Abstract
OBJECTIVE:
This study examined the 24-month outcomes of a randomized controlled trial of a group-based behavioral weight control (BWC) program combined with either activity-based peer intervention or aerobic exercise.
METHODS:
At baseline, 118 obese adolescents (68% female; BMI = 31.41 ± 3.33) ages 13 to 16 years (mean = 14.33; SD = 1.02) were randomized to receive 1 of 2 weight loss interventions. Both interventions received the same 16-week group-based cognitive-behavioral treatment, combined with either aerobic exercise or peer-based adventure therapy. Eighty-nine adolescents (75% of original sample) completed the 24-month follow-up. Anthropometric and psychosocial measures were obtained at baseline, at the end of the 16-week intervention, and at 12 and 24 months following randomization.
RESULTS:
An intent-to-treat mixed factor analysis of variance indicated a significant effect for time on both percent over 50th percentile BMI for age and gender and standardized BMI score, with no differences by intervention group. Post hoc comparisons showed a significant decrease in percent overweight at 4 months (end of treatment), which was maintained at both 12- and 24-month follow-up visits. Significant improvements on several dimensions of self-concept were noted, with significant effects on physical appearance self-concept that were maintained through 24 months.
CONCLUSIONS:
Both BWC conditions were effective at maintaining reductions in adolescent obesity and improvements in physical appearance self-concept through 24-month follow-up. This study is one of the first to document long-term outcomes of BWC intervention among adolescents.
KEY WORDS: adolescents, overweight, weight management, behavioral weight control
What’s Known on This Subject:
Comprehensive lifestyle interventions for adolescent weight management, including diet, physical activity, and behavioral intervention, have been found to demonstrate modest, short-term success. However, very little is known about the long-term effectiveness of adolescent behavioral weight management trials.
What This Study Adds:
This randomized controlled trial demonstrates that two 16-week group-based behavioral weight loss programs, when combined with either aerobic exercise or peer-based adventure therapy, produced sustained improvements in BMI among overweight/obese adolescents through 24 months.
The prevalence of obesity and overweight is increasing throughout the world, with more than 30% of children and adolescents in the United States considered overweight or obese.1 Obesity in adolescence has been associated with increased risk of obesity in adulthood.2 Modest decreases in BMI among overweight children and adolescents have been shown to be related to significant improvements in health outcomes, including lowered blood pressure and cholesterol, and improved insulin and lipid values.3
Both a recent Cochrane Collaborative Review4 and a review by Tsiros and colleagues5 conclude that comprehensive lifestyle interventions, including diet, physical activity, and behavioral intervention, demonstrate short-term efficacy in addressing obesity in children and adolescents. Very few lifestyle interventions have exclusively targeted adolescents, and few of these provide long-term effectiveness results, rarely going beyond 6- or 12-month outcomes. Of note, a recent trial by Savoye and colleagues6 found that obese children and teenagers (ages 8–15) who were randomized to a 12-month lifestyle intervention were more likely to maintain weight loss at 24-month follow-up than those randomized to a clinic control group; however, this sample was not comprised exclusively of adolescents and was limited by a poor retention rate (43.7%) at 24-month follow-up. A 2-year, family-based behavioral treatment program for overweight adolescents (mean age = 13 years) in China found a BMI reduction of 9.8% among those receiving monthly home visits, as opposed to no cumulative weight change among the control group.7 The long-term impact of this intervention is unknown, as is replication of these results in the United States.
