Abstract
Objective
To describe the prevalence of acute stress disorder (ASD) symptoms and examine proposed DSM-5 symptom criteria in relation to concurrent functional impairment in children.
Method
From an international archive, datasets were identified which included assessment of acute traumatic stress reactions and concurrent impairment in children age 5 to 17. Data came from 15 studies conducted in the US, UK, Australia, and Switzerland with 1645 children. Dichotomized items were created to indicate the presence or absence of each of the 14 proposed ASD symptoms and functional impairment. The performance of a proposed diagnostic criterion (number of ASD symptoms required) was examined as a predictor of concurrent impairment.
Results
Each ASD symptom was endorsed by 14% to 51% of children; 41% reported clinically-relevant impairment. Children reported from 0 to 13 symptoms (mean = 3.6). Individual ASD symptoms were associated with greater likelihood of functional impairment. The DSM-5 proposed 8-symptom requirement was met by 202 (12.3%) children, and had low sensitivity (.25) in predicting concurrent clinically-relevant impairment. Requiring fewer symptoms (three to four) greatly improved sensitivity while maintaining moderate specificity.
Conclusions
This group of symptoms appears to capture aspects of traumatic stress reactions that can create distress and interfere with children’s ability to function in the acute post-trauma phase. Results provide a benchmark for comparison with adult samples; a smaller proportion of children met the 8-symptom criterion than reported for adults. Symptom requirements for the ASD diagnosis may need to be lowered to optimally identify children whose acute distress warrants clinical attention.
Keywords: acute stress disorder, DSM-5, diagnostic criteria
Introduction
Assessment of acute traumatic stress symptoms in children and adolescents poses both practical and conceptual challenges. On a practical level, children who have recently experienced a potentially traumatic event rarely present for formal mental health services, and thus assessment to discern who is in need of clinical attention may best be accomplished in other settings (health care settings, schools, post-disaster community settings). Empirically sound self-report1 and interview2 measures of child acute traumatic stress are a relatively recent development, and these measures require additional validation in a range of populations. In the aftermath of trauma it can be challenging to distinguish acute distress in children which will resolve (with time and family support) from acute distress which will persist or worsen without clinical attention and intervention. Improving the conceptual basis for assessment and ensuring that diagnosis of acute traumatic stress in children appropriately identifies those in need of assistance are thus key challenges for the field.
The stated goal of the workgroup developing proposed DSM-5 criteria for acute stress disorder (ASD) is to set criteria that will capture a severity of acute stress reactions within the first month that warrants clinical attention.3 The workgroup also aims to set diagnostic criteria that will identify a minority of trauma-exposed persons, arguing that if the majority of those exposed to trauma are diagnosed with ASD, they have not succeeded in identifying those most at need.3 There are two substantivel changes in the proposed conceptualization of the ASD diagnosis. First, it is intended to capture severe early distress without regard to whether these symptoms predict ongoing or persistent traumatic stress, and second, diagnostic status is determined based on an overall ASD symptom picture rather than separate symptom categories. The current proposed diagnostic criteria require that eight of 14 symptoms (of any type: including intrusion symptoms, dissociative symptoms, avoidance symptoms, and arousal symptoms) be present, and that “the disturbance causes clinically significant distress or impairment in social, occupational, or other important areas of functioning.”3 The ASD workgroup proposed that this criterion be tested across datasets. This manuscript follows their recommendation by examining the utility of the proposed criterion in a large combined international dataset of children and adolescents.
One way to distinguish transient acute stress reactions following a traumatic event from severe symptoms that warrant clinical attention is to ascertain the likelihood that a given symptom level is associated with significant impairment. Thus, in the case of children, an optimal ‘cut-off’ for the number of symptoms required for a diagnosis of acute stress disorder would have good sensitivity and specificity with regard to identifying those with concurrent impairment in social, academic, or interpersonal functioning. It is possible that optimal diagnostic criteria for traumatic stress disorders in school-age children and adolescents may differ from those for adults.4–6 Indeed, current proposed symptom criteria for posttraumatic stress disorder (PTSD) in DSM-5 include lower symptom thresholds for children.7 Further, prior studies suggest that children and adolescents might differ from adults with regard to the prevalence of acute traumatic stress symptoms,8–9 or the association of these symptoms with concurrent or persistent impairment.10–11
To understand the full range of children’s potential responses to acute traumatic events and to be able to examine the boundaries between normative responses and diagnostic-level acute stress reactions, it is important to assess both symptoms and functional impairment prospectively (because later retrospective reports may be clouded by concurrent symptom status12) in samples identified based on exposure to an event rather than referral for clinical attention. The purpose of the current analyses was to utilize a newly available data archive of child traumatic stress studies to (a) describe the prevalence of each ASD symptom and the number of ASD symptoms endorsed in school-age and adolescent children assessed prospectively within one month of exposure to acute trauma, and (b) examine the proposed DSM-5 symptom count criterion (and alternative symptom counts) in relation to concurrent functional impairment in these children,
Method
This project made use of a new and unique data resource, the PTSD after Acute Child Trauma (PACT) Data Archive. This international archive contains investigator-provided, de-identified datasets from prospective studies of children exposed to an acute potentially traumatic event. Currently, the archive contains datasets from 19 studies and from four countries. Each dataset in the archive includes basic data on demographics, trauma characteristics, one or more potential predictors of ongoing traumatic stress assessed soon after a traumatic event, and at least one measurement of traumatic stress symptoms at a later time point. The Institutional Review Board (IRB) of the Archive’s home institution determined that the PACT Data Archive is exempt from IRB review per 45 CFR 46.101(b) #4.
