Abstract
Stem cell and gene therapies are being pursued as strategies for repairing damaged cardiac tissue following myocardial infarction in an attempt to prevent heart failure. The chemokine receptor-4 (CXCR4) and its ligand, CXCL12, play a critical role in stem cell recruitment post-acute myocardial infarction. Whereas progenitor cell migration via the CXCL12/CXCR4 axis is well characterized, little is known about the molecular mechanisms of CXCR4 mediated modulation of cardiac hypertrophy and failure. We used gene therapy to test the effects of CXCR4 gene delivery on adverse ventricular remodeling due to pressure overload. We assessed the effect of cardiac overexpression of CXCR4 during trans-aortic constriction (TAC) using a cardiotropic adeno-associated viral vector (AAV9) carrying the CXCR4 gene. Cardiac overexpression of CXCR4 in mice with pressure overload prevented ventricular remodeling, preserved capillary density and maintained function as determined by echocardiography and in vivo hemodynamics. In isolated adult rat cardiac myocytes, CXCL12 treatment prevented isoproterenol induced hypertrophy and interrupted the calcineurin/NFAT pathway. Finally, a complex involving the L-type calcium channel, β2-adenoreceptor, and CXCR4 (Cav1.2/β2AR/CXCR4) was identified in healthy cardiac myocytes and was shown to dissociate as a consequence of heart failure. CXCR4 administered to the heart via gene transfer prevents pressure overload induced heart failure. The identification of CXCR4 participation in a Cav1.2-β2AR regulatory complex provides further insight into the mechanism by which CXCR4 modulates calcium homeostasis and chronic pressure overload responses in the cardiac myocyte. Together these results suggest AAV9.CXCR4 gene therapy is a potential therapeutic approach for congestive heart failure.
Keywords: heart failure, cardiac remodeling, gene delivery, adeno-associated virus, chemokines
1. Introduction
CXCR4, a G protein–coupled 7-transmembrane receptor, in conjunction with its primary ligand CXCL12, is a critical determinant of stem cell recruitment to the heart post-ischemia promoting cardiac myocyte survival and angiogenesis. This ligand/receptor system may also participate in cardiac regeneration during acute myocardial ischemic events [1–3]. At the molecular level, CXCR4 appears to modulate at least two other membrane-associated functions in cardiac myocytes, namely β-adrenergic signaling and L-type calcium channel (LTCC) activity [4]. In failing myocardium, CXCR4 association with β2-adrenergic receptors (β2-AR) in the cardiac myocyte may contribute to cardioprotective signaling [5]. However, the role of CXCR4 on long-term ventricular remodeling due to hypertrophy and heart failure is still unknown.
CXCL12 plays an essential role in recruiting and homing of bone marrow derived progenitor cells [6, 7]. The increased expression of CXCL12 in ischemic tissue is postulated to act as a cellular signal that attracts potentially beneficial stem cells to the heart. The recruited stem cells can potentiate the repair, and possibly regenerate, damaged myocardium by preventing apoptosis, inducing angiogenesis and inhibiting fibrosis, all leading to a preservation of global cardiac function. CXCL12, acting through CXCR4 has indeed been shown to recruit bone marrow-derived cells to the infarcted heart, and to increase homing of the bone marrow derived cells following injury. [11, 13, 14]}. CXCL12 gene therapy induces recruitment of circulating progenitor cells to the myocardium in rodent infarct models leading to cardioprotection through angiogenesis, cardiogenesis, and enhancing cell survival thereby improving ventricular function and survival [8–11] Such findings support CXCL12 as a potential therapeutic modality in ischemic cardiovascular disease. For this reason, human clinical trials utilizing CXCL12 gene therapy have been initiated for the treatment of acute MI and also in acute limb ischemia (Clinical Trials.gov: NCT01082094, NCT01410331). Conversely, elevated expression of the CXCL12/CXCR4 axis may be detrimental rather than beneficial depending on disease pathogenesis. Specifically, ectopic expression of CXCR4 increases myocardial infarct size and impairs cardiac pump function in the setting of ischemia/reperfusion injury in the rat [12]. The beneficial effect of CXCL12 may potentially be masked by its simultaneous recruitment of inflammatory cells, which can damage myocardium and augment apoptosis [12]. Moreover, CXCL12 can induce both survival and apoptotic signals via CXCR4 which may ultimately determine the fate of afflicted tissues [15, 16]. The impact of CXCR4 in regulating myocardial function and cardiac myocyte survival may be dependent on the myocardial microenvironment. These studies highlight the critical balance between inflammation and progenitor cell repair mechanisms in the heart.