Identification of factors that improve or impede weight loss efforts of adolescents is critical to the mission of improving weight loss programs for this age group. The role of psychological constructs, such as self-efficacy and self-concept, have been found to be important predictors of treatment success among overweight adults.8 At the core of Social Cognitive Theory, Bandura9 defined self-efficacy as an individual’s belief in his or her ability to succeed in specific situations. Self-concept is a multidimensional construct that refers simply to an individual's perception of “self” in relation to any number of characteristics. Indeed, improvements in these constructs are related to end-of-treatment reductions in BMI among adolescents.10 Thus, these may be important factors to consider when promoting adolescent weight control.11
This article provides 24-month follow-up data from a randomized trial of two 6-month group-based behavioral weight loss programs for obese adolescents. We have previously reported that adolescents who were randomized to either behavioral weight control (BWC) plus peer-based adventure therapy intervention (BWC+PEAT) or BWC plus supervised exercise (BWC+EXER) had significant decreases in BMI at 6 months, which were maintained at 12-month follow-up.10 We have also described significant positive correlations between improvements in global self-concept and physical appearance–related self-concept and reductions in BMI at end of treatment. Further, these improvements in perceived self-confidence during active treatment were maintained at 12-month follow-up.
The goals of the current study were twofold: (1) to examine 24-month follow-up data from a randomized controlled trial comparing group-based BWC+PEAT with BWC+EXER, and (2) to determine the contribution of treatment-related improvements in self-efficacy and self-concept to BMI change.
Methods
Participants and Procedures
Participants aged 13 to 16 years, who were between 30% and 90% overBMI (as defined with reference to median BMI for age and gender), had at least 1 parent available to participate, and were English speaking, were recruited via local newspaper advertisements and pediatricians’ offices to participate in a weight control study. Written informed consent was obtained from parents and assent was obtained from adolescents. The study protocol was approved by the Miriam Hospital’s institutional review board (Providence, RI).
Intervention
Adolescents were randomized to 1 of 2, 16-week, group-based BWC interventions that differed only in the exercise component. An urn randomization procedure12 with percent overBMI and gender as covariates was used to assign participants to 1 of 2 intervention conditions, thus allowing for optimal equivalency across groups. Participants received 16 weeks of either a group-based BWC+PEAT or a group-based BWC+EXER. Groups met twice a week for 16 weeks, once a week for BWC intervention content and once a week for on-site physical activity. Weekly BWC intervention consisted of nutrition intervention, physical activity prescription, and topics on behavior modification. Treatment groups were conducted by doctoral-level psychologists with experience in adolescent weight management. The nutrition intervention consisted of a prescribed balanced-deficit diet of 1400 to 1600 calories, with a focus on obtaining a balance of nutrients and calories across the day (ie, breakfast, lunch, dinner, and snacks). Participants were asked to complete weekly detailed nutrition journals, with feedback provided by the study dietician. Nutrition topics included presentation of the dietary exchange system, portion control, dining out, dietary fat, and healthy snack choices, presented by a registered dietitian. The physical activity prescription included gradual increase to a minimum of 30 minutes a day of aerobic activity for 5 days per week. Behavioral topics included self-monitoring of diet and physical activity, portion control, problem solving, goal setting, use of stimulus control strategies, motivation for weight loss, social influences on diet and exercise, and relapse prevention. Each adolescent participated in the BWC intervention with a parent, attending concurrent but separate group meetings. Parent group sessions focused on similar content, as well as guidance regarding family-level support and implementation of behavioral changes. Following the 16 weekly sessions, adolescents were asked to attend 4 biweekly maintenance group sessions. After completion of these 20 group sessions, periodic (quarterly) activities were scheduled to encourage and maintain study contact. These largely consisted of seasonal activities (eg, apple picking, miniature golf) and contained no BWC content.
Treatment groups differed in the weekly on-site activity program that accompanied the standard BWC program. Adolescents randomized to BWC+PEAT participated in weekly peer-based physical activity based on the principles of Outward Bound and designed to increase teamwork, social skills, and self-efficacy. Adolescents randomized to BWC+EXER participated in weekly supervised aerobic exercise sessions. These activity sessions were supervised by either an exercise physiologist or physical therapist. Additional details of the intervention components have been described elsewhere.10,13
Measures
All measures were obtained at baseline, at the end of the 16-week intervention, and at 12 and 24 months following randomization. Participants were offered monetary compensation for time spent completing initial and follow-up evaluations.
