Abstract
The current study examined whether changes in maternal behaviors following an evidence-based treatment—Parent Child Interaction Therapy (PCIT)—was associated with improvements in cardiac vagal regulation in young children born premature. Participants included 28 young children (mean age = 37.79 months) that were born premature and presented with elevated externalizing behavior problems. To assess cardiac vagal regulation, resting measures of respiratory sinus arrhythmia (RSA) and RSA change (withdrawal or suppression) to a clean-up task were derived pre and post-treatment. Results indicated that an increase in behaviors mothers are taught to use during treatment (i.e., do skills—praise, reflection, and behavioral descriptions) were associated with an improvement in children’s post-treatment RSA suppression levels. The current study illustrates the important role of caregiver behavior in promoting physiological regulation in children born premature.
Keywords: cardiac vagal regulation, RSA suppression, emotion regulation, prematurity, child, parent training
1. Introduction
Broadly speaking, self-regulation refers to an individual’s efforts to alter his or her inner states or responses (Baumeister & Vohs, 2004). Recent work in both developmental and clinical psychology has noted a significant association between child self-regulation skills and adaptive functioning across a range of domains, such as behavioral, social, and academic (Baumeister & Vohs, 2004; Calkins & Fox, 2002; Graziano, Reavis, Keane, & Calkins, 2007; Keenan, 2000; Shaw, Keenan, Vondra, Delliquadri, & Giovannelli, 1997). Self-regulation is a multi-level construct with control efforts that rely on physiological, attentional, emotional, and behavioral processes. These processes are hierarchically organized and become more sophisticated and integrated throughout development (Calkins, 2007). For example, recent psychophysiological research has highlighted the maturation of the parasympathetic branch of the autonomic nervous system as a critical factor in supporting the development of these increasingly sophisticated biobehavioral regulation processes (Calkins, 2007; Porges, 2007). Specifically, cardiac vagal tone–an index of the parasympathetic influence on the heart–has emerged as a psychophysiological marker for many aspects of self-regulation (e.g., emotion regulation) in both children and adults (Beauchaine, 2001; Calkins, 1997; 2007; Grossman & Taylor, 2007; Porges, 1995; 2003; 2007).
Assessing the functional output of the vagal pathways on the heart is accomplished non-invasively by quantifying the amplitude of respiratory sinus arrhythmia (RSA), a component of heart rate variability. Research has indicated that RSA, under controlled respiratory conditions, is uninfluenced by variations in sympathetic activity, and provides a sensitive index of cardiac vagal tone, even when alterations in parasympathetic activity are small (Grossman, Stemmler, & Meinhardt, 1990). Of particular interest to researchers studying self-regulation is measurement of vagal regulation of the heart when the organism is challenged. Vagal regulation refers to a withdrawal in RSA during a challenging state (i.e., vagal tone decreases from baseline to challenging task, reflected by a positive vagal regulation score) or to an augmentation in RSA (i.e., vagal tone increases from baseline to challenging task, reflected by a negative vagal regulation score). According to polyvagal theory, successful vagal regulation is marked by RSA withdrawal, which is thought to facilitate a child’s ability to cope with challenging states by mediating metabolic output via heart rate increases (Porges, Doussard-Roosevelt, Portales, & Greenspan, 1996; Porges, 2003). Indeed, research has shown that young children with greater levels of RSA withdrawal or suppression display better self-regulation and active coping skills, social competence, sustained attention, and fewer behavior problems (Calkins, Graziano, & Keane, 2007; El-Sheikh & Whitson, 2006; Graziano, Keane, & Calkins, 2007; Porges, 1991; 1995; 2001; Porges et al., 1996; Propper & Moore, 2006; Wilson & Gottman, 1996; DeGangi, DiPietro, Greenspan, & Porges, 1991; Huffman et al., 1998; Calkins, 1997; Calkins & Dedmon, 2000; Calkins & Keane, 2004; Suess, Porges, & Plude, 1994). Given these findings, considerable empirical and theoretical research has recently been conducted to examine the predictors of individual differences in RSA suppression.
In the current study, we were particularly interested in the role of the caregiver behavior in supporting the development of vagal regulation. Research has documented that early in development, children’s successful self-regulation largely depends on caregiver support and flexible responding (Kopp, 1982; Calkins & Fox, 2002; Sroufe, 2000). Caregivers must be able to accurately read children’s signals/needs and respond in sensitive ways that minimize distress and encourage positive interactions. Maternal behaviors indicative of emotional support, such as the use of praise, display of warmth/positive affect, responsiveness and sensitivity, and taking the child’s developmental level into consideration are viewed as crucial scaffolding behaviors towards the development of self-regulation skills during infancy and throughout childhood (Landry, Miller-Loncar, Smith, & Swank, 2002). On the other hand, maternal behaviors that do not provide emotional support negatively affect children’s self-regulation development. For example, harsh parenting behaviors such as being hostile, punitive, and expressing high levels of negativity is associated with high levels of stress and emotional overarousal in children, which may affect their ability to self-regulate (Blair, 2002; Hoffman, 2000). Intrusive behaviors that are characterized by the use of excessive demands and re-directing without sensitivity to the child’s cues may be particularly frustrating for children who are beginning to engage in more autonomous behaviors (Calkins & Johnson, 1998).
While animal studies have clearly shown that caregiver behaviors can affect offspring’s stress reactivity and physiological regulation (Caldji et al., 1998; Calatayud, Coubard, & Belzung, 2004; Champagne & Meaney, 2001; Francis et al., 1999), fewer studies have examined similar association in humans. Preliminary findings indicate that children with higher RSA suppression tend to have mothers who concurrently display high levels of responsiveness/warmth, good co-regulated communication patterns, and low levels of intrusiveness/hostility (Calkins, Smith, & Gill, 1998; Haley & Stansbury, 2003; Kennedy, Rubin, Hastings, & Maisel, 2004; Moore & Calkins, 2004; Porter, 2003). The context of children’s physiological regulation also provides evidence for the importance of maternal behaviors as children display significantly greater RSA suppression during mother-child interaction tasks compared to more independent tasks (Calkins & Keane, 2004; Calkins, Graziano, Berdan, Keane, & Degnan, 2008). Additionally, greater levels of maternal sensitivity have also been shown to buffer genetic risk factors (e.g., DRD2 risk allele) in the prediction of infants’ RSA suppression levels (Propper et al., 2008). A longitudinal study also found that a maternal-child relationship quality consisting of low levels of hostility, high levels of positive behaviors, and low levels of parent-child dysfunctional interactions predicted improvements in children’s RSA suppression from age 2 to 5.5 (Calkins, et al., 2008). What remains unexplored, however, is the extent to which treatment targeting changes in parent-child interactions can also lead to improvements in young children’s vagal regulation.
Examining this research question within a sample of young children born premature is particularly relevant because of their well-documented difficulties in physiological and behavioral regulation thought to be due to prenatal and perinatal risk factors affecting brain stem and limbic functioning (Geva & Feldman, 2008; Minde, 2000). For example, research has demonstrated that preterm infants born premature display lower levels of baseline RSA and RSA suppression compared to full-term infants (Porges et al., 1996; Portales et al. 1997). The importance of preterm infants’ physiological regulation for later adaptive functioning has also been documented such that maturation of baseline RSA during infancy was associated with better social competence at 3 years of age (Doussard-Roosevelt, McClenny, & Porges, 2001). A more recent longitudinal study employed structural equation modeling to demonstrate that low baseline RSA of preterm neonates predicts a higher prevalence of behavior problems at 5 years both directly and indirectly via emotional and attentional processes during the first 2 years of life (Feldman, 2009). Given the above findings, determining the extent to which evidence-based interventions can improve underdeveloped physiological regulation in children born premature is of significant importance because it would provide information as to whether such treatments are targeting an underlying physiological mechanism that contributes to such adaptive functioning problems.
Parent-training interventions are the treatment of choice for young children with externalizing behavior problems (Eyberg, Nelson, & Boggs, 2008), who inherently have significant self-regulation difficulties across several domains (Keenan & Shaw, 2003). Parent-Child Interaction Therapy (PCIT) is an evidence-based parent-training intervention that been shown to be effective in reducing externalizing behavior problems in young children born premature (Bagner, Sheinkopf, Vohr, & Lester, 2010). Consistent with our discussion of caregiver behaviors that support children’s emotional functioning, in the first phase of PCIT (described in more depth in the Method section), parents are taught to use “do skills” (e.g., praise, reflection, behavioral descriptions) to improve warmth and responsiveness in the parent-child relationship during a child-directed play. Parents are also taught to avoid “don’t skills” (e.g., commands, questions, and negative statements) and ignore inappropriate child behaviors during a child-directed play.