For the current analyses, we identified 15 datasets in the PACT Archive which included data from children and adolescents age 5 to 17 regarding acute traumatic stress symptoms and concurrent impairment two days to one month after an acute potentially traumatic event. These datasets represent studies conducted in four countries (US, UK, Australia, and Switzerland) with 1645 children. Table 1 shows sample characteristics and measures of acute traumatic stress and impairment in datasets included in the current analyses. In each study, children were recruited for participation based on their exposure to a potentially traumatic event (i.e. non-clinical samples)
Table 1.
Study characteristics: Datasets included in analyses
| Trauma type(s) | Age range | Country | N | Measure(s) of acute stress reactions | Mode of administration | Types of symptoms assessed |
|---|---|---|---|---|---|---|
| 1 Unintentional injury/Road traffic accident11 | 8–17 | US | 219 | CASQ25d | Questionnaire | intrusion, dissociation, avoidance, arousal, impairment |
| 2 Unintentional injury/Road traffic accident26 | 5–7 | US | 90 | CASQ25d | Questionnaire | intrusion, dissociation, avoidance, arousal, impairment |
| 3 Unintentional injury/Acute medical event1 | 8–17 | US | 164 | ASC-Kids1d | Questionnaire | intrusion, dissociation, avoidance, arousal, impairment |
| 4 Interpersonal violence27 | 8–17 | US | 38 | ISRC28 | Questionnaire | intrusion, dissociation, avoidance, arousal |
| 5 Unintentional injury/Acute medical event/Interpersonal violence/Road traffic accident a | 8–17 | US | 363 | ASC-Kids1d | Questionnaire | intrusion, dissociation, avoidance, arousal, impairment |
| 6 Unintentional injury28 | 8–17 | US | 88 | CPSS26 | Questionnaire | intrusion, dissociation, avoidance, arousal |
| 7 Unintentional injury b | 8–17 | US | 53 | ASC-Kids1d | Questionnaire | intrusion, dissociation, avoidance, arousal, impairment |
| 8 Interpersonal violence c | 12–17 | US | 61 | ISRC28 | Questionnaire | intrusion, dissociation, avoidance, arousal |
| 9 Unintentional injury20 | 7–16 | Australia | 131 | CRIES13–14 CTSQ27 | Questionnaire Questionnaire |
intrusion, avoidance, arousal intrusion, arousal |
| 10 Unintentional injury29 | 6–14 | Australia | 98 | CRIES13–14 CTSQ27 | Questionnaire Questionnaire |
intrusion, avoidance, arousal intrusion, arousal |
| 11 Unintentional injury30 | 6–14 | Australia | 45 | CTSQ27, TSCC31 | Questionnaire Questionnaire |
Intrusion, arousal intrusion, dissociation, avoidance, arousal |
| 12 Interpersonal violence/Road traffic accident21 | 10–16 | UK | 79 | CRIES13–14, ADIS15d | Questionnaire Interview |
intrusion, avoidance, arousal intrusion, dissociation, avoidance, arousal, impairment |
| 13 Road traffic accident5 | 5–10 | UK | 45 | CRIES13–14, CAPS-CA24d | Questionnaire Interview |
intrusion, avoidance, arousal intrusion, dissociation, avoidance, arousal, impairment |
| 14 Unintentional injury/Acute medical event/Interpersonal violence/Road traffic accident22 | 7–17 | Australia | 121 | ASC-Kids1d CPSS26d | Questionnaire Questionnaire |
intrusion, dissociation, avoidance, arousal, impairment intrusion, dissociation, avoidance, arousal, impairment |
| 15 Road traffic accident32 | 7–14 | Switzerland | 50 | IBS-A-KJ32–33d | Interview | intrusion, dissociation, avoidance, arousal, impairment |
Note: ADIS = Anxiety Disorders Interview Schedule; ASC-Kids = Acute Stress Checklist for Children; CAPS-CA = Clinician-Administered Posttraumatic Stress Disorder (PTSD) Scale for Children and Adolescents; CASQ = Child Acute Stress Questionnaire; CPSS = Child PTSD Symptom Scale; CRIES = Children’s Impact of Event Scale; CTSQ = Child Traumatic Stress Questionnaire; IBS-A-KJ = Interview zu Akute Belastungsstörungen bei Kindern und Jugendlichen; ISRC = Immediate Stress Reaction Questionnaire; TSCC = Trauma Symptom Checklist for Children
Kassam-Adams, N. and Gold, J. Unpublished data, 2011.
