Abstract
Homeless youth are at high risk for human immunodeficiency virus (HIV) and other sexually transmitted infections (STI), yet those at greatest risk may never have been tested for HIV or STI. In a probability sample of sexually active homeless youth in Los Angeles (n =305), this study identifies factors associated with HIV/STI testing status. Most youth (85%) had ever been tested and 47% had tested in the past 3 months. Recent testing was significantly more likely among youth who self-identified as gay, were Hispanic, injected drugs, and used drop-in centers, and marginally more likely among youth with more depressive symptoms. Drop-in center use mediated the association of injection drug use with HIV/STI testing. HIV/STI testing was unrelated to sexual risk behavior. Drop-in centers can play an important role in facilitating testing, including among injection drug users, but more outreach is needed to encourage testing in other at-risk subgroups.
Keywords: homeless youth, HIV testing, STI testing
INTRODUCTION
Homeless youth in the United States are at high risk for contracting and transmitting human immunodeficiency virus (HIV) and other sexually transmitted infections (STI). HIV seroprevalence estimates among homeless youth vary greatly depending on the sample [e.g., 5% (Luna & Rotheram-Borus, 1992), 12% (Pfeifer & Oliver, 1997), and 17% (Sweeney, Lindegren, Buehler, Onorato, & Janssen, 1995)], but even the lowest estimate is at least two times higher than seroprevalence in non-homeless populations of youth (DiClemente, 1992; Sweeney, et al., 1995; Walters, 1999). Rates of HIV and STI testing among homeless youth tend to be higher than testing rates among youth in the general population, with more than half of homeless youth having ever been tested for either HIV or STI (E. Goodman & Berecochea, 1994; Gwadz, et al., 2010; Tyler & Melander, 2010; Young & Rice, 2011) compared with only 22.6% of the general population of sexually active youth (Balaji, et al., 2012). Nonetheless, homeless youth at the highest risk for HIV and STI may not be testing regularly or at all (Gwadz, et al., 2010).
HIV testing is the primary strategy recommended by the CDC for reducing the transmission of HIV (Centers for Disease Control and Prevention, 2006). Early detection of HIV can slow the progression and transmission of the disease through anti-retroviral treatment (Castilla, et al., 2005; Centers for Disease Control and Prevention, 2009) and by increasing protective behaviors such as condom use (Marks, Crepaz, & Janssen, 2006; Ober, et al., 2010). The rate of HIV transmission from those who are unaware of their HIV status is an estimated 3.5 times higher than transmission from individuals who know they are HIV positive (Marks, et al., 2006). This is consistent with the basic elements of the health belief model which suggest that awareness of one’s own risk for and susceptibility to disease are associated with protective health behaviors (Janz, Champion, & Strecher, 2002). Testing and getting treated for sexually transmitted infections (STI) other than HIV also is important to reducing the spread of HIV because having an STI increases the likelihood of HIV transmission (Venkatesh, et al., 2011).
A small number of prior studies have examined predictors of HIV/STI testing among homeless youth, suggesting that certain factors are associated with higher rates of testing more than others. For example, youth who engage in riskier sexual behaviors, such as having a greater number of sexual partners (E. Goodman & Berecochea, 1994) and engaging in risky sex with partners outside of their social networks (Tyler & Melander, 2010), are more likely to get tested. Homeless youth who inject drugs (E. Goodman & Berecochea, 1994) and use amphetamines (Solorio, Milburn, Weiss, & Batterham, 2006) are also more likely to get tested. There are demographic differences as well, with testing more likely among females and older youth (E. Goodman & Berecochea, 1994; Solorio, Milburn, Weiss, et al., 2006; Tyler & Melander, 2010), African American and mixed race youth, and males who self-identify as gay or bisexual (Solorio, Milburn, Weiss, et al., 2006). In addition, youth who have become or gotten someone pregnant are more likely to test (Solorio, Milburn, Rotheram-Borus, Higgins, & Gelberg, 2006), possibly because they use services more frequently, are offered HIV/STI testing as part of prenatal care, or because they engage in risky sexual behaviors such as unprotected sex and seek services to find out if they have an STI. Finally, at-risk youth who are depressed may exhibit higher risk behaviors than youth who are not depressed (Tolou-Shams, Brown, Houck, & Lescano, 2008), potentially leading to a higher probability of using services and receiving an HIV or other STI test than youth who are not depressed. However, there are limitations to these studies that suggest the need for further research in this area. For example, findings from some of these studies are based on convenience samples of homeless youth and thus are not generalizable to homeless youth outside of study samples. Further, these studies have tended to focus primarily on demographic and behavioral factors, not considering structural factors such as service use that may be associated with HIV/STI testing.
