Abstract
Objective
To evaluate whether routinely performed ECGs in older people from the general population have added value for cardiovascular risk management beyond the information that is already available from their medical records
Design
Observational, prospective cohort study.
Setting
General population.
Subjects
A total of 566 participants aged 85 years (377 women, 189 men)
Methods
Lifelong history of cardiovascular disease was assessed through medical records obtained from general practitioners. Baseline ECGs were evaluated for prior myocardial infarction and atrial fibrillation. During a 5-year follow-up period, complete cardiovascular mortality and morbidity data were gathered
Results
During 5 years of follow-up, 262/566 (46%) participants died, of whom 102/262 (39%) died from cardiovascular disease. Participants with a history of cardiovascular disease at age 85 years (284/566, 50%) had an increased cardiovascular mortality (HR 2.7, 95% CI 1.8–4.1) and morbidity (HR myocardial infarction 2.1, 95% CI 1.3–3.6; HR stroke 2.7, 95% CI 1.6–4.9) compared with those without such a history. Participants with major ECG abnormalities (102/566, 18%) had an increased cardiovascular mortality (HR 1.8, 95% CI 1.1–2.8), but no increase of cardiovascular morbidity compared with those without major ECG abnormalities. In both participants with and without a history of cardiovascular disease, the presence of major ECG abnormalities was not associated with increased cardiovascular mortality or morbidity
Conclusions
In older people from the general population, a history of cardiovascular disease is a strong predictor of cardiovascular mortality and morbidity. Although abnormal findings on routine ECGs predict cardiovascular mortality, they do not provide additional prognostic information beyond the information available from medical records. Therefore, when accurate medical records are available, programmatic ECG recording is not effective in older people.
Keywords: Aged 80 and over, aged, cardiovascular diseases, electrocardiography, family practice, medical records, risk management
Preventive therapy in older people with cardiovascular disease is considered effective, but the elderly at risk are often under-treated. Routinely performed ECGs in the general population could possibly identify older people at increased risk of cardiovascular mortality and accelerated functional decline.
Medical information about patients’ history of cardiovascular disease, available from the medical records from general practitioners, effectively selects the elderly at increased cardiovascular risk (both mortality and morbidity).
Although abnormal findings on routine ECGs in elderly people predict cardiovascular mortality, they do not provide additional prognostic information beyond the information available from medical records.
When accurate medical records are available, programmatic ECG recording is not effective in older people from the general population.
Although the debate is ongoing [1], numerous studies have indicated that preventive measures in older people with cardiovascular disease are probably (at least) as effective as in younger age groups [2–9], and as a consequence age limits have gradually disappeared from cardiovascular guidelines [10–14]. In the cardiovascular risk management of older people, the majority of older patients with a history of cardiovascular disease are identified by the medical records held by their primary care physicians. Nevertheless, routinely performed electrocardiograms (ECGs) may have added value for cardiovascular risk management of the older population, and this has so far never been studied.
Earlier we have shown that routinely performed ECGs in a population-based sample of 85-year-olds result in detection of individuals with atrial fibrillation (prevalence 10%) and prior myocardial infarction (prevalence 9%), both associated with (cardiovascular) mortality and accelerated functional decline [15]. Because both prior myocardial infarction and atrial fibrillation are often clinically unrecognized in older people [15–17], these conditions frequently remain untreated. Programmatic recording of ECGs could improve identification of older people not known to have cardiovascular disease, and thus possibly improve the treatment and prognosis of these patients.
Until now, a programme of routine ECGs in older people in the general population has not been implemented. To examine whether such an approach is useful, one needs to know whether routinely recorded ECGs add valuable information beyond that provided by patients’ medical records, which are often easily accessible and already contain accurate information on existing cardiovascular disease and previous cardiovascular events.
Therefore, in a prospective, population-based cohort study of 566 individuals aged 85 years who were followed up for 5 years, we evaluated whether ECG recording in older people from the general population has additional value for cardiovascular risk management, beyond information derived from existing medical records.
Material and methods
Study population
The Leiden 85-plus Study is an observational, prospective population-based study of inhabitants of the city of Leiden in the Netherlands. Between September 1997 and September 1999, 705 persons reached the age of 85 years and were eligible to participate. There were no selection criteria regarding health or demographic characteristics. A total of 599 (85%) persons were enrolled. All participants gave informed consent. Participants were visited at their homes, where face-to-face interviews, blood samples and an ECG were obtained.
