Abstract
The objective was to determine prevalence and predictive risk factors of suicidality in a large sample of epilepsy outpatients. We prospectively examined 193 consecutive adult epilepsy outpatients for depression, including suicidal ideation. Demographic and epilepsy factors, medication toxicity and health-related quality of life were also evaluated. The prevalence of suicidal ideation within the past two weeks was 11.9%. Although medication toxicity, health-related quality of life and BDI scores were each associated with suicidal ideation in the bivariate analyses, only the BDI remained significant in the logistic regression analysis. About one-fourth of the subjects with suicidal ideation had no significant symptoms of depression. Recent thoughts of suicide are a common occurrence in the outpatient epilepsy clinic setting, but are not predicted by gender, age, seizure factors, medication toxicity or self-perceived quality of life. Although depression is associated with suicidal ideation, about one-fourth of suicidal subjects was euthymic or only mildly depressed.
Keywords: Epilepsy, Suicide, Suicidal ideation, Beck Depression Inventory, Depression
INTRODUCTION
Suicide risk is elevated in persons with epilepsy compared to the general population and completed suicide is an important contributor to their increased mortality[1,2]. Suicide is ranked as the second leading cause of death in a young, working age population, in the recent report by the Center for Disease Control and Prevention (CDC)[3]. Each year about 5 million people in the US have suicidal ideation, and nearly half of individuals express their intent prior to suicide[4,5]. Thus, suicidal ideation may be an important warning sign that precedes suicide, especially in population with increased risk such as epilepsy.
Robertson[5] reviewed rates of suicides in epilepsy patients and found in more than twenty available studies that, on average, 11.5% of all deaths were due to suicide. This is about 10-fold higher rate than 1.4% of deaths by suicide in the general population[6]. Jones et al.[1] recently reported from a multicenter trial that included 139 patients with epilepsy, in which our center also participated with a different group of patients, that suicidal ideation is common in patients with epilepsy. Using specific modules of the Mini International Neuropsychiatric Interview (M.I.N.I.) as part of their psychiatric evaluation, the group found that 12.2% of patients had recent suicidal ideation. Intuitively one may assume that people with epilepsy become suicidal due to the chronic, disabling nature of their illness. This “reactive model” is supported by data indicating that the concept of learned helplessness and attributional style in particular is related to the pathogenesis of depression in epilepsy[7]. Recent studies showed that premorbid suicidal behavior may have an important role in the neurobiology of epilepsy. A study from Iceland suggests that suicide attempt, and not only depression, is independent risk factor for the development of unprovoked seizures[8]. In this population the risk for unprovoked seizure was 3.5-fold higher and remained significant after adjusting for major depression, bipolar disorder and cumulative alcohol intake. This suggests that suicidal behavior can precede the occurrence of a first unprovoked seizure. Increased prevalence of depression in epilepsy patients may also contribute to their increased suicidal rate, but this was not systematically investigated. The prevalence of depression in persons with epilepsy is significantly higher than in the general population, occurring in 25–55% patients with pharmacoresistant epilepsy and it is lower but still elevated in persons with fully controlled seizures[2,9].
In this study we evaluated the prevalence of suicidal ideation in a tertiary epilepsy clinic. This is the first study to our knowledge to determine predictive factors for suicidal ideation in epilepsy patients. We hypothesized that depression would be a stronger independent predictor of suicidality than seizure factors or social and vocational dysfunction.
METHODS
Subjects
We analyzed a group of 193 consecutive adults with epilepsy in the tertiary epilepsy clinics at Washington University. All participants signed an informed consent form approved by the Institutional Review Board. Demographic variables for age, gender, race, employment, marital status, chemical dependency, years of education, and seizure factors for type of epilepsy, localization of seizure focus, seizure frequency and epilepsy duration were evaluated. Medication toxicity was assessed with the Adverse Events Profile (AEP). The QOLIE-89 was used to measure self-perceived quality of life.
Clinical and Epilepsy Assessments
Seizure classification was based on the definitions proposed by the International League Against Epilepsy (ILAE)[10]. Seizures were monitored by seizure records maintained by the subjects in conjunction with their physicians. Seizure frequency was defined as the total number of complex partial and generalized seizures in a month, and averaged for the previous six months. We also assessed type of and number of drugs subjects were using at the time of their evaluation for suicidal ideation.
