Summary
Tobacco use behaviors have changed significantly over the past century. Compared to 1964, smoking prevalence rates have halved from 40% to 20% and as a result there has been a slow but steady decline in the rates of tobacco-induced diseases such as heart disease and cancer. Growing awareness of the health risks of smoking were aided by the United States Surgeon Reports which were issued on a nearly annual basis starting in 1964. Concerns about the hazards of breathing in secondhand smoke pollution further contributed to the declining social acceptance of smoking, which evolved into regulatory actions restricting smoking on buses, planes, retail outlets, restaurants and bars. Today, 23 states and 493 localities have comprehensive laws restricting indoor smoking. This paper examines public policies that have made a significant impact on smoking and lung cancer rates and discusses potential future research directions to further reduce the diseases caused by smoking.
Keywords: Tobacco control, Tobacco policy, Lung Cancer, Tobacco taxation, Clean Air Laws
Introduction
Current estimates suggest that tobacco use, mainly cigarette smoking, is responsible for approximately 440,000 deaths annually in the United States, of which nearly 157,000 are deaths from lung cancer (1). The number of people currently alive with a smoking caused illness such as cancer, heart disease or chronic obstructive lung disease is roughly 20 times greater than the number of deaths annually (2). Cigarette smoking is responsible for 90% of all lung cancers, and 1/3rd of all cancer deaths; 80% of cases of chronic obstructive lung disease and about 20% of deaths from heart disease (3). Health-related costs of tobacco-induced illness total nearly $200 billion dollars annually (1,4).
The situation was much different at the turn of the 20th century when cigarettes were not the predominate form of tobacco consumed, and as a result cigarettes were not a major contributor to cancer or other serious illnesses. The rapid rise in lung cancer deaths that occurred in the early part of the 20th century can be traced to the invention and widespread use of the modern American cigarette that used a blend of tobaccos (burley, bright, and oriental) that made it possible to easily inhale the smoke into the lungs, speeding nicotine to the brain and making cigarette smoking highly addictive (5). The most popular early cigarettes brands were Chesterfield (introduced in 1896), Camel (1913), and Lucky Strike (1916) which accounted for about 80% of the market before 1940. In their marketing, the companies competed with each other in touting the mildness and easy inhalability of their cigarettes. However, as the early cohorts of cigarette smokers began to die of lung cancer in large numbers, it became more difficult to persuade the American public that cigarette smoking was not detrimental to health. In the 1950’s and 60’s cigarette companies moved to introduce filters on cigarettes and lower yield cigarettes (which were essentially the same cigarettes with tiny vent holes added to the filter) in an effort to address growing health concerns about the risks of smoking. Unfortunately, these product innovations did little to reduce the diseases caused by smoking and more than likely delayed a more rapid decline in cigarette smoking as the public was persuaded to switch to these new products under the false assumption that they were safer.
Growing awareness of the health risks of smoking were aided by the US Surgeon Reports, which were issued on nearly an annual basis starting in 1964. Concerns about the hazards of breathing in secondhand smoke pollution further contributed to the declining social acceptance of smoking which evolved into regulatory actions restricting smoking on buses, planes, retail outlets, restaurants and bars. Today, 23 states and 493 localities have adopted laws restricting indoor smoking (6). Compared to 1964, smoking prevalence rates have halved from 40% to 20% and as a result there has been a slow but steady decline in the rates of tobacco-induced diseases such as heart disease and cancer. This paper examines efforts to discourage cigarette smoking over the past century with a focus on public policies that have made a significant impact on smoking and lung cancer rates. Potential future research directions to further reduce the diseases caused by smoking are also discussed.
Early efforts to reduce cigarette smoking
At the turn of the 20th century most tobacco consumed in the United States was in the form of chewing tobacco and/or cigars. Cigarettes were largely a novelty item. In 1881 James Bonsack invented the automated cigarette making machine that ushered in the mass production of cigarettes. The Bonsack device could make 200 cigarettes per minute, about 60 times faster than a skilled hand roller, displacing more than 700 jobs at Buck Duke's (American Tobacco) factories in Durham and New York. Tuberculosis was a major health problem and several states and communities enacted anti spitting laws intended to prevent the spread of tuberculosis. In addition, cigarettes became linked to the temperance movement of the day. Lucy Page Gaston, a teacher, writer, lecturer and member of the Woman's Christian Temperance Union, founded The Anti-Cigarette League of America in 1890. Gaston maintained that cigarette smoking was a "dangerous new habit, particularly threatening to the young and thus likely to lead to the use of alcohol and narcotics which was prevalent in the 1890s” (7). Between 1890 and 1930, 15 States enacted laws banning the sale, manufacture, possession, or use of cigarettes, and 22 other States considered such legislation. Eventually, all the states repealed their cigarette prohibition laws with Kansas as the last to do so, in 1927.
World War I provided the perfect opportunity to market cigarettes. Soldiers received a weekly ration of 50 cigarettes. General John J. Pershing, commander-in-chief of the American forces in France in 1917, called tobacco "indispensable to the daily ration. You ask me what we need to win this war. I answer tobacco, as much as bullets” (8). As a result of the distribution of free cigarettes to the soldiers, many returned from Europe as addicted smokers. Organizations such as the YMCA that had been active in Lucy Gaston’s Temperance movement against cigarette smoking changed their position by aiding in the distribution of free packs of cigarettes to the soldiers as part of the war effort.
