Abstract
The number of kidneys obtained from deceased diabetic donors available for transplantation has increased >8-fold increase in the past 15 years. We assessed allograft outcomes associated with deceased diabetic donors and compared them with that of standard and extended criteria donors in the UNOS data registry. We identified 1982 recipients of diabetic standard criteria donors over a 10-year period from 1995 through 2004. Both overall and death-censored survival of organs from diabetic standard criteria donors, was significantly better than that of organs obtained from non-diabetic extended criteria donors while inferior to that from nondiabetic standard criteria donors. Compared with ECD donors, diabetic donors had lower serum creatinine, less cold ischemia and these kidneys were less likely to be pump-perfused. Recipients of diabetic kidneys were younger and less likely to experience delayed graft function compared with recipient of ECD kidneys. More recently, many diabetic donor kidneys have been given to diabetic recipients with early graft survival being similar to that among non-diabetic recipients. These findings demonstrate the potential to expand and to improve utilization of this resource without compromising outcomes for recipients. Improved, evidence-based evaluation and allocation of deceased diabetic donor kidneys is needed to optimize their use.
Keywords: Diabetic kidney donor, extended criteria donor, graft survival, kidney transplant outcomes
Introduction
The continually growing number of patients being waitlisted for renal transplantation leads to an urgent need for novel approaches to expand the donor pool.(1) There has been a steady increase in the number of deceased donor organs obtained from individuals with obesity, metabolic syndrome and diabetes mellitus in the United States, where the prevalence of these characteristics has increased significantly in the last two decades, - a trend which is likely to continue to for the foreseeable future. Since there is only limited data available in the literature about the function and survival of allografts obtained from diabetic deceased donors, we felt it important to obtain a better understanding of current utilization patterns and outcomes for organs these donors, in particular non-extended criteria diabetic donors (referred to as diabetic standard criteria donors (D-SCD).(2)
The reversal of early changes of diabetic nephropathy after transplantation of deceased diabetic donor kidneys into euglycemic individuals, first demonstrated in 1983 by Abouna, following experimental data in rodents, raised the possibility of the effective use of kidneys from D-SCDs.(3) In these initial cases, kidneys procured from a single diabetic donor were transplanted into two non-diabetic recipients. Follow up biopsies performed at 7 months after transplantation demonstrated reversal of mesangial diabetic changes. One patient died with a functioning allograft at 22 months and the other patient had a functioning allograft at 36 months, despite the development of new onset diabetes after transplantation.(3, 4) Following this initial report on the use of diabetic donor kidneys, several centers began to use allografts from D-SCDs with acceptable graft survival rates. These early results suggested that organs from D-SCDs who have normal renal function and potentially reversible mesangial pathologic changes could be used successfully for transplantation and would safely expand the organ donor pool.(5-7) More recent analyses, however, have found significantly worse long-term outcomes of kidneys from D-SCDs in comparison to organs obtained from non-diabetic standard criteria donors, although the absolute difference was relatively small.(2, 6, 8) While the shortened D-SCDs allograft survival has not prevented the continued use of these organs, a large number of these organs continue to be discarded as well. Existing studies have not compared outcomes using D-SCDs kidneys with the function and survival of kidneys obtained from the expanded donor pool (extended criteria donors (ECD)) and thus fail to take into consideration the overall context for evaluating the outcomes associated with these “marginal” organs. In light of this we utilized the UNOS database to analyze the graft survival of kidneys obtained from deceased diabetic donors and compared their outcomes with those of both non-diabetic standard criteria donors and with another group of marginal donors (non-diabetic extended criteria donors, ND-ECD) which have achieved greater acceptance among the transplant community, at least for certain preselected recipients, and now represent nearly 20% of deceased donor transplants.
Methods
We compared outcomes for transplants of renal allografts obtained from diabetic and non-diabetic deceased donors performed during a 10-year period (from 1995 through the end of 2004) and distinguished those that met the definition for extended criteria from those that did not. We identified 1982 patients in the UNOS database who received transplants from D-SCD donors from 1995 through 2004 and compared death censored as well as overall graft survival of these D-SCD kidneys to the outcomes of 11,087 kidneys obtained from non-diabetic SCDs, and non-diabetic extended criteria donors (ND-ECDs) transplanted over the same time period. We also included diabetic extended criteria donors (D-ECDs) in our analysis for completion. Donors whose diabetes status was listed as “unknown” were excluded from our analysis. Univariate analysis was used to assess the impact of various donor and recipient characteristics other than diabetes on the survival of allografts from D-SCDs. A Cox proportional hazards model was used for multivariate analysis of factors, which influence D-SCD allograft survival. During our 10-year study period only 31 recipients of diabetic organs were identified as having diabetes before transplantation – partly a result of unknown diabetes status for a large number of recipients during this period.