The effectiveness of parent-training interventions such as PCIT in improving children’s behavioral regulation are well documented (Nixon, Sweeny, Erickson, & Touyz, 2003; Schuhmann, Foote, Eyberg, Boggs, & Algina, 1998; Zisser & Eyberg, 2010), but few treatment studies have measured changes in children’s physiological regulation. In addition, those studies have typically examined children’s physiological functioning as a moderator of treatment outcome rather than an outcome of treatment. For example, school-age children with higher baseline heart rate before treatment were reported by parents as having greater reductions in externalizing behavior problems after receiving Pelham’s 2-week summer treatment program (2000) in conjunction with a parent training component (Stadler, et al., 2008). Another significant limitation in these past studies is that physiological functioning was measured during a restful or baseline period and not in response to more challenging tasks. Therefore, children’s actual physiological regulation was not examined. In addition, none of these previous studies or any to our knowledge have examined whether an evidence-based intervention is associated with improvements in children’s RSA suppression.
The current study is the first to examine whether PCIT, an evidence-based intervention, is associated with improvements in children’s physiological regulation as indexed by RSA suppression. In addition, no study has examined the relationship between changes in physiological regulation and treatment response among children born premature, a population at risk for behavior problems and difficulties with physiological regulation (Geva & Feldman, 2008; Minde, 2000). Recent findings also show that infants born premature with low cardiac baseline vagal tone receive the lowest amounts of maternal supportive behavior (e.g., positive affect, affectionate touch) and infant-mother synchrony compared to infants born premature with high cardiac baseline vagal tone (Feldman & Eidelman, 2007). Given the susceptibility of dysregulated preterm infants in eliciting appropriate care, the focus on improving maternal interactions in PCIT represents an ideal evidence-based intervention to implement and study with this at-risk population.
Consistent with past developmental work in which positive caregiver behaviors that provide emotional support promote the development of self-regulation, we expected that mothers’ increase in do skills taught during PCIT to be associated with improvements in children’s RSA suppression. Given that PCIT also aims to decrease parent’s use of excessive questions, commands, and negative statements, a reduction in these don’t skills was also expected to be associated with improvements in children’s RSA suppression. Finally, it is important to examine an interactive effect between positive and negative parental behaviors on children’s physiological regulation. Specifically, past research examining the efficacy of PCIT has shown greater effect sizes in parents’ increase in use of do skills versus decrease in use of don’t skills following treatment (Bagner & Eyberg, 2007). It may be the case that increasing parents’ use of positive do skills is what is accounting for children’s improvements in various outcomes, even while parents continue to engage in some don’t skills. It is also important to note that the use of excessive commands that capture the essence of don’t skills are different from more hostile and punitive parenting behaviors that are associated with worse child outcomes, including physiological functioning (Calkins et al., 1998; Luecken & Lemery, 2004). Therefore, mothers’ improved use of do skills may buffer any potential negative association between continued use of don’t skills and children’s RSA suppression.
2. Method
2.1. Participants
Participants were 28 mothers and their child (Mean age = 37.79 months; SD = 13.29) who was born < 37 weeks gestation. Children were referred between August 2007 and December 2008 by the director (BRV) of a neonatal follow-up clinic (79%), health professionals at other pediatric sites (9%), staff at state-funded early intervention programs (6%), or self-referred by their mother after seeing a study brochure (6%). Children were mostly boys (71%), with a racial composition of 82% White, 10% Biracial, 4% African American, and 4% Asian, and 21% of children were Hispanic. Families had a mean Hollingshead (1975) score of 43.39 (SD = 13.21), which falls in the middle range of socioeconomic status.
For study inclusion, mothers had to rate their child above the clinically significant range on a measure of child externalizing behavior problems and be able to speak and understand English. Exclusion criteria for children included major sensory impairments (e.g., deafness, blindness), significant motor impairments (e.g., cerebral palsy significantly affecting mobility), and oxygen dependence for chronic lung disease. Children with symptoms of autism spectrum disorder were excluded at the screening evaluation (n = 2). Mothers had to obtain a score of at least 75 on a cognitive screening measure, but no mother was excluded based on this criterion. Seven children did not meet entry criteria at the screening evaluation due to scores below the borderline clinically significant range on the measure of externalizing behavior problems.
2.2. Screening Measures
Child Behavior Checklist for 1½ to 5 Year Olds (CBCL; Achenbach & Rescorla, 2001)
The CBCL is a 99-item parent-rating scale designed to measure the frequency of children’s behavior and emotional problems. The CBCL has demonstrated very good 8-day test-retest reliability (r = .68 to .92, mean r = .84), interrater reliability (mean mother-father r = .61, mean parent–child care provider r = .65), and success in discriminating between referred and nonreferred children (Achenbach & Rescorla, 2001). A T-score greater than 60 on the Externalizing Problems scale was required for study inclusion.
Modified Checklist for Autism in Toddlers (M-CHAT; Robins, Fein, Barton, & Green, 2001)
The M-CHAT is a 23-item parent-rating scale designed to identify children at risk for autism and is considered appropriate for children ages 18–48 months (Snow & Lecavalier, 2008). The M-CHAT was used for children between the ages of 18 and 48 months to exclude children with symptoms of autism spectrum disorder. Parent report in conjunction with clinical judgment was used for identification of autism in children older than 48 months.
Wechsler Abbreviated Scale of Intelligence (WASI; Wechsler, 1999)
The WASI is a short and reliable measure of intelligence that has high reliability and validity with other tests of intelligence (Hays, Reas, & Shaw, 2002). The WASI was used to exclude mothers with cognitive impairment.
2.3. Study Design and Procedure
This study was approved by the Hospital Institutional Review Board. A randomized, controlled trial was used to determine the efficacy of Parent-Child Interaction Therapy (PCIT) compared to a waitlist control (WL) comparison group. Results for this randomized trial have been reported elsewhere (XXX, 2010). For this study, we were interested in the effect of PCIT on physiological regulation for all children in the study that received PCIT. All families participated in a pretreatment assessment scheduled immediately prior to beginning treatment and a posttreatment assessment scheduled 4 months after the pretreatment assessment. Of the 28 families, 22 completed the posttreatment assessment. Six families (21%) withdrew from treatment and did not complete the posttreatment assessment.
At the pretreatment and posttreatment assessments, each mother and child were observed during a 10-min baseline period watching a pleasant video to obtain resting cardiac measures (HR and RSA). An undergraduate research assistant who was masked to intervention status coded the start and end time of the videos in order to determine the start and end time of the baseline period. Following the baseline episode, cardiac measures were collected during a clean-up task (5 min), in which mothers were instructed to have their child pick up all of the toys in the room. Four months after the pretreatment assessment, all families were seen for the posttreatment assessment, which included the same physiological data collection as the pretreatment assessment (baseline, mother-child interaction, and clean-up tasks). All assessments were conducted in the clinic.
2.4. Intervention Description
PCIT is a manualized parent-training intervention with extensive research demonstrating its efficacy and long-term maintenance in treating young children with disruptive behavior disorders (Blake, Rodriguez, & Bagner, in press; Eyberg, et al., 2008) and showing promise with other at-risk populations, such as children with abuse history (Chaffin, et al., 2004), chronic illness (Bagner, Fernandez, & Eyberg, 2004), and mental retardation (Bagner & Eyberg, 2007). With foundations in attachment and social learning theories, PCIT was designed to change parent-child interaction patterns and thereby change child disruptive behavior. Treatment progresses through two distinct phases: Child-Directed Interaction (CDI) resembles traditional play therapy, and Parent-Directed Interaction (PDI) resembles clinical behavior therapy.
During CDI, the parents follow their child’s lead in play by using the non-directive PRIDE (i.e., “do”) skills: Praising the child, Reflecting the child’s statements, Imitating the child’s play, Describing the child's behavior, and using Enthusiasm. They learn to direct the PRIDE skills to the child’s appropriate play and ignore undesirable behaviors. They also learn to avoid verbalizations that take the lead away from the child during the play (i.e., “don’t skills”), including questions, commands, and negative statements. During PDI, the parents set limits to reduce child noncompliance and negative behavior. They learn to use effective commands and consistently follow through with timeout for noncompliance. The PDI procedure is only used at times when it is important that the child obey a specific command. The parents are also taught variations of the PDI procedure to deal with aggressive behavior and public misbehavior. During all sessions, the therapist coaches each parent in-vivo through a one-way mirror (using a wireless headset) in their use of the CDI and PDI skills with their child.
