Abstract
Study Design
Retrospective review of the data collected prospectively through the Spine Patient Outcomes Research Trial (SPORT).
Objective
Determine the effect that race or ethnicity had on outcomes following spine surgery in the three arms of SPORT.
Summary of Background Data
There is a dearth of research regarding the effect of race or ethnicity on outcome following treatment for spinal disorders.
Methods
All participants from the three arms of the SPORT were evaluated in an as-treated analysis with patients categorized as white, black, or other. Baseline and operative characteristics of the groups were compared using the chi-square test and ANOVA. Differences in the changes between baseline and 1-, 2-, 3-, and 4-year time-points in the operative and non-operative treatments were evaluated with a mixed effects longitudinal regression model and differences between racial groups were compared with a multiple degrees of freedom Wald test.
Results
Included were 2,427 patients (85% white, 8% black, 7% other). Surgery was performed on 67% of white patients, 54% of blacks, and 68% of others. Whites and others were significantly more likely to undergo surgery than blacks (67% and 68% vs 54%, p=0.003). Complications and the risk of additional surgeries were not significantly different between racial groups. Regardless of race, all patients improved more with surgical management than with nonoperative treatment for all outcome measures at all time-points. The average 4-year area- under-the-curve results revealed surgical and non-operative treatment resulted in statistically significant improvement in whites relative to blacks for BP (p<0.001), SF (p<0.001), and ODI (p<0.001). No significant differences were appreciated in treatment effect for primary outcome measures or self-rated progress across racial groups.
Conclusion
These results illustrate important differences between racial groups in terms of response to spine care. While there were quantitative differences between groups, these findings are not necessarily indications of healthcare disparities.
Keywords: spine surgery, race, ethnicity, outcome, healthcare disparities
INTRODUCTION
Concerns regarding access to care and the disparate treatment of patients because of their race or ethnicity have existed within the medical community since the start of the twentieth century. Indeed, a number of well-known studies have demonstrated disparities in the quality and efficacy of healthcare offered to racial and ethnic minorities.1-6 These have included diminished rates of cardiac pacer implantation5, coronary artery bypass grafting3, aortic valve replacement1,7, and organ transplantation for black patients relative to whites7. While many of these interventions are accepted as the standard of care for their respective conditions and would not be expected to vary among different populations8,9, orthopaedic procedures enjoy less well-defined procedural efficacy and may show greater variation among those with reduced access to healthcare2,8,9.
Not surprisingly, previous research has highlighted substantial variation in terms of the types of orthopaedic services available to racial and ethnic minorities, as well as inferior outcomes and an increased risk of complications.6,10,11,12 Of note, most prior studies have focused on the field of joint arthroplasty10,11,12 and comparatively little work has been conducted with respect to the effect of race, ethnicity, or socioeconomic status on outcomes, morbidity, or mortality following elective spine surgery.
The limited available research, however, suggests inequalities in spine care for minority groups similar to that encountered in other fields of medicine.6,7,13,14,15 With respect to outcomes, prior works have reported that black patients are at greater risk of morbidity and mortality following spine surgery13,16,17. While such studies highlight concern in the current healthcare environment, it is important to recognize that most were conducted in a retrospective fashion and many relied on patient samples or large databases compiled for purposes other than spine treatment outcomes. To the best of our knowledge, only one previous clinical investigation has specifically sought to evaluate outcomes for racial or ethnic minorities undergoing spine surgery.13
The goal of the current study was to use the prospectively collected, patient-focused data from the *** (***) to evaluate the effect that race or ethnicity has on outcomes following spine surgery. As a National Institutes of Health (NIH) funded study, the recruitment of minorities into the investigational cohort was deemed a priority from its inception. Moreover, the *** clinical sites were specifically selected in order to provide an ethnically, racially, and socioeconomically diverse population. Taking advantage of these features, it was anticipated that the data available from the *** would be able to provide high quality evidence regarding the influence of race and ethnicity on outcomes following common spine surgical interventions.
MATERIALS AND METHODS
Patient Population
The methodology of the *** investigations has been previously described in detail.18-23 In brief, this prospective study was conducted between 2000 and 2005 at 13 medical centers in 11 states across the U.S. The investigation was approved by the investigational review boards at all participating institutions. Three arms of the trial existed, one for intervertebral disc herniation (IDH)21, another for spinal stenosis (SpS)23, and a third for degenerative spondylolisthesis (DS)22. Patients who met the inclusion criteria were invited to enroll in the randomized portion of the study, where operative or non-operative management was assigned at random. Those individuals who refused randomization received the intervention mutually agreed upon by the patient and their physician, and were followed in the observational cohort of the study. Patients were followed for a period of 4 years following enrollment in the investigation.
Within the IDH arm, surgical intervention consisted of a standard open discectomy, while open laminectomy was performed for SpS and decompressive laminectomy and fusion with autogenous iliac crest bone graft was typically carried out for those with DS. In instances of lumbar fusion, the choice of whether or not to use pedicle screw instrumentation was left to the discretion of the treating surgeon. In all three arms of the ***, non-operative management was individualized to each patient but consisted of education, physical therapy, and non-steroidal anti-inflammatory drugs at a minimum.
Race and ethnicity were recorded by patient self-report in the baseline survey of the ***. Individuals had the opportunity to select from one of eight ethnic/racial categories. For the purposes of this investigation, due to limited patient numbers in certain ethnic/racial groups, patients were grouped into one of three classifications: white (White race, not-Hispanic or Latino), black (Black race/African-American, not-Hispanic or Latino) and other (Hispanic or Latino, Native American/Alaskan, Asian, Native Hawaiian/Pacific Islander, more than one race reported).