The relative percentage of recipients with “unknown diabetes status” started to decrease starting in 2002 as the rate of identification of the diabetes status of recipients before transplantation improved considerably over time. Therefore, we performed a separate analysis to compare outcomes based on the diabetes status of the recipient using data on patients transplanted between 2002 through 2009 – a period when the vast majority of transplants of diabetic organs to diabetic recipients was identifiable in the UNOS registry.
All data was obtained from the standard transplant and research (STAR) file by the United Network for Organ Sharing (UNOS) dated November 27th 2009. Organ discard data was also obtained from UNOS and was based on OPTN data as of January 7th 2011. We also obtained organ discard data directly from UNOS for the period from 1995 through 2008 as part of separate data requests (request 122810-9 and 20120108-3). Statistical analysis was performed with Stata 11.2 (Stata Corp., College Station, TX).
Results
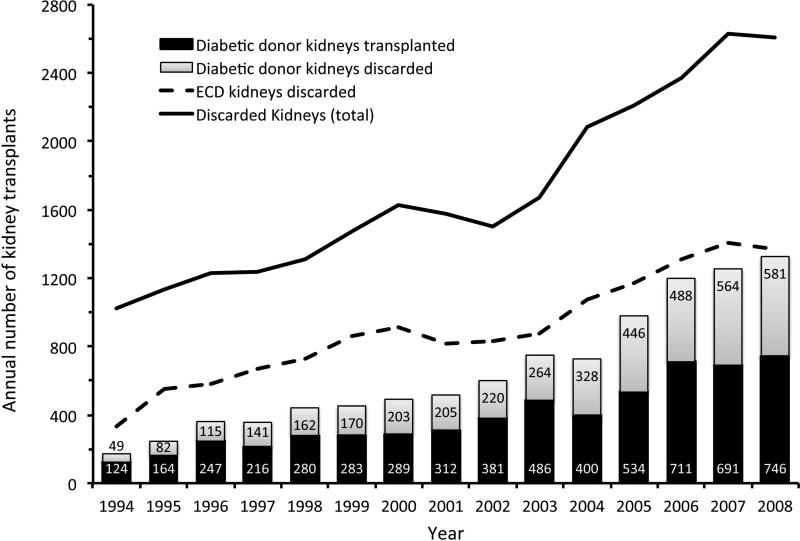
Between 1994 and 2008, the number of kidneys recovered from deceased diabetic donors increased from 173 to 1327 annually – almost an 8-fold increase (figure 1). However, this was also accompanied by a 13-fold increase in the discard rate of kidneys from diabetic donors, from 49 to 581 kidneys annually. Due this increase in discard rate, despite the overall increase in number, there was an overall decrease in the utilization of D-SCD kidneys for transplantation during that period, from 71.6% to 56.2% (figure 1, p<0.001).
Figure 1.
Annual trend in the number of kidneys from diabetic donors that were transplanted. Despite the increasing use of organs from diabetic (and extended criteria) donors, the total number of kidneys discarded – particularly from diabetic donors – continues to rise over time.
It is important to note that between 1994 and 2008 the number of kidneys discarded from all deceased donors also increased significantly but at a slower rate, from 1020 to 2608 (an increase from 10.7 to 19.1% of kidneys recovered from all deceased donors, χ2 =253, p<0.001). Almost a third of this increase in the overall discard rate of deceased donor kidneys was from the diabetic donor pool, which overall constituted only 4.8% of discarded kidneys in 1994 but as much as 22.3% of all discarded kidneys by 2008 (χ2 =174.3, p<0.001). Over the same period there was a three-fold increase in ECD organs procured (from 1003 in 1994 to 3211 in 2008) with relatively small increase in the rate of discard of these organs from 33.2% to 43.6% (see Figure 1).
From 1994 to 2008, the last complete year for which data were available in the STAR file, we noted a 6-fold increase, from 124 to 746, in the absolute number of diabetic deceased donor kidneys transplanted annually (Figure 1). As a result, renal allografts from diabetic donors surprisingly represent now a significant percentage of the total number of deceased donor kidneys transplanted in the United States – a rise from 1.5% in 1994 to 6.4% in 2008 (χ2 =832.7, p<0.001). During the same period, the use of ECD kidneys also increased 2.8 fold from 679 to 1887 transplants reflecting an increase from 8% to 15.9% of all deceased kidney transplants in the United States (see Figure 1).
Outcomes
As expected kidneys obtained from Diabetic donors were overall inferior to those of non-diabetic donors (Log rank = 147.77, p<0.001). The presence of diabetes in ECD donors was associated with a worse outcome compared with non-diabetic ECD organs (Log rank =6.54, p=0.0106). Similarly, the diagnosis of diabetes in SCD donors also predicted a worse graft survival compared with non-diabetic SCD donors (Log rank =70.9, p<0.001). (Figure 2). We also compared outcomes between kidneys obtained from D-SCDs and those obtained from non-diabetic ECDs. On univariate analysis, death censored survival of allografts obtained from D-SCDs was inferior to that of kidneys obtained from a non-diabetic SCD's; it was, however, significantly better than that of kidneys obtained from nondiabetic ECDs (Log Rank =21.65, p<0.001) (figure 2). Further analysis suggested that the risk of graft failure attributable to diabetes was significantly different between SCD and ECD organs (Breslow Day χ2 = 9.38, p =0.0022) with the odds ratio for death censored graft failure among diabetic SCD compared to nondiabetic SCD being 1.42 (95% confidence interval 1.29 – 1.56). The odds ratio for failure among diabetic ECD donors versus nondiabetic ECD donors was 1.1 (95% confidence interval 0.97 – 1.26) with a wide confidence interval that was likely to be a result of the relatively small sample size.