CXCR4 has been shown to associate with β2-adrenergic receptors (β2-AR) in cardiac myocytes [5]. β-ARs are intimately involved in the pathogenesis of heart failure. β-AR signaling through G-protein cascades play pivotal roles in normal cardiac myocyte function by directly or indirectly regulating Ca2+ influx and consequently, myocardial contractility. β1AR and β2AR have unique spatial organization in the CM leading to compartmentalization of their respective signals [17]. Myocardial failure typically involves an increase in Gαs activity of β1-ARs, and this activity may be countered by β2-AR expression and signaling [18]. CXCR4 reported involvement with β2-AR pro-survival pathways, the enhancement of Erk 1/2 phosphoryaltion and the inhibition of p38, suggests a role for CXCR4 in cardioprotection [5].
Chronic left ventricular (LV) pressure overload, as seen in long-standing systemic arterial hypertension or LV outflow tract obstruction, induces myocardial compensation but ultimately leads to adverse ventricular remodeling and heart failure. The physiological relevance of CXCR4 in chronic pressure overload responses is not known. We utilized the Transverse Aortic Constricton (TAC) model in the mouse to induce hypetrophy and heart failure. Cardiac gene therapy using AAV vectors has been proven to be safe and efficacious in humans and we tested whether AAV9.CXCR4 could prevent maldaptive ventricular remodeling and heart failure.
2. Material and methods
The investigation conforms with the Guide for the Care and Use of Laboratory Animals published by the US National Institutes of Health.
2.1. Transverse-aortic constriction (TAC)
Studies were conducted in male mice 8 to 10 weeks of age (25–30g). Mice were anesthetized with 0.5–0.7 ml of a 1x Avertin solution (mixtures of 2-2-2 tribromoethanol and tert-amyl alcohol) administered via intraperitoneal injection. The mice were ventilated with a tidal volume of 0.1 ml and a respiratory rate of 120 breaths per minute (Harvard Apparatus). A longitudinal incision of 2–3 mm was made in the proximal sternum to allow visualization of the aortic arch. The transverse aortic arch was ligated between the innominate and left common carotid arteries with an overlaid 27-gauge needle. The needle was then immediately removed, leaving a discrete region of constriction.
2.2. Echocardiography and in vivo hemodynamic
Eight-week old C57BL/6 mice were acquired from Jackson laboratories. Mice were anesthetized with intraperitoneal ketamine (100µg/g) for echocardiographic analysis. Two-dimensional images and M-mode tracings were recorded on the short-axis at the level of the papillary muscle to determine percent fractional shortening and ventricular dimensions (GE Vivid 7 Vision). One day after echocardiography, in vivo hemodynamics were performed using a 1.2Fr pressure-volume (PV) conductance catheter (Scisense, Ontario, Canada). Mice were anesthetized with an intraperitoneal injection mixture of urethane (1mg/g), etomidate (10µg/g), morphine (1µg/g) and were then intubated via a tracheotomy and mechanically ventilated at 7µl/g tidal volume and 125 respirations/minute. The PV catheter was placed in the left ventricle via an apical stab approach as previously described [19]. Pressure-volume data were analyzed using IOX2 software (EMKA technologies). All procedures were approved by and performed in accordance with the Institutional Animal Care and Use Committee of the Mount Sinai School of Medicine. The investigation conforms with the Guide for the Care and Use of Laboratory Animals published by the US National Institutes of Health (NIH Publication No. 85-23, revised 1996).
2.3. AAV9 production
Self-complementary AAV9 was generated using pds.AAV2.eGFP and the CXCR4 gene was cloned from pcDNA6.CXCR4 (provided by Dr. George Diaz, Mount Sinai). The eGFP was removed from the AAV construct due to viral packaging constraints. The CXCR4 consensus sequence was amplified using PCR, and the product was gel purified. CXCR4 was ligated into the pds.AAV9 backbone and construct integrity was confirmed by sequencing. The recombinant AAVs were produced by transfecting 293T cells with two plasmids, one containing the AAV viral genome and the other containing the genes for replication, the capsid protein, and the Adenovirus helper function. The AAV particles in the cell culture media were collected by precipitation with ammonium sulfate and then purified by ultracentrifugation on an iodixanol gradient. The AAV was concentrated with the iodixanol being exchanged for Lactate Ringers solution by multiple dilution-and-concentration steps using a centrifugal concentrator. The AAV titer was determined by quantitative real time PCR and western blots.