Baseline clinical data
In the Netherlands, all inhabitants are registered at a local general practice, or, when institutionalized, are cared for by a nursing-home physician. For each participant, the general practitioner (or, where applicable, the nursing home physician) was asked about the history of cardiovascular disease using a standardized questionnaire, which included questions on present and past cardiovascular pathologies, including myocardial infarction, stroke, angina pectoris, arrhythmias, peripheral arterial disease, and heart failure. When any or a combination of these pathologies was confirmed, participants were considered to have a history of cardiovascular disease. For all participants, classic (cardiovascular) risk factors, including hypertension, hypercholesterolemia, diabetes mellitus, and (history of) smoking were determined. Hypertension was defined as a history of hypertension confirmed by the primary care physician or a mean systolic blood pressure > 160 mmHg (Korotkoff phase I), measured on two occasions with a mean interval of two weeks. Hypercholesterolemia was mapped to a total cholesterol level of ≥6.5 mmol/L. Diabetes mellitus was considered present when confirmed by the primary care physician, when non-fasting glucose levels were > 11.0 mmol/L, or when, according to pharmacist's records, a participant was taking anti-diabetic medication. All participants were interviewed about present and past smoking habits. Current and past smokers of cigarettes, cigars, and pipes were considered to have a smoking history.
Baseline ECG recording
Electrocardiograms were recorded on a Siemens Sicard 440 (Erlangen, Germany) and transmitted to the ECG Core Laboratory in Glasgow Royal Infirmary for automated Minnesota Coding, in one batch after completion of the study [18], [19]. In addition ECGs were reviewed by one of the authors (PWM) to exclude coding errors due to technical causes. Prior myocardial infarction and atrial fibrillation were considered “major ECG abnormalities” because they are highly prevalent and may have therapeutic implications. Prior myocardial infarction was defined as the presence of Minnesota Code 1-1 or 1-2 (excluding 1-2-8), and atrial fibrillation was mapped to Minnesota Code 8-3-1. Treating physicians were not informed about ECG results, unless participants had acute clinical symptoms during the screening visit and a preliminary evaluation by the ECG apparatus revealed major abnormalities requiring therapeutic intervention according to existing guidelines in 1997–1999.
Clinical endpoints
All-cause and cause-specific mortality
All participants were followed for mortality until aged 90 years using data from the municipal Register Office. Causes of death were obtained from Statistics Netherlands, where all national death certificates were coded according to the ICD, 10th revision [20]. The causes of death were divided into cardiovascular (ICD-10 codes I00–I99) and non-cardiovascular causes (all other ICD-10 codes). The assignment of cause of death was made independent of study ECG results.
(Non-)fatal myocardial infarction
All participants were followed for incident non-fatal and fatal myocardial infarction until aged 90 years. An incident myocardial infarction on the annual ECG was defined as the first appearance of Minnesota Codes 1-1 or 1-2, or the first appearance of Minnesota Code 1-3 in combination with the first appearance of Minnesota Code 5-x in the same myocardial area. All incident myocardial infarctions recorded by ECG were visually confirmed by one of the authors (PWM). Also, information was collected yearly from the primary care physicians on clinically proven incident myocardial infarctions. A fatal incident myocardial infarction was categorized by cause of death codes I21–I23 (ICD-10).
(Non-)fatal stroke
All participants were followed for the occurrence of stroke until aged 90 years. Information on clinically diagnosed incident stroke was collected annually from the primary care physicians. A fatal incident stroke was categorized by cause of death codes I61–I69 (ICD-10).
Data analysis
Incidence of cardiovascular mortality and morbidity was calculated by the life table method and expressed as a percentage per observed person year at risk. Hazard ratios and 95% confidence intervals were calculated in a Cox proportional-hazards model, and adjusted for sex, income, and education. Data analysis was performed using SPSS 12.0 for Windows (SPSS Inc., Chicago, IL, USA).