Figure 2.
Kaplan Meier survival curves showing death censored graft survival for renal allografts from diabetic donors, extended criteria donors in comparison to the reference group of non-diabetic and standard criteria donors. (Supplemental figure 1 demonstrates overall graft survival, i.e. not death censored, for the same groups)
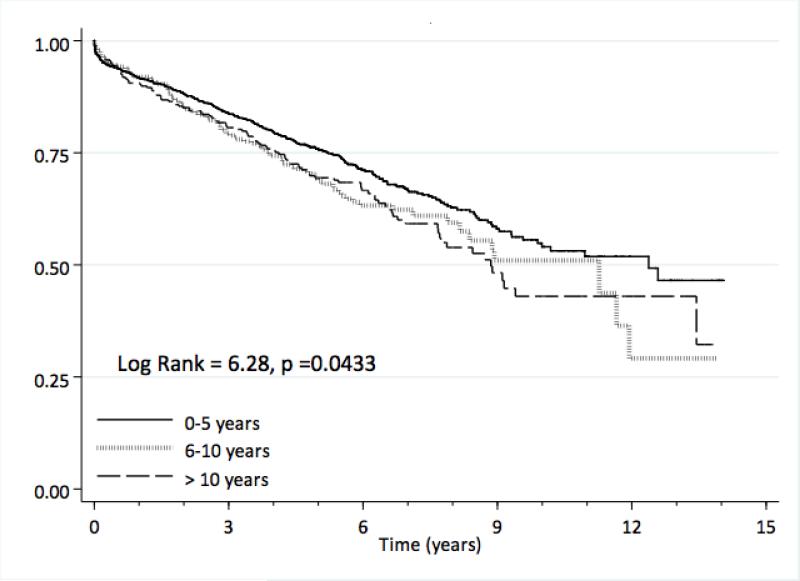
We also found a significant difference in allograft survival depending on the duration of donor diabetes as recorded by UNOS (divided into 3 groups: 0 – 5 years, 6 – 10 years and > 10 years) (figure 3, Log Rank = 6.28, p=0.0433,) with a significant trend toward worse survival of D-SCD kidneys with longer duration of diabetes (Log Rank test for trend = 5.60, p=0.0179). Kaplan Meier estimates for death censored and overall graft survival are presented in supplementary tables 1a and 1b.
Figure 3.
Death censored renal allograft survival outcomes by reported duration of diabetes in the donor. (Supplemental figure 2 demonstrates overall graft survival, i.e. not death censored, for the same groups)
In Table 1, we compare donor, organ and recipient characteristics for D-SCDs, ND-SCDs, D-ECDs and ND-ECDs from 1995 through 2004 using the nonparametric Kruskal-Wallis rank test because of unequal variances and sizes of the groups for continuous variables and the Chi squared test for categorical variables. In addition DSCDs were compared to ND-ECDs using the Mann Whitney U test and the Chi squared test. Diabetic SCDs were older, heavier, more likely to be female and hypertensive as compared to ND-SCDs while organs from D-SCDs had similar terminal creatinine, experienced slightly longer cold ischemia and were slightly more likely to be placed on a perfusion pump. Recipients of the D-SCD organs tended to older with longer waitlist times, were less likely to diabetic and experienced more delayed graft function than recipients who received kidneys from ND-SCDs. Diabetic SCD donors were significantly younger, heavier and more likely to be male when compared to ND-ECD donors. The kidneys from the diabetic donors tended to have lower terminal serum creatinine, marginally shorter cold ischemia time and were less likely to be placed on a pump than non-diabetic ECD organs. Recipients of kidneys from D-SCD were significantly younger than those transplanted with ECD organs, but had a similar gender distribution, BMI's, and times on the waitlist; they were less likely to experience delayed graft function.
Table 1.