Study Measures
The data employed in this investigation was obtained from the patient questionnaires completed at baseline, and at the 6-week, 3-month, 6-month, 1-, 2-, 3-, and 4-year time-points following enrollment. Data included the SF-36 bodily pain (BP) score, the SF-36 physical function (PF) score, the SF-36 mental component summary (MCS), physical component score (PCS), the Oswestry Disability Index (ODI), the Sciatica/Stenosis Bothersomeness Index, patient-rated level of satisfaction, and self-rated progress. The ODI and SF-36 subscales range from 0-100, and the Sciatica/Stenosis Bothersomeness Index ranges from 0-24. Higher scores on the SF-36 subscales are indicative of less severe symptoms, while higher scores on the ODI and Sciatica/Stenosis Bothersomeness Index represent more severe symptomatology. For the purposes of this investigation, patient satisfaction and self-rated progress were graded as the percentage of individuals somewhat, or very satisfied with their symptoms and percent reporting major improvement from baseline, respectively.
Additionally, for patients who underwent surgical intervention, operative characteristics such as operative time, intra-operative blood loss, and complications were recorded. Post-operative morbidity, mortality, and subsequent surgeries were also captured.
STATISTICAL ANALYSIS
The *** design initially intended for both randomized and observational cohorts within each arm of the study. However, as outlined in previous publications21-23, there was a high-degree of cross-over between treatment groups within the randomized cohort of all three study arms. Therefore, in this investigation, data from both the randomized and observational cohorts of the three *** studies were combined in an as-treated analysis. The scientific rationale behind the as-treated analysis has been explained in previous works.20
The baseline characteristics of the white, black, and other racial groups were compared using the chi-square test for categorical variables and ANOVA for continuous data. Primary analysis compared changes from baseline at each follow-up in the primary outcome measures for operative and non-operative treatment between the racial groups with a mixed effects longitudinal regression model including a random individual effect to account for correlation between repeated measurements within individuals. The treatment effect of surgery was also compared between racial groups using the formula:
Treatment group was determined by the actual treatment received by each patient at each time-point in the analysis. In this as-treated analysis, the treatment indicator was a time-varying covariate, allowing for variable times of surgery. Data collected on patients prior to undergoing surgery is included in the non-operative estimate with follow-up time measured from enrollment. Data collected on patients following surgical intervention is included in the operative estimate and follow-up represents the time from surgery. Repeated measures of outcomes were used as the dependent variables, and treatment received was included as a time-varying covariate. To adjust for potential confounding, baseline variables associated with missing data or treatment received were included as adjusting covariates in longitudinal regression models. In addition, age, gender, diagnosis, center, and baseline outcome scores (for SF36 and ODI) were included in longitudinal regression models. Secondary and binary outcomes were analyzed using generalized estimating equations (GEEs) that assumed a compound symmetry working correlation structure. The outcomes were stratified by race and outcomes between these sub-groups at each time-point were compared using a multiple degrees of freedom Wald test. Across the four-year follow-up, overall comparisons of area-under-curve between these sub-groups were made using a Wald test.
In all statistical considerations, significance was determined a-priori as p <0.05 on the basis of a 2-sided hypothesis test with no adjustments made for multiple comparisons. Computations were performed using SAS version 9.2 (SAS Institute Inc., Cary, NC) with the SAS PROC MIXED and PROC GENMOD procedures employed for continuous data with normal random effects and non-normal outcomes, respectively.
Source of Funding
The *** investigation was supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases (U01-AR45444) and the Office of Research on Women’s Health, the National Institutes of Health, and the National Institute of Occupational Safety and Health, the Centers for Disease Control and Prevention.
RESULTS
Patient Population
In total, 2,427 patients were included for analysis in this investigation (Table 1). Eighty-five percent of the cohort (n = 2,072) were white, 8% (n = 188) were black, and 7% (n = 167) were other (i.e. non-white, non-black). The surgical group was ultimately comprised of 1,593 patients (66%), with the remainder having received non-operative management exclusively. Eighty-seven percent (n = 1,378) of the surgical group was white, with 6% (n = 102) of the group composed of blacks and 7% (n = 113) consisting of other. Within the racial categories, surgery was performed on 67% of white patients, 54% of blacks, and 68% of others. Surgical information was available for 1,367 white, 101 black, and 112 other patients who received surgery and specific procedural information was accessible for 1,350 white, 98 black, and 111 other individuals.