Adverse Medication Effects Assessment
The Adverse Events Profile (AEP) was developed to evaluate the most common negative side effects reported by patients taking antiepileptic drugs (AED)[11]. The AEP is a self-report instrument that consists of 19 items for evaluation of antiepileptic drug side effects, using a Likert scale from 1 to 4, with 4 indicating more frequent occurrences. A score ranging from 19 to 76 may be calculated to measure total side effect burden of a medication regimen. The AEP was demonstrated to differentiate and quantify the severity of side effects of AEDs[11].
Quality of Life Assessment
The QOLIE-89 is widely used inventory for assessment of self-perceived quality of life in persons with epilepsy[12,13]. This instrument contains the Short Form (SF)-36, a comprehensively studied health-related quality of life (HRQOL) questionnaire used in various investigations determining effect of chronic diseases, and 53 additional items assessing influence of recurrent seizures and epilepsy-related disability. It includes 17 subscales to examine broad range of domains of social, vocational and seizure factors. The scales produce a score ranging from 0 to 100, with higher scores indicating better self-perceived life quality.
Assessment of suicidal ideation and depressive symptoms
During a routine clinic visit all patients were evaluated for the presence of depression with a clinical interview and were asked to rate presence of suicidal ideation. This evaluation included the Beck Depression Inventory (BDI), a widely used test for assessment of recent symptoms of depression, also validated for use in epilepsy[1]. The BDI requires a self-rating from 0–3 on 21 items based on experience in the past 14 days; a cumulative total from the addition of individual scores is recorded. Scores of 11 to 15 are indicative of mild, 16–23 of moderate, and 24 or greater of severe depression. A score greater than 15 is considered to represent clinically significant depression[14]. Question 9 of the BDI asks specifically about suicidal thoughts or wishes. It provides following options: 0 [I don’t have any thoughts of killing myself], 1 [I have thoughts of killing myself, but I would not carry them out], 2 [I would like to kill myself] and 3 [I would kill myself if I had the chance]. Using these categories we split subjects into two groups: one group consisted of patients who marked the answers “1”, “2” or “3”, i.e. with suicidal ideation; and the other group of patients who marked the answer “0”, without suicidal ideation.
Statistical Analyses