Demographic Variables
Basic demographic variables were collected from adolescents and parents, including age, gender, and race/ethnicity. Parent education level was collected as a proxy measure of socioeconomic status.
Anthropometric Variables
Adolescent weight and height were obtained by trained research assistants. Participants’ height was measured without shoes by using a stadiometer (Perspective Enterprises, Portage, MI). Participants’ weight was measured on a balance beam scale in a hospital gown and without shoes. Weight and height were used to calculate BMI (kg/m2), standardized BMI score (z-BMI), and percent overBMI, which are standardized for age and gender. Percent overBMI provides a value relative to the 50th percentile BMI for the appropriate age and gender, where positive values are over the 50th percentile and negative values are under the 50th percentile. It is calculated as teen BMI – BMI at 50th% for age and gender/BMI at 50th% × 100. Percent overBMI is easily understood, and has demonstrated some advantage with regard to sensitivity to changes in weight status.14
Self-Concept
The Self-Perception Profile for Adolescents15 is a widely used 45-item multidimensional questionnaire used to measure adolescents’ perceptions of competence across 8 specific domains. Dimensions of physical appearance, close friendship, athletic competence, social acceptance, and global self-worth were included in this study, with higher scores indicating greater levels of self-concept in that domain. Internal consistency for the 5 subscales included in this study ranged from good to excellent (α = 0.79–0.90).
Self-Efficacy
Two measures of self-efficacy, or the belief in one’s ability to succeed, were used. The Weight Efficacy Life-Style Questionnaire (WEL)16 is a 20-item questionnaire used to assess self-efficacy for eating behaviors and weight loss. Higher scores on the WEL total score are indicative of greater self-efficacy, or belief in one’s ability to succeed in weight loss. Internal consistency of the WEL total score was excellent in this sample (α = 0.90). The Physical Self-Efficacy Questionnaire (PSEQ)17 is an 8-item measure designed to assess confidence related to participation in physical activity, with higher scores indicative of greater levels of confidence in physical activity skills. Internal consistency of the PSEQ total score was α = 0.85 in the current sample.
Intervention-Related Variables
Intervention-specific information was collected during active treatment to explore the relationship between these factors and long-term weight outcomes. These variables included parent BMI change from baseline to 4 months (ie, during treatment), percent of nutrition journals completed by teen and by parent, and attendance at group sessions.
Statistical Analysis
Mixed factor analysis of variance (ANOVA) was used to evaluate changes across time by intervention condition. Treatment condition served as the between-subjects factor and time (baseline, end-of-treatment [4 months], 12 months, and 24 months) as the repeated measure. The primary outcome measures were percent overBMI and z-BMI. Analyses included all randomized participants (intent to treat; n = 118), assuming no change from baseline for noncompleters and by using SPSS for Windows (v19.0) (SPSS Inc, Chicago, IL). Multivariate ANOVAs were conducted on self-concept and self-efficacy of follow-up completers (n = 89). Significant multivariate ANOVA findings were followed by univariate ANOVA, allowing for reduced risk of Type 1 error and accounting for the correlation between dependent variables. Correlational analyses were conducted between primary outcomes and exploratory intervention-related variables.
Results
Participants
A total of 118 obese adolescents (68% female; mean BMI = 31.41; SD = 3.33) ages 13 to 16 years (mean = 14.33; SD = 1.02) entered the trial, averaging 6 to 8 adolescents per treatment group cohort. Of these, 100 (85%) completed the 16-week intervention, attending on average more than 80% of sessions. Ninety-three adolescents (79%) completed the 12-month follow-up, and 89 (75%) participants completed 24-month evaluation. The 24-month completers were 76% White, 13% African American, 7% Hispanic, and 70% female, with an average age of 14.29 years (SD = 0.98), average percent overweight of 161.07 (SD = 16.67), and average BMI of 31.23 (SD = 3.45). Those who dropped out of the study were similar to 24-month completers on baseline demographic variables and anthropometric measures. As shown in the consort diagram in Fig 1, the most common reasons for dropping out were similar in both groups.