Table 1.
Patient Baseline Demographic Characteristics, Comorbid Conditions, Clinical Findings, and Health Status Measures.
| Characteristics | White (n=2072) |
Black (n=188) |
Other (n=167) |
p-value |
|---|---|---|---|---|
| Mean Age (SD) | 53.9 (16.4) | 54.2 (13.8) | 50.8 (16.6) | 0.052 |
| Female - no. (%) | 977 (47%) | 118 (63%) | 73 (44%) | <0.001 |
| Ethnicity: Not Hispanic† | 2045 (99%) | 185 (98%) | 99 (59%) | <0.001 |
| Education - At least some college | 1456 (70%) | 111 (59%) | 118 (71%) | 0.006 |
| Income - Under $50,000 | 669 (32%) | 69 (37%) | 56 (34%) | 0.45 |
| Marital Status - Married | 1474 (71%) | 100 (53%) | 103 (62%) | <0.001 |
| Work Status | <0.001 | |||
| Full or part time | 979 (47%) | 69 (37%) | 64 (38%) | |
| Disabled | 208 (10%) | 32 (17%) | 29 (17%) | |
| Other | 885 (43%) | 87 (46%) | 73 (44%) | |
| Compensation - Any‡ | 227 (11%) | 30 (16%) | 40 (24%) | <0.001 |
| Mean Body Mass Index (BMI), (SD)§ | 28.5 (5.8) | 31 (5.9) | 28.6 (4.8) | <0.001 |
| Smoker | 328 (16%) | 42 (22%) | 25 (15%) | 0.061 |
| Comorbidities - no. (%) | ||||
| Hypertension | 589 (28%) | 94 (50%) | 43 (26%) | <0.001 |
| Depression | 269 (13%) | 26 (14%) | 14 (8%) | 0.21 |
| Diabetes | 170 (8%) | 33 (18%) | 21 (13%) | <0.001 |
| Joint Problem | 763 (37%) | 88 (47%) | 60 (36%) | 0.023 |
| Stomach Problem | 344 (17%) | 36 (19%) | 34 (20%) | 0.34 |
| Time since recent episode < 6 months | 1233 (60%) | 109 (58%) | 94 (56%) | 0.68 |
| SF-36 scores, mean (SD)†† | ||||
| Bodily Pain (BP) | 30.9 (20) | 25.5 (17.3) | 28.9 (21.7) | 0.001 |
| Physical Functioning (PF) | 37 (24.3) | 29 (22) | 33.5 (25) | <0.001 |
| Mental Component Summary (MCS) | 47.8 (11.7) | 45.7 (12.6) | 44.9 (12.1) | <0.001 |
| Physical Component Summary (PCS) |
30.3 (8.5) | 27.9 (8) | 29.9 (8.9) | 0.001 |
| Oswestry (ODI) (SD)‡‡ | 45.2 (20.2) | 47.7 (19.4) | 48.6 (20) | 0.039 |
| Sciatica/Stenosis Frequency Index (0- 24) (SD)§§ |
14.7 (5.6) | 15.6 (5.6) | 15.7 (6) | 0.022 |
| Sciatica/Stenosis Bothersome Index (0- 24) (SD)§§ |
14.9 (5.5) | 16.1 (5.6) | 15.9 (5.6) | 0.001 |
| Satisfaction with symptoms - very dissatisfied |
1543 (74%) | 137 (73%) | 123 (74%) | 0.87 |
| Patient self-assessed health trend - no. (%) |
0.76 | |||
| Getting better | 225 (11%) | 19 (10%) | 19 (11%) | |
| Staying about the same | 802 (39%) | 65 (35%) | 64 (38%) | |
| Getting worse | 1025 (49%) | 103 (55%) | 83 (50%) | |
| Treatment preference at baseline - no. (%) |
<0.001 | |||
| Preference for non-surg | 719 (35%) | 87 (46%) | 52 (31%) | |
| Not sure | 382 (18%) | 43 (23%) | 30 (18%) | |
| Preference for surgery | 967 (47%) | 58 (31%) | 84 (50%) | |
| Diagnosis - no. (%) | 0.034 | |||
| IDH | 1033 (50%) | 75 (40%) | 84 (50%) | |
| SPS | 533 (26%) | 52 (28%) | 49 (29%) | |
| DS | 506 (24%) | 61 (32%) | 34 (20%) | |
| Pain Radiation - no. (%) | 1815 (88%) | 166 (88%) | 148 (89%) | 0.90 |
| Straight Leg Raise Test - Ipsilateral | 760 (37%) | 65 (35%) | 58 (35%) | 0.76 |
| Straight Leg Raise Test - Contralateral/Both |
201 (10%) | 10 (5%) | 18 (11%) | 0.12 |
| Any Neurological Deficit | 1353 (65%) | 111 (59%) | 114 (68%) | 0.15 |
| Reflexes - Asymmetric Depressed | 712 (34%) | 42 (22%) | 45 (27%) | <0.001 |
| Sensory - Asymmetric Decrease | 809 (39%) | 68 (36%) | 77 (46%) | 0.13 |
| Motor - Asymmetric Weakness | 714 (34%) | 53 (28%) | 57 (34%) | 0.22 |
| Herniation Level | 0.47 | |||
| L2-L3 / L3-L4 | 78 ( 4%) | 6 ( 3%) | 4 ( 2%) | |
| L4-L5 | 401 (19%) | 22 (12%) | 33 (20%) | |
| L5-S1 | 554 (27%) | 47 (25%) | 46 (28%) | |
| Herniation Type | 0.26 | |||
| Protruding | 272 (13%) | 27 (14%) | 23 (14%) | |
| Extruded | 682 (33%) | 46 (24%) | 55 (33%) | |
| Sequestered | 79 ( 4%) | 2 ( 1%) | 5 ( 3%) | |
| Posterolateral herniation | 798 (39%) | 55 (29%) | 66 (40%) | 0.039 |
| Pseudoclaudication - Any | 985 (48%) | 111 (59%) | 83 (50%) | 0.01 |
| SLR or Femoral Tension | 1028 (50%) | 79 (42%) | 80 (48%) | 0.13 |
| Listhesis Level | 0.15 | |||
| L3-L4 | 53 ( 3%) | 2 ( 1%) | 2 ( 1%) | |
| L4-L5 | 453 (22%) | 59 (31%) | 32 (19%) | |
| Stenosis Levels | ||||
| L2-L3 | 207 (10%) | 7 (4%) | 18 (11%) | 0.017 |
| L3-L4 | 561 (27%) | 49 (26%) | 46 (28%) | 0.94 |
| L4-L5 | 976 (47%) | 105 (56%) | 78 (47%) | 0.068 |
| L5-S1 | 192 (9%) | 21 (11%) | 17 (10%) | 0.66 |
| Stenotic Levels (Mod/Severe) | 0.032 | |||
| None | 28 ( 1%) | 7 ( 4%) | 3 ( 2%) | |
| One | 503 (24%) | 63 (34%) | 38 (23%) | |
| Two | 350 (17%) | 37 (20%) | 26 (16%) | |
| Three+ | 158 ( 8%) | 6 ( 3%) | 16 (10%) | |
| Stenosis Locations | ||||
| Central | 927 (45%) | 91 (48%) | 74 (44%) | 0.62 |
| Lateral Recess | 883 (43%) | 94 (50%) | 72 (43%) | 0.15 |
| Neuroforamen | 385 (19%) | 43 (23%) | 22 (13%) | 0.063 |
| Stenosis Severity | 0.36 | |||
| Mild | 28 ( 1%) | 7 ( 4%) | 3 ( 2%) | |
| Moderate | 420 (20%) | 43 (23%) | 34 (20%) | |
| Severe | 591 (29%) | 63 (34%) | 46 (28%) | |
| Instability | 35 (2%) | 6 (3%) | 6 (4%) | 0.098 |
| Received surgery* | 1378 (67%) | 102 (54%) | 113 (68%) | 0.003 |
Race or ethnic group was self-assessed. Whites and blacks could be either Hispanic or non-Hispanic.
This category includes patients who were receiving or had applications pending for workers compensation, Social Security compensation, or other compensation.