Results
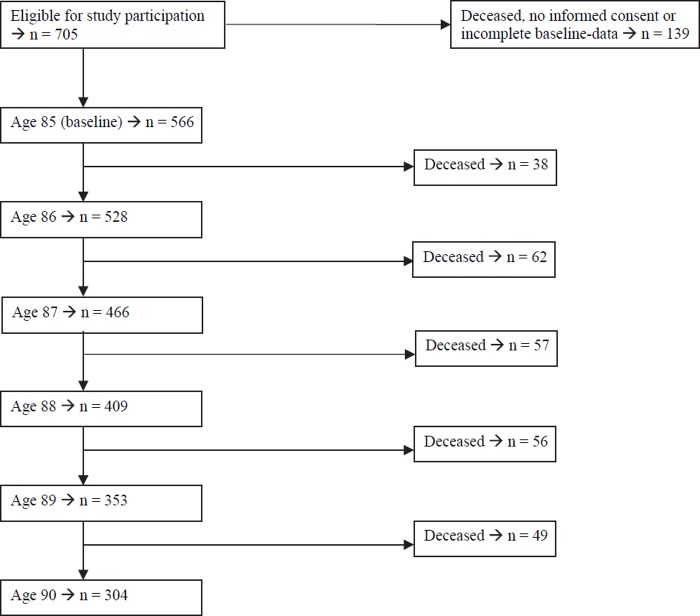
From the 599 participants who were enrolled in the Leiden 85-plus Study, a total of 566 participants completed all baseline measurements. Due to mortality the number of participants gradually diminished to 304 by age 90 years (Figure 1). All participants were followed for mortality and causes of death, the yearly rate of missing clinical data varying between 2% and 5%.
Figure 1. .
Annual numbers of survivors and deceased in the Leiden 85-plus Study.
Table I summarizes baseline characteristics of all participants. In 284/566 (50%) of all participants, the general practitioner reported a history of cardiovascular disease. In 102/566 (18%) of all participants, major ECG abnormalities were observed. Of these, 52 (9%) had prior myocardial infarction and 56 (10%) had atrial fibrillation. Six participants (1%) had both. Of the classic risk factors, hypertension (325/558, 58%) and a history of smoking (271/556, 49%) were highly prevalent.
Table I.
Sociodemographic and cardiovascular characteristics at age 85 years (n = 566).
| n | % | |
| Sociodemographic characteristics | ||
| Women | 377 | 67 |
| Monthly family income > €750 | 273 | 49 |
| Non-institutionalized living | 464 | 82 |
| Additional education after primary school | 196 | 35 |
| History of cardiovascular disease | ||
| No cardiovascular pathology | 282 | 50 |
| One or more cardiovascular pathologies | 284 | 50 |
| Specification of cardiovascular pathologies | ||
| Myocardial infarction | 57 | 10 |
| Stroke | 55 | 10 |
| Angina pectoris | 107 | 19 |
| Arrhythmia | 115 | 20 |
| Peripheral arterial disease | 62 | 11 |
| Heart failure | 70 | 12 |
| Major ECG abnormalities | ||
| Prior myocardial infarction | 52 | 9 |
| Atrial fibrillation | 56 | 10 |
| Classic risk factors | ||
| Hypertension | 325 | 58 |
| Hypercholesterolemia | 125 | 22 |
| Diabetes mellitus | 91 | 16 |
| Present or past smoking | 271 | 49 |
Notes: History of cardiovascular disease (according to general practitioner) included myocardial infarction, stroke, angina pectoris, arrhythmia, peripheral arterial disease and heart failure. Major ECG abnormalities included prior myocardial infarction (Minnesota Codes 1-1 or 1-2, excluding 1-2-8) and atrial fibrillation (Minnesota Code 8-3-1). Hypertension defined as systolic blood pressure > 160 mmHg or history of hypertension (according to general practitioner). Hypercholesterolemia defined as total cholesterol level ≥ 6.5 mmol/L.
During 5 years of follow-up, 262/566 (46%) participants died, with cardiovascular disease as the cause of death in 102/262 (39%) participants. Table II shows incidences of mortality and cardiovascular morbidity during follow-up, depending on a history of cardiovascular disease and on major ECG abnormalities successively, followed by the corresponding hazard ratios. Participants with a history of cardiovascular disease and participants with major ECG abnormalities had increased hazard ratios for (cardiovascular) mortality during the follow-up period. Participants with a history of cardiovascular disease also had increased cardiovascular morbidity risks (see Table II).
Table II.