We used Student’s t-test and chi-square test for group comparisons for clinical variables and for the BDI, AEP and QOLIE-89 total scores, and a Mann-Whitney U test for independent group comparisons. A value of p< 0.05 was considered as significant. All statistical analyses were performed in SPSS (SPSS Inc., Chicago, IL).
RESULTS
We found that 11.9% (23 out of 193) of patients with epilepsy had recent suicidal thoughts. Two of these patients also stated they would kill themselves if they had a chance.
Demographic, vocational, social and seizure-related variables were similar in the patients that endorsed suicidal ideation (N= 23) and the group without suicidal ideation (N= 170). Depression, medication toxicity and QOLIE-89 scores were significantly worse in the patients that endorsed suicidal ideation (χ2, p< 0.0001 for each). In addition, there were more patients who attempted suicide in the past in the group with current suicidal ideation (χ2, p< 0.05), Table 1.
Table 1.
Clinical variables in the group of epilepsy patients with and without suicidal ideation
| Suicidal ideation N= 23 | No suicidal ideation N= 170 | |
|---|---|---|
| AGE (yrs) | 37±12 | 39±12 |
|
| ||
| GENDER (M/F in %) | 48/52 | 52/48 |
|
| ||
| RACE (White/Afr.Amer. in %) | 95.7/4.3 | 84.7/14.7 |
|
| ||
| SEIZURE TYPE (%) | ||
| Simple partial | 4.3 | 15.3 |
| Complex partial | 78.3 | 65.9 |
| IGE | 17.4 | 18.8 |
|
| ||
| SEIZURE LOCALIZATION (%) | ||
| temporal R/L | 21.7/13.0 | 17.6/22.4 |
| frontal R/L | 4.3/0 | 1.2/8.8 |
| parietal R/L | 0/0 | 1.2/2.9 |
| generalized | 8.7 | 18.8 |
|
| ||
| SEIZURE FREQUENCY/Month | 7.7±18.2 | 4.0±8.5 |
|
| ||
| NUMBER OF AEDs | 1.9±0.9 | 1.6±0.8 |
|
| ||
| EDUCATION (yrs) | 13.0±2.9 | 13.7±2.6 |
|
| ||
| EMPLOYED (Y/N) | 30.4/69.6 | 54.2/45.8 |
|
| ||
| MARRIED/SINGLE | 45.5/54.5 | 53.6/46.4 |
|
| ||
| BDI score | 22.5±8.6* | 7.7±7.8 |
|
| ||
| AEP score | 48.3±8.7* | 37.5±11.4 |
|
| ||
| QOLIE-89 score | 46.7±12.5* | 67.5±19.9 |
|
| ||
| PRIOR SUICIDE ATTEMPT (%) | 13*(n= 3) | 1 (n= 2) |
χ2, p< 0.0001
IGE idiopathic generalized epilepsy
AED antiepileptic drug
BDI Beck Depression Inventory
AEP Adverse Events Profile
QOLIE Quality of Life In Epilepsy
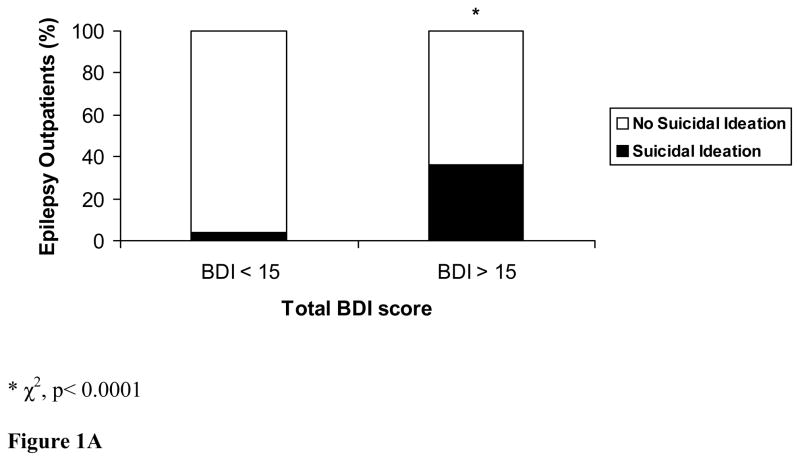
In our total sample (n= 193), 38.4% of patients endorsed significant symptoms of depression defined as a BDI >11. More patients with moderate to severe depression, which is defined by a total BDI ≥15, had recent suicidal thoughts (17 out of 44, 38%), than euthymic or mildly depressed patients, with the BDI<15 (6 out of 149, 4%), χ2, p< 0.0001, Figure 1A.
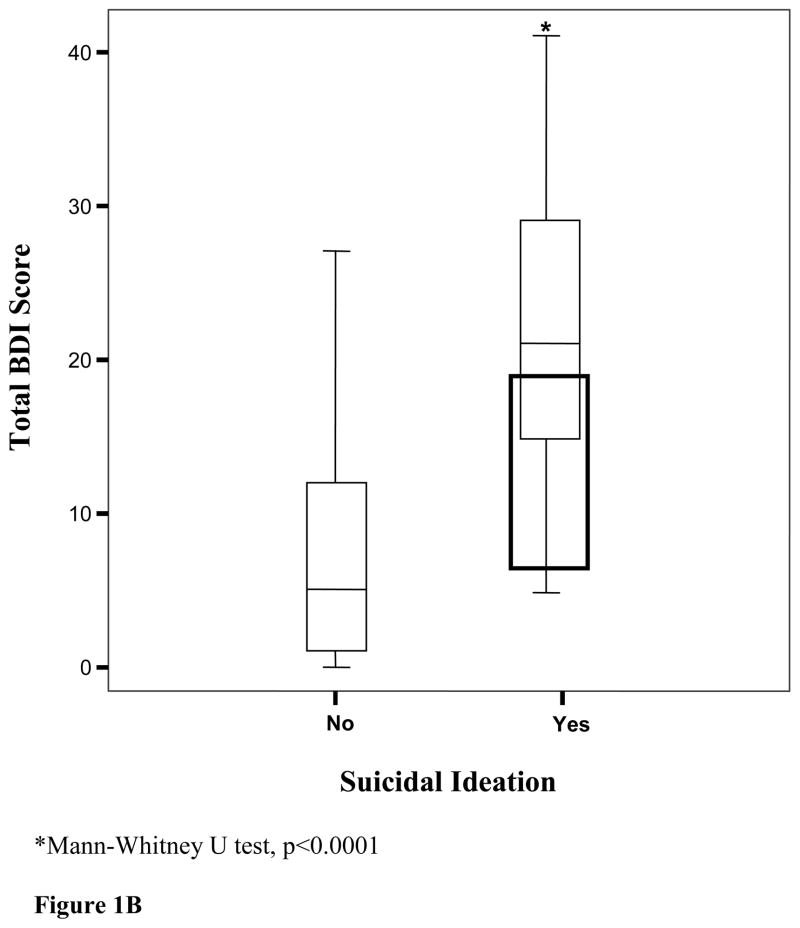
Figure 1.