The body-mass index is the weight in kilograms divided by the square of the height in meters.
The SF-36 scores range from 0 to 100, with higher score indicating less severe symptoms.
The Oswestry Disability Index ranges from 0 to 100, with lower scores indicating less severe symptoms.
The Sciatica Bothersomeness index and Sciatica Frequency index range from 0 to 24, with lower scores indicating less severe symptoms.
Low Back Pain Bothersomness Scale ranges from 0 to 6, with lower scores indicating less severe symptoms.
Patients received surgery were classified according to whether they received surgical treatment during the first 4 years of enrollment.
Comparison of Baseline Characteristics
The initial comparison of baseline patient demographics, medical co-morbidities, clinical findings, and health status measures revealed several differences between racial groups (Table 1). Females composed a larger percentage of the black cohort relative to whites and others (p <0.001). Blacks were also less likely to be married (p<0.001), to be employed (p<0.001), and to have some degree of college education (p=0.006). Mean age (p=0.052) and income (p=0.45) were not different between racial groups, but blacks and others were more likely to be receiving or have applications pending for worker’s compensation, Social Security compensation, or other compensation programs (p<0.001).
In terms of medical co-morbidities, Body Mass Index (BMI) was higher among black patients relative to whites and others (p<0.001). Blacks were also more likely to suffer from hypertension (p<0.001), diabetes (p<0.001), and to report a history of joint problems (p=0.023). A trend was noted for blacks to report a history of smoking (p=0.061) (Table 1).
Diagnosis at baseline was significantly different between racial groups (p=0.034) with blacks having a greater percentage of individuals with DS, and fewer IDH patients relative to whites and others (32% vs. 24% and 20% and 40% vs. 50% and 50%, respectively) (Table 1). A statistically significant difference in baseline SF-36 BP (p=0.001), PF (p<0.001), MCS (p<0.001), PCS (p=0.001), ODI (p=0.039) and Sciatica/Stenosis Bothersomeness Index (p=0.001) was also noted with blacks and others reporting more severe symptoms and reduced functionality relative to whites. No significant difference between groups was appreciated for satisfaction with symptoms at baseline (p=0.87), with the vast majority of patients across all races reporting that they were ‘very dissatisfied’ with symptoms. As reported previously24, there was a significant difference in terms of preference for surgery at baseline, with the plurality of black patients (46%, p<0.001) expressing a preference for non-surgical management. Whites and others were significantly more likely to receive surgery relative to blacks (p=0.003).
Comparison of Operative Characteristics
The surgical procedures performed between racial groups were significantly different (p=0.004), with whites and others undergoing more stand-alone decompression procedures (74% and 75% of the cohorts, respectively), while the highest percentage of instrumented fusions (33%) were performed in blacks (Table 2). This was expected, however, given the higher prevalence of spondylolisthesis among black patients. Operative times were significantly increased in blacks and others (p=0.003), as was intra-operative blood loss (p=0.001). This may also be attributed to the increased rate of arthrodesis procedures performed for spondylolisthesis within this group.
Table 2.
Operative characteristics, post-operative complications/events, and mortality.
| Characteristics | White (n=1367)* |
Black (n=101)* |
Other (n=112)* |
p-value |
|---|---|---|---|---|
| Procedure - no. (%) | 0.004 | |||
| Decompression only | 997 (74%) | 65 (66%) | 83 (75%) | |
| Non-instrumented fusion | 98 ( 7%) | 1 ( 1%) | 5 ( 5%) | |
| Instrumented fusion | 255 (19%) | 32 (33%) | 23 (21%) | |
| Discectomy Level | ||||
| L2-L3 | 15 (2%) | 1 (2%) | 0 (0%) | 0.54 |
| L3-L4 | 31 (4%) | 1 (2%) | 3 (5%) | 0.71 |
| L4-L5 | 311 (42%) | 19 (39%) | 23 (39%) | 0.80 |
| L5-S1 | 400 (54%) | 31 (63%) | 33 (56%) | 0.48 |
| Multi-level fusion | 99 (7%) | 3 (3%) | 7 (6%) | 0.25 |
| Laminectomy Level | ||||
| L2-L3 | 165 (22%) | 11 (16%) | 17 (29%) | 0.23 |
| L3-L4 | 412 (55%) | 31 (46%) | 38 (64%) | 0.10 |
| L4-L5 | 676 (89%) | 62 (91%) | 54 (92%) | 0.80 |
| L5-S1 | 277 (37%) | 17 (25%) | 17 (29%) | 0.083 |
| Levels decompresssed | 0.12 | |||
| 0 | 611 (45%) | 33 (33%) | 53 (47%) | |
| 1 | 288 (21%) | 32 (32%) | 20 (18%) | |
| 2 | 233 (17%) | 21 (21%) | 19 (17%) | |
| 3+ | 235 (17%) | 15 (15%) | 20 (18%) | |
| Operation time, minutes (SD) | 119.3 (77.9) | 144.9 (90.4) | 132.8 (81.3) | 0.003 |
| Blood loss, cc (SD) | 241 (351.9) | 336.4 (422.9) | 348.3 (614.2) | 0.001 |
| Blood Replacement - no. (%) | ||||
| Intraoperative replacement | 146 (11%) | 18 (18%) | 12 (11%) | 0.086 |
| Post-operative transfusion | 86 (6%) | 9 (9%) | 6 (5%) | 0.50 |
| Days of hospital stay (SD)** | 2.4 (2.7) | 3 (2.2) | 2.6 (2.1) | 0.10 |
| Intraoperative complications§ | ||||
| Dural tear/ spinal fluid leak | 81 (6%) | 8 (8%) | 13 (12%) | 0.053 |
| Nerve root injury | 2 (0%) | 0 (0%) | 0 (0%) | 0.86 |
| Vascular injury | 1 (0%) | 0 (0%) | 0 (0%) | 0.92 |
| Other | 13 (1%) | 2 (2%) | 0 (0%) | 0.33 |
| None | 1271 (93%) | 91 (90%) | 99 (88%) | 0.11 |
| Postoperative complications/events¶ | ||||
| Nerve root injury | 2 (0%) | 0 (0%) | 0 (0%) | 0.86 |
| Wound hematoma | 8 (1%) | 1 (1%) | 0 (0%) | 0.61 |
| Wound Infection | 32 (2%) | 3 (3%) | 3 (3%) | 0.90 |
| Other | 76 (6%) | 7 (7%) | 4 (4%) | 0.53 |
| None | 1171 (86%) | 82 (83%) | 100 (89%) | 0.39 |
| Post-operative mortality (death within 6 weeks of surgery) |
2 (0.1%) | 0 (0%) | 0 (0%) | 0.14 |
| Post-operative mortality (death within 3 months of surgery) |
2 (0.1%) | 1 (0.1%) | 1 (0.1%) | 0.78 |
| Additional surgeries (1-year rate)∥ | 80 (6%) | 9 (9%) | 3 (3%) | 0.15 |
| Additional surgeries (2-year rate)∥ | 122 (9%) | 13 (13%) | 8 (7%) | 0.31 |
| Additional surgeries (3-year rate)∥ | 146 (11%) | 14 (14%) | 10 (9%) | 0.47 |
| Additional surgeries (4-year rate)∥ | 169 (12%) | 15 (15%) | 10 (9%) | 0.39 |
| Recurrent disc herniation/stenosis/progressive listhesis |
86 (6%) | 6 (6%) | 5 (4%) | |
| Pseudarthrosis / fusion exploration | 3 (0.2%) | 0 | 2 (1.8%) | |
| Complication or Other | 50 (4%) | 5 (5%) | 4 (4%) | |
| New condition | 25 (2%) | 2 | (2%) 0 |
Surgical information was available for 1367 white, 101 black and 112 other. Specific procedure information was available on 1350 white, 98 black and 111 other.