The early evidence on the adverse health effects of cigarette smoking began to appear in the medical literature in the 1920’s and 1930’s as lung cancer death rates accelerated. In a 1927 letter to Lancet, a medical doctor named Frank E Tylecote divulged "I have no statistics with regard to tobacco, but I think that in almost every case I have seen and known of, the patient has been a regular smoker, generally of cigarettes" (9).
Reports linking smoking to lung cancer began to appear in medical journals with greater frequency in the early 1950s. An article published in the June issue of Cancer Research reported the results of experiments where cancerous tumors formed on the backs of the laboratory mice that were exposed to cigarette tar (10). This paper received wide publicity when Life Magazine ran an article recounting these experiments in its December issue. In the same year, a nationwide survey commissioned by Philip Morris found that 58% of men and 36% of women were current smokers, and less than 1% mentioned cancer as a health issue linked to smoking. However, the evidence indicting smoking as a cause of cancer continued to accumulate and by end of the 1950’s there was little doubt among scientists that cigarette smoking caused cancer.
In March 1962, President John F. Kennedy was asked at a news conference about a recent report from the Royal College of Physicians that had concluded that cigarette smoking was a cause of lung cancer. Not knowing about the report, President Kennedy asked the US Public Health Service to examine the issue and produce a report on the subject. On January 11, 1964, the first Surgeon General’s Report on smoking and health was issued and gained wide publicity across the country. The report concluded that, smokers, compared to non-smokers, had a 10 fold increased risk of developing lung and laryngeal cancer. Smoking was also linked to chronic bronchitis and emphysema, cardiovascular mortality, and low birth weight infants (11). While cigarette consumption did drop in the months immediately following the release of the report, per capita sales rebounded to reach record high levels by the end of 1966.
Efforts to reduce smoking following the release of the 1964 SGR
Declining cigarette consumption after 1964 corresponded to increased public awareness of the dangers of tobacco use, changing social norms about tobacco and increased governmental actions to regulate the use, sale, and advertising of tobacco products (12–14). The most comprehensive change has been in attitudes and rules about smoking in enclosed public places. As late as 20 years ago, smoking was effectively ubiquitous in most places, with smoking allowed virtually everywhere (except where there was a danger or fires or damage to equipment). Over time the environment which had supported smoking indoors has transformed. Today, 23 states and 493 localities have adopted laws restricting indoor smoking (6). Limiting where people can smoke has contributed to the social marginalization of smoking as an accepted behavior.
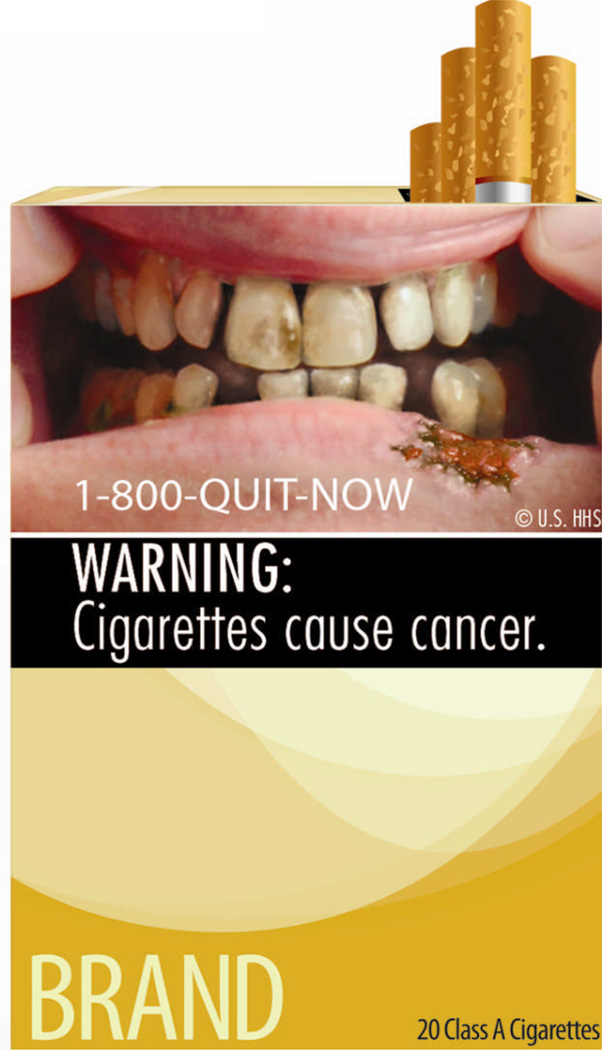