A. Relation of presence of suicidal ideation in epilepsy outpatients without (BDI < 15) and with clinically significant depressive symptoms (BDI ≤ 15). B. Boxplots with median lines and extremes show association of presence (Yes) and absence (No) of suicidal ideation with the BDI total score
Multivariate regression analysis including demographic factors (age and gender), seizure-related factors (seizure frequency and epilepsy duration), medication toxicity (AEP score), self-perceived quality of life (QOLIE-89 total score) and the BDI total score as independent variables, found that only the BDI total score had significant association (β of 0.177, p< 0.0001), Table 2.
Table 2.
Multivariate regression analysis: total BDI score was the only independent predictor of suicidal ideation
| β | p< | |
|---|---|---|
| BDI | 0.177 | 0.0001 |
| AEP | −0.008 | 0.85 |
| QOLIE-89 | −0.007 | 0.82 |
| Seizure frequency | 0.011 | 0.65 |
| Age | −0.054 | 0.06 |
| Gender | −0.049 | 0.93 |
Although suicidal ideation was associated with higher BDI scores, 26% (6 of 23) of this group scored in the euthymic or mildly depressed range with the BDI< 15, Figure 1B.
DISCUSSION
We found that on average every 8–9th patient in this study group endorsed suicidal ideation during previous two weeks. Although self-perceived quality of life, medication toxicity, and the BDI score were each associated with suicidal ideation, regression analysis demonstrated that only depression remained a significant predictor of suicidal thoughts.
Our results indicate that suicidal ideation in epilepsy outpatients is common; 10.9% of patients endorsed recent suicidal ideas, and additional 1.0% stated that they would have killed themselves if they had a chance. Moreover, three patients had already attempted suicide in the past. This confirms earlier finding from Jones et al.[1]. In their study 12.2% of patients reported recent interictal suicidal thoughts. This group used a different instrument, the M.I.N.I., in structured psychiatric interviews and found that suicidal ideas in epilepsy patients are more common in patients with current Axis I disorder, primarily major depression, anxiety or both, but did not examine other possible risk factors.
Standardized mortality ratio (SMR) in epilepsy patients is increased and in most studies is in the range of 1.6–5.3[15–17]. The SMR in newly diagnosed epilepsy was highest during the first year after diagnosis at 5.1 (95% CI 3.8–6.5), and declined to 2.5 (95% CI 1.5–3.9) at 3 years, and 1.3 (95% CI 0.7–2.0) at 5 years. The SMR for patients with idiopathic epilepsy was 1.6 (95% CI 1.0–2.4), for remote symptomatic epilepsy 4.3 (95% CI 3.3–5.5) and for an acute symptomatic epilepsy 2.9 (95% CI 1.7–4.5)[17]. A recent study examined records from 224 patients with epilepsy in Iceland and found highest mortality rate due to suicide (SMR was 5.8, 95% CI 1.56–14.84), than any other causes of death in men with epilepsy[18]. Another large study of 9061 epilepsy patients in Sweden using hospital discharge diagnosis of epilepsy, also reported an excess mortality rate due to suicide (SMR 3.5, 95% CI 2.6–4.6)[19].
Christensen et al.[20] conducted a large population-based, case control study of more than 20,000 persons who committed suicide from 1981 to 1997 in Denmark. In this study it was observed that epilepsy patients had 3 times higher risk of comitting suicide compared to controls (rate ratio 3.17, 95% CI 2.88–3.50). The risk remained high (1.99, 95% CI 1.71–2.32) after excluding those with a history of psychiatric disease and adjusting for socioeconomic factors. The highest risk of suicide was identified in epilepsy patients with comorbid psychiatric disease (rate ratio 13.7, 95% CI 11.8–16.0). Causality of suicidal ideation and attempted and completed suicide has been examined in prior studies. In the longitudinal National Comorbidity survey of the general population in the US, 13.5% participants reported lifetime suicidal ideation, 3.9% a suicide plan, and 4.6% a suicide attempt. Cumulative probabilities were 34% for the transition from ideation to a plan and 72% from a plan to an attempt, and 26% from ideation to an unplanned attempt[21]. About 90% of unplanned and 60% of planned first attempts occurred within one year of the onset of ideation. In a recent study of newly diagnosed unprovoked seizures among Icelandic men[8], a history of attempted suicide was 5.1-fold more common in epilepsy patients than in controls. Suicide attempt was significantly associated with an increased risk for development of unprovoked seizure, even after adjusting for age, sex, cumulative alcohol intake and major depression. A relationship of suicide attempts among patients with epilepsy and comparably handicapped controls with other chronic disabilities found that 30% of patients with epilepsy had attempted suicide as compared with 7% of the handicapped controls[22].
