c633. [DOI] [PubMed] [Google Scholar]
- 71.Mizuno J, Iwata K, Takei Y. Immunohistochemical study of hemangioblastoma with special reference to its cytogenesis. Neurol Med Chir (Tokyo) 1993;33(7):420–424. doi: 10.2176/nmc.33.420. doi:10.2176/nmc.33.420. [DOI] [PubMed] [Google Scholar]
- 72.Morello G, Bianchi M. Cerebral Hemangioblastomas: Review of Literature and Report of Two Personal Cases. J Neurosurg. 1963;20:254–264. doi: 10.3171/jns.1963.20.3.0254. doi:10.3171/jns.1963.20.3.0254. [DOI] [PubMed] [Google Scholar]
- 73.Moss JM, Choi CY, Adler JR, Jr, Soltys SG, Gibbs IC, Chang SD. Stereotactic radiosurgical treatment of cranial and spinal hemangioblastomas. Neurosurgery. 2009;65(1):79–85. doi: 10.1227/01.NEU.0000348015.51685.D2. discussion doi:10.1227/01.NEU.0000348015.51685.D2. [DOI] [PubMed] [Google Scholar]
- 74.Murali R, Jones WI, Ma Wyatt J. A 57-year-old man with a dural-based parietal lobe tumor. Brain Pathol. 2007;17(4):460–463. doi: 10.1111/j.1750-3639.2007.00091_1.x. 74 doi:10.1111/j.1750-3639.2007.00091_1.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Neumann HP, Eggert HR, Weigel K, Friedburg H, Wiestler OD, Schollmeyer P. Hemangioblastomas of the central nervous system. A 10-year study with special reference to von Hippel-Lindau syndrome. J Neurosurg. 1989;70(1):24–30. doi: 10.3171/jns.1989.70.1.0024. doi:10.3171/jns.1989.70.1.0024. [DOI] [PubMed] [Google Scholar]
- 76.Niemela M, Lim YJ, Soderman M, Jaaskelainen J, Lindquist C. Gamma knife radiosurgery in 11 hemangioblastomas. J Neurosurg. 1996;85(4):591–596. doi: 10.3171/jns.1996.85.4.0591. doi:10.3171/jns.1996.85.4.0591. [DOI] [PubMed] [Google Scholar]
- 77.O'Reilly GV, Rumbaugh CL, Bowens M, Kido DK, Naheedy MH. Supratentorial haemangioblastoma: the diagnostic roles of computed tomography and angiography. Clin Radiol. 1981;32(4):389–392. doi: 10.1016/s0009-9260(81)80276-0. doi:10.1016/S0009-9260(81)80276-0. [DOI] [PubMed] [Google Scholar]
- 78.Ohata K, Takami T, Tsuyuguchi N, Hara M, Haque M. Hemangioblastoma of hippocampus without von Hippel-Lindau disease: case report and review of literature. Neurol India. 2006;54(1):89–90. doi: 10.4103/0028-3886.24718. doi:10.4103/0028-3886.24718. [DOI] [PubMed] [Google Scholar]
- 79.Orakcioglu B, Sakowitz OW, Perren A, Heppner FL, Yonekawa Y. An unusual case of a highly progressive supratentorial capillary haemangioblastoma - histopathological considerations. Acta Neurochir (Wien) 2007;149(4):419–423. doi: 10.1007/s00701-006-1100-2. doi:10.1007/s00701-006-1100-2. [DOI] [PubMed] [Google Scholar]
- 80.Ozveren MF, Topsakal C, Erol FS, Kaplan M, Uchida K, Tanik C. Tentorial vascularization in solid hemangioblastoma–case report. Neurol Med Chir (Tokyo) 2001;41(4):201–205. doi: 10.2176/nmc.41.201. doi:10.2176/nmc.41.201. [DOI] [PubMed] [Google Scholar]
- 81.Pan L, Wang EM, Wang BJ, et al. Gamma knife radiosurgery for hemangioblastomas. Stereotact Funct Neurosurg. 1998;70(suppl 1):179–186. doi: 10.1159/000056420. doi:10.1159/000056420. [DOI] [PubMed] [Google Scholar]
- 82.Peker S, Kurtkaya-Yapicier O, Sun I, Sav A, Pamir MN. Suprasellar haemangioblastoma. Report of two cases and review of the literature. J Clin Neurosci. 2005;12(1):85–89. doi: 10.1016/j.jocn.2004.02.025. doi:10.1016/j.jocn.2004.02.025. [DOI] [PubMed] [Google Scholar]
- 83.Perks WH, Cross JN, Sivapragasam S, Johnson P. Supratentorial haemangioblastoma with polycythaemia. J Neurol Neurosurg Psychiatry. 1976;39(3):218–220. doi: 10.1136/jnnp.39.3.218. doi:10.1136/jnnp.39.3.218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Peyre M, Di Rocco F, Varlet P, et al. Supratentorial hemangioblastoma in the neonatal period. Pediatr Neurosurg. 2009;45(2):155–156. doi: 10.1159/000209656. doi:10.1159/000209656. [DOI] [PubMed] [Google Scholar]