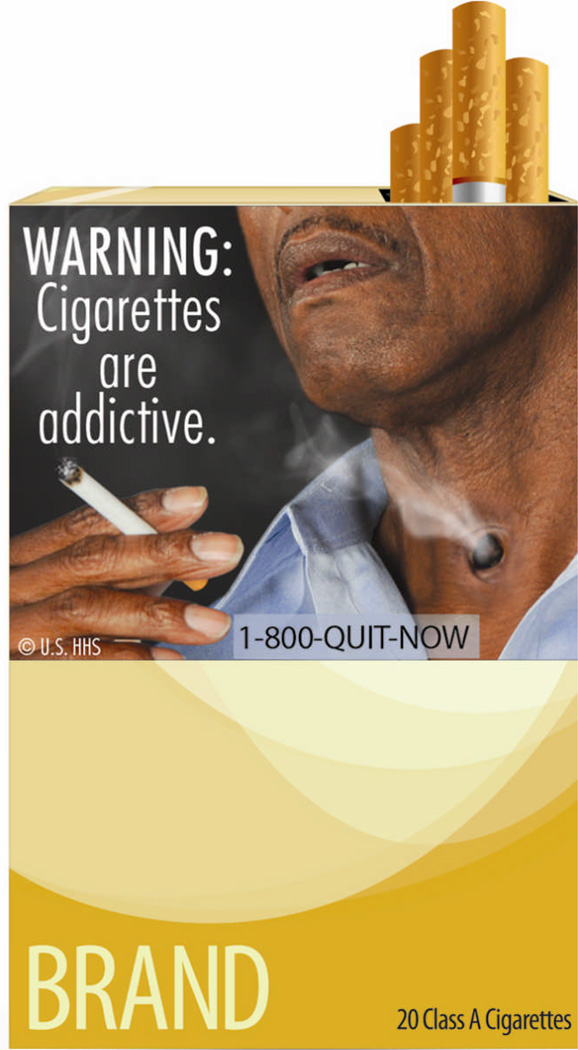
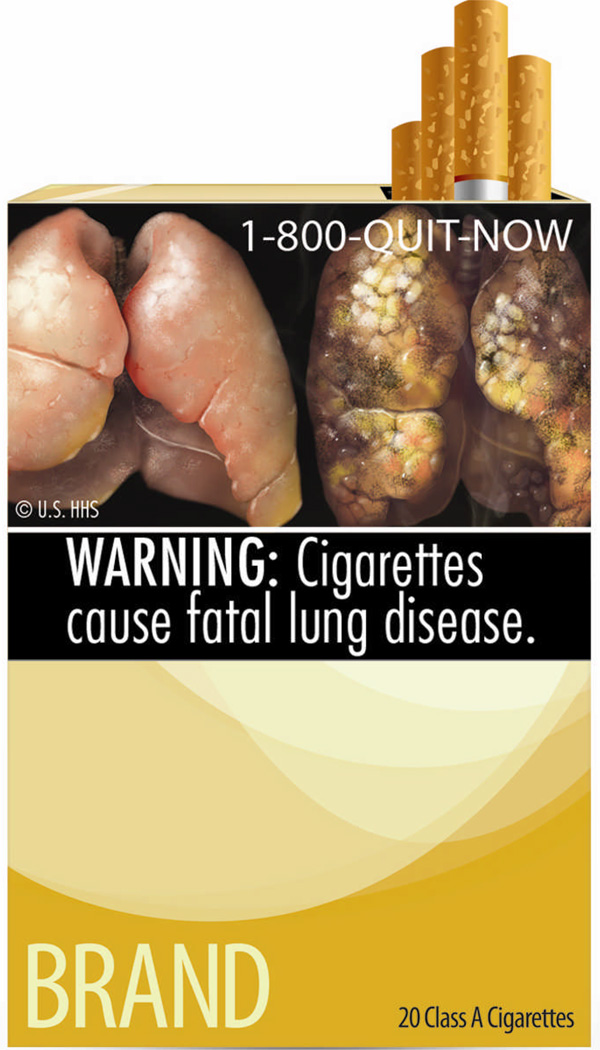
Communicating the health effects of smoking has been a primary goal of tobacco control efforts since the first Surgeon General’s report was issued nearly 50 years ago (15–18). The provision of health warnings and/or product information on tobacco packages currently represents an important means of informing consumers about the health risks of smoking as a first step towards changing behavior. Virtually all countries throughout the world require package warning labels on cigarettes, although the content and size of the warnings vary widely (19,20).
In 1966 the first caution label appeared on cigarette packs in the United States, telling smokers “Caution, smoking may be dangerous to your health.” This warning was strengthened in 1970 to read: “The Surgeon General Has Determined that Cigarette Smoking is Dangerous to Your Health.” In March 1972, Federal Trade Commission (FTC) rules went into effect requiring manufacturers to display the same health warning mandated on cigarette packages on all cigarette advertising. In 1984, Congress enacted the Comprehensive Smoking Education Act, which required four rotating health warnings on all cigarette packages and advertisements beginning in 1985 (21):
SURGEON GENERAL'S WARNING: Smoking Causes Lung Cancer, Heart Disease, Emphysema, and May Complicate Pregnancy.
SURGEON GENERAL'S WARNING: Quitting Smoking Now Greatly Reduces Serious Risks to Your Health.
SURGEON GENERAL'S WARNING: Smoking by Pregnant Women May Result in Fetal Injury, Premature Birth, and Low Birth Weight.
SURGEON GENERAL'S WARNING: Cigarette Smoke Contains Carbon Monoxide.
Studies that have evaluated the US health warnings suggest that the warnings have been largely ineffective in changing behavior (22). A 1967 FTC report concluded that “the warning label on cigarette packages has not succeeded in overcoming the prevalent attitude toward cigarette smoking created and maintained by the cigarette companies through their advertisements, particularly the barrage of commercials on television, which portray smoking as a harmless and enjoyable activity that is not habit forming and involves no hazards to health” (23).
In a more recent study that used a sophisticated eye-tracking methodology to assess exposure to the health warnings in advertising, 44% of adolescents asked to view cigarette advertisements did not even look at the warning label displayed on the advertisement (24). In 2009 the U.S. Food and Drug Administration (FDA) was given the authority by Congress to regulate tobacco products, including a mandate to update the current health warning labels on cigarettes (25). The FDA recommended that a series of pictorial health warnings appear on cigarette packs beginning in 2012 (see figures 1–3) (25). Studies in countries that have adopted pictorial pack warnings have found that they are more likely to be noticed, result in improved awareness of the health risks of smoking, and motivate quit attempts in comparison to the text only warnings (26).
