Abstract
Introduction
Pituitary tumors from lactotrope cells account for about 40% of all functioning pituitary cancers. Men tend to present with a larger, more invasive and rapid growth prolactinomas than women, possibly because hypogonadism features are less evident.
Case report
A 27-year-old, previously asymptomatic Saudi man presented with a 3-day history of emesis with severe left-sided frontal headache, left face and right upper limb numbness, with signs of obstructive hydrocephalus. Brain Computed Tomography (CT) and Magnetic Resonance Imaging (MRI) revealed a giant pituitary mass occupying several regions (sellar, infra-sellar, and supra-sellar) measuring 6.5 × 5.7 × 5.9 cm, and invading the sphenoid sinus as well as the cavernous sinuses bilaterally, with intra-pituitary hemorrhage compressing the third ventricle causing obstructive hydrocephalus. Prolactin levels were >200,000 mIU/L, consistent with invasive giant prolactinoma (IGP). He was treated with Cabergoline which eventually normalized the prolactin level and significantly reduced the size of IGP.
Conclusion
This is a rare case of obstructive hydrocephalus with super-imposed intra-pituitary hemorrhage secondary to IGP, highlighting the importance of a full hormonal assessment for proper diagnosis and management.
Keywords: (IGP) invasive giant prolactinoma, obstructive hydrocephalus
Introduction
Pituitary tumors from lactotrope cells account for about 40% of all functioning pituitary cancers.1 Men tend to present with a larger, more invasive and rapid growth prolactinomas than women, possibly because hypogonadism features are less evident.2 Non- specific manifestations include menstrual irregularities for women, sexual dysfunction, galactorrhea,3 and osteopenia.4 Other signs and symptoms are due to compression and obstruction effects, most common of which is the loss of vision and bitemporal hemianopia.5 Rarely, patients with prolactinoma will present with obstructive hydrocephalus or seizures.6 Current recommendations suggest Dopamine agonists as the treatment of choice for prolactinomas, including giant and invasive types as these drug suppresses PRL secretion and synthesis as well as lactotrope cell proliferation.7
Case Presentation
A previously asymptomatic, 27-year-old Saudi man, presented with a 3-day severe unilateral headache involving the left eye, not relieved with medications, accompanied with emesis and prick-like sensation at the left part of his face and right upper limb. Patient had a history of blurred vision, no fever. On examination, patient was fully conscious and oriented. Vital signs revealed hypotension (94/68 mmHg) and bradycardia (50 bpm, regular). Temperature was 37 °C. The rest of the routine physical and laboratory exams were unremarkable. ECG showed sinus bradycardia. CT scan of brain without contrast revealed hyper-dense sellar, supra-sellar mass extending to the left pontine area obstructing third ventricle with mild subarachnoid hemorrhage. Few days later, patient became drowsy, with no significant changes in physical signs. Patient was kept head up 30°. Dexamethazone and Tegretol were given, and emergent ventricle-portal shunt has been placed. Patient thereafter experienced improvement in headache and vomiting. CSF revealed WBC: 2 c/cumm; RBC: 2.196; glucose: 67 mg/dL and protein 17 mg/dL. CSF culture was negative. He was subsequently referred to our department.
Upon referral, patient denied history of syncope, fever, night sweats, and skin dryness. He noted a decrease in his libido, impotence, decreased facial and chest hair one year before his presentation but did not seek medical advice. On examination, he was conscious, coherent and ambulatory. He was obese with a BMI 35.6 kg/m2, blood pressure 115/70 mmHg, heart rate 64 bpm regular, respiratory rate 22 bpm, oxygen saturation 96% in room air and afebrile. Secondary sexual characteristic features revealed decreased facial and trunk hair, neck and cranial nerve examinations were unremarkable. Further investigations and endocrine work up is shown in Table 1. Prolactin level ≥ 100,000 mIU/L (normal 86–390 mIU/L); repeat measurement revealed ≥ 200,000 mIU/L. Other hormones IGF-I, GH, ACTH were normal.
Table 1.
Hormonal assessment of the patient from baseline to 18 months.