FIGURE 1.
CONSORT flow diagram of enrollment, randomization, and follow-up of study participants at all time points.
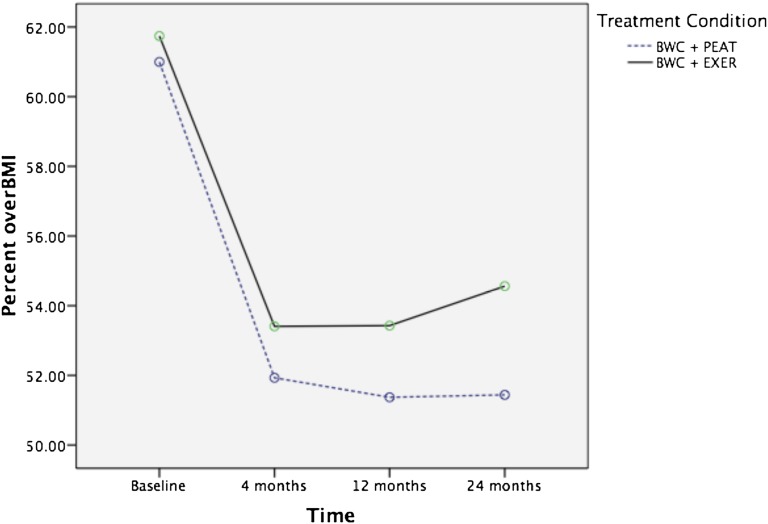
Weight Status Changes Across Time
A consistent pattern was noted in results for primary weight status outcome measures (percent overBMI and z-BMI) and for both intent-to-treat and completer analyses (see Table 1). Mixed factor ANOVA indicated a significant effect of time on percent overBMI, F(3,82) = 36.56, P < .001, with no effect of condition or time × condition interaction. Bonferroni pairwise comparisons showed a significant decrease in percent overBMI from baseline to 4 months (end of treatment) (P < .001), baseline to 12 months (P < .001), and baseline to 24 months (P < .001) (see Fig 1). No significant differences were noted between 4-month, 12-month, and 24-month follow-up points (see Fig 2). Similarly, there was a significant effect of time on z-BMI, F(3,82) = 39.20, P < .001, with no effect of condition or time × condition interaction. Post hoc analyses again showed a significant decrease in z-BMI from baseline to 4 months (P < .001), baseline to 12 months (P < .001), and baseline to 24 months (P < .001). An identical pattern was noted in mixed factor ANOVA conducted with only those completing follow-up visits (n = 86), for both effect of time on percent overBMI, F(3, 84) = 48.46, P < .001, and z-BMI, F(3, 82) = 46.87, P < .001.
TABLE 1.