Comparison of donor and recipient characteristics
| Non-diabetic SCD | Diabetic SCD | Non diabetic ECD | Diabetic ECD | p value | |
|---|---|---|---|---|---|
| N | 79,846 | 1982 | 11087 | 1076 | na |
| Donor age (years) | 30.6 ± 14.4 | 40.7 ± 12.6 | 60.5 ± 6.5a | 59.4 ± 6.2 | 0.0001 |
| Donor gender (% male) | 62.1 | 53.5 | 45.5a | 56.5 | <0.001 |
| Donor weight (Kg) | 71.9 ± 22.4 | 84.2 ± 26.1 | 78.6 ± 19a | 88.3 ± 20.8 | 0.0001 |
| History of hypertension (%) | 10 | 38.3 | 63.8a | 82.4 | <0.001 |
| Terminal creatinine (mg/dL) | 1.1 ± 1.3 | 1.12 ± 1.04 | 1.23 ± 1.58b | 1.3 ±1.8 | 0.0001 |
| Cold ischemia time (hours) | 18.9 ± 18.4 | 20.2 ± 8.3 | 20.7 ± 8.7b | 20.9 ± 8.5 | 0.0001 |
| Organ placed on pump (%) | 74.7 | 80.7 | 86.1b | 84.2 | <0.001 |
| Recipient age (years) | 44.6 ± 14 | 48.4 ± 13.4 | 53.1 ± 12.7a | 54.4 ± 12 | 0.0001 |
| Recipient gender (% male) | 60 | 59.6 | 61.4 | 61.3 | 0.028 |
| Recipient BMI (kg/m2) | 26.6. ± 5.5** | 27 ± 11.1 | 26.9 ± 5.5 | 26.9 ± 5.1 | 0.0001 |
| Recipient Diabetes (%) | 34.3 | 26.1 | 29.8 | 31 | <0.001 |
| HLA mismatch | 3.5 ± 1.8 | 3.5 ± 1.8 | 3.6 ± 1.7a | 3.7 ± 1.7 | 0.0001 |
| Patients with PRA > 80% | 7.38%c | 7.33%c | 4.71%c | 4.56%c | <0.001 |
| Patients with previous transplants | 13.1%c | 14.9%c | 9.04% | 7.90% | <0.001 |
| Waitlist duration (years) | 1.68 ± 1.65 | 1.95 ± 1.76 | 1.87 ± 1.66 | 1.90 ± 1.62 | 0.0001 |
| Delayed graft function (%) | 20.7 | 26.7 | 35a | 38.4 | <0.001 |
na = not applicable
Comparison of diabetic SCD and nondiabetic ECD p< 0.001
Comparison of diabetic SCD and nondiabetic ECD p< 0.05
Comparison of diabetic to nondiabetic donors (either ECD or SCD) were not significant
Using the Cox proportional hazards model for patients transplanted with D-SCD kidneys, we found that neither the gender or body mass index of the donor and recipient, nor a history of donor hypertension significantly influenced the outcomes of renal allografts, (see table 2). Neither preservation on a perfusion pump nor the total cold ischemia time of the donor organ appeared to significantly impact allograft survival in this study. However recipient and donor age, terminal donor creatinine, duration of diabetes in the donor, time spent by the recipient on the waitlist (rather than dialysis time) and the degree of HLA mismatch were found to significantly influence outcomes (table 2).(9) The factors that were found significant on univariate analysis were then included in the multivariate model, where donor age, recipient age and recipient BMI > 40 Kg/m2 remained significant. Models, adjusted for the same characteristics using death censored and overall graft survival for diabetic donors as well as all donors are included in the supplementary data section.
Table 2.
Cox proportional hazards model for kidney graft survival outcomes from diabetic SCD donors