PCIT sessions were conducted once a week for approximately 1 hour in length. In both phases of treatment, the therapist actively coaches parents toward mastery of the interaction skills as assessed during a 5-min parent-child observation at the start of each session. For this study, CDI was limited to five coaching sessions before beginning the PDI phase of treatment. However, CDI continued to be assessed and coached along with PDI skills in the PDI phase of treatment. Treatment is not time limited and continues until parents demonstrate mastery of the interaction skills (M treatment length = 13.05 sessions, SD = 2.18). In addition to helping parents master the CDI and PDI skills, additional procedures are used in PCIT to help reduce attrition, such as providing support to parents about concerns other than child management and making weekly reminder calls.
All therapy sessions were videotaped, and 25% were selected and coded for integrity by a research assistant uninvolved in coding behavioral observations. Accuracy, defined as the percent with which the therapist adhered to key elements of each session detailed in the treatment manual, was 94% (range = 89% – 99%).
2.5. Measures
Dyadic Parent-Child Interaction Coding System (DPICS)
The DPICS is a behavioral coding system with documented reliability and validity that measures the quality of the parent-child interactions (Eyberg, Nelson, Duke, & Boggs, 2004). Several categories of parent and child behaviors may be selected for coding. Behaviors are coded by recording the frequency of each occurrence in real time using a video coding system. Given this study’s focus on parenting behaviors during social interactions, we created a composite of do skills (behavior descriptions, reflections, praises) and don’t skills (questions, commands, and negative talk) reflecting behaviors parents are taught during treatment to use and not use during a child-led play. Undergraduate student coders, who were blind to children’s treatment status, were trained to 80% agreement with a criterion tape and coded 57% of the observations at the pretreatment a second time for reliability. Kappa for the do and don’t skills were .69 and .60, respectively.
Cardiac Vagal Tone (VT)
Two types of cardiac vagal regulation measures were derived from the laboratory assessments: baseline RSA and RSA suppression (i.e., baseline RSA – challenge RSA). RSA measures were derived from Electrocardiogram (ECG) signals that were recorded by telemetry and digitized at a 1 millisecond sampling rate using the BIOPAC MP100 Data Acquisition System (BIOPAC Systems Inc., Goleta, CA). ECG was acquired by placing three electrodes on the child’s chest and abdomen. The electrodes were connected to a wireless transmitter, stored in a small backpack worn by the child, and sent to a PC in an adjacent observation room. The electrocardiogram (ECG) signal was digitized and recorded, with heart beats represented by the presence and timing of the R-waves in the ECG signal and heart period calculated from the interval between R-waves. RSA was derived from time-series analysis of R–R intervals from digitized ECG recordings. HR was derived from interbeat intervals defined by detection of R-waves to the nearest millisecond. The system coordinated behavioral events and physiological signals by marking the videotape and physiological data with the same time stamp.
In accordance with recent recommendations (Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology, 1996), RSA values were calculated based on a combination of an automated approach and a manual approach (Berntson, et al., 1997). First, postprocessing of the ECG took place offline by use of a series of automated algorithms. To control for movement-related artifact, including activity level of the child, artifact detection for the ECG time series used a moving confidence interval that detected R–R intervals outside of expected values. Missed or spurious R-waves were detected, flagged, and corrected by linear interpolation. Subsequent processing employed a time-series analysis and a moving polynomial filter to remove low frequency trends in the ECG signal. This process removes periodicities in the ECG signal that are outside the frequency range of the respiratory cycle.
Second, following the automated approach of interpolating abnormal R – R intervals, RSA values were calculated based on a set of stringent criteria. Baseline RSA was collected during a 10-min baseline period and represents an average score of the first continuous 2 min with no more than 15% artifact rates on average. RSA collected during the clean-up task represents an average score of the middle 2 min of each task with no more than 15% artifact rates on average. Estimates of RSA were calculated using Porges’ (1985) method to analyze the interbeat intervals (IBI) data. This method applies an algorithm to the sequential heart period data. The algorithm uses a moving 21-point polynomial to detrend periodicities in heart period (HP) slower than RSA. A band-pass filter then extracts the variance of HP within the frequency band of spontaneous respiration in young children, 0.24–1.04 Hz. Although lower frequency bands may be studied, research with young children has consistently examined this band and identified associations to child functioning (Huffman, et al., 1998; Porges et al., 1996).
The estimate of RSA was derived by calculating the natural log of this variance and is reported in units of ln(msec)2. Descriptive statistics for RSA for the baseline and challenge episodes are reported in Table 1. Vagal regulation scores indexed by change scores were computed for each challenge episode by subtracting the challenge episode RSA from the baseline RSA. These change scores are also reported in Table 1. Consistent with previous research methodology (Blair & Peters, 2003; Calkins & Keane, 2004; Graziano et al., 2007; Porges et al., 1996), positive change scores indicate a decrease in RSA from baseline to task (i.e., RSA withdrawal or suppression). Only RSA collected during the clean-up task was used in the calculation of a RSA suppression score. The clean-up situation was used as the stressor condition because it is a situation most young children resist (Miron, Marva, &Zeanah, 2009), particularly children with externalizing behavior problems. In addition, baseline levels of RSA are predictive of change scores of RSA, so baseline levels were also covaried.
Table 1.
Descriptive statistics for Parenting and Physiological Regulation Measures
| M | SD | Min | Max | |
|---|---|---|---|---|
| Parenting Measures | ||||
| Pre-treatment: “Do skills” | 6.64 | 6.49 | 0 | 27 |
| Pre-treatment: “Don’t skills” | 36.4 | 16.54 | 9 | 61 |
| Post-treatment: “Do skills” | 15.73 | 10.59 | 2 | 29 |
| Post-treatment: “Don’t skills” | 11.10 | 7.85 | 2 | 29 |
| Physiological Measures | ||||
| Pre-treatment: Baseline RSA | 6.05 | 1.58 | 1.91 | 8.23 |
| Pre-treatment: Clean-up RSA | 5.62 | 1.23 | 2.28 | 7.33 |
| Post-treatment: Baseline RSA | 6.12 | 1.29 | 3.22 | 8.35 |
| Post-treatment: Clean-up RSA | 5.68 | .91 | 3.93 | 7.55 |
| RSA Suppression Scoresa | ||||
| Pre-treatment: Clean-up | .44 | 1.38 | −2.36 | 2.64 |
| Post-treatment: Clean-up | .45 | .88 | −.83 | 2.29 |
RSA= respiratory sinus arrhythmia,
Positive change scores indicate a decrease in RSA from baseline to task (i.e., RSA suppression)
2.6. Data Analysis Plan
In this study, we focused on examining whether changes in observed parenting skills (i.e., do and don’t skills) following treatment are associated with improved physiological functioning among children born premature. First, initial paired-sample t-tests were conducted to determine whether parents’ use of do skills increased and don’t skills decreased between the pre and posttreatment assessments. Second, regression analyses were conducted to determine whether changes in these parenting skills predicted changes in children’s physiological regulation as measured via RSA suppression. Finally, we examined an interaction between changes in do skills and don’t skills to determine whether improved positive do skills can buffer the potential negative aspects of parents not decreasing their don’t skills during treatment.
2.7. Missing Data
Missing data was minimal. Baseline RSA data was not collected in 2 children due to technological problems. RSA data was also not collected from the 6 families that did not complete the posttreatment assessment. RSA scores were imputed using the expectation maximization (EM) method as implemented in SPSS. There were no statistically significant differences between the families with missing data (n = 8) and those without missing data (n = 20) on any of the RSA measures and other baselines measures (e.g., demographic variables, pretreatment parent behaviors). Additionally, results were the same when examining only children with complete data.
3. Results
3.1. Preliminary Analyses
Preliminary analyses examined whether there were any relations between demographic variables and the physiological measures of baseline and task RSA and parenting measures of do skills and don’t skills. Consistent with previous research (Calkins & Keane, 2004; Kennedy et al., 2004), children’s age was significantly associated with pre-treatment baseline RSA (r = .41, p < .05) with older children displaying higher baseline levels of RSA. Additionally, the length of treatment sessions was negatively associated with pre-treatment RSA suppression levels (r = −.50, p < .05) such that families who needed more sessions to complete PCIT had children with lower levels of RSA suppression before treatment started. There were no other significant associations between demographic variables and the physiological and parenting measures. It is also important to note that no indices of prematurity, prenatal or perinatal factors were related to any of our independent or dependent variables. Therefore, only age and length of treatment were covaried in subsequent analyses.