Figure 1.
Figure 3.
Changes in smoking behavior have mirrored population trends in awareness about smoking as a cause of lung cancer and rates of smoking cessation (27). The first large scale national counter-advertising campaign to educate the public about the health risks of tobacco use occurred between 1967 and 1970 when the Federal Communications Commission (FCC) required licensees who broadcast cigarette commercials to provide free media time for antismoking public service announcements (PSA) under the Fairness Doctrine (21). The Fairness Doctrine obligated licensed broadcasters to encourage and implement the broadcast of all sides of controversial public issues over their facilities, over and beyond their obligation to make available on demand opportunities for the expression of opposing views (21). In January 1967, an attorney by the name of John Banzhaf petitioned the FCC to apply the Fairness Doctrine to cigarette advertising (21). In June of 1967, the FCC granted Banzhaf's petition and ruled that licensed broadcasters were required to air roughly one antismoking message for every three cigarette brand commercials. In July 1967, antismoking PSAs developed by the government and voluntary health agencies began to air. Unlike most public service advertising campaigns, many of the antismoking ads were aired during prime time. The time donated for the antismoking messages amounted to approximately nearly 300 million dollars per year. The Fairness Doctrine campaign ended in January 1971 as a result of a federal law that banned cigarette advertising on television and radio. After 1970, the number of antismoking PSAs declined markedly as antismoking messages were forced to compete for donated airtime. Between 1967 and 1970 cigarette consumption in the US dropped at a much faster rate than during the period immediately before or after the time when the Fairness Doctrine antismoking campaign was operational (21). While it is impossible to rule out the effects of other influences that may have contributed to the decline in cigarette consumption between 1967 and 1970, several studies have concluded that the antismoking messages mandated by the Fairness Doctrine were responsible for much of the reduction in smoking during this period (13,28–30).
The 1998 Master Settlement Agreement (MSA) between the tobacco industry and state governments provided resources to create a new foundation that had as one of its mandates sponsorship of a national counter-advertising campaign (31,32). The American Legacy Foundation was created in 1999 and has spent approximately $100 million annually on a nationwide broadcast counter-advertising campaign (known as “the truth campaign”) targeting teens and young adults. The campaign has been successful in creating a high level of awareness of its messages among the intended target audience and smoking rates have declined among teenagers as a result.
In 1969, Congress passed the Public Health Cigarette Smoking Act that prohibited cigarette advertising in the broadcast media effective beginning in 1971 (21). Congress extended the ban on broadcast advertising to little cigars in 1973, and to smokeless tobacco products in 1986 (21). The federal law banning cigarette advertising on television and radio also included a clause preempting states and localities from regulating or prohibiting cigarette advertising or promotions for health reasons. The purpose of the preemption was to avoid chaos created by different, potentially conflicting regulations. However, the effect of the federal preemption was that few states and localities have attempted to regulate advertising of tobacco products (21). In recent years, a number of cities and states have acted to restrict transit advertising, the free distribution of tobacco product samples, and point-of-sale advertising. In 1998, as part of the MSA, cigarette manufacturers agreed to discontinue billboard advertising, advertising in magazines with a high percentage of underage readers, and place limits on their sponsorship of sporting and cultural events (33). In 2010, the FDA banned the use of misleading descriptor labels on cigarettes such as “light,” “low tar” and “mild” (25). Unfortunately, cigarette manufacturers altered their packs using different color schemes to convey the same misleading perceptions about the strength of their cigarettes (light colors for previously labeled light cigarettes, blue and green for mint and menthol flavorings, etc) which means that many consumers continue to be misled about the fact that there is really no benefit to be gained by smoking a filtered or so-called low yield product as currently marketed.
It is well recognized in economic theory, as well as in everyday life, that purchasing decisions are influenced by the affordability of a product. The price of cigarettes is determined by the manufacturer's price, wholesale and retail markups and tobacco taxes. Perhaps the straightforward and reliable way to reduce cigarette consumption is to increase the price of cigarettes by raising the tax. In the US, tobacco taxes are levied at the federal, state, and local levels. During the first part of the century taxes of tobacco products were typically very low, were primarily used to generate revenue, and were raised infrequently. In 1951, the Federal tax was set at 8 cents per pack, the level at which it would remain for more than 30 years. Views about taxing cigarettes started to change after the release of the 1964 Surgeon General’s Report on smoking. Many states began increasing cigarette excise taxes in an apparent effort to reduce smoking and its consequences. Economists and others began producing studies documenting the impact of cigarette taxes and prices on smoking, particularly among youth and young adults. These findings led to growing pressure from public health groups for further increases in state and federal cigarette taxes. Eventually, the federal cigarette tax was doubled to 16 cents per pack on January 1, 1983. In the 1990s federal cigarette taxes were progressively raised and in 2008 were increased to its current rate of $1.01 per pack. Since 1980, most states have increased taxes on tobacco products, with some increases of 200% or more. Economists use estimates of the price elasticity of demand to quantify the impact of a change in price on consumption. Formally, the price elasticity of demand is defined as the percentage change in consumption resulting from a 1% increase in price. While a relatively wide range of estimates has been produced for the price elasticity of demand for cigarettes, most of the estimates from the US and other high-income countries tend to fall in the relatively narrow range from −0.30 to −0.50 (12,34,35). Thus, estimates suggest that an increase of 10% in the price of cigarettes would decrease cigarette consumption by 3–5%, and, if implemented comprehensively, could prevent 5–16 million smoking-related deaths worldwide (34,36). A number of studies have demonstrated that youth are relatively more sensitive to price than adults, implying that raising cigarette taxes would be a useful tobacco prevention intervention.