None of the following were reported: aspiration, operation at wrong level.
Any reported complications up to 8 weeks post operation. None of the following were reported: bone graft complication, CSF leak, paralysis, cauda equina injury, wound dehiscence, pseudarthrosis.
One-, two-, three- and four-year post-surgical re-operation rates are Kaplan Meier estimates and p-values are based on the log-rank test. Numbers and percentages are based on the first additional surgery if more than one additional surgery.
One patient in the white race group had a length of hospital stay of 372 days—not counting that case the average length of hospital stay for the white group would be 2.4 (2.7).
A trend was noted (p=0.053) for others to have a greater likelihood of incidental durotomy during the surgical procedure, but this value did not reach significance. Blacks were not found to be at a greater risk of intra-operative complications, post-operative morbidity or mortality, or additional surgeries (Table 2). The racial category of other was also not found to be at greater risk for post-operative morbidity, mortality, or additional surgeries (Table 2).
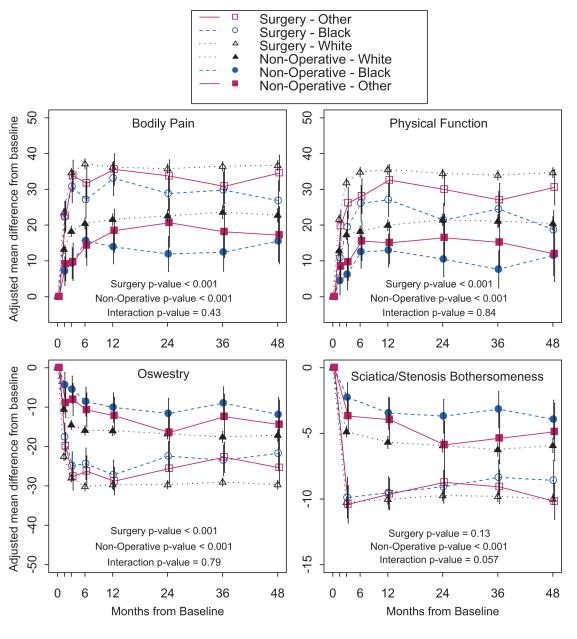
Comparison of Outcomes
Regardless of racial classification, all patients improved more with surgical management than with non-operative treatment for all outcome measures at all time-points in the study. Irrespective of treatment intervention, however, white patients reported better results than black patients, with significant differences appreciated for PF at every time-point in the study (Figure 1). Significant differences for surgical intervention in BP were encountered at 2-, 3- and 4-year time-points and significant differences for non-operative management were appreciated at all evaluations (Figure 1). Similarly, there was a significant difference for surgical intervention for ODI between whites and blacks at 2-, 3-, and 4-year evaluations, with significant differences in non-operative treatment identified at all time-points. The greatest difference between whites and blacks were encountered for the SF-36 BP and PF in the surgically treated groups at the 4-year time-point [36.7 vs. 26.8 (p=0.003) and 34.7 vs. 18.7 (p<0.001), respectively).
Figure 1.
Primary outcomes over time for race White, Black and Other
Interestingly, no significant differences in treatment effect were appreciated at the 3-year time-point except for the MCS. Here there was a significant difference between whites and blacks, with surgical intervention showing a significant improvement among blacks due to poor outcomes in MCS for the black non-operative group. Additionally, there were no differences that reached significance for patient satisfaction [treatment effect for whites 31.1% (26%, 36.3%) vs. 28.5% (11.2%, 45.9%) for blacks, p=0.97], or self-rated progress [treatment effect for whites 34% (28.9%, 39.2%) vs. 41.3 % (25.2%, 57.3%) for blacks, p=0.67], across racial groups at the 4-year time-point.
In the average over 4-year area-under-the-curve results surgical and non-operative treatment resulted in statistically significant improvement in whites relative to blacks for the SF-36 BP, PF, and ODI (Table 3). Once again, there was no significant difference in treatment effect, except for an advantage for surgery among black patients in the SF-36 MCS that was due to low average scores in this criterion for blacks who received non-operative management.
Table 3.