Mortality and cardiovascular morbidity from age 85 years onwards, depending on history of cardiovascular disease and presence of major ECG abnormalities at age 85 years (n = 566).
| History of cardiovascular disease |
Major ECG abnormalities |
|||||
| Yes (n = 284) | No (n = 282) | Hazard ratio | Yes (n = 102) | No (n = 464) | Hazard ratio | |
| Mortality | ||||||
| All-cause | 15.9 (13.5–18.4) | 8.5 (6.9–10.2) | 1.9 (1.5–2.4) | 17.0 (12.7–21.3) | 11.0 (9.4–12.5) | 1.4 (1.1–1.9) |
| Cardiovascular | 7.0 (5.3–8.6) | 2.7 (1.8–3.6) | 2.7 (1.8–4.1) | 7.9 (5.0–10.9) | 4.0 (3.1–4.9) | 1.8 (1.1–2.8) |
| Non-cardiovascular | 9.0 (7.1–10.8) | 5.9 (4.5–7.2) | 1.5 (1.1–2.1) | 9.1 (5.9–12.2) | 6.9 (5.7–8.1) | 1.2 (0.8–1.8) |
| (Non-)fatal MI | 4.9 (3.5–6.3) | 2.4 (1.5–3.3) | 2.1 (1.3–3.6) | 3.9 (1.8–6.0) | 3.5 (2.6–4.3) | 1.1 (0.6–2.1) |
| (Non-)fatal stroke | 5.5 (4.0–6.9) | 1.9 (1.1–2.7) | 2.7 (1.6–4.9) | 5.3 (2.8–7.7) | 3.1 (2.3–4.0) | 1.6 (0.9–2.8) |
Notes: MI = myocardial infarction. Incidence data are presented as point estimates per 100 person years at risk (95% confidence interval); hazard ratios by Cox regression, adjusted for sex, education, and income (95% confidence interval). History of cardiovascular disease (according to general practitioner) included myocardial infarction, stroke, angina pectoris, arrhythmia, peripheral arterial disease, and heart failure. Major ECG abnormalities included prior myocardial infarction (Minnesota Codes 1-1 or 1-2, excluding 1-2-8) and atrial fibrillation (Minnesota Code 8-3-1).
Table III shows the association between the presence of major ECG abnormalities and mortality and cardiovascular morbidity, in strata depending on history of cardiovascular disease. Among participants without a history of cardiovascular disease, participants with (previous undetected) major ECG abnormalities (29/282, 10%) had roughly similar risks of cardiovascular mortality and morbidity compared with those without major ECG abnormalities. Among the participants with a history of cardiovascular disease, participants with major ECG changes (73/284, 26%) had similar risks of cardiovascular mortality and morbidity compared with those with a history of cardiovascular disease but without major ECG abnormalities (see Table III).
Table III.
Association between the presence of major ECG abnormalities and mortality and cardiovascular morbidity, in strata depending on history of cardiovascular disease at age 85 years (n = 566).
| History of cardiovascular disease |
||
| Yes (n = 284) | No (n = 282) | |
| Major ECG abnormalities yes/no (n/n) | 73/211 | 29/253 |
| Mortality | ||
| All-cause | 1.2 (0.8–1.6) | 1.5 (0.9–2.7) |
| Cardiovascular | 1.4 (0.8–2.3) | 1.8 (0.7–4.8) |
| Non-cardiovascular | 1.0 (0.6–1.6) | 1.4 (0.7–2.9) |
| (Non-)fatal myocardial infarction | 1.0 (0.5–2.0) | 0.8 (0.2–3.3) |
| (Non-)fatal stroke | 1.1 (0.6–2.1) | 1.8 (0.5–6.3) |
Notes: Data are presented as hazard ratios (95% confidence interval), adjusted for sex, education, and income. History of cardiovascular disease (according to general practitioner) included myocardial infarction, stroke, angina pectoris, arrhythmia, peripheral arterial disease, and heart failure. Major ECG abnormalities included prior myocardial infarction (Minnesota Codes 1-1 or 1-2, excluding 1-2-8) and atrial fibrillation (Minnesota Code 8-3-1).
Discussion
In older people from the general population, a history of cardiovascular disease (present in 50%) is a strong predictor of cardiovascular mortality and morbidity. Therefore, knowledge of previous or present cardiovascular disease from an accurate medical record is the cornerstone of cardiovascular risk management for patients in old age [21]. In addition to these medical records data, the present study shows that the programmatic recording of a routine ECG does not add prognostic information on cardiovascular risks in older people. Therefore, programmatic recording of routine ECGs in elderly people, when accurate medical records are available, is probably not effective.