While cigarette taxes represent a fairly direct means of influencing consumption, other price policies can also alter smoking behavior. For example, some employers have started to charge higher health insurance premiums to employees who smoke; while others have chosen not to hire smokers at all (37). Litigation and regulation of tobacco products has also had the effect of increasing the price of tobacco products, as these costs are merely passed onto consumers when they buy a pack of cigarettes.
Policies restricting where people can smoke correspond to changing attitudes about smoking and reductions in smoking behavior. Today, 23 states and 493 individual communities in the United States have adopted comprehensive smoke-free laws that prohibit smoking in non-hospitality workplaces, restaurants and bars (6). Today the negative health effects (e.g., lung cancer, heart disease) of secondhand smoke are unequivocal. Studies have shown that smoke-free ordinances decrease secondhand smoke exposure and yield measurable improvements in public health. One meta-analysis documented a 19% reduction in hospital admissions for acute myocardial infarctions following passage of smoke-free laws (38). Smoking restrictions have also been found to increase quit attempts among smokers as well as decrease total cigarette consumption (39–42). Some estimates suggest that smoke-free worksites produce a 4% reduction in the overall prevalence of tobacco use, which roughly equals 3.1 fewer cigarettes consumed per day (43).
Historically, the vast majority (>90%) of former smokers have reported that they stopped smoking without receiving formal assistance or help from anyone (44). However, this statistic has changed with the introduction and wide availability of effective drug therapies to help smokers alleviate withdrawal symptoms commonly associated with cessation (45,46). First line pharmacotherapy to support a quit attempt include nicotine replacement (gum, patch, lozenge, nasal spray or inhaler), bupropion, or varenicline, and use of these agents can increase quit rates by 1.5 to 3-fold (47–49). Several studies have shown that combining the nicotine patch with either gum or nasal spray can increase quit rates over single modality therapy (48).
The potential impact of treatments for tobacco dependence not only depends on their efficacy but also the extent to which these treatments reach those who might benefit from them. Today, there is not much evidence to support the idea that therapies for treating nicotine dependence have dramatically influenced rates of tobacco use on a population level (45,48,50–52). The main reason for this failure is the generally low utilization of these therapies, which may be due in part to the failure of health-care workers to aggressively assist their tobacco-using patients in quitting (15,17,47,50,51). Policies that can increase the reach, appeal and use of effective cessation treatments such as promotion of a national quit line number on cigarette packs, the development and marketing of more consumer appealing stop smoking treatments, and the creation of health care systems that require cessation treatment to be offered as routine care hold great untapped potential to reduce overall adult smoking prevalence and growing disparities in tobacco use in the future (15,17,47,48,51).
The Future
As a result of the policies described above, cigarette consumption has fallen steadily in the United States over the past 50 years and lung cancer mortality and other smoking induced diseases have also declined. However, while future predictions for cigarette trends in United States have consumption dropping to near trivial levels in 50 years, the trend outside the United States are not so positive. Cigarette consumption is actually increasing in low and middle income countries and as a result cigarette manufacturers have shifted their focus to these emerging economies (53). Even in the United States today, most of the tobacco used in cigarettes is imported from overseas. The global effort to reduce the burden of tobacco use has been aided by the World Health Organization’s Framework Convention on Tobacco Control (FCTC) which is the first global health treaty negotiated under the auspices of the WHO (54,55). The FCTC has been ratified by over 170 countries. Ratification of the treaty obligates countries to implement a comprehensive set of policies including higher taxes, effective health warning labels, and smoke-free policies (55). However, the tobacco industry is working to counteract the FCTC by using its economic power and influence to lead governments to adopt policies that, although compliant with the FCTC, are actually ineffective. Thus, it is more critical than ever that the medical and public health community adopt evidence-based guidelines to ensure that governments adopt the kinds of policies and programs that will be effective in reducing tobacco use.
Product regulations which include rules about what types of products might be sold, disclosure of information about products, requirements for testing products, and mandated performance standards for products offer new opportunities to reduce the harm caused by cigarettes (56). In 2009, the Congress enacted the Family Smoking Prevention and Tobacco Control Act which gave the FDA authority to regulate tobacco products so as to benefit the public’s health (25). However, deciding how to implement product regulations that will actually reduce the harm caused by cigarettes, short of banning them (which is actually prohibited by the law), is of debate and future research. What is clear is that cigarette smoking is harmful because people get addicted leading to persistent exposure to carcinogens and other poisons in tobacco smoke which eventually results in the many cancers and other illnesses caused by tobacco use. In theory it should be possible to engineer tobacco products so that they are no so addictive. For example, regulating the blending methods, additives, and filters used in cigarettes could so that the product is not so easy to inhale would have a dramatic impact on usage patterns. Lowering the nicotine delivery could also allow smokers to quit more easily than is the case with today’s cigarettes (17). However, whether these types of regulatory measures will ever be adopted is another question.
Another important future direction for both medicine and public health is lung cancer screening. The National Lung Screening Trial (NSLT) provides evidence to support the use of low dose CT scanning for high risk current and former cigarette smokers (over age 55 years with >30 pack-year history of smoking) to identify cancers in an early treatable stage thereby lowering lung cancer mortality (57). The opportunity exists over the next decade to dramatically change the prognosis of lung cancer from one of death sentence to one where cancer can be detected early and cured or managed effectively. However, concerns about who will pay for the costs of screening and disease management will likely delay efforts to realize the potential of lung cancer screening for high risk current and former smokers. Here, government could make a wise choice and raise tobacco taxes to prevent young people from taking up smoking, while earmarking these tax dollars to assist addicted smokers to quit and cover the costs of screening and disease management for those at risk of developing lung cancer.