Our data suggest that recent thoughts of suicide are strongly associated with depression and not by seizure factors (epilepsy type or localization of seizure focus, seizure frequency and duration of epilepsy), age, gender, medication toxicity or decreased quality of life. In this study 38.4% patients had recent depressive symptoms, and suicidal ideation was more common in patients with clinically significant symptoms of depression. The generally difficult psychosocial conditions of patients with chronic epilepsy have frequently been assumed as the major risk factor for elevated suicide rate. Although studies agree that only a complete seizure freedom can improve quality of life[23], some suggested that decreased quality of life may be due to increased seizure severity, epilepsy duration, patients’ age and medication toxicity. Baker et al.[24] evaluated psychological and social factors in adolescents with epilepsy and reported that high seizure frequency and lower levels of knowledge about epilepsy were significantly associated with depressive symptoms, lower self-esteem and higher levels of social anxiety. In this study, we also show that although depression was associated with suicidal ideation, 26% of patients were euthymic or had only mild depressive symptoms. This is similar to observation by Hesdorffer et al.[8] that a significant number of subjects who attempted suicide previously never met criteria for major depression according to DSM-IV.
We showed that depression and not seizure factors or quality of life predicts suicidal ideation, which is a novel contribution to the research of neurobiology of depression in epilepsy. Some authors already hypothesized that the underlying cause of depression could be a specific aspect of structural or functional brain abnormality, rather than a result of various social and vocational factors. Quiske et al[25] found an association between mesial temporal sclerosis and depressive symptoms, and other groups found association of glucose metabolism[26] or cerebral blood flow[27] in the prefrontal or temporal regions in patients with complex partial seizures and depressive symptoms. In our earlier report, we observed that in the group of 62 epilepsy patients those with recent depressive symptoms assessed with the BDI, had decreased cerebral glucose metabolism limited to the temporal regions, irrespectively of their age, type of seizures or seizure frequency, or medication toxicity[28].
In this study we also looked at type or number of antiepileptic drugs the subjects were taking at the time of their assessment. We found no association of suicidal ideation when we compared subjects taking one or more antiepileptic drugs concomitantly (χ2 of 0,53). No specific antiepileptic drug was associated with significant suicidal ideation. In fact, lamotrigine was the most frequently used drug in the subjects that endorsed suicidal ideas, but lamotrigine is considered to have a positive psychotropic effects and it has an FDA indication for treatment of bipolar disorder. Although some medications have positive psychotropic effect, like SSRIs, that are associated with suicidal ideation, it was only in children, therefore it is unlikely that lamotrigine had this effect in our patients. There are a number of limitations to this study. Our data are cross-sectional and longitudinal studies may be necessary to establish causality and correlate clinical symptoms with changes in dynamic brain function over time. Another limitation to the study is that we assessed patients from a specialty clinic in a tertiary center, and the results presented might not be generalizable to patients with well-controlled seizures. Psychiatric literature indicates that anxiety can contribute to suicidal ideations.
In summary, we found that suicidal ideation is a common finding in epilepsy outpatients. Depression and not seizure factors or self-perceived quality of life is an independent predictor of suicidal ideation in this study. Our data also emphasize the importance of identifying and treating depression in epilepsy population. Greater attention should be directed to early recognition of suicidal ideation, because self-reported instruments we used were not sufficient. This study suggests that we need to directly evaluate for presence of suicidal ideations and suicidal plan. It shows that the BDI overall score in normal range does not exclude and is not sufficient to detect all subjects with suicidal ideation.
Highlights.