- 85.Pinto JA, Pereira JR, Guimaraes A, Veiga-Pires JA. The value of CT-scanning in supratentorial haemangioblastomas. Neuroradiology. 1987;29(6):573–575. doi: 10.1007/BF00350445. doi:10.1007/BF00350445. [DOI] [PubMed] [Google Scholar]
- 86.Prieto R, Roda JM. Hemangioblastoma of the lateral ventricle: case report and review of the literature. Neurocirugia (Astur) 2005;16(1):58–62. doi: 10.1016/s1130-1473(05)70436-x. [DOI] [PubMed] [Google Scholar]
- 87.Rachinger J, Buslei R, Prell J, Strauss C. Solid haemangioblastomas of the CNS: a review of 17 consecutive cases. Neurosurg Rev. 2009;32(1):37–47. doi: 10.1007/s10143-008-0166-0. discussion -8 doi:10.1007/s10143-008-0166-0. [DOI] [PubMed] [Google Scholar]
- 88.Raila FA, Zimmerman J, Azordegan P, Fratkin J, Parent AD. Successful surgical removal of an asymptomatic optic nerve hemangioblastoma in von Hippel-Lindau disease. J Neuroimaging. 1997;7(1):48–50. doi: 10.1111/jon19977148. [DOI] [PubMed] [Google Scholar]
- 89.Rho YM. Von Hippel-Lindau's disease: a report of five cases. Can Med Assoc J. 1969;101(3):135–142. [PMC free article] [PubMed] [Google Scholar]
- 90.Richmond BK, Schmidt JH., 3rd Congenital cystic supratentorial hemangioblastoma. Case report. J Neurosurg. 1995;82(1):113–115. doi: 10.3171/jns.1995.82.1.0113. doi:10.3171/jns.1995.82.1.0113. [DOI] [PubMed] [Google Scholar]
- 91.Rickert CH, Hasselblatt M, Jeibmann A, Paulus W. Cellular and reticular variants of hemangioblastoma differ in their cytogenetic profiles. Hum Pathol. 2006;37(11):1452–1457. doi: 10.1016/j.humpath.2006.05.004. doi:10.1016/j.humpath.2006.05.004. [DOI] [PubMed] [Google Scholar]
- 92.Rivera E, Chason JL. Cerebral hemangioblastoma. Case report. J Neurosurg. 1966;25(4):452–454. doi: 10.3171/jns.1966.25.4.0452. doi:10.3171/jns.1966.25.4.0452. [DOI] [PubMed] [Google Scholar]
- 93.Roberti F, Jones RV, Wright DC. Cranial nerve hemangioblastomas. Report of a rare case and review of literature. Surg Neurol. 2007;67(6):640–646. doi: 10.1016/j.surneu.2006.08.085. discussion 6 doi:10.1016/j.surneu.2006.08.085. [DOI] [PubMed] [Google Scholar]
- 94.Romero FJ, Rovira M, Ortega A, Ibarra B. Computed tomography in supratentorial hemangioblastoma. Comput Radiol. 1984;8(5):319–323. doi: 10.1016/0730-4862(84)90044-1. doi:10.1016/0730-4862(84)90044-1. [DOI] [PubMed] [Google Scholar]
- 95.Rumboldt Z, Gnjidic Z, Talan-Hranilovic J, Vrkljan M. Intrasellar hemangioblastoma: characteristic prominent vessels on MR imaging. AJR Am J Roentgenol. 2003;180(5):1480–1481. doi: 10.2214/ajr.180.5.1801480. [DOI] [PubMed] [Google Scholar]
- 96.Sajadi A, de Tribolet N. Unusual locations of hemangioblastomas. Case illustration. J Neurosurg. 2002;97(3):727. doi: 10.3171/jns.2002.97.3.0727. doi:10.3171/jns.2002.97.3.0727. [DOI] [PubMed] [Google Scholar]
- 97.Sawin PD, Follett KA, Wen BC, Laws ER., Jr Symptomatic intrasellar hemangioblastoma in a child treated with subtotal resection and adjuvant radiosurgery. Case report. J Neurosurg. 1996;84(6):1046–1050. doi: 10.3171/jns.1996.84.6.1046. doi:10.3171/jns.1996.84.6.1046. [DOI] [PubMed] [Google Scholar]
- 98.Sharma RR, Cast IP, O'Brien C. Supratentorial haemangioblastoma not associated with Von Hippel Lindau complex or polycythaemia: case report and literature review. Br J Neurosurg. 1995;9(1):81–84. doi:10.1080/02688699550041809. [PubMed] [Google Scholar]