Conclusion
Cigarette use in the United States has declined significantly since the 1960’s, as have rates of lung cancer, due in large measure to various tobacco control policies that have made smoking less affordable, less convenient, and less socially acceptable. However, despite an abundance of evidence linking smoking to lung cancer and other illnesses, 20% of adults in America still smoke cigarettes and too many young people still perceive smoking as a rite of passage to adulthood. While numerous clinical trials have demonstrated the effectiveness of smoking cessation medications, too few smokers use them when they try to quit. Clearly, governments can and should be doing more to reduce smoking. As the state of California has demonstrated, consistent funding of a comprehensive tobacco control program can lead to accelerated declines in smoking behavior leading to reductions in heart disease and cancer mortality and ultimately saving taxpayers money (58). Thus, earmarking cigarette taxes to cover implement effective public education campaigns, stop smoking services, and lung cancer screening for high risk current and former smokers would seem to make sense. The implementation of product regulations that would reduce the addictiveness and appeal of cigarettes would also make sense as a way to further reduce cigarette consumption here in the United States and worldwide.
Figure 2.
Acknowledgments
Dr. Silvestri has received funding in the form of a K24 grant from the National Institute of Health (NIH) and has received grant funding from Olympus. Dr. Carpenter has received funding in the form of an NIH Career Development Grant (NIDA K23 grant). Dr. Cummings has received grant funding from the NIH, has received payment from the NIH as a grant reviewer, has received payment from Pfizer for consulting work, and as a paid witness for plaintiffs in litigation against the tobacco industry. For the remaining authors none were declared.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of Interest and Source of Funding:
There are no conflicts of interest in this manuscript.
Contributor Information
Luca Paoletti, Division of Pulmonary and Critical Care Medicine, Department of Medicine, Medical University of South Carolina, 96 Jonathan Lucas St, CSB Suite 812, Charleston, SC 29412, lucap@musc.edu.
Bianca Jardin, Department of Psychiatry, Hollings Cancer Center, Medical University of South Carolina, 86 Jonathan Lucas St, Charleston, SC 29425, jardin@musc.edu.
Matthew Carpenter, Department of Psychiatry and Behavioral Sciences, Hollings Cancer Center, Cancer Prevention and Control, Medical University of South Carolina, 68 President St, BE 103, MSC 955, Charleston, SC 29425, carpente@musc.edu.
K. Michael Cummings, Department of Psychiatry and Behavioral Sciences, Hollings Cancer Center, Cancer Prevention and Control, Medical University of South Carolina, 68 President St., Charleston, SC 29425, cummingk@musc.edu.
Gerard A. Silvestri, Department of Medicine, Division of Pulmonary/Critical Care Medicine, Medical University of South Carolina, 96 Jonathan Lucas St., CSB 812 Suite 812, Charleston, SC, 29425, silvestr@musc.edu.
References
- 1.Centers for Disease Control and Prevention (CDC) Smoking-attributable mortality, years of potential life lost, and productivity losses--United States, 2000–2004. MMWR Morb Mortal Wkly Rep. 2008;57:1226–1228. [PubMed] [Google Scholar]
- 2.Tobacco Use Targeting the Nation's Largest Killer. National Center for Chronic Disease Prevention and Health Promotion; [Accessed February 1, 2012]. CDC website available at: http://www.cdc.gov/chronicdisease/resources/publications/aag/pdf/2011/Tobacco_AAG_2011_508.pdf. [Google Scholar]
- 3.United States Department of Health and Human Services. How Tobacco Smoke Causes Disease: The Biology and Behavioral Basis for Smoking-Attributable Disease: A Report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2010. [PubMed] [Google Scholar]
- 4.Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Actual causes of death in the United States, 2000. JAMA. 2004;291:1238–1245. doi: 10.1001/jama.291.10.1238. [DOI] [PubMed] [Google Scholar]
- 5.Borio G. [Accessed on February 2, 2012];The Tobacco Timeline [Tobacco.org website] 1993–2007. Available at http://www.tobacco.org/resources/history/Tobacco_History20-1.htm.
- 6. [Accessed February 1, 2012];Americans for Nonsmokers Rights. 2012 Jan 2; Available at: http://www.no-smoke.org/pdf/mediaordlist.pdf.