Our study is the first to describe a pragmatic, dual approach to cardiovascular risk management in old age, by first using all relevant clinical data in medical records, and then taking into account the main results from routine ECGs. Earlier studies of cohorts of older people have described the value of the ECG in identifying previously undetected ECG abnormalities [16], [17], [22–24]. However, these investigations focused on one specific abnormality, mainly either myocardial infarction or atrial fibrillation and not both anomalies as in the present study. Furthermore, in these earlier studies the history of specific cardiovascular pathologies was self-reported by participants, which in older persons is known to be associated with misclassification and under-reporting [25].
The present population-based cohort study has several strengths. First, recruitment was highly successful and follow-up data were nearly complete, due to annual visits to the participants and general practitioners. Second, data on participants’ history of cardiovascular disease and incident cardiovascular events were obtained from the medical records held by general practitioners, independent of study ECG results. In the Netherlands, where thorough record keeping is customary, these records are usually accurate, also because inhabitants are enlisted in only one general practice. Third, study ECG recordings were evaluated by a validated computerized method based on the Minnesota Code, frequently used in large epidemiological studies [18], [19]. Although this method is not recommended for use in daily practice, in clinical studies it not only avoids observer bias but also is at least as accurate as visual evaluation by experts who are blinded for clinical data [26], [27]. Finally, during follow-up, all study endpoints were accurately obtained by combining clinical information from general practitioners, annual ECG recordings, and data from municipal and national death registries, thus increasing the power of the study. However, type-2 error due to a relatively small sample size, as indicated by the wide 95% confidence intervals in Table III, may still have influenced our results.
Earlier studies have shown that preventive measures against cardiovascular disease are often lacking in older people [28–30]. The findings of this study have implications for cardiovascular risk management in older people. As a first step, a thorough search through the medical records for any history of cardiovascular disease may be important, given that this study identified 50% of older people at an increased risk of (cardiovascular) mortality and recurrent cardiovascular events from details recorded in their medical records. These elderly people have every right to receive secondary preventive treatment according to current guidelines.
Additional routine ECG recording in older people with a history of cardiovascular disease does not add substantial risk information to that already known. In these patients, major ECG abnormalities on routine ECGs are generally already known and would therefore not render new therapeutic implications. Performing routine ECGs in older people without a history of cardiovascular disease has no added prognostic value either, although 10% of these older people in the present study had previously undetected atrial fibrillation or prior myocardial infarction. Although the cardiovascular mortality and morbidity risks of this group of participants were not significantly increased, clinicians might individually consider therapeutic and secondary preventive measures for these patients, making the interpretation of the relevance of these unrecognized major ECG abnormalities more complicated.
In conclusion, a structured approach to routinely recording ECGs in older people with or without a history of cardiovascular disease has no prognostic value beyond the information already documented in the medical record. Therefore, programmatic routine ECG screening in elderly people is not recommended. Exploring the medical records of older people for a history of cardiovascular disease plays a key role in their cardiovascular risk stratification, identifying 50% of the older population as candidates for preventive measures. Medical records should thus be kept precisely.
Acknowledgements
The Leiden 85-plus Study was partly supported by an unrestricted grant from the Dutch Ministry of Health, Welfare and Sports.
Ethics approval
Ethics approval was given by the Medical Ethical Committee of the Leiden University Medical Center.
Conflict of interest
None declared.