| Univariate | Multivariate | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Hazard Ratio | Standard Error | z | p value | 95% Confidence Interval | Hazard Ratio | Standard Error | z | p value | 95% Confidence Interval | |
| Donor age | 1.011 | 0.003 | 3.16 | 0.002 | 1.004 – 1.017 | 1.017 | 0.6 | 3.11 | 0.002 | 1.007 – 1.029 |
| Male donor | 1.030 | 0.085 | 0.40 | 0.692 | 0.879 – 1.214 | |||||
| Donor creatinine | 1.059 | 0.025 | 2.47 | 0.014 | 1.012 – 1.109 | 1.05 | 0.031 | 1.73 | 0.084 | 0.993 – 1.115 |
| Donor weight (Kgs) | 1.000 | 0.002 | -0.11 | 0908 | 0996 – 1.002 | |||||
| Donor DM duration | 1.135 | 0.061 | 2.36 | 0.018 | 1.021 – 1.262 | 1.034 | 0.087 | 0.40 | 0.692 | 0.876 – 1.220 |
| Donor hypertension | 1.110 | 0.094 | 1.23 | 0.217 | 0.940 – 1.311 | |||||
| Cold ischemia time (hours) | 1.009 | 0.005 | 1.85 | 0.064 | 0.999 – 1.020 | |||||
| Organ pumped | 1.261 | 0.367 | 0.80 | 0.426 | 0.713 – 2.230 | |||||
| Recipient age | 0.990 | 0.003 | -3.33 | 0.001 | 0.984 – 0.996 | 0.969 | 0.005 | -5.85 | 0.000 | 0.958 – 0.979 |
| Male recipient | 1.027 | 0.086 | 0.32 | 0.749 | 0.872 – 1.209 | |||||
| Recipient BMI (<20 Kg/m2) | 1.236 | 0.038 | 6.91 | 0.000 | 1.164 – 1.312 | 0.603 | 0.166 | -1.84 | 0.066 | 0.352 – 1.034 |
| Recipient BMI (20-30 Kg/m2) | Ref | Ref | ||||||||
| Recipient BMI (30-40 Kg/m2) | 1.147 | 0.029 | 5.45 | 0.000 | 1.092 – 1.206 | 1.54 | 0.242 | 2.75 | 0.006 | 1.132 – 2.097 |
| Recipient BMI >40 Kg/m2) | 1.248 | 0.095 | 2.92 | 0.004 | 1.076 – 1.449 | 1.85 | 0.722 | 1.58 | 0.144 | 0.863 – 3.974 |
| Recipient Diabetes | 0.785 | 0.556 | -0.34 | 0.732 | 0.195 – 3.150 | |||||
| HLA mismatch | 1.083 | 0.025 | 3.43 | 0.001 | 1.035 – 1.135 | 1.069 | 0.042 | 1.68 | 0.092 | 0.989 – 1.155 |
| Time on waitlist | 1.052 | 0.024 | 2.22 | 0.027 | 1.006 – 1.010 | 1.071 | 0.398 | 1.85 | 0.064 | 0.995 – 1.152 |
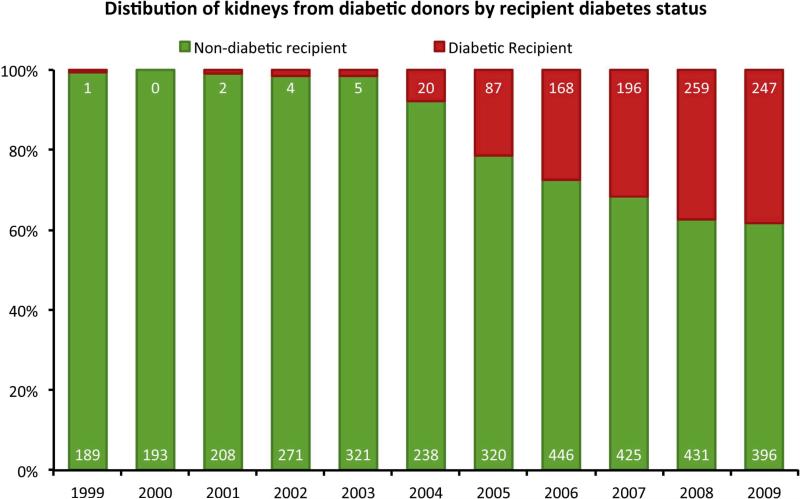
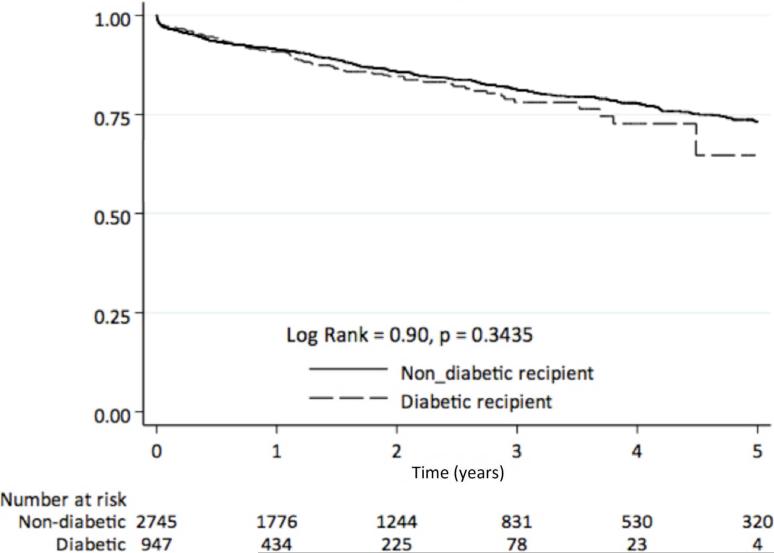
We have also found that in the past several years there has been a sharp increase in the use of organs from diabetic donors for diabetic recipients. The percentage of kidneys from diabetic donors transplanted into diabetic recipients rose significantly from 0 - 0.5% before 2002 to 38.4% in 2008 (Figure 4, χ2 >1000, p<0.001). While only 7 diabetic kidneys were transplanted into diabetic recipients prior to 2002, 259 diabetic recipients received diabetic donor kidneys in 2008. Overall graft survival of organs from diabetic donors was significantly worse among diabetic recipients than among non-diabetic recipients. (Figure 5a. Log Rank = 11.83, p=0.0006). However, Death censored survival of allografts obtained from diabetic donors was similar among diabetic and non-diabetic recipients for the period of available follow-up after transplantation (Figure 5b, Log rank =0.9, p=0.3435).
Figure 4.