There is some evidence suggesting that HIV and STI testing may be more likely among youth who use services such as shelters and drop-in centers. For example, HIV testing varies by sub-group of homeless youth, with “service-involved” youth (i.e., youth living in temporary placements, such as shelters, which are connected to services) more likely to test for HIV than “street” youth (those living on the streets) or “nomads” (youth who travel around) (Gwadz, et al., 2010). Because service-involved youth are more likely to test for HIV and other STI, as are youth that engage in high-risk behaviors, there may be an indirect relationship between high-risk behaviors and HIV/STI testing that is mediated by use of services – drop-in center use in particular. Drop-in centers offer a wide variety of services that can include health, mental health and substance abuse counseling, case management, and needle exchange. These centers have particular appeal to homeless youth in that they are perceived as offering greater flexibility, less paperwork, and less necessity to disclose personal information than other types of services; in fact, 78% of homeless youth report accessing needed services at drop-in centers whereas only 40% of homeless youth report using shelters (De Rosa, et al., 1999). High-risk youth, including those who are depressed, may test more because of their greater use of drop-in center services and the availability of testing at service agencies. Further examination of factors associated with HIV/STI testing, particularly the relationship between high-risk behaviors, use of services, and HIV/STI testing, is needed to better understand HIV/STI testing behaviors and to inform the development of interventions to increase HIV/STI testing in this population.
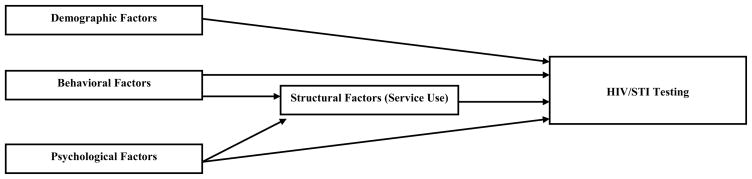
This study sought to supplement existing literature by examining the demographic, psychological, behavioral, and structural factors associated with HIV/STI testing and whether the association between some of these factors and HIV/STI testing is mediated by drop-in center use among homeless youth in Los Angeles County (Figure 1). We hypothesized that youth would be more likely to test if they engaged in HIV risk behaviors (such as injection drug use and high-risk sexual behaviors), self-identified as gay, perceived themselves to be more susceptible to HIV, experienced more depressive symptoms, and accessed services at either a youth homeless shelter or drop-in center. We also hypothesized that the association between high-risk behaviors and HIV/STI testing would be mediated by drop-in center use. Specifically, we expected that youth in greater need of services such as injection drug users (who may use drop-in centers for needle exchange), youth experiencing more depressive symptoms (who may seek counseling services), and youth who self-identify as gay (who may seek services tailored to the needs of sexual minorities) would be more likely to test for HIV/STI potentially because of their greater use of drop-in centers.
Figure 1.
Conceptual Model
METHODS
Study Design
We recruited a sample of homeless youth from shelters, drop-in centers, and street venues in Los Angeles County between October 2008 and August 2009. Because a sampling frame of all the homeless youth in the study area is not available, we adopted a multi-stage design. Specifically, we adopted a two-stage design that involved first developing a sampling frame of sites used by homeless youth and then sampling youth within the selected sites. We developed two sampling frames of sites: one for eligible service sites (shelters and drop-ins) and the other for street sites(or “hangouts”) in the study area. The first sampling frame, for service sites, was developed using existing directories of services for homeless individuals. Service sites were considered eligible if they were located in the study area and the majority of their clientele was ages 13 to 24 and English speaking. Service sites not limited to that age group were eligible if they had a specific program geared toward youth. In addition, for short-term transitional housing programs the average length of stay had to be one year or less. Our final list of service sites consisted of 22 eligible sites: 15 shelters and 7 drop-in centers. All the eligible service sites in the study area that agreed to participate into the study were selected with certainty and thus the sites can be considered strata.
The second sampling frame, for street sites, was developed with input from service providers, outreach agencies, and homeless youth. We ultimately identified 19 street sites in the study area where homeless youth were known to congregate and hang out. All of these street sites were included in the study and thus can be considered as strata. Each of the 41 service and street sites were investigated intensively with the purpose of obtaining an estimate of the average number of youth served daily by the service sites and the average number of youth that congregate at the street venues in a given day. This information was used to assign an overall complete quota to each site which was approximately proportional to the size of a site. The second stage of the sampling design consisted of drawing a probability sample of homeless youth from the 41 study sites. A probability sampling method is any method of sampling that utilizes some form of random selection. In order to have a random selection method, you must set up some process or procedure that assures that the different units in your population have equal probabilities of being chosen. Strategies specific to the type of sites were developed to randomly select the youths to be approached, screened and interviewed.
The sampling design deviates from a proportionate-to-size stratified random sample (where a constant proportion of the population is sampled from every site) for the following reasons: changes in the sampling rates during the fielding period; differential response rates of youths across sites; and variability in how frequently youth access shelters, drop-ins and street venues. This last factor meant that some youth were more likely than others to be included in the sample for a given site. We accounted for the differential frequency of using sites by asking participants how often they had gone to a shelter, drop-in or street site in the study area during the past 30 days and using this information to correct their sampling probability. We corrected departures from a proportionate-to-size stratified random sample with sampling weights.