Kassam-Adams, N. and Winston, F. Unpublished data, 2006.
Fein J. Unpublished data, 2003.
Measure used to assess impairment in this study
The original studies from which these data were drawn used a range of different measures to assess acute traumatic stress symptoms and impairment, including both questionnaire and interview measures (see Table 1.) In order to combine data on specific acute traumatic stress symptoms (at the item level) across studies, we first identified candidate congruent items from each available measure within the dataset. For each DSM-5 ASD symptom, the core group of investigators in the PACT Project Group (N.K.A., P.P., J.K., D.D., R.L., R.N., R.M.S.) then reviewed available items and arrived at consensus regarding the combination of items for analysis. This expert group determined a) that each candidate item adequately represented the specific symptom construct (e.g. intrusive distressing memories), and b) that the candidate items from disparate measures were sufficiently congruent in wording to be combined for these analyses. Not all studies (datasets) were able to contribute to the assessment of every acute traumatic stress symptom (see Table 1). As one example, we identified that the proposed DSM-5 symptom of “spontaneous or cued recurrent, involuntary, intrusive distressing memories of the traumatic event” had been assessed on checklist measures via items such as “I can’t stop thinking about it” (Acute Stress Checklist for Children [ASC-Kids]1), “Having upsetting thoughts or images about the event that came into your head when you didn’t want them to” (Child PTSD Symptom Scale [CPSS]26), “Do you think about it even when you don’t mean to?” (Children’s Impact of Event Scales [CRIES]13–14), and on interview measures via prompts such as “Did you think about (event) even when you didn’t want to?” (Clinician-Administered PTSD Scale for Children and Adolescents [CAPS-CA]24), and “Do you have a lot of thoughts that you don’t want to have about (frightening event)?” (Anxiety Disorders Interview Scale [ADIS]15). The expert panel found that these were sufficiently congruent to be combined (as dichotomized ratings) for analysis.
Item ratings were then dichotomized utilizing each measure’s standard scoring rules for symptom presence; if such a standard was not available, this expert group reached consensus on an appropriate cut-point in the item rating scale for presence versus absence of the symptom, comparable to those utilized for similar measures. We also created a dichotomous variable for the presence/absence of concurrent impairment, based on items available within many of the traumatic stress measures assessing impairment in social, academic, or other functioning; such as “Since this happened, getting along with friends or family is harder for me.” (ASC-Kids1). These common dichotomous variables (14 symptom items and presence/absence of impairment) allowed analyses of pooled data from all 15 datasets regarding acute stress symptoms, and from nine of these datasets with regard to impairment. This approach to pooling data from existing studies is consistent with an “integrative data analysis” approach, with the potential advantages of increased sample heterogeneity and increased statistical power.16
Data analysis
Based on the common dichotomized ASD symptom items, we created an ASD symptom count variable (number of symptoms present) with potential scores ranging from 0 to 14. To evaluate the relationship between ASD symptoms and concurrent impairment, we first examined bivariate associations between each symptom item and impairment by means of Chi square analyses. We then examined the performance of different cut-off scores (i.e. the number of ASD symptoms required) to best predict the presence of concurrent impairment. All analyses were conducted with SPSS version 20 (SPSS, Chicago IL).
Results
Sample characteristics
Table 2 shows demographic characteristics, trauma type, and country of residence for the total combined sample across all 15 datasets. Children in this combined sample ranged in age from 5 to 17 years (mean = 11.6; SD = 3.0), about two thirds were male, and nearly half were of minority ethnicity. The most common index trauma was injury, although categories were not mutually exclusive, i.e. a child who was injured and was in a road traffic accident was counted in both categories. Mean time from the acute event to assessment of acute stress reactions was 13.1 days (SD = 8.3).
Table 2.
Characteristics of combined sample (n = 1645)
| n (%) | |
|---|---|
| Age in years | |
| 5 to 7 | 149 (9.1) |
| 8 to 11 | 615 (37.4) |
| 12 to 14 | 556 (33.8) |
| 15 to 17 | 325 (19.8) |
| Sex (male) | 1067 (64.9) |
| Ethnic minority | 760 (46.2) |
| Trauma type (not mutually exclusive) | |
| Unintentional injury | 1177 (71.6) |
| Road traffic accident | 519 (31.6) |
| Interpersonal violence | 187 (11.4) |
| Acute medical event (non-injury) | 105 (6.4) |
| Country | |
| Australia | 395 (24.0) |
| Switzerland | 50 (3.0) |
| United Kingdom | 124 (7.5) |
| United States | 1076 (65.4) |
Prevalence of proposed DSM-5 ASD symptoms and functional impairment in children
See Table 3 for prevalence of each ASD symptom and of impairment. The most commonly reported symptoms were avoidance of thoughts, conversations, or feelings (51.4%), altered sense of reality (42.5%), and intrusive distressing memories (40.6%). Flashbacks or reliving (15.6%) and distressing dreams (13.6%) were least commonly endorsed. The number of symptoms reported by children ranged from 0 to 13 (median = 3 symptoms; mean = 3.6; SD = 3.0), with 202 (12.3%) reporting eight or more symptoms. Impairment ratings were available for a total of 1172 children, from nine of the 15 datasets. Less than half of the children reported impairment. One hundred twenty-three (10.5%) children met proposed DSM-5 ASD criteria of eight or more symptoms plus significant impairment.