3.2. Changes in Parenting Skills Following PCIT Treatment
Paired-sample t-tests indicated significant changes in both do skills and don’t skills from pre to posttreatment, t(27) = 5.69, p < .001, Cohen’s d = 2.19, and t(27) = −7.64, p < .001, Cohen’s d = 2.94, respectively. Specifically, mothers were observed as displaying significantly greater do skills at post-treatment (M = 15.42, SD = 7.78) compared to pre-treatment (M = 6.78, SD = 6.14) and fewer don’t skills at post-treatment (M = 12.05, SD = 7.25) compared to pre-treatment (M = 36.84, SD = 15.66).
3.3. Changes in Parenting Skills and Children’s Physiological Regulation
Regression analyses were conducted to determine whether changes in parenting skills predicted changes in children’s physiological regulation as measured via RSA suppression. Pretreatment parenting skills and RSA suppression were placed in the first step of the regression analyses as control variables. Given the association between children’s age with baseline RSA and the association between treatment length and pre-treatment RSA suppression, as well as the associations between baseline RSA and RSA suppression, age, treatment length, and baseline RSA measures were also covaried. The main effects of post-treatment parenting skills were then placed in the second step of the regression with post-treatment RSA suppression as the dependent variable. Controlling for pre-treatment parenting skills allows us to interpret the simple main effects of posttreatment parenting skills as actual change in parenting skills between the pre and posttreatment assessments and is a preferred statistical method compared to computing raw change scores (Cohen, Cohen, West, & Aiken, 2003). The interaction between do skills and don’t skills post-treatment was placed in the third step of the regression. As recommended by Jaccard and Turrisi (2003), all covariates and independent variables were mean centered. Due to the number of predictors/covariates in our regression model, collinearity statistics were examined and results suggested no problems with multi-collinearity among the predictor variables (VIF < 10 and Tolerance values >.10 for all variables).
In terms of the control variables and as displayed in Table 2, only postreatment baseline RSA was positively associated with posttreatment RSA suppression. Hence, higher levels of baseline RSA during posttreatment was associated with higher levels of RSA suppression at the end of treatment. No other control variable was significantly associated with posttreatment RSA suppression. In terms of the main effects, parents’ use of do skills post-treatment was positively associated with posttreatment RSA suppression such that improvements in the use of do skills was positively associated with improvements in RSA suppression (p < . 03, Cohen’s d = .68). Of note, 45% of the sample experienced a meaningful improvement in RSA suppression (i.e., greater than 1 SE of the M). However, there was a marginally significant interaction between do and don’t skills in predicting posttreatment RSA suppression (p < .09, Cohen’s d = .46).
Table 2.
Regression analyses testing post-treatment parenting “Do skills” and “Don’t skills” as predictors of change in children’s RSA suppression
| β | R2 | R2 Change | F Change | |
|---|---|---|---|---|
| Step 1. | .70 | .70 | 4.37* | |
| Age | .02 (.00) | |||
| Number of treatment sessions | −.09 (−.03) | |||
| Pre-treatment Baseline RSA | −.58 (−.29) | |||
| Post-treatment Baseline RSA | .82 (.54)*** | |||
| Pre-treatment RSA suppression | .59 (.36)+ | |||
| Pre-treatment “Do skills” | −.26 (−.03) | |||
| Pre-treatment “Don’t skills” | .20 (.01) | |||
| Step 2. | .81 | .11 | 3.16+ | |
| Post-treatment “Do skills” | .82 (.07)* | |||
| Post-treatment “Don’t skills” | .60 (.06)+ | |||
| Step 3. | .87 | .05 | 3.78+ | |
| Interaction between post-treatment “Do skills” and “Don’t skills” | .42 (.01)+ |
p <.09,
p <.05,
p < .01,
p < .001.
Note scores in parentheses represent unstandardized beta weights).
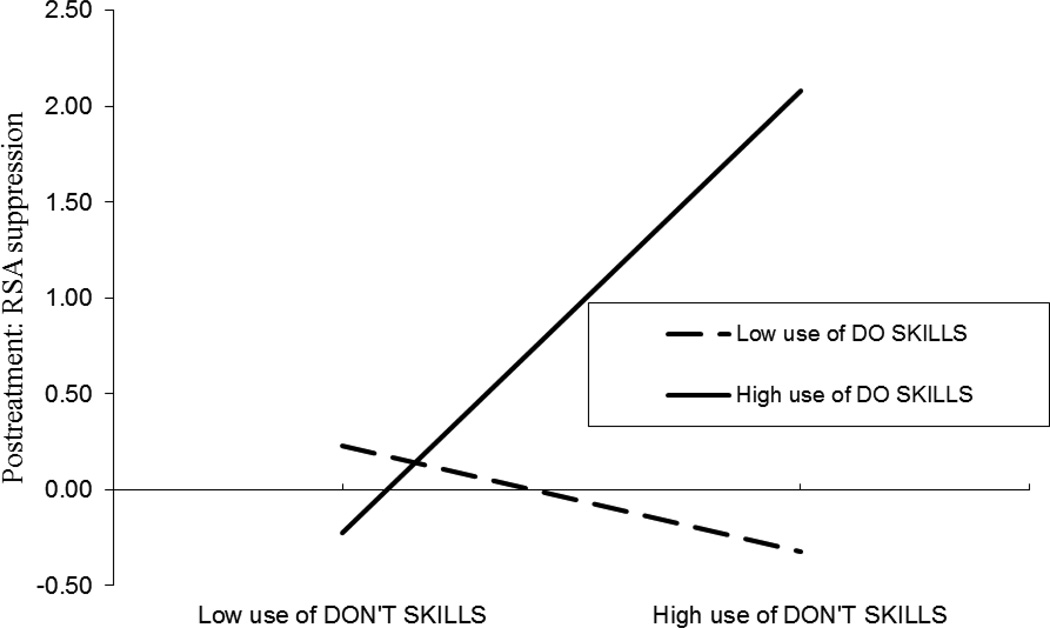
Following procedures outlined by Aiken and West (1991), these interactions were plotted by regressing posttreatment RSA suppression (y) on the don’t skills (x) as a function of two values of do skills, ZL and ZH (i.e., one standard deviation below the mean and one standard deviation above the mean, respectively). Unstandardized B was used to calculate the regression lines. As depicted in Figure 1, mothers’ high use of do skills buffered the negative effect of mothers’ high use of don’t skills on children’s RSA suppression. Finally, t-tests were computed, using Hayes and Matthes’ (2009) macro, to determine whether the slopes of the lines plotted in Figure 1 were significantly different from zero. The resulting t-tests indicated that for Figure 1, the slope for low use of do skills was not significantly different from zero, t(27) = .55, p = .59, b = .02 whereas the slope for high use of do skills was significantly different from zero, t(27) = 2.28, p < .05, b = .12, Cohen’s d = .88.
Figure 1.
Interaction between posttreatment DO and DON'T skills in predicting posttreatment children’s RSA suppression. Note. Interaction controls for pretreatment parenting skills and RSA measures.
4. Discussion
The current study examined whether changes in maternal behavior following PCIT, an evidence-based parent-training intervention, were associated with changes in children’s physiological regulation capabilities as indexed by RSA suppression. We examined this question with an at-risk sample of children who were born premature given their well-documented physiological and behavioral regulation difficulties (Geva & Feldman, 2008; Minde, 2000). First, it is important to note that mothers who completed PCIT displayed significant changes in parenting behaviors as measured via observational coding. Specifically, mothers displayed significantly improved positive interactions with their children at the end of treatment as evidenced by increased use of do skills (i.e., praise, reflections, and behavioral descriptions) during the child-directed play. Mothers were also successful in being less directive in the child-directed play by reducing the use of don’t skills (i.e., commands, questions, and negative statements). Given these observed changes in parental behaviors, which are well-documented in other PCIT efficacy studies (e.g., Bagner & Eyberg, 2007; Schuhmann, Foote, Eyberg, Boggs, & Algina, 1998; Nixon, Sweeney, Erickson, & Touyz, 2003), we were then able to examine whether these changes were related to children’s physiological regulation.