Participants
Youth were eligible for the study if they: a) were between the ages of 13–24; b) were not currently living with a parent or guardian; c) were not getting most of their support for food and housing from family or a guardian; d) spent the previous night in a shelter, outdoor or public place, hotel or motel room rented with friends (because of no place else to go), or other place not intended as a domicile; and e) were English speaking. Interviews were conducted between October 2008 and August 2009. Of 446 youth who initially screened eligible for the study, 437 were interviewed. Of those interviewed, 18 were later found to be ineligible and excluded from the sample because they were too old (n = 2), or were suspected to be not homeless (n = 1), or a repeater (n = 15). This resulted in a study sample of 419 and a response rate of approximately 98%. For the present analysis, we selected a subsample of this population that consisted of youth who reported having sexual intercourse (either vaginal or anal) with at least one sexual partner in the past three months (n = 305). (309 youth reported having intercourse in the past three months, but four were missing data for their last sexual event and thus could not be included in our event model. As such, our data reflect the 305 who were included in this model.) The analytic sample had a mean age of 20 (SD = 2.28), 24% were Black, 36% White, 19% Hispanic, and 21% of another race or ethnicity (Table 1). Half had no high school diploma or GED, 30% had a diploma or GED, and 20% had some college or had finished college. Most youth (66%) reported being heterosexual, while 26% identified as bisexual, and 8% reported they were homosexual
Table 1.
Demographic and Risk Characteristics
| No HIV Test (N=163) | HIV Test (N=142) | |
|---|---|---|
|
| ||
| Mean (SE) or % | Mean (SE) or % | |
| Demographic Characterstics | ||
| Age | 20.16 (0.21) | 20.7 (0.20) |
| Male | 60% | 68% |
| Race | ||
| Black | 27% | 20% |
| White | 38% | 35% |
| Hispanic | 14% | 24% |
| Other | 21% | 21% |
| Levels of Education | ||
| No High School Diploma or GED | 48% | 52% |
| High School Diploma or GED | 32% | 26% |
| Some College | 20% | 23% |
| Sexual Orientation | ||
| Heterosexual | 71% | 63% |
| Homosexual | 3% | 12% |
| Bisexual | 26% | 25% |
| Psychological Charactersitics | ||
| Depression Score (CESD, range 0–3) | 0.83 (0.06) | 1.00 (0.07) |
| Perceived Susceptibility to HIV (range 1–4) | 2.39 (0.08) | 2.27 (0.09) |
| Behavioral Characteristics | ||
| Traveler | 37% | 37% |
| Injection drug use in past 6 months | 12% | 21% |
| Number of sex partners in past 3 months | 2.07 (0.19) | 2.46 (0.26) |
| Any unprotected sex with a casual or need-based partner | 26% | 27% |
| Number of recent sex partners who were casual or need-based | ||
| 0 were casual or need-based | 54% | 48% |
| 1 was casual or need-based | 25% | 18% |
| 2 or more were casual or need-based | 21% | 34% |
| Number of recent sex partners who respondent thinks had risky sex | ||
| 0 had risky sex | 17% | 15% |
| 1–2 had risky sex | 31% | 33% |
| 3 or more had risky sex | 52% | 52% |
| Structural Characteristics | ||
| Used a drop-in center the last month | 58% | 76% |
| Stayed in a shelter in the last month | 22% | 22% |
Procedures
After providing informed consent, trained study personnel conducted computer-assisted face-to-face structured interviews. These interviews lasted an average of 60 minutes, and youth were paid $25. The research protocol was approved by the institution’s internal review board and a Certificate of Confidentiality was obtained from the National Institutes of Health.
Measures
Our binary dependent variable was whether the participant had an HIV or STI test within the last three months. Four categories of predictors were considered : (1) demographic factors; (2) psychological factors; (3) behavioral factors; and (4) structural factors.
Demographic factors
Demographic factors included age in years, biological sex, race (Black, White, Hispanic or another race), level of education (a three-level categorical variable, treated as a continuous in the analysis: no high school diploma or GED, high school diploma or GED, had some college or completed college), and sexual orientation (a categorical variable indicating whether the youth reported being homosexual, bisexual, or heterosexual).
Psychological factors
Psychological factors included depressive symptoms and perceived susceptibility to HIV. We measured depressive symptoms with the 4-item Center for Epidemiologic Studies Depression (CESD) scale(Melchior, Huba, Brown, & Reback, 1993) (α = .81). The mean of the following 3 items was used to measure perceived susceptibility to HIV: “It would be easy for you to get the HIV infection or AIDS”, “Your behavior puts you at risk of HIV or AIDS” and “You worry about getting HIV or AIDS”(1 = strongly disagree to 4 = strongly agree) (α = .59).