Table 3.
Prevalence of DSM-5 acute stress disorder (ASD) symptoms and functional impairment in children in combined sample (overall n = 1645)
| ASD symptom | Prevalence of symptom: n (%) | n for analyses | Number of studies |
|---|---|---|---|
| 1. Intrusive distressing memories of event | 666 (40.6) | 1640 | 15 |
| 2. Recurrent distressing dreams | 225 (13.7) | 1586 | 15 |
| 3. Flashbacks/re-living | 256 (15.6) | 1553 | 15 |
| 4. Intense distress at reminders | 522 (35.2) | 1481 | 15 |
| 5. Numbing, detachment, reduced responsiveness | 292 (23.5) | 1241 | 12 |
| 6. Altered sense of reality | 449 (42.5) | 1056 | 10 |
| 7. Inability to remember important aspect(s) of event | 351 (25.9) | 1356 | 13 |
| 8. Avoidance of thoughts, conversations, feelings | 845 (51.4) | 1643 | 15 |
| 9. Avoidance of activities, places, physical reminders | 541 (35.1) | 1540 | 13 |
| 10. Sleep disturbance | 455 (28.6) | 1592 | 15 |
| 11. Hypervigilance | 480 (36.3) | 1323 | 14 |
| 12. Irritable or aggressive behavior | 412 (26.0) | 1585 | 15 |
| 13. Exaggerated startle response | 393 (24.7) | 1593 | 15 |
| 14. Agitation or restlessness | 78 (20.5) | 380 | 4 |
| Impairment from ASD symptoms | 485 (41.4) | 1172 | 9 |
Association of ASD symptoms with concurrent reports of impairment in children
Individual ASD symptoms were associated with greater likelihood of concurrent impairment. For 13 of the proposed 14 DSM-5 symptoms, Chi square analyses revealed that a higher proportion of children who reported the specific symptom also reported impairment (see Table 4). This was true for all symptoms other than agitation (smaller sample size available for analysis may account for this non-significant finding.)
Table 4.
Association of each DSM-5 acute stress disorder (ASD) symptom with concurrent functional impairment (overall n = 1172)
| ASD symptom | Proportion with functional impairment | n for analysis | χ2 (df=1) | |
|---|---|---|---|---|
| With Symptom (%) | Without symptom (%) | |||
| 15. Intrusive distressing memories of event | 58.3 | 31.6 | 1167 | 79.75* |
| 16. Recurrent distressing dreams | 66.1 | 37.3 | 1169 | 49.91* |
| 17. Flashbacks/re-living | 70.1 | 36.3 | 1162 | 69.59* |
| 18. Intense distress at reminders | 57.7 | 33.0 | 1056 | 58.99* |
| 19. Numbing, detachment, reduced responsiveness | 59.1 | 35.5 | 1051 | 44.09* |
| 20. Altered sense of reality | 49.3 | 34.1 | 948 | 22.16* |
| 21. Inability to remember important aspect(s) of event | 50.2 | 37.8 | 1146 | 14.31* |
| 22. Avoidance of thoughts, conversations, feelings | 48.6 | 33.3 | 1172 | 28.38* |
| 23. Avoidance of activities, places, physical reminders | 53.3 | 32.7 | 1120 | 45.19* |
| 24. Sleep disturbance | 63.9 | 32.1 | 1168 | 100.67* |
| 25. Hypervigilance | 63.8 | 39.5 | 900 | 46.74* |
| 26. Irritable or aggressive behavior | 62.3 | 34.9 | 1161 | 64.46* |
| 27. Exaggerated startle response | 59.3 | 36.6 | 1164 | 41.46* |
| 28. Agitation or restlessness | 30.0 | 19.8 | 307 | 3.24 |
Note:
p < .001
We examined the utility of the proposed 8-symptom requirement for ASD by assessing how well this symptom cutoff discriminated between children with and without significant acute functional impairment (see Table 5). Positive predictive value (PPV) was high; 75% of children with at least 8 symptoms reported impairment (compared to 36% of those with fewer than 8 symptoms). However, sensitivity was low (.25), such that only one quarter of those with acute impairment would have met criteria for an ASD diagnosis if 8 symptoms were required.
Table 5.