Group Differences for Measures of Weight, Height, BMI, Percent OverBMI, and z-BMI at Baseline, 4 Months, 12 Months, and 24 Months Across Conditions for Follow-up Completers
| Baseline, Mean (SD) | 4 mo, Mean (SD) | 12 mo, Mean (SD) | 24 mo, Mean (SD) | |
|---|---|---|---|---|
| Weight, kg | 187.39 (30.91) | 179.82 (31.64) | 185.16 (33.21) | 193.39 (34.66) |
| BWC+EXER | 187.78 (31.17) | 180.55 (32.06) | 187.12 (35.56) | 197.36 (37.54) |
| BWC+PEAT | 187.04 (30.91) | 179.11 (31.54) | 183.28 (31.06) | 189.24 (31.26) |
| Height, cm | 164.24 (8.22) | 165.24 (7.82) | 166.53 (7.68) | 167.71 (7.96) |
| BWC+EXER | 164.58 (8.32) | 165.78 (7.88) | 166.96 (7.72) | 168.57 (8.08) |
| BWC+PEAT | 163.93 (8.18) | 164.72 (7.80) | 166.12 (7.70) | 166.77 (7.83) |
| BMI | 31.41 (3.33) | 29.77 (3.64) | 30.19 (4.03) | 31.13 (4.47) |
| BWC+EXER | 31.33 (3.10) | 29.67 (3.41) | 30.32 (4.01) | 31.39 (4.32) |
| BWC+PEAT | 31.49 (3.55) | 29.87 (3.88) | 30.08 (4.08) | 30.86 (4.66) |
| Percent overBMI | 161.34 (16.77) | 152.62 (17.96) | 152.34 (19.17) | 152.91 (20.17) |
| BWC+EXER | 161.74 (15.44) | 153.41 (17.05) | 153.43 (18.70) | 154.56 (19.54) |
| BWC+PEAT | 161.00 (17.99) | 151.93 (18.85) | 151.37 (19.69) | 151.44 (20.75) |
| z-BMI | 2.05 (0.30) | 1.86 (0.39) | 1.83 (0.45) | 1.82 (0.48) |
| BWC+EXER | 2.05 (0.27) | 1.86 (0.35) | 1.85 (0.43) | 1.88 (0.45) |
| BWC+PEAT | 2.02 (0.34) | 1.80 (0.44) | 1.78 (0.49) | 1.77 (0.52) |
FIGURE 2.
Intent-to-treat analysis of the relationship between changes in percent overBMI by treatment condition, from baseline to 4-month, 12-month, and 24-month follow-up.
Self-Concept and Self-Efficacy Changes Across Time
Mixed factor ANOVA demonstrated significant improvements over time on the Harter dimensions of physical appearance, F(3,78) = 19.37 (P < .001); social acceptance, F(3,78) = 2.76 (P < .05); and global self-worth, F(3,78) = 3.35 (P < .05), with no effect of condition or time × condition interaction noted. Bonferroni pairwise comparisons showed significant improvements in physical appearance self-concept from baseline to 4 months (P < .001), baseline to 12 months (P < .001), and baseline to 24 months (P < .01). Significant improvement in social acceptance self-concept was noted from baseline to 4 months (P < .05). Finally, global self-concept scores from baseline to 4 months (P < .05) and baseline to 12 months (P < .05) demonstrated significant improvements. No other scales assessing self-concept or physical appearance self-concept reached significance.
There were no significant changes observed across time on the WEL or PSEQ, measures assessing self-efficacy. Additionally, no significant correlations were observed between changes in percent overBMI or z-BMI at 24 months and dimensions of self-concept or self-efficacy.
Association of Intervention-Related Variables With 24-Month Weight-Status Change
We completed additional analyses evaluating correlations between change in percent overBMI or z-BMI at 24 months and measures of intervention compliance. No significant correlations were noted, with change in weight status at 24 months not significantly related to parent BMI change at 4 months, number of journals completed by the adolescent or by the parent, or attendance at group sessions. Parents and teens completed on average 50% of nutrition journals, whereas those who completed the program attended 81% of group sessions.