- 7.Tate Cassandra. Cigarette Wars: The Triumph of "The Little White Slaver". New York: Oxford University Press; 1999. [PubMed] [Google Scholar]
- 8.Brandt Allan. The Cigarette Century: The Rise, Fall, and Deadly Persistence of the Product That Defined America. New York: Basic Books; 2007. [Google Scholar]
- 9.Tylecote FE. Prognosis: A Series of Signed Articles contributed by invitation. Lancet. 1935;225:1117–1118. [Google Scholar]
- 10.Wynder EL, Graham EA, Croninger AB. Experimental production of carcinoma with cigarette tar. Cancer Res. 1953;13:855–864. [PubMed] [Google Scholar]
- 11.United States Department of Health, Education, and Welfare. Smoking and Health: Report of the Advisory Committee to the Surgeon General of the Public Health Service. Washington: U.S. Department of Health, Education, and Welfare, Public Health Service, Center for Disease Control; 1964. PHS Publication No. 1103. [Google Scholar]
- 12.Warner KE. Selling Smoking: Cigarette Advertising and Public Health. Washington, DC: AAPHA; 1986. [Google Scholar]
- 13.Warner KE. Effects of the antismoking campaign: an update. Am J Public Health. 1989;79:144–151. doi: 10.2105/ajph.79.2.144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cummings KM. Programs and policies to discourage the use of tobacco products. Oncogene. 2002;21:7349–7364. doi: 10.1038/sj.onc.1205810. [DOI] [PubMed] [Google Scholar]
- 15.Fiore MC, Croyle RT, Curry SJ, et al. Preventing 3 million premature deaths and helping 5 million smokers quit: a national action plan for tobacco cessation. Am J Public Health. 2004;94:205–210. doi: 10.2105/ajph.94.2.205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Frieden TR, Mostashari F, Kerker BD, Miller N, Hajat A, Frankel M. Adult tobacco use levels after intensive tobacco control measures: New York City, 2002–2003. Am J Public Health. 2005;95:1016–1023. doi: 10.2105/AJPH.2004.058164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Institute of Medicine. Ending the Tobacco Problem: A Blueprint for the Nation. Washington, DC: The National Academies Press; 2007. [Google Scholar]
- 18.World Health Organization. WHO report on the global tobacco epidemic, 2008: The MPOWER package. Geneva, Switzerland: World Health Organization; 2008. [Google Scholar]
- 19.Hammond D. Tobacco Labeling Resource. Waterloo, Ontario: Univ. Waterloo; 2008. [Accessed on February 1, 2012]. Available at http://www.tobaccolabels.org. [Google Scholar]
- 20.Hammond D. Tobacco Labeling & Packaging Toolkit: A Guide to FCTC Article 11. Waterloo, Ontario: Univ. Waterloo; 2008. [Google Scholar]
- 21.Center for Disease Control. Reducing the health consequences of smoking: 25 years of progress—a report of the Surgeon General. Rockville, MD: US Department of Health and Human Services, Public Health Service; 1989. DHHS Publication No. (CDC)89-8411. [Google Scholar]
- 22.Hammond D, Fong GT, McNeill A, Borland R, Cummings KM. Effectiveness of cigarette warning labels in informing smokers about the risks of smoking: findings from the International Tobacco Control (ITC) Four Country Survey. Tob Control. 2006;15(Suppl 3):iii19–iii25. doi: 10.1136/tc.2005.012294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dixon R. Ftc. Federal Trade Commission Report to Congress Pursuant to the Federal Cigarette Labeling and Advertising Act. [Accessed on February 1, 2012];Current Practices and Methods of Cigarette Advertising and Promotion. 1967 Jun 30; Available at: http://tobaccodocuments.org/rjr/502071083-1102.html.
- 24.Fischer PM, Richards JW, Jr, Berman EJ, Krugman DM. Recall and eye tracking study of adolescents viewing tobacco advertisements. JAMA. 1989;261:84–89. [PubMed] [Google Scholar]
- 25.United States Food and Drug Administration. Family Smoking Prevention and Tobacco Control Act, H.R. 1256, 111th Cong 2009. [Google Scholar]
- 26.Centers for Disease Control and Prevention (CDC) Cigarette package health warnings and interest in quitting smoking --- 14 countries, 2008–2010. MMWR Morb Mortal Wkly Rep. 2011;60:645–651. [PubMed] [Google Scholar]
- 27.Pierce JP, Gilpin EA. News media coverage of smoking and health is associated with changes in population rates of smoking cessation but not initiation. Tob Control. 2001;10:145–153. doi: 10.1136/tc.10.2.145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.O'Keefe MT. The anti-smoking commercials: a study of television's impact on behavior. Public Opinion Quarterly. 1971;35:242–248. [Google Scholar]
- 29.Hamilton JL. The demand for cigarettes: advertising, health scare, and the cigarette advertising ban. Rev Econ Stat. 1972;54:401–411. [Google Scholar]
- 30.Simonich WL. Government Anti-Smoking Policies. New York: Lang Publishing; 1991. [Google Scholar]
- 31.Dalton MA, Sargent JD, Beach ML, et al. Effect of viewing smoking in movies on adolescent smoking initiation: a cohort study. Lancet. 2003;362:281–285. doi: 10.1016/S0140-6736(03)13970-0. [DOI] [PubMed] [Google Scholar]
- 32.Healton C. Who's afraid of the truth? Am J Public Health. 2001;91:554–558. doi: 10.2105/ajph.91.4.554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jones WJ, Silvestri GA. The Master Settlement Agreement and its impact on tobacco use 10 years later: lessons for physicians about health policy making. Chest. 2010;137:692–700. doi: 10.1378/chest.09-0982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ranson MK, Jha P, Chaloupka FJ, Nguyen SN. Global and regional estimates of the effectiveness and cost-effectiveness of price increases and other tobacco control policies. Nicotine Tob Res. 2002;4:311–319. doi: 10.1080/14622200210141000. [DOI] [PubMed] [Google Scholar]
- 35.Gallet CA, List JA. Cigarette demand: a meta-analysis of elasticities. Health Econ. 2003;12:821–835. doi: 10.1002/hec.765. [DOI] [PubMed] [Google Scholar]
- 36.Jha P, Chaloupka FJ. Tobacco control in developing countries. New York: Oxford University Press; 2000. [Google Scholar]
- 37.Debucquoy-Dodley D. [Accessed on December 30, 2011];Hospital: Smokers need not apply [CNN website] 2011 Dec 30; Available at http://articles.cnn.com/2011-12-30/us/us_pennsylvania-nicotine-testing_1_secondhand-smoke-smokers-nicotine?_s=PM:US.