Average over four years area under the curve results (per year) from adjusted as-treated outcome analysis by race for the randomized and observational cohorts combined SPORT patients.
| Race | Surgical | Non- operative |
Treatment Effect† (95% CI) |
|
|---|---|---|---|---|
| SF-36 Bodily Pain (BP) (0-100) (SE) |
White | 35.2 (0.5) | 21.6 (0.6) | 13.6 (12.3, 14.9) |
| Black | 28.8 (1.7) | 12.7 (1.7) | 16.1 (12.2, 20) | |
| Other | 32.3 (1.6) | 17.4 (2.2) | 15 (10.3, 19.6) | |
| p-value | <0.001 | <0.001 | 0.43 | |
|
| ||||
| SF-36 Physical Function (PF) (0-100) (SE) |
White | 33.4 (0.5) | 19.8 (0.6) | 13.6 (12.4, 14.9) |
| Black | 22.5 (1.7) | 10 (1.7) | 12.6 (8.7, 16.4) | |
| Other | 28.6 (1.7) | 14.4 (2.2) | 14.2 (9.7, 18.7) | |
| p-value | <0.001 | <0.001 | 0.84 | |
|
| ||||
| SF-36 Mental Component Summary (MCS) (0-100) (SE) |
White | 4.8 (0.2) | 3.2 | (0.2) 1.6 (1, 2.1) |
| Black | 3.9 (0.7) | 0 (0.7) | 4 (2.3, 5.6) | |
| Other | 4.5 (0.7) | 0.7 (0.9) | 3.7 (1.8, 5.7) | |
| p-value | 0.48 | <0.001 | 0.004 | |
|
| ||||
| Oswestry Disability Index (ODI) (0-100) (SE) |
White | −28.7 (0.4) | −16.2 (0.5) | −12.5 (−13.5, −11.5) |
| Black | −23.3 (1.4) | −9.7 (1.4) | −13.5 (−16.6, −10.4) | |
| Other | −25 (1.4) | −12.9 (1.8) | −12 (−15.7, −8.4) | |
| p-value | <0.001 | <0.001 | 0.79 | |
|
| ||||
| Sciatica/Stenosis Bothersomeness Index (0-24) (SE) |
White | −9 (0.1) | −5.3 (0.2) | −3.7 (−4.1, −3.3) |
| Black | −8.1 (0.4) | −3.1 (0.5) | −5.1 (−6.2, −4) | |
| Other | −8.5 (0.4) | −4.5 (0.6) | −4 (−5.3, −2.7) | |
| p-value | 0.13 | <0.001 | 0.057 | |
DISCUSSION
Over the last three decades several studies have highlighted disparities in the medical care afforded to blacks and other racial or ethnic minorities relative to the white population of the United States.1-7,10-17 Inequalities in care have been thought to arise from socio-economic factors within a population, differences in access to care between groups, and disparity in physician and hospital practices between regions.1,2,7,8,9 Prior research has also reported disparities in the field of orthopaedics as well, albeit primarily in joint replacement surgery.10,11,12 Presently, however, there is a relative lack of research with regard to the effect of race on outcomes following treatment for spinal disorders.
This investigation sought to use the prospectively gathered data from the three arms of the *** to evaluate the effect of race on outcome following operative and non-operative management of patients with IDH, SpS, and DS. The design of the study, as well as the NIH priorities that it espoused, mandated the identical treatment of patients regardless of race or ethnicity. Thus, concerns regarding limited access to care, or disparities in terms of surgical intervention rates could not be evaluated in this investigation.1,2,25
Nonetheless, the results presented here seem to indicate that there are important differences between racial groups that should be recognized. Foremost, as documented in numerous publications1,2,4,6,7,25, black patients in the *** trial appeared to have a lower level of education, maintained a lower socio-economic status, and were more likely to have medical co-morbidities such as elevated BMI, hypertension, and diabetes. While all patients who received surgical intervention for their spinal conditions achieved superior outcomes to those undergoing non-operative management, white patients attained a better result than blacks in every category regardless of the type of treatment rendered. Statistically significant differences in outcome were appreciated between racial groups for operative management in BP, PF, and ODI. Significant differences between racial groups were also evident for non-operative treatment in BP, PF, MCS, ODI and Sciatica/Stenosis Bothersomeness Index. In some instances, such as BP and PF, the non-operative white group’s results approximated that of the black group receiving surgery (Figure 1).
No significant differences in treatment effect were encountered between racial groups except in MCS where surgical intervention significantly improved outcomes in blacks. Importantly, there were also no significant differences in post-operative complications or mortality following surgery and no significant differences in 4-year patient satisfaction or self-rated progress could be identified.
This is in contrast to several prior studies which identified race or ethnicity as a risk factor for post-operative morbidity or mortality relative to whites.13,16,17 In their study regarding complications after spinal cord tumor surgery, Patil et al. reported that black patients were at a significantly higher risk of post-operative morbidity relative to whites.17 In a review of complications after spinal fusion involving bone-morphogenetic protein, Cahill et al. maintained that non-whites had an elevated risk of complications after cervical fusion, thoracic fusion, and lumbar fusion.16 The work of Alosh et al., however, was the only research specifically intended to compare outcomes following spine surgery between whites and racial or ethnic minorities.13 In this investigation the authors used the Nationwide Inpatient Sample to evaluate the effect of race/ethnicity on in-hospital mortality following anterior cervical spine surgery and found that black race was a significant risk factor for post-operative death.13
Disparities in spine care between racial and ethnic groups may result from numerous factors, including racially based obstacles resulting from education, socio-cultural attitudes to health care, historical circumstances, and socio-economic status.7,10,14,15 Further inequalities may result from health-care segregation, or a bias (whether conscious or sub-conscious) on the part of spine-care practitioners.1,2,15 The design of the *** limited the potential for many of these factors to play a role in this investigation. While appreciating this fact, it is apparent that although there were quantitative differences in outcomes between racial groups, there do not appear to be substantive qualitative disparities. Although whites attained better outcomes regardless of treatment rendered, blacks and others demonstrated the same trends for improvement after surgery when compared to non-surgical management and no differences were appreciated in treatment effect or self-reported patient progress and satisfaction. Furthermore, there were no significant differences in complication rates, post-operative mortality, or the need for re-operation between racial groups (Table 2).