- 99.Sherman JH, Le BH, Okonkwo DO, Jane JA. Supratentorial dural-based hemangioblastoma not associated with von Hippel Lindau complex. Acta Neurochir (Wien) 2007;149(9):969–972. doi: 10.1007/s00701-007-1180-7. discussion 72 doi:10.1007/s00701-007-1180-7. [DOI] [PubMed] [Google Scholar]
- 100.Sobottka SB, Frank S, Hampl M, Schackert HK, Schackert G. Multiple intracerebral haemangioblastomas in identical twins with von Hippel-Lindau disease–a clinical and molecular study. Acta Neurochir (Wien) 1998;140(3):281–285. doi: 10.1007/s007010050096. doi:10.1007/s007010050096. [DOI] [PubMed] [Google Scholar]
- 101.Stefani FH, Rothemund E. Intracranial optic nerve angioblastoma. Br J Ophthalmol. 1974;58(9):823–827. doi: 10.1136/bjo.58.9.823. doi:10.1136/bjo.58.9.823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Stein AA, Schilp AO, Whitfield RD. The histogenesis of hemangioblastoma of the brain. A review of twenty-one cases. J Neurosurg. 1960;17:751–761. doi: 10.3171/jns.1960.17.4.0751. doi:10.3171/jns.1960.17.4.0751. [DOI] [PubMed] [Google Scholar]
- 103.Takeuchi H, Hashimoto N, Kitai R, Kubota T. A report of supratentorial leptomeningeal hemangioblastoma and a literature review. Neuropathology. 2008;28(1):98–102. doi: 10.1111/j.1440-1789.2007.00834.x. doi:10.1111/j.1440-1789.2007.00834.x. [DOI] [PubMed] [Google Scholar]
- 104.Tan DS, Evanson J, Plowman PN, Chew SL. Post-radiation inflammatory reaction controlled with thalidomide and rofecoxib. Clin Oncol (R Coll Radiol) 2004;16(8):585–586. doi: 10.1016/j.clon.2004.09.005. doi:10.1016/j.clon.2004.09.005. [DOI] [PubMed] [Google Scholar]
- 105.Tekkok IH, Sav A. Supratentorial cystic hemangioblastoma with infratentorial extension–a unique location and a rare infant case. Childs Nerv Syst. 2006;22(9):1177–1181. doi: 10.1007/s00381-006-0052-4. doi:10.1007/s00381-006-0052-4. [DOI] [PubMed] [Google Scholar]
- 106.Tomaccini D, Cordelli F, Luzi P, Scarfo GB. Supratentorial hemangioblastoma in childhood. Childs Brain. 1980;6(6):313–317. doi: 10.1159/000119919. [DOI] [PubMed] [Google Scholar]
- 107.Tomasello F, Albanese V, Iannotti F, Di Iorio G. Supratentorial hemangioblastoma in a child. Case report. J Neurosurg. 1980;52(4):578–583. doi: 10.3171/jns.1980.52.4.0578. doi:10.3171/jns.1980.52.4.0578. [DOI] [PubMed] [Google Scholar]
- 108.Vuia O. Malignant haemangioblastoma (haemangiosarcoma) of the meninges. Neurochirurgia (Stuttg) 1978;21(5):164–172. doi: 10.1055/s-0028-1090340. [DOI] [PubMed] [Google Scholar]
- 109.Wakai S, Inoh S, Ueda Y, Nagai M. Hemangioblastoma presenting with intraparenchymatous hemorrhage. J Neurosurg. 1984;61(5):956–960. doi: 10.3171/jns.1984.61.5.0956. doi:10.3171/jns.1984.61.5.0956. [DOI] [PubMed] [Google Scholar]
- 110.Wylie IG, Jeffreys RV, Maclaine GN. Cerebral haemangioblastoma. Br J Radiol. 1973;46(546):472–476. doi: 10.1259/0007-1285-46-546-472. doi:10.1259/0007-1285-46-546-472. [DOI] [PubMed] [Google Scholar]
- 111.Yamakawa N, Noda M, Ohyama T, Furuno M, Tsutsumi A, Taki W. A cellular variant of supratentorial hemangioblastoma. Brain Tumor Pathol. 2000;17(1):15–19. doi: 10.1007/BF02478913. doi:10.1007/BF02478913. [DOI] [PubMed] [Google Scholar]
- 112.Zamzuri I, Ghazali MM, Zainuddin N, et al. Molecular genetic analysis of a supratentorial haemangioblastoma in a non-Von Hippel Lindau patient. Med J Malaysia. 2005;60(3):360–363. [PubMed] [Google Scholar]