Performance of different acute stress symptom requirements in predicting concurrent ratings of impairment (n = 1172).
| Minimum number of acute stress symptoms required | Sensitivity | Specificity | PPV | NPV | % correctly classified |
|---|---|---|---|---|---|
| 13 symptoms | .01 | 1.00 | 1.00 | .59 | 58.9 |
| 12 symptoms | .04 | 1.00 | .95 | .60 | 60.0 |
| 11 symptoms | .07 | 1.00 | .92 | .60 | 61.3 |
| 10 symptoms | .13 | .99 | .90 | .62 | 63.5 |
| 9 symptoms | .21 | .97 | .81 | .63 | 65.2 |
| 8 symptoms | .25 | .94 | .75 | .64 | 65.5 |
| 7 symptoms | .31 | .89 | .67 | .65 | 65.0 |
| 6 symptoms | .40 | .85 | .66 | .67 | 66.6 |
| 5 symptoms | .52 | .76 | .60 | .69 | 65.7 |
| 4 symptoms | .61 | .65 | .55 | .70 | 63.5 |
| 3 symptoms | .73 | .57 | .54 | .75 | 63.6 |
| 2 symptoms | .84 | .43 | .51 | .80 | 60.2 |
| 1 symptom | .92 | .22 | .45 | .79 | 50.8 |
Note: The workgroup developing proposed DSM-5 criteria for acute stress disorder (ASD) has suggested 8 symptoms as a diagnostic criterion (in bold). NPV = Negative predictive value; PPV = Positive predictive value.
Table 5 presents sensitivity, specificity, PPV, negative predictive value (NPV), and percent correctly classified for the 8-symptom requirement and alternative symptom counts. In receiver operating characteristics (ROC) curve analyses of ASD symptom count as a ‘predictor’ of concurrent impairment, the area under the curve (AUC) was .70 (95% CI: .67–.73). Examining the coordinates of the ROC curve (Figure 1 and Table 5) suggests that an optimal balance of sensitivity and specificity is achieved at a cutpoint of 3 or 4 symptoms. For example, a 3-symptom rule resulted in greater sensitivity than the 8-symptom rule (detecting three quarters of those with impairment), moderate specificity, and a similar proportion of children correctly classified. Compared to the 10.5% of children who had at least eight ASD symptoms and impairment, 356 (30.4%) had at least three ASD symptoms and impairment.
Figure 1.
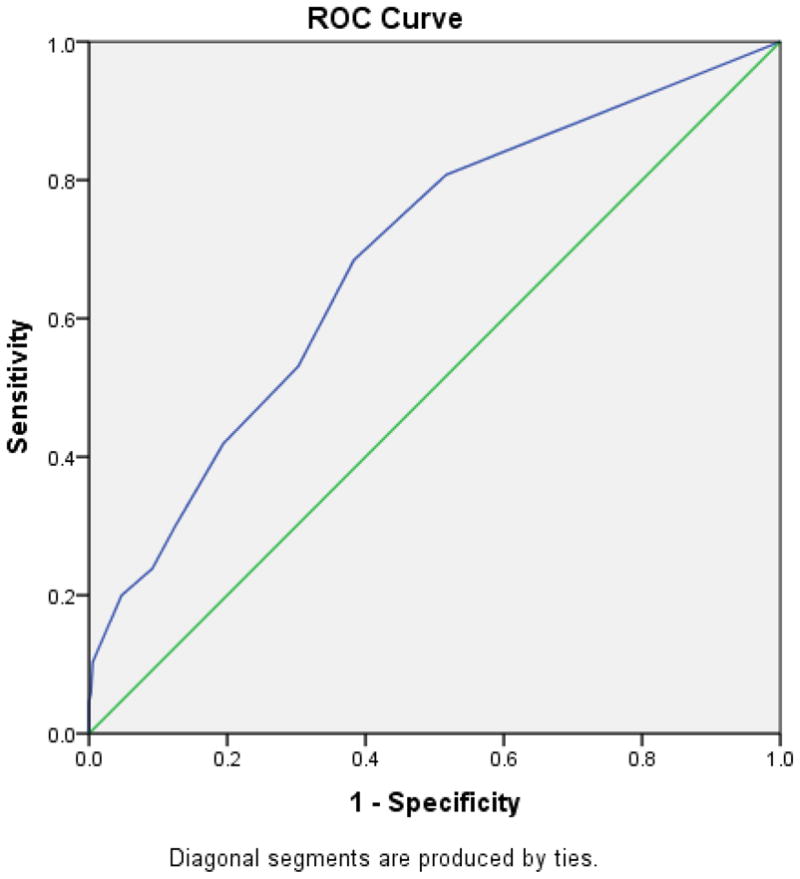
Receiver Operating Characteristics (ROC) curve for acute stress disorder (ASD) symptom count as a predictor of the presence of concurrent functional impairment.
In exploratory analyses, we examined the performance of the 8-symptom requirement for school-age children (ages 5 to 11 years; n = 552) and for adolescents (age 12 to 17 years; n = 620) separately. For the younger group, sensitivity = .32, specificity = .92; for the older group, sensitivity = .20, specificity = .95. A 3-symptom rule resulted in improved sensitivity in both younger and older children (.79 and .69, respectively) and retained moderate sensitivity in each age group (.51 and .62, respectively)
Discussion
Clear conceptualization and empirically-validated diagnostic criteria can advance efforts to identify children and youth with significant distress who need increased psychosocial supports or formal clinical attention. Data from 15 studies including 1645 children assessed soon after an acute trauma were combined to examine the utility of proposed DSM-5 ASD symptom criteria. Each symptom was endorsed by 14% to 51% of children. Thirteen of the 14 symptoms were individually associated with impairment, suggesting that this list of symptoms does capture key aspects of traumatic stress responses that can create distress and interfere with children’s ability to function in the acute post-trauma phase. These analyses provide an initial benchmark for comparison with adult samples. For example, the ASD workgroup reported that 20% of adults in three “large scale datasets” from Israel, the UK, and Australia met the 8-symptom criterion3. In the current large combined dataset of children and adolescents, a smaller proportion (12%) met this proposed symptom criterion.