There are several limitations to this study that must be appreciated. Foremost, the *** investigations were not originally intended to analyze differences in treatment outcomes between racial groups and, as a result, may have been underpowered to do so. Admittedly, the racial and ethnic minorities enrolled in *** comprised only 15% of the entire cohort. Arega et al. previously reported that, as in many clinical trials, minorities were under-represented in the *** relative to their proportion in the United States population.24 Moreover, while controlling for many confounders in the model, our analyses did not control for other factors that could impact outcome, such as education level, employment status, and presence of workman’s compensation claim. While potentially important, the influence of these factors on our findings cannot be quantified. It should also be recognized that, while diagnosis was controlled for in this analysis, the differences in racial composition, as well as outcome, within the conditions under study (i.e. a significantly greater number of black patients in the DS group) may have influenced our results.
We also acknowledge that the racial and ethnic minorities included in this investigation may not be representative of other individuals who self-ascribe to such groups throughout the country. This fact is most markedly embodied in our use of the term “other” to categorize diverse racial and ethnic minorities including Hispanics, Native Americans, and Asians. Therefore, the ability to generalize our findings regarding the “other” group to any particular minority cannot be supported and may be seen as a further limitation.
While intended to be as inclusive as possible with regard to minorities, the recruitment pattern of the *** may also be seen as a weakness because, at baseline, it eliminated several of the sociological factors that are seen to precipitate healthcare disparities between racial and ethnic groups.1,2,7,10,14,15,25 As the *** was designed to enroll patients from diverse backgrounds, and invite all candidates to participate regardless of race or ethnicity at 11 medical centers across the nation, factors such as healthcare-segregation, inadequate access to care, and provider bias were largely eliminated. Thus, while there do not appear to be important disparities in outcome between racial groups in this analysis, the findings presented here cannot be extrapolated to all medical centers in the United States, other spinal conditions, or the healthcare environment as a whole. Nor do they address issues such as access to care, or the quality of care afforded to minorities.
Lastly, the use of the *** data in an as-treated analysis has been cited in the past as a study limitation, because the benefits of randomization are lost.19-23 This is exemplified by the fact that baseline differences have been appreciated between surgical and non-operative groups in some *** subgroup analyses.19 Baseline differences were appreciated between whites and the minority groups in this analysis as well. However, these findings may be more indicative of important distinctions that exist within the populations themselves (i.e. elevated rates of hypertension, diabetes, and smoking among blacks) as has been recognized in previous works.1,25 Our use of longitudinal regression analysis was made in an attempt to control for the baseline differences between racial groups but, nonetheless, the potential for confounding still exists.
While recognizing these limitations, we seek to emphasize that this investigation represents one of the few studies to evaluate outcomes, morbidity and mortality between racial groups undergoing treatment for spinal disorders, and the only work to do so using prospectively collected data. The results presented here do point to important differences between whites and members of minority groups, however, these distinctions do not necessarily equate to disparities in care. However, these findings must be appreciated in light of the design of the ***, and are not necessarily applicable to the nation as a whole. Ultimately, more prospective research must be conducted in order to define the true nature of spinal healthcare disparities within the United States, as well as the etiologies behind its existence.
KEY POINTS.
- In the three arms of the SPORT, surgical and non-operative treatment resulted in statistically significant improvement in white patients as compared to blacks.
- Although quantitative differences exist between the racial groups in this study, the findings presented here are no necessarily indicative of inequality in healthcare.
- This research is among the few studies that address outcomes, complications and mortality between racial and ethnic groups receiving treatment for spinal disorders. More research regarding this issue should be conducted in the future.
Acknowledgments
Source of Funding The *** investigation was supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases (U01-AR45444) and the Office of Research on Women’s Health, the National Institutes of Health, and the National Institute of Occupational Safety and Health, the Centers for Disease Control and Prevention.
Footnotes
The manuscript submitted does not contain information about medical device(s)/drug(s). National Institute of Arthritis and Musculoskeletal and Skin Diseases (U01-AR45444) and the Office of Research on Women’s Health; National Institutes of Health; and the National Institute of Occupational Safety and Health, the Centers for Disease Control and Prevention funds were received to support this work. One or more of the author(s) has/have received or will receive benefits for personal or professional use from a commercial party related directly or indirectly to the subject of this manuscript: e.g., honoraria, gifts, consultancies, royalties, stocks, stock options, decision making position.