Consistent with our hypotheses, we found that improvements in parental use of do skills predicted improvements in children’s RSA suppression. It is important to note that this finding emerged even after controlling for baseline levels of RSA that are well-documented to influence levels of RSA suppression (Porges et al., 1996; Calkins et al., 2008; Graziano et al., 2007). However, in contrast to our hypothesis, no association was found between parental decrease of the use of don’t skills and children’s physiological regulation. Our simple main effect was also qualified by a marginally significant interaction between do skills and don’t skills in predicting RSA suppression. Specifically, the association between mothers’ high use of do skills and children’s RSA suppression is greatest while mothers are also using high levels of don’t skills. This finding is consistent with our hypothesis that high use of positive parenting behaviors (i.e., do skills) would buffer the negative association of don’t skills and children’s physiological regulation.
As mentioned in the introduction, the use of excessive commands and questions that capture the essence of don’t skills are different from more hostile and punitive parenting behaviors that are associated with worse child outcomes, including physiological functioning (Calkins et al., 1998; Luecken & Lemery, 2004). In fact, in our study, there were relatively few negative statements/criticisms (M = 7.36, SD = 7.12) or physical touches (M = 3.24, SD = 5.07) displayed by mothers compared to commands and questions (M = 36.4, SD =16.54). It may be the case that for parents who display high levels of do skills, their high use of don’t skills are more indicative of high levels of overall communication or expressiveness, which also involves commands and questions.
From a Vygotskian perspective, caregivers use of leading questions are seen as verbal problem-solving strategies aimed at facilitating the child’s self-regulation development by improving his or her language skills (Vygotsky, 1978; Berk & Winsler, 1995). Significant research has documented the important association between maternal speech, including the use of questions and prompts, and children’s language abilities (Hoff, 2003; Tamis-LeMonda, Bornstein, & Baumwell, 2001). The importance of children’s language abilities for their self-regulation skills is also well-documented (Kopp, 1989; Stansbury & Zimmerman, 1999). For example, a recent study using growth curve modeling showed that toddlers’ expressive language skills at 2 years of age predicted growth in self-regulation (Vallotton & Ayoub, in press). The internalization of language (i.e., use of private speech) across development is also well-documented and is associated with children’s behavioral regulation (Barkley, 1997; Winsler, 1998). Greater physiological regulation, as index by RSA suppression, has also been found to predict language scores in infants, especially for boys (Suess & Bornstein, 2000). Future research should clarify what types of verbal communication expressed by mothers (e.g., use of questions versus behavioral descriptions) relate to their children’s language skills and subsequent self-regulation. This type of research would provide important information as to the mechanisms of PCIT and the importance of reinforcing and reducing certain patterns of communication in treatment. It would be important for future research to clarify whether the link between mothers’ use of do skills and children’s RSA suppression is mediated by children’s language abilities and/or that mothers of children with better language skills have an easier time implementing the do skills they learn during PCIT.
Our findings indicate that parents who use high levels of praise/responsiveness (i.e., do skills) have children who show greater improvement in physiological regulation across treatment. Past research examining the efficacy of PCIT has shown greater effect sizes in parents’ increase use of do skills versus don’t skills following treatment (Bagner & Eyberg, 2007). Our findings further support the notion that increasing parents’ use of positive do skills is what is accounting for children’s improvements in various outcomes, not just simply decreasing some of their negative don’t skills. This may have significant implications for treatment and suggests that clinicians should focus more on increasing parents’ use of do skills than on reducing parents’ use of don’t skills, particularly commands and questions. Indirectly this focus on increasing do skills may lead to lower drop-out rates for families by focusing more on increasing the positive skills to their already formed parenting basis (Miller & Rollnick, 2002). Similarly, longer duration of PCIT treatment was negatively associated with RSA suppression such that families who took longer to complete PCIT had children with lower levels of pre-treatment RSA suppression. Children with poorer physiological regulation may make it more difficult for parents to implement newly learn skills and/or may need a longer period of time to respond to these skills via observable improvements in behaviors that often accompany improved physiological regulation. While the current results suggest possibilities for adaptations of PCIT (e.g., focus more on the do skills) for children with poor physiological regulation, any changes should be empirically tested before implementation.
Our findings also contribute to the emergent literature on the psychobiological influence of caregiver’s behaviors (Calkins & Hill, 2007; Calkins et al., 2008; Propper & Moore, 2006; Propper et al., 2008) by showing how changes in parenting behaviors, most notably positive behaviors, are associated with positive changes in children’s cardiac vagal regulation as index by RSA suppression. Obtaining this finding with children born premature is especially important given their high-risk status for behavioral and physiological regulation difficulties (Geva & Feldman, 2008; Minde, 2000), as well as the finding that those with low baseline RSA receive lower amounts of maternal supportive behaviors, such as affectionate touch (Feldman & Eidelman, 2007). It is important to note that it remains unclear whether mothers of infants born premature are deliberately avoiding greater supportive behaviors (e.g., affectionate touch) so as to avoid over-stimulating these infants until they have matured. Nevertheless, research on preterm infants has shown the power of mother-infant skin-to-skin contact in improving the infant’s physiological functioning, such as respiratory patterns, oxygen saturation, bradycardia, and weight gain (Acolet, Sleath, Whitelaw, 1989; Ludington-Hoe, Hashemi, Argote, Medellin, & Rey, 1992), as well as improving their cognitive and motor development (Feldman, Eidelman, Sirota, & Weller, 2002). Specifically related to our interest in physiological regulation, a recent study also indicated how such mother-infant-skin contact promotes higher baseline RSA and lower cortisol reactivity (Feldman, Singer, & Zagoory, 2010). Our study extends such research by showing that improved levels of maternal verbal praise and responsiveness can also provide physiological regulation benefits, as indexed by RSA suppression, to toddlers and young children.
There were some limitations to the current study that need to be addressed. First, while our analyses were statistically significant for the main effect of change in do skills in predicting children’s RSA suppression, the sample size was relatively small with the interaction only being marginally significant. While our results should be replicated in a larger sample, it is important to note that PCIT studies generally demonstrate large effect sizes (Nixon et al., 2003; Schuhmann et al., 1998) which allow for the use of smaller samples. Second, there was no control group of children that were born full term. Therefore, it would be important to examine whether changes in parenting behaviors during treatment are associated with changes in the physiological regulation of children born full-term or whether this effect is specific to children born premature. A no treatment comparison group would also be an important next step given that baseline RSA, which influences the degree of RSA suppression, is known to increase normatively over the first years of life (Izard et al., 1991; Calkins et al., 2008; Kennedy et al., 2004). Additionally, it is important to note that we did not assess the father-child interaction. Given that mother and fathers interact differently with their children, with fathers proportionally spending more of their interactions with children in a play setting (see Lamb, 2010 for a review), it will be important to determine whether changes in fathers’ interaction style also relate to observable physiological regulation changes in their children. Lastly, given the small sample, we did not have sufficient power to examine separate aspects of both do skills and don’t skills in order to examine if there are specific skills that are more important for promoting children’s physiological regulation. It would be interesting to examine whether parents who use high levels of do skills can continue to use some don’t skills (e.g., questions), which may promote language skills. Given that the overall use of negative statements was low in our sample, it will be important for future research to examine this hypothesis in a higher risk population, such as parents with a history of physically abusing their children.
In sum, the current study focused on a novel and relatively unexplored research question by examining the extent to which observed changes in maternal behavior following an evidence-based parent training treatment (i.e., PCIT) relates to changes in children’s physiological regulation as indexed by RSA suppression. Addressing this question in sample of children born premature, an at-risk population for impaired physiological regulation, represents another unique aspect of this study. The preliminary finding that parents who show greater improvements in their use of praise/responsiveness (i.e., do skills) have children who show greater improvement in physiological regulation across treatment has implications to improve treatment (e.g., having clinicians focusing more on improving parental warmth/responsiveness). Conducting a randomized treatment study of PCIT in which half of the families focus only on improving the do skills while the other half completes a typical treatment that focuses on both do skills and don’t skills would provide information as to the optimal parental behaviors that are associated with both behavioral and physiological regulation success.
In addition, while the role of the parasympathetic nervous system for children’s self-regulation is important and well-documented (Calkins, 2007; Porges, 2007), recent research has highlighted the importance of obtaining multiple physiological measures of self-regulation, including those tapping into the sympathetic nervous system. For example, research within the developmental literature suggests that coinhibition of parasympathetic and sympathetic activity constitute higher risks for the development of externalizing problems that are characterized by self-regulation deficits (El-Sheikh et al., 2009; Beauchaine, Gatzke-Kopp, & Mead, 2007). Hence, future research should examine whether the effect of an evidence-based intervention like PCIT on children’s self-regulation skills are also observed via specific sympathetic linked cardiac activity such as preejection periods (PEP) or cortisol reactivity. Lastly, it will be important for future research to demonstrate the extent to which observed physiological regulation changes relate to children’s behavioral regulation (e.g., performance on a delay of gratification task), as it would provide a more comprehensive understanding of the mechanisms of psychosocial treatment for young children with behavioral problems.