Distribution of diabetes among recipients of kidneys obtained from deceased diabetic kidney donors. (Numbers on the bars represent the actual number of diabetic donor kidneys transplanted in each category of recipient for each year)
Figure 5a.
Comparison of renal allograft survival of organs obtained from diabetic donors directed to diabetic and non-diabetic recipients.
Figure 5b.
Comparison of overall renal allograft survival of organs obtained from diabetic donors directed to diabetic and non-diabetic recipients. (p=0.0006)
Discussion
We utilized the UNOS database to analyze the procurement and transplant rates of kidneys from deceased donors with diabetes mellitus, and the outcomes of transplantation with these kidneys. The overall number of deceased diabetic donor kidneys procured and transplanted has increased dramatically over the past decade. Despite the increase in the use of renal allografts from diabetic donors, there appears to be a relative paucity of data focusing on the outcomes of kidneys obtained from diabetic donors. A small single center in 2002 analysis demonstrated the absence of significant differences in graft survival between recipients of diabetic and non-diabetic donor kidneys.(6) An early analysis of the UNOS registry (2000) suggested a slightly lower 3-year graft survival (75% vs 72%) for organs from diabetic donors compared to controls. In this study, the duration of donor diabetes was not an independent predictor of outcomes.(10) A more recent propensity score matched comparison of diabetic donor outcomes also demonstrated statistically significant inferior outcomes for these organs but noted that the absolute difference in graft survival was small (hazard ratio of 1.11) over the 10 year study period, supporting the utilization of these organs.(8) In contrast, this analysis suggested that longer duration of diabetes in the donor was associated with worse outcomes.(8) The rising prevalence of obesity and diabetes in the population is changing the comorbidity profile of the deceased donor pool. This change is being accompanied by an increasing procurement rate of diabetic donor kidneys.
Before 2000, overall 15% of kidneys obtained from deceased donors were discarded – but over 50% of kidneys obtained from donors older than 60 were discarded.(11, 12) Appropriate characterization of kidneys from older donors and quantification in 2001 of the risk of graft failure associated with transplantation of such organs (eventually labeled as extended criteria donors) contributed to an increased use of ECD kidneys.(11, 12) Notably donor diabetes is not included as a part of the definition for extended criteria donors. Some centers reported doubling of their transplant volume with the use of ECD labeled organs for pre-selected recipients; there was a parallel increase in the number of recovered organs by organ procurement organizations from donors who were older than 60.(13-15) Following implementation of the ECD policy there was an increase in the allocation of ECD organs to older recipients shortening their time on the waiting list, and this appeared consistent with the analyses of certain patients are likely to benefit the most from the use of such organs.(16, 17)
Before discarding diabetic donor kidneys, one must consider the clear evidence that renal transplantation provides a significant survival benefit among patients with end stage renal disease as compared to hemodialysis.(18-20) This leads to an obvious impetus to increase the donor pool of usable kidneys. To accomplish this there is a need to develop a better understanding of outcomes associated with the use of organs from “marginal” donors. We need to expand the number of kidneys available for transplantation, and then ensure appropriate allocation of such organs to patients most likely to benefit and thus improve overall outcomes. Kidneys obtained from diabetic donors who may be best characterized as “marginal” may have a poorer outcome than those obtained with SCD kidneys but when D-SCD allograft survival is compared not with SCD organs but rather with survival of currently acceptable ECD kidneys, they have reasonable outcomes and provide a very useful organ donor source.
Inferior outcomes of grafts obtained from deceased diabetic donors in comparison to kidneys obtained from similar non-diabetic donors are not unexpected but they provide a potential source of organs for certain predefined recipients. Ten-year graft survival rates are 69.5% - 6.8% lower that those obtained from non-diabetic SCD kidneys (76.3%), but better than that seen with nondiabetic ECD kidneys (68.2%). It may be appropriate to develop formal allocation system for diabetic donor kidneys perhaps not unlike that used to optimize the use of ECD kidneys.
It is important to note from our study that survival and function of organs from standard criteria diabetic donors appear to be influenced by the duration of donor diabetes, age of the recipient, the degree of HLA mismatch and the recipient BMI (table 2). Interestingly, the age of older recipients appears to have a small protective effect on allograft survival of kidneys obtained from D-SCD.
The use of renal allografts obtained from D-SCDs appears to be associated with acceptable outcomes and such kidneys should be offered at least to certain select recipients. Patients who are euglycemic at the time of transplant and who are at low risk of developing new onset diabetes (e.g. BMI 20 -30 Kg/m2) after transplantation are theoretically most likely to benefit from a D-SCD kidney, particularly since early diabetic changes in the donor kidney may reverse with extended periods of euglycemia.(3, 21) However, the relatively recent and rapid increase in the use of allografts from diabetic donors into diabetic recipients (since 2002 to the present) has shown that early death censored graft outcomes are similar in both diabetic and non-diabetic recipients of these D-SCD kidneys (Figure 5). This suggests that at least certain select diabetic recipients may also be suitable candidates for renal allografts from D-SCD particularly when viewed in the context of poor diabetic patient survival on hemodialysis.(22, 23) Of note, overall graft outcomes with diabetic donor organs was significantly worse among diabetic recipients than among nondiabetic recipients. However, a detailed comparison of outcomes of these organs in diabetic and non-diabetic recipients and evaluation of the differences between the death censored and overall graft survival analysis is beyond the scope of our current discussion.