Behavioral factors
Behavioral factors included whether or not the youth was a “traveler,” that is, whether they had lived in at least two states besides California since they left home (or since leaving home the last time, for those who had left home more than once), with at least one of those states being a non-neighboring state to California (i.e., a state other than Arizona, Nevada, or Oregon). Injection drug use was a binary variable measuring whether the participant had injected any drugs in the past six months. Four indicators of sexual risk behavior were examined: (a) the total number of sexual partners in the past 3 months, with sex defined as vaginal or anal intercourse (continuous), derived from the answer to the question “How may male/female partners did you have in the last three months”; (b) the number of sexual partners who were casual or need-based in the past 3 months, with casual partner defined for participants as “… someone who is not steady like a boyfriend or girlfriend, but instead is more casual, like once-in-a-while, ‘in the moment,’ or may be ‘just for fun,’” and need-based partner defined as “someone a person has sex with because they need money, food, a place to stay, drugs or alcohol, or something like that” (categorized as 0, 1, 2 or more); (c) any sex without a condom with a casual or need-based partner in the past 3 months, derived from answers to the question “how many of these times [the times having sex with the partner] did you use a condom”; and (d) the number of sexual partners within participants’ social networks (they identified 20 people they knew who also knew them, and of those, identified which were sexual partners) who were believed to engage in risky sexual behaviors such as having multiple sex partners, having sex with someone they didn’t know, or not using a condom with a new partner (categorized as 0, 1–2, 3 or more). The variables assessing number of and unprotected sex with casual or need-based partners were derived from information obtained on up to four recent sex partners.
Structural factors
Separate items assessed whether respondents used a drop-in center or used an emergency shelter or transitional housing in the past 30 days.
Statistical Analysis
We began our analysis by using logistic regression to estimate the bivariate association between HIV/STI testing and each of our demographic, behavioral, psychological, and service use factors. Next, we estimated a multivariable logistic regression model of HIV/STI testing that included as predictors only those variables that were bivariately associated with HIV/STI testing at p < .10. Drop-in center use was not included as a predictor in the multivariable regression model, regardless of its bivariate association with HIV/STI testing, as this would interfere with our ability to evaluate this variable as a mediating factor in the final step of our analysis. The final step of our analysis involved estimating a path model to test for evidence of a mediating role of service use in the associations between HIV/STI testing and depressive symptoms, injection drug us, and self-identification as gay. In this path model, we estimated direct paths from each predictor to HIV/STI testing, as well as indirect paths that went through drop-in center use. We concluded that there was evidence of mediation if: (a) a demographic, behavioral, or psychological factor was associated with HIV/STI testing in the multivariable regression model; (b) the demographic, behavioral, or psychological factor was associated with drop-in center use in the path model and drop-in center use was in turn associated with HIV/STI testing; and (c) the association between the demographic, behavioral, or psychological factor and HIV/STI testing was reduced when drop-in center use was introduced to the model (Baron & Kenny, 1986).
RESULTS
The majority of youth (85%) reported that they had tested for HIV or other STI at least once in their life and just under half (47%) said they had received an HIV or STI test in the last three months. Of youth who tested in the last three months, almost all (95%) said they had received their test results. The mean CESD depression score (range 0–3) was 1.00 for youth who had received an HIV or STI test and .83 for those who had not, with higher scores indicating greater depressive feelings.
Youth reported a substantial amount of risky drug use and sexual behavior. Fifteen percent of all youth in the sample reported having injected drugs in the last six months, with 21% of those who had taken an HIV/STI test reporting injection drug use compared with 12% of those who had not. Youth reported an average of 2.3 sexual partners in the last three months, with over 80% reporting that their sexual partners had risky sex with other partners in the last three months. About half of youth reported having at least one casual or need-based partner in the last three months, with 34% of youth who had received an HIV/STI test and 21% of those who had not reporting two or more. Over half of all youth believed that their sexual partners had risky sex with other people. With respect to service usage, two-thirds of the youth reported that they had used a drop-in center at least one time in the past 30 days. Seventy-six percent of those who had taken an HIV/STI test and received their results reported using a drop-in center compared with 58% of those who had not taken a test. Only about one-fifth of the youth in the study reported using a shelter in the past month, with 22% of youth who did not have an HIV/STI test and 22% of those who did reporting shelter use.
In bivariate models, factors significantly (p < .05) associated with increased odds of testing for HIV/STI in the past three months include self-identifying as gay (OR = 3.96, 95% CI = 1.32–11.89) and having been to a drop-in center in the past month (OR = 2.30, 95% CI = 1.32–3.98). Factors marginally associated (p < .10) with increased odds of being tested (and also included in the multivariable regression analysis) were older age (OR = 1.10, 95% CI = 0.99–1.23), Hispanic ethnicity (OR = 1.89, 95% CI = 0.91–3.93), more depressive symptoms (OR = 1.36, 95% CI = 0.97–1.91), injection drug use in the past six months (OR = 2.05, 95% CI = 0.97–4.34), and having two or more casual or need-based partners in the past three months (OR = 1.71, 95% CI = 0.92–3.18). Factors not associated with HIV/STI testing in bivariate models were gender, self-identification as bisexual, perceived susceptibility to HIV, being a “traveler,” number of sexual partners, unprotected sex with a casual or need-based partner, number of sexual partners perceived to be having risky sex, and shelter use in the last month.