Discussion
This study shows that a behavioral weight loss program can produce sustained improvements in BMI in overweight and obese adolescents through 24 months. The initial 16-week intervention was effective in reducing zBMI by –0.19 U, and follow-up at 24 months showed that this reduction was maintained. Indeed, the magnitude of improvements noted in 24-month zBMI change are consistent with other 24-month outcomes6 reported and exceed end-of-treatment outcomes3,18 reported in other intensive behavioral weight loss trials for children and teens. For instance, reductions in zBMI were noted to be twice as large as those found in a 12-month investigation comparing conventional isocaloric diet and isocalorie meal replacement diets among obese teenagers.19 The current study adds to a growing body of literature documenting modest reductions in weight status with lifestyle interventions for adolescents.4 These modest reductions in weight have yielded clinically significant improvements in systolic blood pressure, total cholesterol, triglycerides, insulin, and fasting glucose.3,19
Contrary to expectation, there was no advantage observed for the peer-enhanced activity condition. Improvements in weight status were observed in both BWC interventions, with both equally effective in producing reductions in z-BMI and percent overBMI that were maintained at 24-month follow-up. As previously noted, this may have stemmed from the fact that participating in physical activity in a group setting accorded many of the same benefits related to self-concept and team building as the peer condition.10
Reductions in weight status were paralleled by improvements in multiple domains of self-concept, including physical appearance, social acceptance, and global self-concept. Of note, only improvements in physical appearance–related self-concept were retained at 24 months. As with changes in z-BMI, there was no advantage observed for the peer-enhanced condition. Although these improvements co-occurred with reductions in weight status, changes in self-concept were not related to z-BMI or percent overBMI at 24 months. The lack of association suggests that participation in a weight loss program confers benefits on self-concept that are independent of the changes in weight, such as other perceived improvements to physical appearance or greater acceptance of physical appearance. Previous research has demonstrated a positive association between increases in physical activity and dimensions of self-concept,20 suggesting that change in variables such as physical activity should not be overlooked.
Although improvements in self-concept were observed, there were no changes in self-efficacy for eating behaviors or self-efficacy for physical activity in adolescents participating in either treatment condition, and self-efficacy was unrelated to weight loss. These results differ from previous findings in adult weight control studies, but confirm findings from a previous study with adolescents.21 It is possible that the measures used to assess self-efficacy related to weight control behaviors did not “translate” well to an adolescent sample, or that adolescents may overestimate their efficacy at the outset. Alternatively, it is also possible that the dimension of physical activity self-efficacy may have little influence on variables such as weight loss if overweight teens have not learned to place significant value on physical activity and the role it can have in improving their health and well-being.
The study findings need to be interpreted with some limitations in mind. First, although retention was quite good for an adolescent weight control trial, only 75% of the sample completed the 24-month assessment. Second, the sample size did not allow for examination of outcomes by gender or race/ethnicity. Future exploration of the roles that gender and race/ethnicity play in initial intervention response, weight loss trajectory, and maintenance of weight loss is imperative as the field considers ways of effectively tailoring and improving interventions for various subgroups of overweight individuals. As might be expected, group attendance while in active treatment has been shown to be a significant predictor of weight loss success22; however, the role of intervention-related variables, such as attendance and completion of nutrition journals, is diminished by 24 months, perhaps an effect of history, or perhaps testimony to the waxing and waning quality of motivation to lose weight. Finally, we compared 2 relatively intensive BWC interventions. Evaluating these BWC interventions relative to a limited-treatment control group would help to better understand the necessary and effective elements for adolescent weight control. Interestingly, in its initial stages, this study included a third treatment arm (standard care), which consisted of 3 individual meetings with a nutritionist. This condition was discontinued early on because of adolescent and parent concerns with treatment acceptability and associated difficulties with retention.
Reversing the trend of increasing childhood and adolescent obesity is critical to improving the short- and long-term health of the next generation of youth. Comprehensive BWC interventions have yielded a modest reduction in BMI.4,5 Although surgical intervention for cases of severe adolescent obesity has garnered much attention recently,23,24 BWC remains the most feasible and clinically appropriate strategy for moderately overweight youth. The current study extends existing literature by providing support for the long-term effectiveness of BWC as a weight maintenance strategy. Improved self-concept, particularly related to physical self-concept, may be an additional benefit to adolescent participation in BWC programs.