Our study represents the first attempt to categorize outcomes of allografts obtained from deceased diabetic donors (D-SCD) and to compare their survival with that of other donor kidneys obtained from non-diabetic donors – both SCD and ECD. The superior outcomes associated with renal allografts from D-SCDs when compared to ECD kidney outcomes, suggest that kidneys from D-SCD, with their relative abundance and superior outcomes relative to non-diabetic ECD donor kidneys, offer the opportunity to effectively further expand the deceased donor pool at least for certain carefully selected recipients.
Conclusion
There is a steady increase in the US in the number of kidneys being recovered and discarded from deceased diabetic donors. Our analysis of the UNOS database clearly demonstrates that acceptable renal allograft survival is obtainable with the use of kidneys from D-SCD's – even when the recipients are diabetic. Our results also suggest that kidneys obtained from standard criteria diabetic donors (D-SCD) have satisfactory outcomes that are superior to the graft survival seen with extended criteria donors (both diabetic and non-diabetic). These findings emphasize the need to develop a better understanding and methodology for evaluation and allocation of deceased diabetic donor kidneys in order to expand and improve utilization of this relatively untapped organ donor resource while ensuring acceptable and improved renal transplantation outcomes for patients with ESRD.
Supplementary Material
Acknowledgments
This work was supported in part by Health Resources and Services Administration contract 234-2005-370011C and in part by NIH 5T32HL007854-15 (MAH). The content is the responsibility of the authors alone and does not necessarily reflect the views or policies of the Department of Health and Human Services, nor does mention of trade names, commercial products, or organizations imply endorsement by the U.S. Government.
Footnotes
Disclosure statement
The authors of this manuscript have no conflicts of interest to disclose as described by the American Journal of Transplantation
Supporting Information
Additional Supporting Information may be found in the online version of this article:
References
- 1.Ramos E, Aoun S, Harmon WE. Expanding the Donor Pool: Effect on Graft Outcome. J Am Soc Nephrol. 2002;13(10):2590–2599. doi: 10.1097/01.asn.0000033462.66353.f5. [DOI] [PubMed] [Google Scholar]
- 2.Akinlolu OO, Alan BL, Jeffrey DP, Julie AH, David MD, Robert AW, et al. Impact of pre-existing donor hypertension and diabetes mellitus on cadaveric renal transplant outcomes. Am J Kid Dis. 2000;36(1):153–159. doi: 10.1053/ajkd.2000.8288. [DOI] [PubMed] [Google Scholar]
- 3.Abouna GM, Al-Adnani MS, Kremer GD, Kumar SA, Daddah SK, Kusma G. Reversal of diabetic nephropathy in human cadaveric kidneys after transplantation into non-diabetic recipients. Lancet. 1983;2(8362):1274–1276. doi: 10.1016/s0140-6736(83)91151-0. [DOI] [PubMed] [Google Scholar]
- 4.Abouna GM, Adnani MS, Kumar MS, Samhan SA. Fate of transplanted kidneys with diabetic nephropathy. Lancet. 1986;1(8481):622–623. doi: 10.1016/s0140-6736(86)92849-7. [DOI] [PubMed] [Google Scholar]
- 5.Orlowski JP, Spees EK, Aberle CL, Fitting KM. Successful use of kidneys from diabetic cadaver kidney donors: 67- and 44-month graft survival. Transplantation. 1994;57(7):1133–1134. [PubMed] [Google Scholar]
- 6.Becker YT, Leverson GE, D'Alessandro AM, Sollinger HW, Becker BN. Diabetic kidneys can safely expand the donor pool. Transplantation. 2002;74(1):141–145. doi: 10.1097/00007890-200207150-00027. [DOI] [PubMed] [Google Scholar]
- 7.van Goor H, Slooff MJ, Kremer GD, Tegzess AM. Results of transplantation of kidneys from diabetic donors. Proc Eur Dial Transplant Assoc Eur Ren Assoc. 1985;21:655–658. [PubMed] [Google Scholar]
- 8.Ahmad M, Cole EH, Cardella CJ, Cattran DC, Schiff J, Tinckam KJ, et al. Impact of deceased donor diabetes mellitus on kidney transplant outcomes: a propensity score-matched study. Transplantation. 2009;88(2):251–260. doi: 10.1097/TP.0b013e3181ac68a9. [DOI] [PubMed] [Google Scholar]