| Hormones | Admission | 2 weeks | 1 month | 2 months | 5 months | 6 months | 10 months | 12 months | 18 months | 24 months |
|---|---|---|---|---|---|---|---|---|---|---|
| Prolactin | 273.86 | 12420 | 2918 | 2017 | 961.3 | 579.4 | 383 | 589 | 148 | 137.5 |
| TSH | 0.16 | – | 5.89 | 6.04 | 1.2 | – | 5.26 | 7.8 | 3.2 | – |
| FT4 | – | – | 11.41 | 11.34 | 17.84 | – | 11.86 | 10.95 | 15.1 | 11.6 |
| Testosterone | 0.07 | – | 2.29 | 3.66 | 6.72 | 1.81 | 2.94 | 12.06 | 3.44 | 2.76 |
| SHBG | 16.3 | – | 16.55 | – | – | 16.04 | 13.61 | 14.77 | – | – |
| Free testosterone index | <0.423 | – | 13.8 | – | – | – | – | 81.7 | – | 8.31 |
| LH | 4.33 | – | 2.14 | 3.72 | – | – | <0.1 | – | – | – |
| FSH | 3.53 | – | 2.18 | 3.78 | – | – | 0.21 | – | – | – |
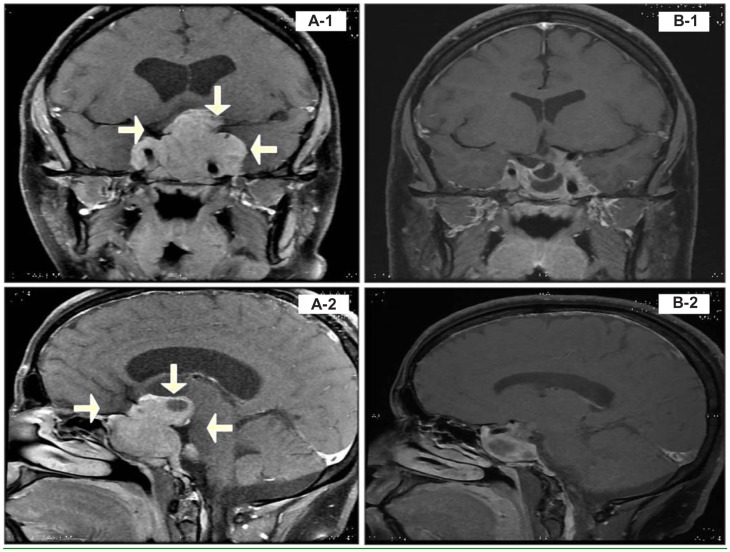
Patient was referred to an ophthalmologist and assessment revealed no evidence of visual field abnormalities; optic disc and macula were normal. The patient was started on Cabergoline 0.25 mg po twice per week with gradual increase in the dose to 1 mg twice a week. Table 1 shows normalization of the prolactin level. MRI 1 year post-treatment showed significant regression in the overall size and extension of the pituitary adenoma with subsequent interval resolution of the mass effect on the suprasellar optic pathway and in the dilatation of third ventricle compared with the previous MRI as shown Figure 1.
Figure 1.
Sagittal and frontal T1 MRI before (A-1 and A-2), and after treatment with Cabergoline (B-1 and B-2).
Notes: MRI of the brain and pituitary gland showed enormous invasive tumor mass lesion is mainly solid with two cystic components at sellar, infra-sellar, and supra-sellar area measures 6.5 × 5.7 × 5.9 cm in its anterior-posterior, transverse, craniocaudal dimensions respectively. The mass displaced the optic chiasm superiorly. Anterior portion shows retrochiasmatic component which is lobulated and shows a small to medium size lobule extending posteriorly to the left CP angle (compressing the the left trigeminal nerve), with another small lobule extending posteriorly to the left orbit through the superior orbit fissure. The two cystic components are noted at the hypothalmic and third ventricle with fluid level (evidence of intra-lesional hemorrhage of the posterior extension of this mass along the left tentorial leaflet and adjacent left lateral border of the brainstem), likely representing pituitary apoplexy.
Discussion
In this case report we present an adult Saudi patient with IGP, who had significant history and signs of hypogonadism for one year without seeking medical consultation, and finally presenting with mass effect symptoms of IGP.
Remarkable progress has been made with regards to the management of giant prolactinoma, the ultimate goal of which is to achieve eugonadism, euprolactinemia status, and reduction of tumor size.8 Other modalities include radiotherapy, which is not the usual preferred treatment because of high complication rates.9 On the other hand, therapy with dopamine agonist drugs (Bromocriptine, Cabergoline), are consistently promising in hypogonadal status reversal, prolactin level correction and regression size of pituitary adenomas.10–15
Conclusion
This case highlights a rare presentation of IGP in the form of obstructive hydrocephalus, and the importance of accurately diagnosing prolactinomas. As was revealed in this case, our patient improved significantly medical therapy, avoiding unnecessary invasive treatments, and preventing short and long term complications.
Consent
Written informed consent was obtained from the patient for publication purposes and accompanying images. A copy is available upon request.
Footnotes
Author’s Contributions
SA and NJ diagnosed, investigated and managed the patient. SA and NJ contributed equally in the writing of this case report. Both authors read and approved the final version of the manuscript.
Competing Interests
The authors have no conflict of interest.
Disclosures and Ethics
As a requirement of publication author(s) have provided to the publisher signed confirmation of compliance with legal and ethical obligations including but not limited to the following: authorship and contributorship, conflicts of interest, privacy and confidentiality and (where applicable) protection of human and animal research subjects. The authors have read and confirmed their agreement with the ICMJE authorship and conflict of interest criteria. The authors have also confirmed that this article is unique and not under consideration or published in any other publication, and that they have permission from rights holders to reproduce any copyrighted material. Any disclosures are made in this section. The external blind peer reviewers report no conflicts of interest.