Results of the multivariable logistic regression model are shown in Table 2. In this model, factors significantly associated with HIV/STI testing include Hispanic ethnicity (OR = 1.60, 95% CI = 1.00–2.96), self-identifying as gay (OR = 2.17, 95% CI = 1.15–5.02), and having injected drugs in the past 6 months (OR = 1.72, 95% CI = 1.08–2.74). Having depressive symptoms was marginally associated with HIV/STI testing in the multivariable regression model (OR = 1.21, 95% CI = 0.97–1.50) and thus was included in the path model. (Drop-in center use was not included in the multivariate model because it would interfere with our ability to evaluate it as a mediating factor.)
Table 2.
Bivariate and Multivariate Logistic Regression Models Predicting the Probability of Being Tested for HIV/STI (N = 305 Participants)
| Bivariate Logistic Regression Models | Multiple Logistic Regression Model | |||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| OR | 95% CI | P-value | OR | 95% CI | P-value | |||
| Demographic Characteristics | ||||||||
| Age | 1.10 | 0.99 | 1.23 | 0.08 | 1.05 | 0.98 | 1.13 | 0.20 |
| Male | 1.42 | 0.83 | 2.45 | 0.20 | ||||
| Race (ref = White) | ||||||||
| African American | 0.83 | 0.42 | 1.62 | 0.58 | 0.89 | 0.56 | 1.65 | 0.64 |
| Hispanic | 1.89 | 0.91 | 3.93 | 0.09 | 1.60 | 1.00 | 2.96 | 0.05 |
| Other | 1.08 | 0.52 | 2.26 | 0.83 | 1.12 | 0.69 | 2.12 | 0.57 |
| Level of education | 1.00 | 0.72 | 1.38 | 0.98 | ||||
| Sexual Orientation (ref = Heterosexual) | ||||||||
| Homosexual | 3.96 | 1.32 | 11.89 | 0.01 | 2.17 | 1.15 | 5.02 | 0.02 |
| Bisexual | 1.08 | 0.59 | 1.99 | 0.81 | 1.06 | 0.72 | 1.76 | 0.76 |
| Psychological Characteristics | ||||||||
| Depression Score | 1.36 | 0.97 | 1.91 | 0.08 | 1.21 | 0.97 | 1.50 | 0.09 |
| Percieved suceptibility to HIV | 0.88 | 0.67 | 1.14 | 0.33 | ||||
| Behavioral Characteristics | ||||||||
| Traveler | 1.03 | 0.59 | 1.79 | 0.93 | ||||
| Injected drugs in the past 6 months | 2.05 | 0.97 | 4.34 | 0.06 | 1.72 | 1.08 | 2.74 | 0.02 |
| Number of sex partners in the past 3 months | 1.06 | 0.96 | 1.17 | 0.24 | ||||
| Any unprotected sex with a casual or need-based partner | 1.07 | 0.59 | 1.93 | 0.83 | ||||
| Number of recent sex partners who were casual or need-based (ref = 0) | ||||||||
| 1 was casual or need-based | 0.77 | 0.40 | 1.48 | 0.44 | 0.84 | 0.55 | 1.47 | 0.42 |
| 2 or more were casual or need-based | 1.71 | 0.92 | 3.18 | 0.09 | 1.21 | 0.81 | 2.06 | 0.36 |
| Number of recent sex partners who respondent thinks had risky sex (ref = 0) | ||||||||
| 1–2 had risky sex | 1.12 | 0.52 | 2.44 | 0.77 | ||||
| 3 or more had risky sex | 1.07 | 0.52 | 2.21 | 0.86 | ||||
| Structural Characteristics | ||||||||
| Used a drop-in center the last month | 2.30 | 1.32 | 3.98 | 0.00 | ||||
| Stayed in a shelter in the last month | 1.00 | 0.55 | 1.79 | 0.99 | ||||
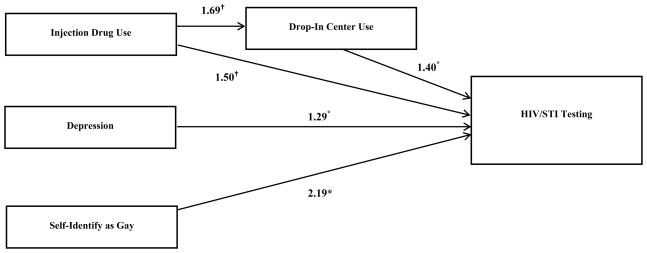
Results of the path model are shown in Figure 2. In this model, drop-in center use was significantly associated with HIV/STI testing (OR = 1.40, 95% CI = 1.13–1.75). There was a direct association between self-identifying as gay and HIV/STI testing (OR = 2.19, 95% CI = 1.25–3.86), but no indirect association involving drop-in center use (i.e., no evidence that drop-in center use mediated this relationship). Likewise, there was a direct association between depression and HIV/STI testing (OR = 1.29, 95% CI = 1.02–1.64), but no indirect association involving drop-in center use (i.e., no evidence of mediation). Injection drug use had a marginal direct association with HIV/STI testing (OR = 1.50, CI = 0.92–2.45) and a marginally significant indirect association with HIV/STI testing via its association with drop-in center use (OR = 1.69, CI = 0.98–2.90). We tested the significance of the indirect effect using a test provided by Goodman (L. A. Goodman, 1960) and found it to be marginally significant (z = 1.67, p = .09). Race/ethnicity was included in the path model because there was evidence of an association between this variable (being Hispanic in particular) and HIV/STI testing in the multiple regression model. Although we do not present this information in Figure 2, the direct association between Hispanic ethnicity and HIV/STI testing remained evident in this model (OR = 1.66, 95% CI = 1.04–2.65). Further, in the path model we also found an association between being Black and using a drop-in center (OR = 1.67, CI = 1.05–2.65), but no evidence that drop-in center use mediates the relationship between being Black and testing for HIV/STI.