Conclusions
This study is noteworthy in documenting promising maintenance of initial weight loss outcomes at 24-month follow-up in overweight adolescents. The current study is one of only a few studies targeting adolescents to include a follow-up period beyond 12 months. Maintenance of weight loss has been given little attention in this population and has been identified as an area of high priority.25 The clinical implications of this research are clear. Comprehensive intervention, including dietary and physical activity prescription along with behavioral modification, can be effective in reducing weight status in obese adolescents. Although these reductions are modest, they are noteworthy given the typical trajectory of weight gain from adolescence into adulthood without intervention.26 An additional potential benefit of this type of intervention is improved self-concept, which is typically diminished among overweight teenagers.
Acknowledgments
Appreciation is expressed to Katherine Flynn-O’Brien, Jamie Kaplan, and Meghan Neill for their assistance with data collection.
Glossary
- ANOVA
analysis of variance
- BWC
behavioral weight control
- BWC+EXER
behavioral weight control plus aerobic exercise
- BWC+PEAT
behavioral weight control plus peer-enhanced adventure therapy
- Percent overBMI
percent over 50th percentile BMI for age and gender
- PSEQ
Physical Self-Efficacy Questionnaire
- WEL
Weight Efficacy Life-Style Questionnaire
- z-BMI
standardized BMI score
Footnotes
All authors have contributed substantive intellectual contributions, including assisting with conception and design, analysis and interpretation of data, and drafting of earlier versions of this work. All authors will contribute to final approval of the version to be published.
Results were previously presented at the 2010 meeting of The Obesity Society, October 8–12, 2010 San Diego, CA.
This trial has been registered at www.clinicaltrials.gov (identifier NCT00285558).
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: This study was supported by grants R01-DK062916 (Dr Jelalian) and K23-HL069987 (Dr Lloyd-Richardson) from the National Institutes of Health/National Heart, Lung, and Blood Institute. Funded by the National Institutes of Health (NIH).
References
- 1.Ogden CL, Lamb MM, Carroll MD, Flegal KM. Obesity and socioeconomic status in children and adolescents: United States, 2005-2008. NCHS Data Brief. 2010 Dec;(51):1–8 [PubMed]
- 2.The NS, Suchindran C, North KE, Popkin BM, Gordon-Larsen P. Association of adolescent obesity with risk of severe obesity in adulthood. JAMA. 2010;304(18):2042–2047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kirk S, Zeller M, Claytor R, Santangelo M, Khoury PR, Daniels SR. The relationship of health outcomes to improvement in BMI in children and adolescents. Obes Res. 2005;13(5):876–882 [DOI] [PubMed]
- 4.Oude Luttikhuis H, Baur L, Jansen H, et al. Interventions for treating obesity in children. Cochrane Database Syst Rev. 2009;(1):CD001872 [DOI] [PubMed]
- 5.Tsiros MD, Sinn N, Coates AM, Howe PR, Buckley JD. Treatment of adolescent overweight and obesity. Eur J Pediatr. 2008;167(1):9–16 [DOI] [PubMed] [Google Scholar]
- 6.Savoye M, Shaw M, Dziura J, et al. Effects of a weight management program on body composition and metabolic parameters in overweight children: a randomized controlled trial. JAMA. 2007;297(24):2697–2704 [DOI] [PubMed]
- 7.Jiang JX, Xia XL, Greiner T, Lian GL, Rosenqvist U. A two year family based behaviour treatment for obese children. Arch Dis Child. 2005;90(12):1235–1238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Teixeira PJ, Silva MN, Coutinho S, et al. Mediators of weight loss and weight loss maintenance in middle-aged women. Obesity. 2010;18(4):725–735 [DOI] [PubMed]