Highlights.
Changes in parenting skills were observed following an evidence-based behavioral treatment
Improvement in positive parenting skills was associated with young children’s RSA suppression
Caregiver behavior promotes physiological regulation in young children born premature.
Acknowledgments
This research was supported by a National Institute of Child Health and Human Development and National Institute of Mental Health awards (F32 HD056748 and K23 MH085659) to the second author.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Achenbach TM, Rescorla LA. Manual for the ASEBA Preschool Forms & Profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, & Families; 2001. [Google Scholar]
- Acolet D, Sleath K, Whitelaw A. Oxygenation, heart rate and temperature in very low birth infants during skin-to-skin contact with their mothers. Acta Paediatrica. 1989;78:189–193. doi: 10.1111/j.1651-2227.1989.tb11055.x. [DOI] [PubMed] [Google Scholar]
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Newbury Park, CA: Sage; 1991. [Google Scholar]
- Bagner DM, Eyberg SM. Parent-child interaction therapy for disruptive behavior in children with mental retardation: a randomized controlled trial. Journal of Clinical Child and Adolescent Psychology. 2007;36:418–429. doi: 10.1080/15374410701448448. [DOI] [PubMed] [Google Scholar]
- Bagner DM, Fernandez MA, Eyberg SM. Parent-child interaction therapy and chronic illness: A case study. Journal of Clinical Psychology in Medical Settings. 2004;11:1–6. [Google Scholar]
- Bagner DM, Sheinkopf SJ, Vohr BR, Lester BM. Parenting Intervention for Externalizing Behavior Problems in Children Born Premature: An Initial Examination. Journal of Developmental and Behavioral Pediatrics. 2010;31:209–216. doi: 10.1097/DBP.0b013e3181d5a294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barkley R. Attention-deficit/hyperactivity disorder, self-regulation, and time: Toward a more comprehensive theory. Journal of Developmental & Behavioral Pediatrics. 1997;18:271–279. [PubMed] [Google Scholar]
- Baumeister R, Vohs K. Handbook of self-regulation: Research, theory, and applications. New York, NY US: Guilford Press; 2004. [Google Scholar]
- Beauchaine TP. Vagal tone, development, and Gray's motivational theory: toward an integrated model of autonomic nervous system functioning in psychopathology. Developmental Psychopathology. 2001;13:183–214. doi: 10.1017/s0954579401002012. [DOI] [PubMed] [Google Scholar]
- Beauchaine TP, Gatzke-Kopp L, Mead HK. Polyvagal Theory and developmental psychopathology: emotion dysregulation and conduct problems from preschool to adolescence. Biological Psychology. 2007;74:174–184. doi: 10.1016/j.biopsycho.2005.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berk LE, Winsler A. Scaffolding children's learning. Vygotsky and early childhood education. Washington, DC: National Association for the Education of Young Children; 1995. [Google Scholar]
- Berntson GG, Bigger JT, Jr, Eckberg DL, Grossman P, Kaufmann PG, Malik M, et al. Heart rate variability: origins, methods, and interpretive caveats. Psychophysiology. 1997;34:623–648. doi: 10.1111/j.1469-8986.1997.tb02140.x. [DOI] [PubMed] [Google Scholar]
- Blair C. School readiness: Integrating cognition and emotion in a neurobiological conceptualization of children’s functioning at school entry. American Psychologist. 2002;57(2):111–127. doi: 10.1037//0003-066x.57.2.111. [DOI] [PubMed] [Google Scholar]
- Blair C, Peters R. Physiological and neurocognitive correlates of adaptive behavior in preschool among children in Head Start. Developmental Neuropsychology. 2003;24:479–497. doi: 10.1207/S15326942DN2401_04. [DOI] [PubMed] [Google Scholar]
- Blake CA, Rodríguez GM, Bagner DM. Parent-child interaction therapy. In: Clements P, Seedat S, editors. Mental health issues of child maltreatment. St. Louis: STM Learning; (in press). [Google Scholar]
- Calatayud F, Coubard S, Belzung C. Emotional reactivity may not be inherited but influenced by parents. Physiology & Behavior. 2004;80:465–474. doi: 10.1016/j.physbeh.2003.10.001. [DOI] [PubMed] [Google Scholar]
- Caldji C, Tannenbaum B, Sharma S, Francis D, Plotsky PM, Meaney MJ. Maternal care during infancy regulates the development of neural systems mediating the expression of fearfulness in the rat. Neurobiology. 1998;9:5335–5340. doi: 10.1073/pnas.95.9.5335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calkins S. Cardiac vagal tone indices of temperamental reactivity and behavioral regulation in young children. Developmental Psychobiology. 1997;31:125–135. doi: 10.1002/(sici)1098-2302(199709)31:2<125::aid-dev5>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- Calkins S. The emergence of self-regulation: Biological and behavioral control mechanisms supporting toddler competencies. In: Brownell C, Kopp C, editors. Socioemotional Development in the Toddler Years. New York: The Guilford Press; 2007. pp. 261–284. [Google Scholar]
- Calkins SD, Dedmon SE. Physiological and behavioral regulation in two-year-old children with aggressive/destructive behavior problems. Journal of Abnormal Child Psychology. 2000;28:103–118. doi: 10.1023/a:1005112912906. [DOI] [PubMed] [Google Scholar]
- Calkins S, Fox N. Self-regulatory processes in early personality development: a multilevel approach to the study of childhood social withdrawal and aggression. Development and Psychopathology. 2002;14:477–498. doi: 10.1017/s095457940200305x. [DOI] [PubMed] [Google Scholar]
- Calkins S, Graziano P, Berdan L, Keane S, Degnan K. Predicting cardiac vagal regulation in early childhood from maternal-child relationship quality during toddlerhood. Developmental Psychobiology. 2008;50:751–766. doi: 10.1002/dev.20344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calkins SD, Graziano P, Keane SP. Cardiac vagal regulation differentiates among children at risk for behavior problems. Biological Psychology. 2007;74:144–153. doi: 10.1016/j.biopsycho.2006.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calkins SD, Hill AL. Caregiver influences on emerging emotion regulation: Biological and environmental transactions in early development. In: Gross J, editor. Handbook of emotion regulation. New York: The Guilford Press; 2007. pp. 229–248. [Google Scholar]
- Calkins SD, Keane SP. Cardiac vagal regulation across the preschool period: Stability, continuity, and implications for childhood adjustment. Developmental Psychobiology. 2004;45:101–112. doi: 10.1002/dev.20020. [DOI] [PubMed] [Google Scholar]
- Calkins SD, Smith CL, Gill KL. Maternal interactive style across contexts: Relations to emotional, behavioral, and physiological regulation during toddlerhood. Social Development. 1998;7:350–369. [Google Scholar]
- Chaffin M, Silovsky JF, Funderburk B, Valle LA, Brestan EV, Balachova T, et al. Parent-child interaction therapy with physically abusive parents: efficacy for reducing future abuse reports. Journal of Consulting and Clinical Psychology. 2004;72:500–510. doi: 10.1037/0022-006X.72.3.500. [DOI] [PubMed] [Google Scholar]
- Champagne F, Meaney MJ. Like mother, like daughter: Evidence for non-genetic transmission of parental behavior and stress responsivity. Progressive Brain Research. 2001;133:287–302. doi: 10.1016/s0079-6123(01)33022-4. [DOI] [PubMed] [Google Scholar]
- Cohen J, Cohen P, West SG, Aiken LS. Applied multiple regression/correlation analysis for the behavioral sciences. 3rd ed. Mahwah, NJ: Erlbaum; 2003. [Google Scholar]
- Cross TG. Mothers' speech and its association with rate of linguistic development in young children. In: Waterson N, Snow C, editors. The development of communication. Chichester, UK: Wiley; 1978. [Google Scholar]
- DeGangi G, DiPietro J, Greenspan S, Porges SW. Psychophysiological characteristics of the regulatory disordered infant. Infant Behavior and Development. 1991;14:37–50. [Google Scholar]
- Doussard-Roosevelt JA, McClenny BD, Porges SW. Neonatal cardiac vagal tone and school-age developmental outcome in very low birth weight infants. Developmental Psychobiology. 2001;38:56–66. [PubMed] [Google Scholar]
- El-Sheikh M, Kouros C, Erath S, Cummings M, Keller P, Staton L. Marital conflict and children’s externalizing behavior: Pathways involving interactions between parasympathetic and sympathetic nervous system activity. Monographs of the Society of Research in Child Development. 2009;74:1–79. doi: 10.1111/j.1540-5834.2009.00501.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Sheik M, Whitson S. Longitudinal relations between marital conflict and child adjustment: Vagal regulation as a protective factor. Journal of Family Psychology. 2006;20:30–39. doi: 10.1037/0893-3200.20.1.30. [DOI] [PubMed] [Google Scholar]
- Eyberg SM, Nelson MM, Duke M, Boggs SR. Manual for the Parent-Child Interaction Coding System. (3rd ed) 2004 Retrieved October 25, 2010, from the University of Florida Parent-Child Interaction Therapy Web site: http://www.pcit.org.