Figure 2.
Path model showing direct and indirect (via drop-in center use) associations between HIV/STI testing, injection drug use, depression, and self-identification as gay. Only statistically significant (p. < 05)* or marginally significant (p<.10)† odds ratios are shown.
DISCUSSION
The present study sought to advance knowledge of factors related to HIV/STI testing in a sample of homeless youth in Los Angeles County. Consistent with our hypothesis, we found that youth were more likely to test if they engaged in injection drug use, self-identified as gay, experienced more depressive symptoms (marginally significant), and used drop-in center services. In addition, Hispanic youth were more likely to be tested for HIV/STI than white youth. However, contrary to expectations, HIV/STI testing was unrelated to engagement in high-risk sexual behaviors, feeling more susceptible to HIV, and staying in a homeless youth shelter or transitional housing. The associations of testing with self-identifying as gay (Solorio, Milburn, Weiss, et al., 2006) and injection drug use (E. Goodman & Berecochea, 1994) are consistent with previous research. However, to the best of our knowledge, this is the first study to document differences in HIV/STI testing among homeless youth by mental health status and drop-in center use, as well as the first to find that Hispanic youth (rather than Black or mixed-race youth) are more likely to take an HIV/STI test. Our expectations about the mediating role of drop-in center use were partially supported. Although the positive association between injection drug use and HIV/STI testing could be explained by injection drug users’ greater proclivity to use drop-in centers, the same was not true for the associations of testing with depressive symptoms or self-identifying as gay.
That drop-in center use is strongly associated with testing over and above other factors, and may mediate the association between other behavioral characteristics and testing, suggests the importance of considering structural factors in interventions to increase HIV/STI testing. We believe this finding to be particularly salient given that homeless youth often prefer to use drop-in centers over other services (e.g., shelters) because drop-in centers are perceived to pose fewer barriers (DeRosa et al., 1999). Among youth in this study who reported any past month drop-in center use, the average number of days used in the past month was 15.75, indicating that this is a steady source of assistance for many of these youth. In light of recent studies showing that a majority of adolescents in a community sample offered a free rapid HIV test were willing to take it (Swenson, Hadley, Houck, Dance, & Brown, 2011), and that increased availability of rapid testing methods and free testing services are among the factors most highly associated with increased acceptance of HIV testing in a general population of youth (Peralta, Deeds, Hipszer, & Ghalib, 2007), regularly offering free rapid testing at drop-in centers may be an effective way to encourage testing among homeless youth. Our findings also suggest that drop-in center use may mediate the relationship between injection drug use and HIV/STI testing. This relationship is logical given that injection drug users may be more in need of the variety of services provided by drop-in centers than other youth. Further, they may seek out drop-in centers in order to find HIV/STI testing.
While prior studies have suggested an association between depression and high-risk behaviors, none has found a direct association between depressive symptoms and HIV/STI testing. We expected that this association would be explained by more frequent use of drop-in centers, but this was not the case. Youth experiencing more depressive symptoms are not more likely to use drop-in centers than youth who are not depressed, but are in fact more likely to test. This may be explained by greater engagement in high-risk behaviors, such as substance use, among youth with more depressive symptoms (Tolou-Shams, et al., 2008), but further study is needed to better understand this association.
Our finding that Hispanic youth are more likely to test for HIV/STI than White youth differs from one prior study which found that Black and mixed race youth are more likely to test for STI than White or Hispanic youth (Solorio, Milburn, Weiss, et al., 2006). However, in that study the authors note that the Black youth were primarily older and thus may have more information about STI risk and the importance of testing. Thus, there may have been an interaction in that study between age and race/ethnicity, with older, Black youth more likely to test than younger youth of other racial and ethnic backgrounds, or a potential confounding of the two variables. That particular study also measured the likelihood of youth to test for STI over time, throughout a 24 month period. A similar study by the most of the same authors (Solorio, Milburn, Rotheram-Borus, et al., 2006) that measured testing at a single point in time among only those who had been sexually active in the past three months (compared with reporting ever having had sex at baseline or sexual activity within three months of any of the measurements) did not find differences by race or ethnicity, possibly suggesting that time on the street could also influence testing rates, that those who are more sexually active may have tested once but not again in the past three months, or that exposure to that study could have increased testing in certain groups. Last, the present study specifically asked about STI or HIV testing while Solario et al., in both studies, asked about STI testing only. Homeless youth may not include HIV as an STI test. Further study is needed to better understand potential cultural differences in HIV and STI testing among homeless youth.