This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Yancy CW, Wang TY, Ventura HO, Piña IL, Vijayaraghavan K, Ferdinand KC, Hall LL, Credo Advisory Group The coalition to reduce racial and ethnic disparities in cardiovascular disease outcomes (credo): Why credo matters to cardiologists. J Am Coll Cardiol. 2011;57:245–252. doi: 10.1016/j.jacc.2010.09.027. [DOI] [PubMed] [Google Scholar]
- 2.Tongue JR, Otsuka NY. Patient-centered care: Communication skills and cultural competence. In: Flynn JM, editor. Orthopaedic Knowledge Update 10. American Academy of Orthopaedic Surgeons; Rosemont, IL: 2011. pp. 109–119. [Google Scholar]
- 3.Bearden D, Allman R, McDonald R, Miller S, Pressel S, Petrovitch H. Age, race, and gender variation in the utilization of coronary artery bypass surgery and angioplasty in SHEP. SHEP Cooperative Research Group. Systolic Hypertension in the Elderly Program. J Am Geriatr Soc. 1994;42:1143–1149. doi: 10.1111/j.1532-5415.1994.tb06979.x. [DOI] [PubMed] [Google Scholar]
- 4.Bhopal R. Is research into ethnicity and health racist, unsound, or important science? Br Med J. 1997;314:1751–1756. doi: 10.1136/bmj.314.7096.1751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Daumit GL, Hermann JA, Coresh J, Powe NR, Ferguson JA. Racial disparity in cardiac decision making. Use of cardiovascular procedures among black persons and white persons: a 7-year nationwide study in patients with renal disease. Ann Intern Med. 1999;130:173–182. doi: 10.7326/0003-4819-130-3-199902020-00002. [DOI] [PubMed] [Google Scholar]
- 6.Gittelsohn AM, Halpern J, Sanchez RL. Income, race, and surgery in Maryland. Am J Public Health. 1991;81:1435–1441. doi: 10.2105/ajph.81.11.1435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Groeneveld PW, Laufer SB, Garber AM. Technology diffusion, hospital variation, and racial disparities among elderly Medicare beneficiaries 1989-2000. Med Care. 2005;43:320–329. doi: 10.1097/01.mlr.0000156849.15166.ec. [DOI] [PubMed] [Google Scholar]
- 8.White KL. Healthcare research: Old wine in new bottles. The Pharos. 1993;56(3):12–16. [PubMed] [Google Scholar]
- 9.Wennberg JE. Understanding geographic variations in healthcare delivery. N Engl J Med. 1999;340:52–53. doi: 10.1056/NEJM199901073400111. [DOI] [PubMed] [Google Scholar]
- 10.Skinner J, Zhou W, Weinstein JN. The influence of income and race on total knee arthroplasty in the United States. J Bone Joint Surg Am. 2006;88:2159–2166. doi: 10.2106/JBJS.E.00271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Irgit K, Nelson CL. Defining racial and ethnic disparities in THA and TKA. Clin Orthop Relat Res. 2011 doi: 10.1007/s11999-011-1885-z. (E-pub ahead of print) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nwachukwu BU, Kenny AD, Losina E, Chibnik LB, Katz JN. Complications for racial and ethnic minority groups after total hip and knee replacement: a review of the literature. J Bone Joint Surg Am. 2010;92:338–345. doi: 10.2106/JBJS.I.00510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Alosh H, Riley LH, 3rd, Skolasky RL. Insurance status, geography, race, and ethnicity as predictors of anterior cervical spine surgery rates and in-hospital mortality: an examination of United States trends from 1992 to 2005. Spine. 2009;34:1956–1962. doi: 10.1097/BRS.0b013e3181ab930e. [DOI] [PubMed] [Google Scholar]
- 14.Schoenfeld AJ, Sieg RN, Li G, Bader JO, Belmont PJ, Jr, Bono CM. Outcomes after spine surgery among racial/ethnic minorities: A meta-analysis of the literature. Spine J. 2011 doi: 10.1016/j.spinee.2011.03.013. (E-pub ahead of print) [DOI] [PubMed] [Google Scholar]
- 15.Taylor BA, Casas-Ganem J, Vaccaro AR, Hilibrand AS, Hanscom BS, Albert TJ. Differences in the work-up and treatment of conditions associated with low back pain by patient gender and ethnic background. Spine. 2005;30:359–364. doi: 10.1097/01.brs.0000152115.79236.6e. [DOI] [PubMed] [Google Scholar]
- 16.Cahill KS, Chi JH, Day A, Claus EB. Prevalence, complications, and hospital charges associated with use of bone-morphogenetic proteins in spinal fusion procedures. JAMA. 2009;302:58–66. doi: 10.1001/jama.2009.956. [DOI] [PubMed] [Google Scholar]
- 17.Patil CG, Patil TS, Lad SP, Boakye M. Complications and outcomes after spinal cord tumor resection in the United States from 1993 to 2002. Spinal Cord. 2008;46:375–379. doi: 10.1038/sj.sc.3102155. [DOI] [PubMed] [Google Scholar]
- 18.Birkmeyer NJ, Weinstein JN, Tosteson AN, Tosteson TD, Skinner JS, Lurie JD, Deyo R, Wennberg JE. Design of the Spine Patient Outcomes Research Trial (***) Spine. 2002;27:1361–1372. doi: 10.1097/00007632-200206150-00020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pearson A, Blood E, Lurie J, Tosteson T, Abdu WA, Hilibrand A, Bridwell K, Weinstein J. Degenerative spondylolisthesis versus spinal stenosis: Does a slip matter? Comparison of baseline characteristics and outcomes (***) Spine. 2010;35:298–305. doi: 10.1097/BRS.0b013e3181bdafd1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tosteson TD, Hanscom B, Blood EA, et al. Statistical methods for cross-over in the *** lumbar disc herniation trial. International Society for the Study of the Lumbar Spine Annual Meeting; Hong Kong. 2007. [Google Scholar]
- 21.Weinstein JN, Lurie JD, Tosteson TD, Tosteson AN, Blood EA, Abdu WA, Herkowitz H, Hilibrand A, Albert T, Fischgrund J. Surgical versus nonoperative treatment for lumbar disc herniation: four-year results for the Spine Patient Outcomes Research Trial (***) Spine. 2008;33:2789–2800. doi: 10.1097/BRS.0b013e31818ed8f4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Weinstein JN, Lurie JD, Tosteson TD, Zhao W, Blood EA, Tosteson ANA, Birkmeyer N, Herkowitz H, Longley M, Lenke L, Emery S, Hu SS. Surgical compared with nonoperative treatment for lumbar degenerative spondylolisthesis: Four-year results in the Spine Patient Outcomes Research Trial (***) randomized and observational cohorts. J Bone Joint Surg Am. 2009;91:1295–1304. doi: 10.2106/JBJS.H.00913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Weinstein JN, Tosteson TD, Lurie JD, Tosteson A, Blood E, Herkowitz H, Cammisa F, Albert T, Boden SD, Hilibrand A, Goldberg H, Berven S, An H. Surgical versus nonoperative treatment for lumbar spinal stenosis four-year results of the Spine Patient Outcomes Research Trial. Spine. 2010;35:1329–1338. doi: 10.1097/BRS.0b013e3181e0f04d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Arega A, Birkmeyer NJ, Lurie JD, Tosteson T, Gibson J, Taylor BA, Morgan TS, Weinstein JN. Racial variation in treatment preferences and willingness to randomize in the Spine Patient Outcomes Research Trial (***) Spine. 2006;31:2263–2269. doi: 10.1097/01.brs.0000232708.66608.ac. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Harris Y, Gorelick P, Samuels P, Bermpong I. Why African Americans may not be participating in clinical trials. J Natl Med Assoc. 1996;88:630–634. [PMC free article] [PubMed] [Google Scholar]