2.4. Isolation of adult rat ventricular myocytes
Ventricular myocytes were isolated from adult rat hearts as described previously [4]. Briefly, rat hearts were excised and the aorta quickly cannulated. The hearts were first perfused with a low calcium Tyrode’s buffer and then with an enzyme solution containing collagenase and protease. They were minced, filtered, and resuspended in Tyrode’s solution, and cultured in medium M199 containing appropriate supplements.
2.5. Calcineurin activity assay
Calcineurin activity was determined in isolated cardiac myocytes treated with CXCL12 (100ng/mL), isoproterenol (10uM) and in combination. Post-treatment, cell lysate was harvested and analyzed as per manufacturer’s protocol (ENZO Lifesciences, Pennsylvania, USA). Briefly, calcineurin activity was demonstrated by adding a calcineurin specific phospho-peptide substrate to the cell lysate and visualization of free-phosphates accomplished by a colorimetric assay.
2.6. Western blot analysis
Membrane and tissue homogenates were prepared as described [5, 20]. Proteins were resolved on 10% SDS-PAGE gels followed by transfer to PVDF membranes (Millipore, Massachusetts, USA). Membranes were probed with designated antibodies.
2.7. Immunoprecipitation
Cardiac myocytes were isolated as previously described [5]. Myocytes were treated with Adeno.flagCXCR4 at MOI 100 for 48 hours in serum-free medium. Anti-flag conjugated beads (Sigma, Missouri, USA) were added to 1 mg of protein lysate and incubated overnight at 4°C. Beads were then collected by centrifugation and washed in TBS. Samples were then boiled in Laemmli’s buffer and subjected to SDS-PAGE and immunoblotted with monoclonal antibodies to the protein of interest: CXCR4, GAPDH (Abcam, Cambridge, MA); β2AR (Santa Cruz, Santa Cruz, CA); and anti-Cav1.2 (Upstate Biotech, NY, USA).
2.8. Quantitative real time PCR
ANF, CXCR4, CXCL12 and VEGF-A mRNA levels were determined by real time-PCR using a QuantiTect SYBR Green real time PCR Kit (Qiagen Ltd;Valencia CA). Total RNA was isolated from samples with Trizol reagent (Gibco BRL; Carlsbad, CA) according to the manufacturer’s instructions. Primers were designed to generate short amplification products. The sequences of the specific primers were: ANF-Forward:5’-CCTAAGCCCTTGTGGTGTGT-3’ and Reverse:5’-CAGAGTGGGAGAGGCAAGAC-3’; CXCR4-Forward:5’-CGTCGTGCACAAGTGGATCT-3’; and Reverse:5’-GTTCAGGCAACAGTGGAAGAAG-3’; CXCL12-Forward:5’-CTTCATCCCCATTCTCCTCA-3’ and Reverse:5’-GACTCTGCTCTGGTGGAAGG-3’; VEGF-A: Forward:5'-TACTGCTGTACCTCCACCTCCACCATG-3' and Reverse:5'-TCACTTCATGGGACTTCTGCTCT-3' and 28SrRNA-Forward:5’-CTCGCTGGCCCTTGAAAATCC-3’; and Reverse:5’-CCCAGCCCTTAGAGCCAATCCTTA-3’. Real time PCR was performed in 20-µl reaction volumes using 10 pmol of primers. Reverse transcription was performed at 50°C for 20 minutes, and cDNA was amplified for 37 cycles: 94°C for 10s, 57°C for 15s, and 72°C for 5s. The relative level of gene expression was calculated according to the manufacturer’s recommendations. 18S was used as an internal control to calculate the relative abundance of mRNAs.
2.9. EnzymeLinked Immunosorbent Assay (ELISA)
The amount of VEGF protein in the heart tissue lysates were determined by sandwich ELISA. Quantitation of the levels of immunoreactive VEGF was performed by using a kit purchased from R&D systems (Minneapolis, MN, USA). ELISA was performed according to manufacturer’s instructions.
2.10. Statistical analyses
Numeric data are presented as mean±s.e.m. One-way ANOVA and Student's t-test were utilized with p-values <0.05 considered statistically significant.
3. Results
3.1. Transcriptional regulation of CXCL12 and CXCR4 during adaptive hypertrophy and late stage heart failure in a murine model of pressure overload
Pressure overload induces a hypertrophic response in the ventricular myocardium. This response decreases myocardial wall stress but activates maladaptive hypertrophic pathways, leading to impaired systolic function, cardiac myocyte apoptosis, and fibrosis [21]. We used this model in the current study to induce heart failure (Fig. 1A).
Fig. 1.