Although our findings support some of our hypotheses and findings from prior studies, not all of the expected associations were found. For example, youth who reported greater sexual risk behaviors, such as having more casual or need-based partners, were not necessarily more likely to get tested or access services at a drop-in center. Similarly, testing was not more likely among those who felt more susceptible to HIV. More than one previous study has found that adolescents who report high-risk behaviors are no more likely to request STI testing than youth who do not engage in high-risk behaviors (Smith, Buzi, & Weinman, 2005; Solorio, Milburn, Rotheram-Borus, et al., 2006; Solorio, Milburn, Weiss, et al., 2006), so this finding has some precedence in the literature. Solario et al, (2006) suggest that the lack of association between high-risk sexual behaviors and testing could be due to some common STI’s, such as Chlamydia and genital herpes, being asymptomatic (Solorio, Milburn, Rotheram-Borus, et al., 2006). Thus, youth with high-risk sexual behaviors may not make a connection between their behavior, having an STI, and needing an STI test. An additional explanation could be that homeless youth in Los Angeles may not perceive their sexual behavior to be particularly risky. While injection drug users and gay youth seem to have gotten the message to get tested, other homeless youth may not be aware of their own susceptibility to HIV. Our findings show similar mean scores on the perceived susceptibility to HIV scale for those who did not get tested (M= 2.41) and those who did (M= 2.24). If homeless youth – including those with high-risk sexual behaviors – truly do not perceive themselves to be at high risk for HIV and other STI, there is a strong need for greater educational outreach and encouragement to test, beyond IDUs and gay youth.
CONCLUSIONS
Our study has several limitations. First, we did not ask whether youth were HIV or STI positive or negative; rather, we only asked them whether they had taken a test. In addition, when we asked about HIV and STI testing, we combined the two in a single question (i.e., we asked “when was your last HIV or STI test”), thus precluding an examination of similarities and differences in the predictors of each type of test. Finally, our findings may not generalize to youth in other geographic areas, such as those with few services specifically for homeless youth, or to those who are Spanish-speaking. Nevertheless, our study presents important new data on predictors of HIV/STI testing in homeless youth that have implications for encouraging more widespread testing. Specifically, the availability and accessibility of HIV and STI testing and/or messages about HIV and STI at venues frequented by homeless youth, such as drop-in centers, may be among the most important factors involved in a youth’s decision to get tested. Structural interventions that increase the accessibility of testing and reach out to youth who do not frequent these venues may be a fruitful direction for future research.
Footnotes
This research was supported by Grant R01DA020351 from National Institute on Drug Abuse. We thank Daniela Golinelli, PhD, of the RAND Corporation for her contributions to the study design. We also thank the youth who shared their experiences with us, the service agencies that collaborated in the study, and the RAND Survey Research Group for their assistance in data collection.
References
- Balaji AB, Eaton DK, Voetsch AC, Wiegand RE, Miller KS, Doshi SR. Association between HIV-related risk behaviors and HIV testing among high school students in the United States, 2009. Arch Pediatr Adolesc Med. 2012 doi: 10.1001/archpediatrics.2011.1131. [DOI] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic and statistical considerations. J Pers Soc Psychol. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Castilla J, del Romero J, Hernando V, Marincovich B, Garcia S, Rodriguez C. Effectiveness of highly active antiretroviral therapy in reducing heterosexual transmission of HIV. JAIDS 2005. 2005;40:96–101. doi: 10.1097/01.qai.0000157389.78374.45. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Revised recommendations for HIV testing of adults, adolescents, and pregnant women in health-care settings. MMWR. 2006;55:RR–14. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Effect of antiretroviral therapy on risk of sexual transmission of HIV infection and super infection. 2009 from http://www.cdc.gov/hiv/topics/treatment/resources/factsheets/pdf/art.pdf.