References
- 1.Strandberg TE, Pitkala KH, Berglind S, Nieminen MS, Tilvis RS. Multifactorial intervention to prevent recurrent cardiovascular events in patients 75 years or older: The Drugs and Evidence-Based Medicine in the Elderly (DEBATE) study: A randomized, controlled trial. Am Heart J. 2006;152:585–92. doi: 10.1016/j.ahj.2006.02.006. [DOI] [PubMed] [Google Scholar]
- 2.Bulpitt CJ. Secondary prevention of coronary heart disease in the elderly. Heart. 2005;91:396–400. doi: 10.1136/hrt.2004.045054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Collaborative meta-analysis of randomised trials of antiplatelet therapy for prevention of death, myocardial infarction, and stroke in high risk patients. BMJ. 2002;324:71–86. doi: 10.1136/bmj.324.7329.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shepherd J, Blauw GJ, Murphy MB, Bollen ELEM, Buckley BM, Cobbe SM, et al. Pravastatin in elderly individuals at risk of vascular disease (PROSPER): A randomised controlled trial. Lancet. 2002;360:1623–30. doi: 10.1016/s0140-6736(02)11600-x. [DOI] [PubMed] [Google Scholar]
- 5.Hunt D, Young P, Simes J, Hague W, Mann S, Owensby D, et al. Benefits of pravastatin on cardiovascular events and mortality in older patients with coronary heart disease are equal to or exceed those seen in younger patients: Results from the LIPID trial. Ann Intern Med. 2001;134:931–40. doi: 10.7326/0003-4819-134-10-200105150-00007. [DOI] [PubMed] [Google Scholar]
- 6.Wei L, Ebrahim S, Bartlett C, Davey PD, Sullivan FM, MacDonald TM. Statin use in the secondary prevention of coronary heart disease in primary care: Cohort study and comparison of inclusion and outcome with patients in randomised trials. BMJ. 2005;330:821. doi: 10.1136/bmj.38398.408032.8F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gotto AM., Jr Statin therapy and the elderly: SAGE Advice? Circulation. 2007;115:681–3. doi: 10.1161/CIRCULATIONAHA.106.678300. [DOI] [PubMed] [Google Scholar]
- 8.Gottlieb SS, McCarter RJ, Vogel RA. Effect of beta-blockade on mortality among high-risk and low-risk patients after myocardial infarction. N Engl J Med. 1998;339:489–97. doi: 10.1056/NEJM199808203390801. [DOI] [PubMed] [Google Scholar]
- 9.Fox KM, Bertrand M, Ferrari R, Remme WJ, Simoons ML, Remme WJ, et al. Efficacy of perindopril in reduction of cardiovascular events among patients with stable coronary artery disease: Randomised, double-blind, placebo-controlled, multicentre trial (the EUROPA study) Lancet. 2003;362:782–8. doi: 10.1016/s0140-6736(03)14286-9. [DOI] [PubMed] [Google Scholar]
- 10.Williams MA, Fleg JL, Ades PA, Chaitman BR, Miller NH, Mohiuddin SM, et al. Secondary prevention of coronary heart disease in the elderly (with emphasis on patients > = 75 years of age): An American Heart Association Scientific Statement from the Council on Clinical Cardiology Subcommittee on Exercise, Cardiac Rehabilitation, and Prevention. Circulation. 2002;105:1735–43. doi: 10.1161/01.cir.0000013074.73995.6c. [DOI] [PubMed] [Google Scholar]
- 11.De Backer G, Ambrosioni E, Borch-Johnsen K, Brotons C, Cifkova R, Dallongeville J, et al. European guidelines on cardiovascular disease prevention in clinical practice: Third Joint Task Force of European and other Societies on Cardiovascular Disease Prevention in Clinical Practice. Eur Heart J. 2003;24:1601–10. doi: 10.1016/s0195-668x(03)00347-6. [DOI] [PubMed] [Google Scholar]
- 12.Smith SC, Allen J, Blair SN, Bonow RO, Brass LM, Fonarow GC, et al. AHA/ACC guidelines for secondary prevention for patients with coronary and other atherosclerotic vascular disease: 2006 update – Endorsed by the National Heart, Lung, and Blood Institute. Circulation. 2006;113:2363–72. doi: 10.1161/CIRCULATIONAHA.106.174516. [DOI] [PubMed] [Google Scholar]
- 13.Clinical Guideline A. London: National Institute for Clinical Excellence; 2006. Prophylaxis for patients who have experienced a myocardial infarction. [Google Scholar]
- 14.Fuster V, Ryden LE, Asinger RW, Cannom DS, Crijns HJ, Frye RL, et al. ACC/AHA/ESC guidelines for the management of patients with atrial fibrillation: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology Committee for Practice Guidelines and Policy Conferences (Committee to develop guidelines for the management of patients with atrial fibrillation) developed in collaboration with the North American Society of Pacing and Electrophysiology. Eur Heart J. 2001;22:1852–923. doi: 10.1053/euhj.2001.2983. [DOI] [PubMed] [Google Scholar]