In constructing diagnostic criteria for mental disorders, the DSM-5 development process has attempted to clarify the distinction between psychiatric symptoms and the potentially disabling consequences of those symptoms.17 However, in the case of early emotional responses to extremely difficult events and experiences, it seems particularly relevant to consider the connection between symptoms and functional impairment in determining what constitutes a ‘disorder.’ The revised ASD diagnostic criteria aim to “facilitate treatment for those suffering significant distress and whose response suggests that this distress may be interfering sufficiently or distressing the person excessively such that treatment may facilitate recovery.”3 Examining the current results from this perspective, the proposed 8-symptom requirement falls short for children and adolescents. Its low sensitivity means that 75% of children who reported impairment had fewer than 8 symptoms and would not have received a diagnosis of ASD. For children and adolescents, requiring fewer symptoms would better achieve the objective of identifying those with clinically relevant distress or interference with functioning. These results suggest that a lower symptom count criterion (three or four symptoms) could achieve higher sensitivity while maintaining a reasonable degree of specificity. This trade-off between specificity and sensitivity is warranted in most clinical settings, where the disadvantages of missing a positive case (i.e., a child in need of clinical attention in the acute aftermath of trauma exposure) are likely to be greater than the disadvantages of offering services to a child who does not need them. Appropriate clinical responses to acute stress disorder include brief interventions that incorporate trauma-focused cognitive behavioral approaches18 and that shore up a child’s existing support systems by helping parents respond appropriately.19
A limitation of this investigation is the need to use solely dichotomous values in order to combine items across different measures in the combined dataset. Another potential limitation is that when both symptoms and impairment are measured by self-report, their association may be in part an artifact of generalized subjective distress. The set of 15 studies included here reflect both the strengths and limitations of existing research studies on acute traumatic stress reactions in children. For example, the datasets included here do not include children from the developing world and thus replication with other populations is needed. We believe that these datasets represent a fairly large proportion of the existing child studies that have assessed ASD symptoms within one month of a potentially traumatic event (the authors welcome contact from investigators who have relevant datasets and would like to learn about adding these to the PACT Archive). Many of the available studies have assessed acute stress reactions after unintentional injuries or road traffic accidents. These represent highly prevalent types of acute child trauma which convey risk for both acute and persistent traumatic stress disorders11, 20–22, and thus have substantial public health impact. Nevertheless, the field would benefit from more prospective studies that carefully assess child acute stress reactions within the first month after other types of traumatic events (e.g., disasters, interpersonal violence). It is possible that symptom criteria might vary for acute events of different types or intensities. Future research efforts should include all fourteen proposed DSM-5 ASD symptoms (and other candidate items which may be relevant for children) in order to test the utility of alternative acute stress symptom requirements as predictors of significant concurrent (and persistent) distress and impairment in children and adolescents exposed to a range of acute traumas. Although it is not the intention of the DSM-5 ASD criteria, the longitudinal association of acute traumatic stress symptoms with ongoing or persistent distress and impairment is certainly of great clinical interest and should continue to be examined in prospective studies.
These analyses represent the fruit of a new and unique data resource for child traumatic stress studies, the PACT Data Archive, which allowed us to combine individual-level data from 15 studies to examine children’s acute traumatic stress reactions. Increasingly, national research funding agencies are encouraging or requiring that data generated from publicly funded research be archived or made available to other investigators beyond the life of the original investigation.23–25 The current analyses demonstrate the potential value of such data-sharing initiatives for integrative data analysis.
Clinical Guidance
Clinicians should inquire about acute traumatic stress reactions in children with a known, recent trauma exposure. Acute traumatic stress reactions in the first month appear to be fairly common: in this large international dataset, half of the children reported avoidance of thoughts, conversations, or feelings about the trauma, and nearly as many experienced dissociation (altered sense of reality), or intrusive distressing memories.
A significant proportion of children (about 4 in 10) had some degree of impairment in functioning within this first month. Having multiple acute stress reaction was associated with a greater likelihood of impairment.
Regardless of whether formal diagnostic criteria for ASD are met, when a child has three or four acute stress reactions in the early aftermath of trauma exposure, clinicians should consider providing services or additional follow-up to monitor the course of emotional recovery.