Funding
Author(s) disclose no funding sources.
References
- 1.Partington MD, Davis DH, Laws ER, Jr, Scheithauer BW. Pituitary adenomas in childhood and adolescence. Results of transphenoidal surgery. J Neurosurg. 1994;80:209–16. doi: 10.3171/jns.1994.80.2.0209. [DOI] [PubMed] [Google Scholar]
- 2.Delgrange E, Trouillas J, Maiter D, Donckier J, Tourniaire J. Sex-related difference in the growth of prolactinomas: a clinical and proliferation marker study. J Clin Endocrinol Metab. 1997;82:2102–7. doi: 10.1210/jcem.82.7.4088. [DOI] [PubMed] [Google Scholar]
- 3.Kleiberg DL, Noel GL, Frantz AG. Galactorrhea. A study of 235 cases, including 48 with pituitary tumors. N Engl J Med. 1977;296:589–600. doi: 10.1056/NEJM197703172961103. [DOI] [PubMed] [Google Scholar]
- 4.Klibanski A, Neer RM, Bitins IZ, Ridgway EC, Zervas NT, McArthur JW. Decreased bone density in hyperprolactinemic women. N Engl J Med. 1980;303:1511–4. doi: 10.1056/NEJM198012253032605. [DOI] [PubMed] [Google Scholar]
- 5.Hollenhorst RW, Younge BR. Ocular manifestations produced by adenomas of the pituitary gland: analysis of 1000 cases. In: Kohler PO, Ross GT, editors. Diagnosis and treatment of pituitary Tumors. New York: Elsevier; 1973. pp. 53–64. [Google Scholar]
- 6.Zikel OM, Atikinson JL, Hurley DL. Prolactinoma manifesting with symptomatic hydrocephalus. Mayo Clin Proc. 1999;74:475–7. doi: 10.4065/74.5.475. [DOI] [PubMed] [Google Scholar]
- 7.Shrivastava RK, Arginteanu MS, King WA, Post KD. Giant prolactinomas: clinical management and long-term follow up. J Neurosurg. 2002;97(2):299–306. doi: 10.3171/jns.2002.97.2.0299. [DOI] [PubMed] [Google Scholar]
- 8.Muralidhara KS, Ahmed A, Darko D. Dramatic response with medical treatment of an extensively invasive ‘giant’ prolactinoma with cabergoline. Endocrine Abstracts. 2004;8:50. [Google Scholar]
- 9.Berwaerts J, Verhelst J, Abs R, Appel B, Mahler C. A giant prolactinoma presenting with unilateral exophthalmos. J Endocrinol Invest. 2000;23(6):393–8. doi: 10.1007/BF03343743. [DOI] [PubMed] [Google Scholar]
- 10.Maccagnan P, Macedo CL, Kayath MJ, Nogueira RG, Abucham J. Conservative management of pituitary apoplexy: a prospective study. J Clin Endocrinol Metab. 1995;80:2190–7. doi: 10.1210/jcem.80.7.7608278. [DOI] [PubMed] [Google Scholar]
- 11.Shrivastava Raj K, Arginteanu Marc S, King Wesley A, Post Kalmon D. Giant prolactinomas: clinical management and long-term follow up. J Neurosurg. 2002;97(2):299–306. doi: 10.3171/jns.2002.97.2.0299. [DOI] [PubMed] [Google Scholar]
- 12.Acharya SV, Gopal RA, Menon PS, Bandgar TR, Shah NS. Giant prolactinoma: Efficacy of medical management. Endocr Pract. 2009;24:1–14. doi: 10.4158/EP09221.OR. [DOI] [PubMed] [Google Scholar]
- 13.Corsello SM, Ubertini G, Altomare M, Lovicu RM, Migneco MG, Colosimo Rota CA. Giant prolactinomas in men: efficacy of cabergoline treatment. Clin Endocrinol. 2003;58(5):662–70. doi: 10.1046/j.1365-2265.2003.01770.x. [DOI] [PubMed] [Google Scholar]
- 14.Wu ZB, Yu CJ, Su ZP, Zhuge QC, Wu JS, Zheng WM. Bromocriptine treatment of invasive giant prolactinomas involving the cavernous sinus: results of a long-term follow up. J Neurosurg. 2006;104(1):54–61. doi: 10.3171/jns.2006.104.1.54. [DOI] [PubMed] [Google Scholar]
- 15.Shimon I, Benbassat C, Hadani M. Effectiveness of long-term cabergoline treatment for giant prolactinoma: study of 12 men. Eur J Endocrinol. 2007;156:225–31. doi: 10.1530/EJE-06-0646. [DOI] [PubMed] [Google Scholar]