- De Rosa CJ, Montgomery SB, Kipke MD, Iverson E, Ma JL, Unger JB. Service utilization among homeless and runaway youth in Los Angeles, California: rates and reasons. J Adolesc Health. 1999;24(6):449–458. doi: 10.1016/s1054-139x(99)00040-3. [DOI] [PubMed] [Google Scholar]
- DiClemente RJ. Epidemiology of AIDS, HIV prevalence, and HIV incidence among adolescents. J Sch Health. 1992;62(7):325–330. doi: 10.1111/j.1746-1561.1992.tb01251.x. [DOI] [PubMed] [Google Scholar]
- Goodman E, Berecochea JE. Predictors of HIV testing among runaway and homeless adolescents. J Adolesc Health. 1994;15(7):566–572. doi: 10.1016/1054-139x(94)90140-x. [DOI] [PubMed] [Google Scholar]
- Goodman LA. On the exact variance of products. Journal of the American Statistical Association. 1960;55:708–713. [Google Scholar]
- Gwadz MV, Cleland CM, Quiles R, Nish D, Welch J, Michaels LS, et al. CDC HIV testing guidelines and the rapid and conventional testing practices of homeless youth. AIDS Educ Prev. 2010;22(4):312–327. doi: 10.1521/aeap.2010.22.4.312. [DOI] [PubMed] [Google Scholar]
- Janz N, Champion J, Strecher V. The Health Belief Model. In: Glanz K, Rimer B, Marcus Lewis F, editors. Health Behavior and Health Education: Theory, Practice, Research. San Francisco: Jossey-Bass; 2002. [Google Scholar]
- Luna GC, Rotheram-Borus MJ. Street youth and the AIDS pandemic. AIDS Educ Prev. 1992;(Suppl):1–13. [PubMed] [Google Scholar]
- Marks G, Crepaz N, Janssen RS. Estimating sexual transmission of HIV from persons aware and unaware that they are infected with the virus in the USA. AIDS. 2006;20(10):1447–1450. doi: 10.1097/01.aids.0000233579.79714.8d. [DOI] [PubMed] [Google Scholar]
- Melchior LA, Huba GJ, Brown VB, Reback CJ. A short depression index for women. Educ Psychol Meas. 1993;53(4):1117–1125. [Google Scholar]
- Ober AJ, Iguchi MY, Weiss RE, Gorbach PM, Heimer R, Ouellet LJ, et al. The relative role of perceived partner risks in promoting condom use in a three-city sample of high-risk, low-income women. AIDS Behav. 2010 doi: 10.1007/s10461-010-9840-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peralta L, Deeds BG, Hipszer S, Ghalib K. Barriers and facilitators to adolescent HIV testing. AIDS Patient Care STDS. 2007;21(6):400–408. doi: 10.1089/apc.2006.0112. [DOI] [PubMed] [Google Scholar]
- Pfeifer RW, Oliver J. A study of HIV seroprevalence in a group of homeless youth in Hollywood, California. J Adolesc Health. 1997;20(5):339–342. doi: 10.1016/S1054-139X(97)00038-4. [DOI] [PubMed] [Google Scholar]
- Smith PB, Buzi RS, Weinman ML. HIV testing and counseling among adolescents attending family planning clinics. AIDS Care. 2005;17(4):451–456. doi: 10.1080/09540120412331291788. [DOI] [PubMed] [Google Scholar]
- Solorio MR, Milburn NG, Rotheram-Borus MJ, Higgins C, Gelberg L. Predictors of sexually transmitted infection testing among sexually active homeless youth. AIDS Behav. 2006;10(2):179–184. doi: 10.1007/s10461-005-9044-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solorio MR, Milburn NG, Weiss RE, Batterham PJ. Newly homeless youth STD testing patterns over time. J Adolesc Health. 2006;39(3):443.e449–443.e416. doi: 10.1016/j.jadohealth.2005.12.017. [DOI] [PubMed] [Google Scholar]
- Sweeney P, Lindegren ML, Buehler JW, Onorato IM, Janssen RS. Teenagers at risk of human immunodeficiency virus type 1 infection. Results from seroprevalence surveys in the United States. Arch Pediatr Adolesc Med. 1995;149(5):521–528. doi: 10.1001/archpedi.1995.02170180051007. [DOI] [PubMed] [Google Scholar]
- Swenson RR, Hadley WS, Houck CD, Dance SK, Brown LK. Who accepts a rapid HIV antibody test? The role of race/ethnicity and HIV risk behavior among community adolescents. J Adolesc Health. 2011;48(5):527–529. doi: 10.1016/j.jadohealth.2010.08.013. [DOI] [PubMed] [Google Scholar]
- Tolou-Shams M, Brown LK, Houck C, Lescano CM. The association between depressive symptoms, substance use, and HIV risk among youth with an arrest history. J Stud Alcohol Drugs. 2008;69(1):58–64. doi: 10.15288/jsad.2008.69.58. [DOI] [PubMed] [Google Scholar]
- Tyler K, Melander L. The effect of drug and sexual risk behaviors with social network and non-network members on homeless youths’ sexually transmissible infections and HIV testing. Sex Health. 2010;7(4):434–440. doi: 10.1071/SH09113. [DOI] [PubMed] [Google Scholar]
- Venkatesh KK, van der Straten A, Cheng H, Montgomery ET, Lurie MN, Chipato T, et al. The relative contribution of viral and bacterial sexually transmitted infections on HIV acquisition in southern African women in the Methods for Improving Reproductive Health in Africa study. Int J STD AIDS. 2011;22(4):218–224. doi: 10.1258/ijsa.2010.010385. [DOI] [PubMed] [Google Scholar]
- Walters AS. HIV prevention in street youth. J Adolesc Health. 1999;25(3):187–198. doi: 10.1016/s1054-139x(98)00155-4. [DOI] [PubMed] [Google Scholar]
- Young SD, Rice E. Online social networking technologies, HIV knowledge, and sexual risk and testing behaviors among homeless youth. AIDS Behav. 2011;15(2):253–260. doi: 10.1007/s10461-010-9810-0. [DOI] [PMC free article] [PubMed] [Google Scholar]