These results point the way to future studies that could help to elucidate the nuances of relationships among child ASD symptoms and impairment in an expanded set of acute trauma populations (e.g., in non-industrialized countries, and with a greater range of types of acute trauma). However, given the time needed to collect prospective data to test new diagnostic criteria (and alternatives) in new research studies, we suggest that the 15 studies included in this large combined dataset represent the best currently available data which can inform the DSM-5 ASD symptom count criteria for children. These results strongly suggest that for trauma-exposed children the proposed 8-symptom rule may be too restrictive, and that serious consideration should be given to implementing alternate criteria for children.
Acknowledgments
This work was supported by grant R21MH086304 from the National Institutes of Mental Health.
Footnotes
Disclosure: Drs. Kassam-Adams, Palmieri, Rork, Delahanty, Kenardy, Landolt, Le Broque, Marsac, Meiser-Stedman, Nixon, and Bui, and Ms. Kohser and McGrath report no biomedical financial interests or potential conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Dr. Nancy Kassam-Adams, Children’s Hospital of Philadelphia and the Perelman School of Medicine, University of Pennsylvania.
Dr. Patrick A. Palmieri, Summa Health System.
Dr. Kristine Rork, University Hospitals, Rainbow Babies and Children’s Hospitals, Case Western Reserve University.
Dr. Douglas L. Delahanty, Kent State University.
Dr. Justin Kenardy, University of Queensland, Australia.
Ms. Kristen L. Kohser, Children’s Hospital of Philadelphia.
Dr. Markus A. Landolt, University Children’s Hospital Zurich, Switzerland.
Dr. Robyne Le Brocque, University of Queensland, Australia.
Dr. Meghan L. Marsac, Children’s Hospital of Philadelphia.
Dr. Richard Meiser-Stedman, Medical Research Council Cognition and Brain Sciences Unit, Cambridge, United Kingdom.
Dr. Reginald D. V. Nixon, Flinders University, Australia.
Dr. Eric Bui, Universite de Toulouse and the Centre Hospitalier Universitaire (CHU) de Toulouse, France, Massachusetts General Hospital, and Harvard Medical School.
Ms. Caitlin McGrath, University of Queensland, Australia.
References
- 1.Kassam-Adams N. The acute stress checklist for children (ASC-Kids): Development of a child self-report measure. J Trauma Stress. 2006;19(1):129–139. doi: 10.1002/jts.20090. [DOI] [PubMed] [Google Scholar]
- 2.Miller A, et al. A diagnostic interview for acute stress disorder for children and adolescents. J Trauma Stress. 2009;22:549–556. doi: 10.1002/jts.20471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bryant R, et al. A review of acute stress disorder in DSM-5. Depress Anxiety. 2011;28:802–817. doi: 10.1002/da.20737. [DOI] [PubMed] [Google Scholar]
- 4.Carrion V, et al. Toward an empirical definition of pediatric PTSD: The phenomenology of PTSD symptoms in youth. J Am Acad Child Adolesc Psychiatry. 2002;41(2):166–73. doi: 10.1097/00004583-200202000-00010. [DOI] [PubMed] [Google Scholar]
- 5.Meiser-Stedman R, et al. The posttraumatic stress disorder diagnosis in preschool- and elementary school-age children exposed to motor vehicle accidents. Am J Psychiatry. 2008;165:1326–1337. doi: 10.1176/appi.ajp.2008.07081282. [DOI] [PubMed] [Google Scholar]
- 6.Scheeringa M, Zeanah C, Cohen J. PTSD in children and adolesccents: Toward an empirically based algorithm. Depress Anxiety. 2011;28:770–782. doi: 10.1002/da.20736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Friedman M, et al. Considering PTSD for DSM-5. Depress Anxiety. 2011;28:750–769. doi: 10.1002/da.20767. [DOI] [PubMed] [Google Scholar]
- 8.Bryant B, et al. Psychological consequences of road traffic accidents for children and their mothers. Psychol Med. 2004;34:335–346. doi: 10.1017/s0033291703001053. [DOI] [PubMed] [Google Scholar]
- 9.Bryant R, Salmon K, Sinclair E. The relationship between acute stress disorder and posttraumatic stress disorder in injured children. J Trauma Stress. 2007;20:1075–1079. doi: 10.1002/jts.20282. [DOI] [PubMed] [Google Scholar]
- 10.Harvey A, Bryant R. The relationship between acute stress disorder and posttraumatic stress disorder: A prospective evaluation of motor vehicle accident survivors. J Consult Clin Psychol. 1998;67(3):507–512. doi: 10.1037//0022-006x.66.3.507. [DOI] [PubMed] [Google Scholar]
- 11.Kassam-Adams N, Winston FK. Predicting child PTSD: The relationship between acute stress disorder and PTSD in injured children. J Am Acad Child Adolesc Psychiatry. 2004;43(4):403–411. doi: 10.1097/00004583-200404000-00006. [DOI] [PubMed] [Google Scholar]
- 12.Harvey A, Bryant R. Two-year prospective evaluation of the relationship between acute stress disorder and posttraumatic stress disorder following mild traumatic brain injury. Am J Psychiatry. 2000;157(2):626–628. doi: 10.1176/appi.ajp.157.4.626. [DOI] [PubMed] [Google Scholar]
- 13.Dyregrov A, Kuterovac G, Barath A. Factor analysis of the impact of Event Scale with children in war. Scand J Psychol. 1996;37(4):339–350. doi: 10.1111/j.1467-9450.1996.tb00667.x. [DOI] [PubMed] [Google Scholar]
- 14.Perrin S, Meiser-Stedman R, Smith P. The Childrens Revised Impact of Event Scale (CRIES): Validity as a Screening Instrument for PTSD. Behav Cogn Psychother. 2005;33:487–498. [Google Scholar]
- 15.Silverman W, Albano A. Anxiety Disorder Interview Schedule for DSM–IV: Child and Parent Interview Schedule. San Antonio, TX: Psychological Corporation; 1996. [Google Scholar]
- 16.Curran P, Hussong A. Integrative Data Analysis: The simultaneous analysis of multiple data sets. Psychol Methods. 2009;14(2):81–100. doi: 10.1037/a0015914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.DSM-5 Impairment and Disability Assessment Study Group. [accessed February 14, 2012];Mental Disorders: Separating Symptoms and Disabilities in the DSM-5 [White Paper] 2010 http://www.dsm5.org/proposedrevision/Documents/ProposedDefin-MentalDisorder_IDASG.pdf.