- 9.Bandura A. Self-efficacy: The Exercise of Control. New York, NY: W H Freeman/Times Books/ Henry Holt & Co; 1997 [Google Scholar]
- 10.Jelalian E, Lloyd-Richardson E, Mehlenbeck RS, et al. Behavioral weight control treatment with supervised exercise or peer-enhanced adventure for overweight adolescents. J Pediatr. 2010;157(6):923–928 [DOI] [PMC free article] [PubMed]
- 11.Nowicka P, Savoye M. Strategies that motivate children and their families to take positive action: empowering self efficacy and change. Int J Pediatr Obes. 2010;5(s1):25–2719437242 [Google Scholar]
- 12.Stout RL, Wirtz PW, Carbonari JP, Del Boca FK. Ensuring balanced distribution of prognostic factors in treatment outcome research. J Stud Alcohol Suppl. 1994;12(suppl 12):70–75 [DOI] [PubMed] [Google Scholar]
- 13.Jelalian E, Mehlenbeck R, Lloyd-Richardson E, Birmaher V, Wing RR. ‘Adventure therapy’ combined with cognitive-behavioral treatment for overweight adolescents. Int J Obes. 2006;30(1):31–39 [DOI] [PubMed]
- 14.Paluch RA, Epstein LH, Roemmich JN. Comparison of methods to evaluate changes in relative body mass index in pediatric weight control. Am J Hum Biol. 2007;19(4):487–494 [DOI] [PubMed] [Google Scholar]
- 15.Harter S. Manual for the Self-perception Profile for Adolescents. Denver, CO: University of Denver Department of Psychology; 1988 [Google Scholar]
- 16.Clark MM, Abrams DB, Niaura RS, Eaton CA, Rossi JS. Self-efficacy in weight management. J Consult Clin Psychol. 1991;59(5):739–744 [DOI] [PubMed]
- 17.Motl RW, Dishman RK, Trost SG, et al. Factorial validity and invariance of questionnaires measuring social-cognitive determinants of physical activity among adolescent girls. Prev Med. 2000;31(5):584–594 [DOI] [PubMed]
- 18.Janicke DM, Sallinen BJ, Perri MG, Lutes LD, Silverstein JH, Brumback B. Comparison of program costs for parent-only and family-based interventions for pediatric obesity in medically underserved rural settings. J Rural Health. 2009;25(3):326–330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Berkowitz RI, Wadden TA, Gehrman CA, et al. Meal replacements in the treatment of adolescent obesity: a randomized controlled trial. Obesity (Silver Spring). 2011;19(6):1193–1199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stein C, Fisher L, Berkey C, Colditz G. Adolescent physical activity and perceived competence: does change in activity level impact self-perception? J Adolesc Health. 2007;40(5):462.e1–462.e8 [DOI] [PMC free article] [PubMed]
- 21.White MA, Martin PD, Newton RL, Walden HM, York-Crowe E, Gordon ST, et al. Mediators of weight loss in a family-based intervention presented over the internet. Obes Res. 2004;12(7):1050–1059 [DOI] [PubMed]
- 22.Jelalian E, Hart CN, Mehlenbeck RS, et al. Predictors of attrition and weight loss in an adolescent weight control program. Obesity (Silver Spring). 2008;16(6):1318–1323 [DOI] [PubMed] [Google Scholar]
- 23.Inge TH, Miyano G, Bean J, et al. Reversal of type 2 diabetes mellitus and improvements in cardiovascular risk factors after surgical weight loss in adolescents. Pediatrics. 2009;123(1):214–222 [DOI] [PubMed] [Google Scholar]
- 24.O’Brien PE, Sawyer SM, Laurie C, et al. Laparoscopic adjustable gastric banding in severely obese adolescents: a randomized trial. JAMA. 2010;303(6):519–526 [DOI] [PubMed] [Google Scholar]
- 25.Butryn ML, Wadden TA, Rukstalis MR, et al. Maintenance of weight loss in adolescents: current status and future directions. J Obes. 2010;2010:789280 [DOI] [PMC free article] [PubMed]
- 26.Nonnemaker JM, Morgan-Lopez AA, Pais JM, Finkelstein EA. Youth BMI trajectories: evidence from the NLSY97. Obesity (Silver Spring). 2009;17(6):1274–1280 [DOI] [PubMed] [Google Scholar]