- 15.De Ruijter W, Westendorp RGJ, Macfarlane PW, Jukema JW, Assendelft WJJ, Gussekloo J. The routine electrocardiogram for cardiovascular risk stratification in old age: The Leiden 85-Plus Study. J Am Geriatr Soc. 2007;55:872–7. doi: 10.1111/j.1532-5415.2007.01180.x. [DOI] [PubMed] [Google Scholar]
- 16.Sheifer SE, Gersh BJ, Yanez ND, III, Ades PA, Burke GL, Manolio TA. Prevalence, predisposing factors, and prognosis of clinically unrecognized myocardial infarction in the elderly. J Am Coll Cardiol. 2000;35:119–26. doi: 10.1016/s0735-1097(99)00524-0. [DOI] [PubMed] [Google Scholar]
- 17.Nadelmann J, Frishman WH, Ooi WL, Tepper D, Greenberg S, Guzik H, et al. Prevalence, incidence and prognosis of recognized and unrecognized myocardial infarction in persons aged 75 years or older: The Bronx Aging Study. Am J Cardiol. 1990;66:533–7. doi: 10.1016/0002-9149(90)90477-i. [DOI] [PubMed] [Google Scholar]
- 18.Macfarlane PW, Latif S. Automated serial ECG comparison based on the Minnesota code. J Electrocardiol. 1996;29 (Suppl):29–34. doi: 10.1016/s0022-0736(96)80016-1. [DOI] [PubMed] [Google Scholar]
- 19.Prineas RJ, Crow RS, Blackburn H. The Minnesota code manual of electrocardiographic findings: Standards and procedures for measurement and classification. Boston, MA: Wright; 1982. [Google Scholar]
- 20.World Health Organization. Geneva: World Health Organization; 2006. International Classification of Diseases and Related Disorders. [Google Scholar]
- 21.Mitka M. Electronic health records, after-hours care lag in US primary care practices. JAMA. 2006;296:2913–4. doi: 10.1001/jama.296.24.2913. [DOI] [PubMed] [Google Scholar]
- 22.Sheifer SE, Manolio TA, Gersh BJ. Unrecognized myocardial infarction. Ann Intern Med. 2001;135:801–11. doi: 10.7326/0003-4819-135-9-200111060-00010. [DOI] [PubMed] [Google Scholar]
- 23.Benjamin EJ, Wolf PA, D'Agostino RB, Silbershatz H, Kannel WB, Levy D. Impact of atrial fibrillation on the risk of death. Circulation. 1998;98:946–52. doi: 10.1161/01.cir.98.10.946. [DOI] [PubMed] [Google Scholar]
- 24.Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation as an independent risk factor for stroke: The Framingham Study. Stroke. 1991;22:983–8. doi: 10.1161/01.str.22.8.983. [DOI] [PubMed] [Google Scholar]
- 25.O'Donnell CJ, Glynn RJ, Field TS, Averback R, Satterfield S, Friesenger GC, et al. Misclassification and under-reporting of acute myocardial infarction by elderly persons: Implications for community-based observational studies and clinical trials. J Clin Epidemiol. 1999;52:745–51. doi: 10.1016/s0895-4356(99)00054-2. [DOI] [PubMed] [Google Scholar]
- 26.Kors JA, van Herpen G, Wu J, Zhang Z, Prineas RJ, van Bemmel JH. Validation of a new computer program for Minnesota coding. J Electrocardiol. 1996;29 (Suppl):83–8. doi: 10.1016/s0022-0736(96)80025-2. [DOI] [PubMed] [Google Scholar]
- 27.Tuinstra CL, Rautaharju PM, Prineas RJ, Duisterhout JS. The performance of three visual coding procedures and three computer programs in classification of electrocardiograms according to the Minnesota Code. J Electrocardiol. 1982;15:345–50. doi: 10.1016/s0022-0736(82)81007-8. [DOI] [PubMed] [Google Scholar]
- 28.Ramsay SE, Whincup PH, Lawlor DA, Papacosta O, Lennon LT, Thomas MC, et al. Secondary prevention of coronary heart disease in older patients after the national service framework: Population based study. BMJ. 2006;332:144–5. doi: 10.1136/bmj.38704.770127.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sudlow M, Rodgers H, Kenny RA, Thomson R. Population based study of use of anticoagulants among patients with atrial fibrillation in the community. BMJ. 1997;314:1529–30. doi: 10.1136/bmj.314.7093.1529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tran CTT, Laupacis A, Mamdani MM, Tu JV. Effect of age on the use of evidence-based therapies for acute myocardial infarction. Am Heart J. 2004;148:834–41. doi: 10.1016/j.ahj.2003.11.028. [DOI] [PubMed] [Google Scholar]