We determined prevalence and predictive risk factors of suicidality in epilepsy
The prevalence of suicidal ideation within the past two weeks was 11.9%
Thoughts of suicide are common in the outpatient epilepsy clinic setting
Depression is associated with suicidal ideation
Over one fourth of suicidal subjects was euthymic or only mildly depressed
Acknowledgments
This work was supported by National Institutes of Health grants NS40808 and NS047551 (FG) and the Epilepsy Foundation Fellowship (HH).
Footnotes
Financial disclosures: None
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Jones JE, Hermann BP, Barry JJ, Gilliam FG, Kanner AM, Meador KJ. Rates and risk factors for suicide, suicidal ideation, and suicide attempts in chronic epilepsy. Epilepsy Behav. 2003;4(Suppl 3):S31–8. S31–S38. doi: 10.1016/j.yebeh.2003.08.019. [DOI] [PubMed] [Google Scholar]
- 2.Kanner AM. Depression in epilepsy: prevalence, clinical semiology, pathogenic mechanisms, and treatment. Biol Psychiatry. 2003;54:388–398. doi: 10.1016/s0006-3223(03)00469-4. [DOI] [PubMed] [Google Scholar]
- 3.National Center for Injury Prevention and Control. Centers for Disease Control and Prevention; 2007. http://www.cdc.gov/ncipc/dvp/suicide/SuicideDataSheet.pdf. [Google Scholar]
- 4.Obafunwa JO, Busuttil A. Clinical contact preceding suicide. Postgrad Med J. 1994;70:428–432. doi: 10.1136/pgmj.70.824.428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Robertson MM. Mood disorders associated with epilepsy. In: Mc Connell HW, Snyder PJ, editors. Psychiatric comorbidity in epilepsy. Washington: American Psychiatric Press; 1998. p. 133. [Google Scholar]
- 6.Nilsson L, Ahlbom A, Farahmand BY, Asberg M, Tomson T. Risk factors for suicide in epilepsy: a case control study. Epilepsia. 2002;43:644–651. doi: 10.1046/j.1528-1157.2002.40001.x. [DOI] [PubMed] [Google Scholar]
- 7.Hermann BP, Trenerry MR, Colligan RC. Learned helplessness, attributional style, and depression in epilepsy. Bozeman Epilepsy Surgery Consortium. Epilepsia. 1996;37:680–686. doi: 10.1111/j.1528-1157.1996.tb00633.x. [DOI] [PubMed] [Google Scholar]
- 8.Hesdorffer DC, Hauser WA, Olafsson E, Ludvigsson P, Kjartansson O. Depression and suicide attempt as risk factors for incident unprovoked seizures. Ann Neurol. 2006;59:35–41. doi: 10.1002/ana.20685. [DOI] [PubMed] [Google Scholar]
- 9.Gilliam F, Hecimovic H, Sheline Y. Psychiatric comorbidity, health, and function in epilepsy. Epilepsy Behav. 2003;4 (Suppl 4):S26–S30. doi: 10.1016/j.yebeh.2003.10.003. [DOI] [PubMed] [Google Scholar]
- 10.Commission on Classification and Terminology of the International League Against Epilepsy, Proposal for revised classification of epilepsies and epileptic syndromes. Epilepsia. 1989;30:389–399. doi: 10.1111/j.1528-1157.1989.tb05316.x. [DOI] [PubMed] [Google Scholar]
- 11.Gilliam FG, Fessler AJ, Baker G, Vahle V, Carter J, Attarian H. Systematic screening allows reduction of adverse antiepileptic drug effects: a randomized trial. Neurology. 2004;62:23–27. doi: 10.1212/wnl.62.1.23. [DOI] [PubMed] [Google Scholar]
- 12.Vickrey BG, Hays RD, Graber J, Rausch R, Engel J, Jr, Brook RH. A health-related quality of life instrument for patients evaluated for epilepsy surgery. Med Care. 1992;30:299–319. doi: 10.1097/00005650-199204000-00002. [DOI] [PubMed] [Google Scholar]
- 13.Birbeck GL, Hays RD, Cui X, Vickrey BG. Seizure reduction and quality of life improvements in people with epilepsy. Epilepsia. 2002;43:535–538. doi: 10.1046/j.1528-1157.2002.32201.x. [DOI] [PubMed] [Google Scholar]