- 9.Schold JD, Sehgal AR, Srinivas TR, Poggio ED, Navaneethan SD, Kaplan B. Marked variation of the association of ESRD duration before and after wait listing on kidney transplant outcomes. Am J Transplant. 2010;10(9):2008–2016. doi: 10.1111/j.1600-6143.2010.03213.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ojo AO, Leichtman AB, Punch JD, Hanson JA, Dickinson DM, Wolfe RA, et al. Impact of pre-existing donor hypertension and diabetes mellitus on cadaveric renal transplant outcomes. Am J Kid Dis. 2000;36(1):153–159. doi: 10.1053/ajkd.2000.8288. [DOI] [PubMed] [Google Scholar]
- 11.Rosengard BR, Feng S, Alfrey EJ, Zaroff JG, Emond JC, Henry ML, et al. Report of the Crystal City Meeting to Maximize the Use of Organs Recovered from the Cadaver Donor. Am J Transplant. 2002;2(8):701–711. doi: 10.1034/j.1600-6143.2002.20804.x. [DOI] [PubMed] [Google Scholar]
- 12.Metzger RA, Delmonico FL, Feng S, Port FK, Wynn JJ, Merion RM. Expanded criteria donors for kidney transplantation. Am J Transplant. 2003;3(Suppl 4):114–125. doi: 10.1034/j.1600-6143.3.s4.11.x. [DOI] [PubMed] [Google Scholar]
- 13.Stratta RJ, Rohr MS, Sundberg AK, Armstrong G, Hairston G, Hartmann E, et al. Increased kidney transplantation utilizing expanded criteria deceased organ donors with results comparable to standard criteria donor transplant. Ann Surgery. 2004;239(5):688–695. doi: 10.1097/01.sla.0000124296.46712.67. discussion 695-687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hirth RA, Pan Q, Schaubel DE, Merion RM. Efficient Utilization of the Expanded Criteria Donor (ECD) Deceased Donor Kidney Pool: An Analysis of the Effect of Labeling. Am J Transplant. 2010;10(2):304–309. doi: 10.1111/j.1600-6143.2009.02937.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sung RS, Guidinger MK, Lake CD, McBride MA, Greenstein SM, Delmonico FL, et al. Impact of the expanded criteria donor allocation system on the use of expanded criteria donor kidneys. Transplantation. 2005;79(9):1257–1261. doi: 10.1097/01.tp.0000161225.89368.81. [DOI] [PubMed] [Google Scholar]
- 16.Schold JD, Howard RJ, Scicchitano MJ, Meier-Kriesche HU. The Expanded Criteria Donor Policy: An Evaluation of Program Objectives and Indirect Ramifications. Am J Transplant. 2006;6(7):1689–1695. doi: 10.1111/j.1600-6143.2006.01390.x. [DOI] [PubMed] [Google Scholar]
- 17.Ojo AO. Expanded criteria donors: process and outcomes. Semin Dial. 2005;18(6):463–468. doi: 10.1111/j.1525-139X.2005.00090.x. [DOI] [PubMed] [Google Scholar]
- 18.Wolfe RA, Ashby VB, Milford EL, Ojo AO, Ettenger RE, Agodoa LY, et al. Comparison of mortality in all patients on dialysis, patients on dialysis awaiting transplantation, and recipients of a first cadaveric transplant. New Engl J Med. 1999;341(23):1725–1730. doi: 10.1056/NEJM199912023412303. [DOI] [PubMed] [Google Scholar]
- 19.Oniscu GC, Brown H, Forsythe JL. Impact of cadaveric renal transplantation on survival in patients listed for transplantation. J Am Soc Nephrol. 2005;16(6):1859–1865. doi: 10.1681/ASN.2004121092. [DOI] [PubMed] [Google Scholar]
- 20.Meier-Kriesche HU, Ojo AO, Port FK, Arndorfer JA, Cibrik DM, Kaplan B. Survival improvement among patients with end-stage renal disease: trends over time for transplant recipients and wait-listed patients. J Am Soc Nephrol. 2001;12(6):1293–1296. doi: 10.1681/ASN.V1261293. [DOI] [PubMed] [Google Scholar]
- 21.Fioretto P, Steffes MW, Sutherland DER, Goetz FC, Mauer M. Reversal of Lesions of Diabetic Nephropathy after Pancreas Transplantation. N Engl J Med. 1998;339(2):69–75. doi: 10.1056/NEJM199807093390202. [DOI] [PubMed] [Google Scholar]
- 22.Hoffmann F, Haastert B, Koch M, Giani G, Glaeske G, Icks A. The effect of diabetes on incidence and mortality in end-stage renal disease in Germany. Nephrol DIal Transpl. 2011;26(5):1634–1640. doi: 10.1093/ndt/gfq609. [DOI] [PubMed] [Google Scholar]
- 23.Villar E, Polkinghorne KR, Chang SH, Chadban SJ, McDonald SP. Effect of type 2 diabetes on mortality risk associated with end-stage kidney disease. Diabetologia. 2009;52(12):2536–2541. doi: 10.1007/s00125-009-1525-2. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.