- 113.Ammerman JM, Lonser RR, Dambrosia J, Butman JA, Oldfield EH. Long-term natural history of hemangioblastomas in patients with von Hippel-Lindau disease: implications for treatment. J Neurosurg. 2006;105(2):248–255. doi: 10.3171/jns.2006.105.2.248. doi:10.3171/jns.2006.105.2.248. [DOI] [PubMed] [Google Scholar]
- 114.Slater A, Moore NR, Huson SM. The natural history of cerebellar hemangioblastomas in von Hippel-Lindau disease. AJNR Am J Neuroradiol. 2003;24(8):1570–1574. [PMC free article] [PubMed] [Google Scholar]
- 115.Wanebo JE, Lonser RR, Glenn GM, Oldfield EH. The natural history of hemangioblastomas of the central nervous system in patients with von Hippel-Lindau disease. J Neurosurg. 2003;98(1):82–94. doi: 10.3171/jns.2003.98.1.0082. doi:10.3171/jns.2003.98.1.0082. [DOI] [PubMed] [Google Scholar]
- 116.Neumann HP, Eggert HR, Scheremet R, et al. Central nervous system lesions in von Hippel-Lindau syndrome. J Neurol Neurosurg Psychiatry. 1992;55(10):898–901. doi: 10.1136/jnnp.55.10.898. doi:10.1136/jnnp.55.10.898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Louis DN, Ohgaki H, Wiestler OD, et al. The 2007 WHO classification of tumours of the central nervous system. Acta Neuropathol. 2007;114(2):97–109. doi: 10.1007/s00401-007-0243-4. doi:10.1007/s00401-007-0243-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Koh ES, Nichol A, Millar BA, Menard C, Pond G, Laperriere NJ. Role of fractionated external beam radiotherapy in hemangioblastoma of the central nervous system. Int J Radiat Oncol Biol Phys. 2007;69(5):1521–1526. doi: 10.1016/j.ijrobp.2007.05.025. doi:10.1016/j.ijrobp.2007.05.025. [DOI] [PubMed] [Google Scholar]
- 119.Smalley SR, Schomberg PJ, Earle JD, Laws ER, Jr, Scheithauer BW, O'Fallon JR. Radiotherapeutic considerations in the treatment of hemangioblastomas of the central nervous system. Int J Radiat Oncol Biol Phys. 1990;18(5):1165–1171. doi: 10.1016/0360-3016(90)90454-r. doi:10.1016/0360-3016(90)90454-R. [DOI] [PubMed] [Google Scholar]
- 120.Sung DI, Chang CH, Harisiadis L. Cerebellar hemangioblastomas. Cancer. 1982;49(3):553–555. doi: 10.1002/1097-0142(19820201)49:3<553::aid-cncr2820490326>3.0.co;2-a. doi:10.1002/1097-0142(19820201)49:3<553::AID-CNCR2820490326>3.0.CO;2-A. [DOI] [PubMed] [Google Scholar]
- 121.Asthagiri AR, Mehta GU, Zach L, et al. Prospective evaluation of radiosurgery for hemangioblastomas in von Hippel-Lindau disease. Neuro Oncol. 2010;12(1):80–86. doi: 10.1093/neuonc/nop018. doi:10.1093/neuonc/nop018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Wang EM, Pan L, Wang BJ, et al. The long-term results of gamma knife radiosurgery for hemangioblastomas of the brain. J Neurosurg. 2005;102(suppl):225–229. doi: 10.3171/jns.2005.102.s_supplement.0225. doi:10.3171/jns.2005.102.s_supplement.0225. [DOI] [PubMed] [Google Scholar]
- 123.Rajaraman C, Rowe JG, Walton L, Malik I, Radatz M, Kemeny AA. Treatment options for von Hippel-Lindau's haemangioblastomatosis: the role of gamma knife stereotactic radiosurgery. Br J Neurosurg. 2004;18(4):338–342. doi: 10.1080/02688690400004944. doi:10.1080/02688690400004944. [DOI] [PubMed] [Google Scholar]
- 124.Jawahar A, Kondziolka D, Garces YI, Flickinger JC, Pollock BE, Lunsford LD. Stereotactic radiosurgery for hemangioblastomas of the brain. Acta Neurochir (Wien) 2000;142(6):641–644. doi: 10.1007/s007010070107. discussion 4–5 doi:10.1007/s007010070107. [DOI] [PubMed] [Google Scholar]
- 125.Patrice SJ, Sneed PK, Flickinger JC, et al. Radiosurgery for hemangioblastoma: results of a multiinstitutional experience. Int J Radiat Oncol Biol Phys. 1996;35(3):493–499. doi: 10.1016/s0360-3016(96)80011-3. doi:10.1016/S0360-3016(96)80011-3. [DOI] [PubMed] [Google Scholar]