- 14.Jones JE, Hermann BP, Woodard JL, et al. Screening for major depression in epilepsy with common self-report depression inventories. Epilepsia. 2005;46:731–735. doi: 10.1111/j.1528-1167.2005.49704.x. [DOI] [PubMed] [Google Scholar]
- 15.Jallon P. Mortality in patients with epilepsy. Curr Opin Neurol. 2004;17:141–146. doi: 10.1097/00019052-200404000-00010. [DOI] [PubMed] [Google Scholar]
- 16.Hauser WA, Annegers JF, Elveback LR. Mortality in patients with epilepsy. Epilepsia. 1980;21:399–412. doi: 10.1111/j.1528-1157.1980.tb04088.x. [DOI] [PubMed] [Google Scholar]
- 17.Cockerell OC, Johnson AL, Sander JW, Hart YM, Goodridge DM, Shorvon SD. Mortality from epilepsy: results from a prospective population-based study. Lancet. 1994;344:918–921. doi: 10.1016/s0140-6736(94)92270-5. [DOI] [PubMed] [Google Scholar]
- 18.Rafnsson V, Olafsson E, Hauser WA, Gudmundsson G. Cause-specific mortality in adults with unprovoked seizures. A population-based incidence cohort study. Neuroepidemiology. 2001;20:232–236. doi: 10.1159/000054795. [DOI] [PubMed] [Google Scholar]
- 19.Nilsson L, Tomson T, Farahmand BY, Diwan V, Persson PG. Cause-specific mortality in epilepsy: a cohort study of more than 9,000 patients once hospitalized for epilepsy. Epilepsia. 1997;38:1062–1068. doi: 10.1111/j.1528-1157.1997.tb01194.x. [DOI] [PubMed] [Google Scholar]
- 20.Christensen J, Vestergaard M, Mortensen PB, Sidenius P, Agerbo E. Epilepsy and risk of suicide: a population-based case-control study. Lancet Neurol. 2007;6:693–698. doi: 10.1016/S1474-4422(07)70175-8. [DOI] [PubMed] [Google Scholar]
- 21.Kessler RD, Borges G, Walters EE. Prevalence of and risk factors for lifetime suicide attempts in the National Comorbidity Survey. Archives of General Psychiatry. 1999;56:617–626. doi: 10.1001/archpsyc.56.7.617. [DOI] [PubMed] [Google Scholar]
- 22.Mendez MF, Cummings JL, Benson DF. Depression in epilepsy. Significance and phenomenology. Arch Neurol. 1986;43:766–770. doi: 10.1001/archneur.1986.00520080014012. [DOI] [PubMed] [Google Scholar]
- 23.Vickrey BG, Hays RD, Rausch R, Sutherling WW, Engel J, Jr, Brook RH. Quality of life of epilepsy surgery patients as compared with outpatients with hypertension, diabetes, heart disease, and/or depressive symptoms. Epilepsia. 1994;35:597–607. doi: 10.1111/j.1528-1157.1994.tb02480.x. [DOI] [PubMed] [Google Scholar]
- 24.Baker GA, Spector S, McGrath Y, Soteriou H. Impact of epilepsy in adolescence: a UK controlled study. Epilepsy Behav. 2005;6:556–562. doi: 10.1016/j.yebeh.2005.03.011. [DOI] [PubMed] [Google Scholar]
- 25.Quiske A, Helmstaedter C, Lux S, Elger CE. Depression in patients with temporal lobe epilepsy is related to mesial temporal sclerosis. Epilepsy Res. 2000;39:121–125. doi: 10.1016/s0920-1211(99)00117-5. [DOI] [PubMed] [Google Scholar]
- 26.Bromfield EB, Altshuler L, Leiderman DB, et al. Cerebral metabolism and depression in patients with complex partial seizures. Arch Neurol. 1992;49:617–623. doi: 10.1001/archneur.1992.00530300049010. [DOI] [PubMed] [Google Scholar]
- 27.Schmitz EB, Moriarty J, Costa DC, Ring HA, Ell PJ, Trimble MR. Psychiatric profiles and patterns of cerebral blood flow in focal epilepsy: interactions between depression, obsessionality, and perfusion related to the laterality of the epilepsy. J Neurol Neurosurg Psychiatry. 1997;62:458–463. doi: 10.1136/jnnp.62.5.458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gilliam F, Santos J, Vahle V, Carter J, Brown K, Hecimovic H. Depression in epilepsy: ignoring clinical expression of neuronal network dysfunction? Epilepsia. 2004;45(Suppl 2):28–33. 28–33. doi: 10.1111/j.0013-9580.2004.452005.x. [DOI] [PubMed] [Google Scholar]