- 38.Glantz SA. Meta-analysis of the effects of smokefree laws on acute myocardial infarction: an update. Prev Med. 2008;47:452–453. doi: 10.1016/j.ypmed.2008.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Warner KE Robert Wood Johnson Foundation. Tobacco control policy. San Francisco: Jossey-Bass; 2006. [Google Scholar]
- 40.Wasserman J, Manning WG, Newhouse JP, Winkler JD. The effects of excise taxes and regulations on cigarette smoking. J Health Econ. 1991;10:43–64. doi: 10.1016/0167-6296(91)90016-g. [DOI] [PubMed] [Google Scholar]
- 41.Farkas AJ, Gilpin EA, White MM, Pierce JP. Association between household and workplace smoking restrictions and adolescent smoking. JAMA. 2000;284:717–722. doi: 10.1001/jama.284.6.717. [DOI] [PubMed] [Google Scholar]
- 42.Albers AB, Siegel M, Cheng DM, Biener L, Rigotti NA. Relation between local restaurant smoking regulations and attitudes towards the prevalence and social acceptability of smoking: a study of youths and adults who eat out predominantly at restaurants in their town. Tob Control. 2004;13:347–355. doi: 10.1136/tc.2003.007336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Fichtenberg CM, Glantz SA. Effect of smoke-free workplaces on smoking behaviour: systematic review. BMJ. 2002;325:188. doi: 10.1136/bmj.325.7357.188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Fiore MC, Novotny TE, Pierce JP, et al. Methods used to quit smoking in the United States. Do cessation programs help? JAMA. 1990;263:2760–2765. [PubMed] [Google Scholar]
- 45.Cummings KM, Hyland A. Impact of nicotine replacement therapy on smoking behavior. Annu Rev Public Health. 2005;26:583–599. doi: 10.1146/annurev.publhealth.26.021304.144501. [DOI] [PubMed] [Google Scholar]
- 46.Cummings KM, Hyland A, Fix B, et al. Free nicotine patch giveaway program 12-month follow-up of participants. Am J Prev Med. 2006;31:181–184. doi: 10.1016/j.amepre.2006.03.027. [DOI] [PubMed] [Google Scholar]
- 47.Brunnhuber K, Cummings KM, Feit S, Sherman S, Woodcock J. Putting Evidence into Practice: Smoking Cessation. BMJ Clinical Evidence. London: BMJ Publishing; 2007. [Google Scholar]
- 48.Cummings KM, Mahoney MC. Strategies for smoking cessation: what is new and what works? Expert Rev Respir Med. 2008;2:201–213. doi: 10.1586/17476348.2.2.201. [DOI] [PubMed] [Google Scholar]
- 49.Clinical Practice Guideline Treating Tobacco Use and Dependence 2008 Update Panel, Liaisons, and Staff. A clinical practice guideline for treating tobacco use and dependence: 2008 update. A U.S. Public Health Service report. Am J Prev Med. 2008;35:158–176. doi: 10.1016/j.amepre.2008.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Cokkinides VE, Ward E, Jemal A, Thun MJ. Under-use of smoking-cessation treatments: results from the National Health Interview Survey, 2000. Am J Prev Med. 2005;28:119–122. doi: 10.1016/j.amepre.2004.09.007. [DOI] [PubMed] [Google Scholar]
- 51.Orleans CT, Woolf SH, Rothemich SF, Marks JS, Isham GJ. The top priority: building a better system for tobacco-cessation counseling. Am J Prev Med. 2006;31:103–106. doi: 10.1016/j.amepre.2006.03.015. [DOI] [PubMed] [Google Scholar]
- 52.Zhu S, Melcer T, Sun J, Rosbrook B, Pierce JP. Smoking cessation with and without assistance: a population-based analysis. Am J Prev Med. 2000;18:305–311. doi: 10.1016/s0749-3797(00)00124-0. [DOI] [PubMed] [Google Scholar]
- 53.Euromonitor. [Accessed on February 1, 2012];The world market for tobacco [Euromonitor International website] 2006 Available at: http://www.euromonitor.com.
- 54.IARC Handbooks of Cancer Prevention. Methods for Evaluating Tobacco Control Policies. Lyon, France: International Agency Research Cancer; 2008. [Google Scholar]
- 55.World Health Organization. WHO Framework Convention on Tobacco Control. Geneva, Switzerland: 2003. [Accessed November 28, 2011]. Available at: http://www.who.int/fctc/en. [Google Scholar]
- 56.Cummings KM, Orleans CT. [Accessed February 2, 2012];Policies to Achieve a Smoke-Free Society: A Research Agenda for 2010–2015 [Substance Abuse Policy Research Program website] 2009 Oct; Available at http://www.saprp.org/research_agenda.cfm.
- 57.Reduced Lung-Cancer Mortality with Low-Dose Computed Tomographic Screening. N Engl J Med. 2011 doi: 10.1056/NEJMoa1102873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lightwood JM, Dinno A, Glantz SA. Effect of the California tobacco control program on personal health care expenditures. PLoS Med. 2008;5:e178. doi: 10.1371/journal.pmed.0050178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.United States Food and Drug Administration. [Accessed on January 2, 2012];Overview: Cigarette Health Warnings. Available at http://www.fda.gov/TobaccoProducts/Labeling/ucm259214.htm.