- 18.National Institute for Clinical Excellence. Clinical Guideline. London: 2005. Post-traumatic stress disorder (PTSD): The management of PTSD in adults and children in primary and secondary care. [Google Scholar]
- 19.Berkowitz SJ, Stover CS, Marans SR. The Child and Family Traumatic Stress Intervention: secondary prevention for youth at risk of developing PTSD. J Child Psychol Psychiatry. 2011;52(6):676–85. doi: 10.1111/j.1469-7610.2010.02321.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Le Brocque RM, Hendrikz J, Kenardy JA. The course of posttraumatic stress in children: Examination of recovery trajectories following traumatic injury. J Pediatr Psychol. 2010;35:637–645. doi: 10.1093/jpepsy/jsp050. [DOI] [PubMed] [Google Scholar]
- 21.Meiser-Stedman R, et al. Acute stress disorder and posttraumatic stress disorder in children and adolescents involved in assaults and motor vehicle accidents. Am J Psychiatry. 2005;162:1381–1383. doi: 10.1176/appi.ajp.162.7.1381. [DOI] [PubMed] [Google Scholar]
- 22.Nixon R, et al. Screening and predicting posttraumatic stress and depression in children following single-incident trauma. J Clin Child Adolesc Psychol. 2010;39(4):588–596. doi: 10.1080/15374416.2010.486322. [DOI] [PubMed] [Google Scholar]
- 23.Research Councils UK. [accessed February 14, 2012];RCUK Common Principles on Data Policy. http://www.rcuk.ac.uk/research/Pages/DataPolicy.aspx.
- 24.Organization for Economic Co-operation and Development. OECD Principles and Guidelines for Access to Research Data from Public Funding. Paris, France: OECD Publications; 2007. [Google Scholar]
- 25.National Institutes of Health. [accessed February 14, 2012];Final NIH Statement on Sharing Research Data (NOT-OD-03-032) 2003 Feb 26; http://grants.nih.gov/grants/guide/notice-files/NOT-OD-03-032.html.
- 26.Feinberg M. Demographic and psychological concomitants of ASD and PTSD: An analysis of children after traffic injury. Graduate School of Education, Univ. of Pennsylvania; 2004. [Google Scholar]
- 27.Fein J, et al. Persistence of posttraumatic stress in violently injured youth seen in the emergency department. Arch Pediatr Adolesc Med. 2002;156(8):836–840. doi: 10.1001/archpedi.156.8.836. [DOI] [PubMed] [Google Scholar]
- 28.Kassam-Adams N, et al. A pilot randomized controlled trial assessing secondary prevention of traumatic stress integrated into pediatric trauma care. J Trauma Stress. 2011;24(3):252–9. doi: 10.1002/jts.20640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kenardy J, et al. Information provision intervention for children and their parents following pediatric accidental injury. Eur Child Adolesc Psychiatry. 2008;17(5):316–325. doi: 10.1007/s00787-007-0673-5. [DOI] [PubMed] [Google Scholar]
- 30.Cox C, Kenardy J. A randomised controlled trial of a web-based early intervention for children and their parents following accidental injury. J Pediatr Psychol. 2010;35:581–592. doi: 10.1093/jpepsy/jsp095. [DOI] [PubMed] [Google Scholar]
- 31.Briere J. Trauma Symptom Checklist for Children. Lutz, FL: Psychological Assessment Resources; 1996. [Google Scholar]
- 32.Zehnder D, Meuli M, Landolt M. Effectiveness of a single-session early psychological intervention for children after road traffic accidents: A randomised controlled trial. Child Adolesc Psychiatry Ment Health. 2010;4:7. doi: 10.1186/1753-2000-4-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Steil R, Füchsel G. Interviews zu Belastungsstörungen bei Kindern und Jugendlichen (IBS-KJ) Göttingen: Hogrefe; 2006. [Google Scholar]