- Eyberg SM, Nelson MM, Boggs SR. Evidence-based psychosocial treatments for children and adolescents with disruptive behavior. Journal of Clinical Child and Adolescent Psychology. 2008;37:1–23. doi: 10.1080/15374410701820117. [DOI] [PubMed] [Google Scholar]
- Feldman R. The development of regulatory functions from birth to 5 years: insights from premature infants. Child Development. 2009;80:544–561. doi: 10.1111/j.1467-8624.2009.01278.x. [DOI] [PubMed] [Google Scholar]
- Feldman R, Eidelman A. Maternal postpartum behavior and the emergence of infant-mother and infant-father synchrony in preterm and full-term infants: The role of neonatal vagal tone. Developmental Psychobiology. 2007;49:290–302. doi: 10.1002/dev.20220. [DOI] [PubMed] [Google Scholar]
- Feldman R, Eidelman AI, Sirota L, Weller A. Comparison of skin-to-skin (kangaroo) and traditional care: parenting outcomes and preterm infant development. Pediatrics. 2002;110:16–26. doi: 10.1542/peds.110.1.16. [DOI] [PubMed] [Google Scholar]
- Feldman R, Singer M, Zagoory O. Touch attenuates infants’ physiological reactivity to stress. Developmental Science. 2010;12:271–278. doi: 10.1111/j.1467-7687.2009.00890.x. [DOI] [PubMed] [Google Scholar]
- Francis DD, Caldji C, Champagne F, Plotsky PM, Meaney MJ. The role of cortcotropin-releasing factor-norepinephrine systems in mediating the effects of early experience on the development of behavioral and endocrine responses to stress. Biological Psychiatry. 1999;46:1153–1166. doi: 10.1016/s0006-3223(99)00237-1. [DOI] [PubMed] [Google Scholar]
- Geva R, Feldman R. A neurobiological model for the effects of early brainstem functioning on the development of behavior and emotion regulation in infants: implications for prenatal and perinatal risk. Journal of Child Psychology and Psychiatry. 2008;49:1031–1041. doi: 10.1111/j.1469-7610.2008.01918.x. [DOI] [PubMed] [Google Scholar]
- Graziano P, Keane SP, Calkins SD. Cardiac vagal regulation and early peer status. Child Development. 2007;78:264–278. doi: 10.1111/j.1467-8624.2007.00996.x. [DOI] [PubMed] [Google Scholar]
- Graziano P, Reavis R, Keane SP, Calkins SD. The role of emotion regulation in children’s early academic success. Journal of School Psychology. 2007;45:3–19. doi: 10.1016/j.jsp.2006.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grossman P, Stemmler G, Meinhardt E. Paced respiratory sinus arrhythmia as an index of cardiac parasympathetic tone during varying behavioral tasks. Psychophysiology. 1990;27:404–416. doi: 10.1111/j.1469-8986.1990.tb02335.x. [DOI] [PubMed] [Google Scholar]
- Grossman P, Taylor E. Toward understanding respiratory sinus arrhythmia; Relations to cardiac vagal tone, evolution, and biobehavioral functions. Biological Psychology. 2007;74:263–285. doi: 10.1016/j.biopsycho.2005.11.014. [DOI] [PubMed] [Google Scholar]
- Haley D, Stansbury K. Infant stress and parent responsiveness: Regulation of physiology and behavior during still-face and reunion. Child Development. 2003;74:1534–1546. doi: 10.1111/1467-8624.00621. [DOI] [PubMed] [Google Scholar]
- Hayes A, Matthes J. Computational procedures for probing interactions in OLS and logistic regressions: SPSS and SAS implementations. Behavior Research Methods. 2009;41:924–936. doi: 10.3758/BRM.41.3.924. [DOI] [PubMed] [Google Scholar]
- Hays JR, Reas DL, Shaw JB. Concurrent validity of the Wechsler abbreviated scale of intelligence and the Kaufman brief intelligence test among psychiatric inpatients. Psychological Reports. 2002;90:355–359. doi: 10.2466/pr0.2002.90.2.355. [DOI] [PubMed] [Google Scholar]
- Hoff E. The specificity of environmental influence: Socioeconomic status affects early vocabulary development via maternal speech. Child Development. 2003;74:1368–1378. doi: 10.1111/1467-8624.00612. [DOI] [PubMed] [Google Scholar]
- Hoffman ML. Empathy and moral development: Implications for caring and justice. Cambridge, UK: Cambridge University Press; 2000. [Google Scholar]
- Hood KK, Eyberg SM. Outcomes of Parent–Child Interaction Therapy: Mothers’ reports of maintenance three to six years after treatment. Journal of Clinical Child and Adolescent Psychology. 2003;32:419–429. doi: 10.1207/S15374424JCCP3203_10. [DOI] [PubMed] [Google Scholar]
- Huffman LC, Bryan Y, del Carmen R, Pederson F, Doussard-Roosevelt J, Porges S. Infant temperament and cardiac vagal tone: Assessments at twelve weeks of age. Child Development. 1998;69:624–635. [PubMed] [Google Scholar]
- Izard C, Porges S, Simons R, Haynes M, Hyde C, Parisi M, et al. Infant cardiac activitiy: Developmental changes and relations with attachment. Developmental Psychology. 1991;27:432–439. [Google Scholar]
- Jaccard J, Turrisi R. Interaction effects in multiple regression. 2nd ed. Thousand Oaks, Calif.: Sage Publications; 2003. [Google Scholar]
- Keenan K. Emotion dysregulation as a risk factor for child psychopathology. Clinical Psychology: Science and Practice. 2000;7:418–434. [Google Scholar]
- Keenan K, Shaw D. Exploring the Etiology of Antisocial Behavior in the First Years of Life. In: Lahey B, Moffitt T, Caspi A, editors. Causes of Conduct Disorder and Juvenile Delinquency. New York: The Guilford Press; 2003. pp. 153–181. [Google Scholar]
- Kennedy AE, Rubin K, Hastings P, Maisel B. Longitudinal relations between child vagal tone and parenting behavior: 2 to 4 years. Developmental Psychobiology. 2004;45:10–21. doi: 10.1002/dev.20013. [DOI] [PubMed] [Google Scholar]
- Kopp C. Antecedents of self-regulation: A developmental perspective. Developmental Psychology. 1982;18:199–214. [Google Scholar]
- Kopp CB. Regulation of distress and negative emotions: A developmental view. Developmental Psychology. 1989;25:343–354. [Google Scholar]
- Lamb M. The role of the father in child development. 5th edition. New Jersey: John Wiley & Sons, Inc.; 2010. [Google Scholar]
- Landry S, Miller-Loncar C, Smith K, Swank P. The role of early parenting in children's development of executive processes. Developmental Neuropsychology. 2002;21:15–41. doi: 10.1207/S15326942DN2101_2. [DOI] [PubMed] [Google Scholar]
- Ludington-Hoe S, Anderson G, Simpson S, Hollingsead A, Argote L, Rey H. Birth-related fatigue in 34–36-week preterm neonates: Rapid recovery with very early kangaroo care. J Obstet Gynecol Neonatal Nurs. 1999;28:94–103. doi: 10.1111/j.1552-6909.1999.tb01970.x. [DOI] [PubMed] [Google Scholar]
- Luecken LJ, Lemery KS. Early caregiving and physiological stress responses. Clinical Psychology Review. 2004;24:171–191. doi: 10.1016/j.cpr.2004.01.003. [DOI] [PubMed] [Google Scholar]
- Miller WR, Rollnick S. Motivational interviewing. New York: Guilford Press; 2002. [Google Scholar]
- Minde K. Prematurity and serious medical conditions in infancy: Implications for development, behavior, and intervention. In: Zeanah CH, editor. Handbook of infant mental health. New York: Guilford; 2000. pp. 176–194. [Google Scholar]
- Miron D, Marva LL, Zeanah CH. Clinical use of observational procedures in early childhood relationship assessment. In: Zeanah CH, editor. Handbook of infant mental health. New York: Guilford; 2009. pp. 252–265. [Google Scholar]
- Moore G, Calkins SD. Infants' vagal regulation in the still-face paradigm is related to dyadic coordination of mother-infant interaction. Developmental Psychology. 2004;40:1068–1080. doi: 10.1037/0012-1649.40.6.1068. [DOI] [PubMed] [Google Scholar]
- Nixon RDV, Sweeney L, Erickson DB, Touyz SW. Parent-interaction therapy: A comparison of standard and abbreviated treatments for oppositional preschoolers. Journal of Consulting and Clinical Psychology. 2003;71:251–260. doi: 10.1037/0022-006x.71.2.251. [DOI] [PubMed] [Google Scholar]
- Pelham WE, Gnagy EM, Greiner AR, Hoza B, Hinshaw SP, Swanson JM, et al. Behavioral versus behavioral and pharmacological treatment in ADHD children attending a summer treatment program. Journal of Abnormal Child Psychology. 2000;28:507–525. doi: 10.1023/a:1005127030251. [DOI] [PubMed] [Google Scholar]
- Portales L, Porges S, Doussard-Roosevelt J, Abedin M, Lopez R, Young M, et al. Vagal regulation during bottle feeding in low-birthweight neonates: Support for the gustatory-vagal hypothesis. Developmental Psychobiology. 1997;30:225–233. [PubMed] [Google Scholar]
- Porges S, Doussard-Roosevelt J, Portales L, Greenspan S. Infant regulation of the vagal “brake” predicts child behavior problems: A psychobiological model of social behavior. Developmental Psychobiology. 1996;29:697–712. doi: 10.1002/(SICI)1098-2302(199612)29:8<697::AID-DEV5>3.0.CO;2-O. [DOI] [PubMed] [Google Scholar]
- Porges SW. Method and apparatus for evaluating rhythmic oscillations in aperiodic physiological response systems. 4520944. United States patent no. 1985
- Porges SW. Vagal tone: An autonomic mediator of affect. In: Garber J, Dodge KA, editors. The Development of Emotional Regulation and Dysregulation. Cambridge: Cambridge University Press; 1991. pp. 111–128. [Google Scholar]
- Porges S. Orienting in a defensive world: Mammalian modifications of our evolutionary heritage. A Polyvagal theory. Psychophysiology. 1995;32:301–318. doi: 10.1111/j.1469-8986.1995.tb01213.x. [DOI] [PubMed] [Google Scholar]
- Porges SW. The polyvagal theory: phylogenetic substrates of a social nervous system. International Journal of Psychophysiology. 2001;42:123–146. doi: 10.1016/s0167-8760(01)00162-3. [DOI] [PubMed] [Google Scholar]
- Porges SW. The polyvagal theory: phylogenetic contributions to social behavior. Physiology and Behavior. 2003;79:503–513. doi: 10.1016/s0031-9384(03)00156-2. [DOI] [PubMed] [Google Scholar]
- Porges SW. The polyvagal perspective. Biological Psychology. 2007;74:116–143. doi: 10.1016/j.biopsycho.2006.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Porter C. Coregulation in mother-infant dyads: links to infants' cardiac vagal tone. Psychological Reports. 2003;92:307–319. doi: 10.2466/pr0.2003.92.1.307. [DOI] [PubMed] [Google Scholar]
- Propper C, Moore G. The influence of parenting on infant emotionality: A multi-level psychobiological perspective. Developmental Review. 2006;26:427–460. [Google Scholar]
- Propper C, Moore G, Mills-Koonce R, Halpern C, Hill-Soderlund A, Calkins S, et al. Gene-environment contributions to the development of infant vagal reactivity: The interaction of dopamine and maternal sensitivity. Child Development. 2008;79:1377–1394. doi: 10.1111/j.1467-8624.2008.01194.x. [DOI] [PubMed] [Google Scholar]
- Robins DL, Fein D, Barton ML, Green JA. The Modified Checklist for Autism in Toddlers: an initial study investigating the early detection of autism and pervasive developmental disorders. Journal of Autism and Developmental Disorders. 2001;31:131–144. doi: 10.1023/a:1010738829569. [DOI] [PubMed] [Google Scholar]
- Schuhmann E, Foote R, Eyberg S, Boggs S, Algina J. Efficacy of parent–child interaction therapy: interim report of a randomized trial with short-term maintenance. Journal of Clinical Child Psychology. 1998;27:34–45. doi: 10.1207/s15374424jccp2701_4. [DOI] [PubMed] [Google Scholar]
- Shaw DS, Keenan K, Vondra J, Delliquadri E, Giovanelli J. Antecedents of preschool children’s internalizing problems: a longitudinal study of low-income families. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:1760–1767. [PubMed] [Google Scholar]
- Snow AV, Lecavalier L. Sensitivity and specificity of the Modified Checklist for Autism in Toddlers and the Social Communication Questionnaire in preschoolers suspected of having pervasive developmental disorders. Autism. 2008;12:627–644. doi: 10.1177/1362361308097116. [DOI] [PubMed] [Google Scholar]
- Sroufe L. Early relationships and the development of children. Infant Mental Health Journal. 2000;21:67–74. [Google Scholar]
- Stadler C, Grasmann D, Fegert JM, Holtmann M, Poustka F, Schmeck K. Heart rate and treatment effect in children with disruptive behavior disorders. Child Psychiatry and Human Development. 2008;39:299–309. doi: 10.1007/s10578-007-0089-y. [DOI] [PubMed] [Google Scholar]
- Stansbury K, Zimmerman LK. Relations among child language skills, maternal socializations of emotion regulation, and child behavior problems. Child Psychiatry and Human Development. 1999;30:121–142. doi: 10.1023/a:1021954402840. [DOI] [PubMed] [Google Scholar]
- Suess PE, Bornstein M. Task-to-task vagal regulation: Relations with language and play in 20-month-old children. Infancy. 2000;1:303–322. doi: 10.1207/S15327078IN0103_2. [DOI] [PubMed] [Google Scholar]
- Suess PE, Porges SW, Plude DJ. Cardiac vagal tone and sustained attention in school-age children. Psychophysiology. 1994;31:17–22. doi: 10.1111/j.1469-8986.1994.tb01020.x. [DOI] [PubMed] [Google Scholar]
- Tamis-LeMonda CS, Bornstein MH, Baumwell L. Maternal responsiveness and children’s achievement of language milestones. Child Development. 2001;72:748–767. doi: 10.1111/1467-8624.00313. [DOI] [PubMed] [Google Scholar]
- Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Heart rate variability: standards of measurement, physiological interpretation and clinical use. Circulation. 1996;93:1043–1065. Retrieved from http://circ.ahajournals.org/cgi/content/full/93/5/1043. [PubMed] [Google Scholar]
- Vallotton C, Ayoub C. Use your words: The role of language in the development of toddlers’ self-regulation. Early Childhood Research Quarterly (2010) doi: 10.1016/j.ecresq.2010.09.002. (in press). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vygotsky LS. In: Mind in society: The development of higher mental processes. Cole M, John-Steiner V, Scribner S, Souberman E, editors. Cambridge, MA: Harvard University Press; 1978. [Google Scholar]
- Wechsler D. Wechsler Abbreviated Scale of Intelligence. San Antonio, TX: Pychological Corportation; 1999. [Google Scholar]
- Wilson B, Gottman J. Attention--the shuttle between emotion and cognition: Risk, Resiliency, and physiological bases. In: Hetherington E, Blechman E, editors. Stress, coping and resiliency in children and families. Mahwah, NJ: Lawrence Erlbaum Associates; 1996. pp. 189–228. [Google Scholar]
- Winsler A. Parent-child interaction and private speech in boys with AD/HD. Applied Developmental Science. 1998;2:17–39. [Google Scholar]
- Zisser A, Eyberg S. Treating oppositional behavior in children using parent-child interaction therapy. In: Kazdin A, Weisz J, editors. Evidence-Based Psychotherapies for Children and Adolescents. 2nd ed. New York: Guilford; 2010. [Google Scholar]