TAC Model. (A) The effect of pressure overload on HW:BW ratio at sham, TAC 1day to TAC 8weeks. (B) Transcriptional profile during hypertrophy and heart failure. RNA was isolated from whole ventricular myocardium. Specific mRNA levels were quantified via real-time RT-PCR performed in triplicate (n=5 mice/group *= p<0.05, **=p<0.01, ***=p<0.001)
One early molecular mediator of the hypertrophic response is the transcription factor hypoxia inducible factor 1-α (HIF1α). Expression of HIF1α is necessary for angiogenesis, which in this context promotes and maintains myocardial hypertrophy and increased wall mass [22]. Mechanistically, HIF1α is a key transcription factor governing the regulation of CXCL12 and CXCR4 [23]. CXCL12, in turn, plays important roles in the hypoxic environment in many cell types including cardiac myocytes and has been shown to be anti-apoptotic in cardiac myocytes exposed to hypoxia [24].
These findings led us to investigate whether expression of HIF1α, CXCL12 and CXCR4 is altered during hypertrophy and heart failure progression. We also found that HIF1α is significantly upregulated in the early stages of hypertrophy and returns to basal levels in the heart by 2 weeks post-TAC (Fig. 1B). Both CXCL12 and CXCR4 follow the same pattern of expression with increased mRNA content at the onset of hypertrophy, peaking at 4–7 days, and returning to basal levels by 2 weeks post-TAC. In contrast, expression of the cardiac-specific protein atrial natriuretic factor (ANF) is increased 6-fold by 4 days post-TAC and remains elevated as heart failure progresses (Fig. 1B), indicating sustained ventricular wall stresses due to pressure overload. These results demonstrate the involvement of the CXCL12/CXCR4 axis in chronic pressure overload responses in the myocardium in vivo.
3.2. AAV9.CXCR4 gene therapy prevents adaptive ventricular remodeling and heart failure due to pressure overload
The CXCL12/CXCR4 axis has been studied extensively in acute ischemia due to its role in progenitor cell recruitment, however, the function of CXCL12/CXCR4 during non-ischemic cardiac injuries such as pressure overload is unknown. We hypothesized CXCR4 may be cardioprotective during pressure overload, especially due to the minimal contribution of inflammatory processes in the initial stages of hypertrophy and heart failure. For this study, we utilized cardiotropic AAV serotype 9 encoding CXCR4 [25]. We generated AAV9 constructs encoding CXCR4 and a LacZ control. A dose response was performed which determined 3×1011 viral genomes (vg) per mouse as the most efficient dose for CXCR4 overexpression in the murine heart as illustrated by quantitative PCR, western blot and immunostaining (Fig. 2A–C).
Fig. 2.
AAV9.CXCR4 dose response in vivo. AAV9.CXCR4WT was injected via the tail vein with increasing viral genomes/mouse, ranging from 2e9 to 3e11. Hearts were harvested four weeks post-injection. (A) CXCR4 mRNA was quantified by RT-PCR. (B) CXCR4 protein expression was assessed by western blot. (C) Immunostaining of CXCR4 in the heart indicated proper membrane localization.
AAV9.CXCR4 and AAV9.LacZ were administered via tail vein injection at a dose of 3×1011 vg/mouse. At 4 weeks post-injection, baseline cardiac function was evaluated. AAV9.CXCR4 mice did not exhibit any echocardiographic (Fig. 3A, Table 1), hemodynamic (Fig. 3B, Table 2), or gross anatomical changes due to cardiac CXCR4 overexpression at 4- or 12-weeks post-AAV injection. This indicates long-term overexpression of CXCR4 has no significant effect on myocardial function in the absence of pathological stresses. Additionally, the heart weight:body weight ratios (HW:BW) were similar to those of controls (Fig. 3C).
Fig. 3.
TAC+AAV9.CXCR4 functional studies. (A) Echocardiographic M-mode images at the level of the papillary muscle in sham operated and TAC 8 week mice injected with AAV9.LacZ and AAV9.CXCR4. (B) In vivo hemodyanmic data were acquired using a pressure-volume conductance catheter via an apical open-chest approach. Pre-load reduction studies were done by transiently occluding the inferior vena cava. AAV9.lacZ (Black) AAV9.CXCR4 (green) at baseline, TAC 2weeks, and TAC 8weeks. (C) HW:BW ratio of AAV9.CXCR4 and AAV9.LacZ during pressure overload. At 12 weeks post injection, AAV9.CXCR4 and AAV.9 Lacz had no effects on cardiac function in an absence of TAC.
Table 1.
Echocardiography
| Sham | Control | AAV.LacZ | AAV.CXCR4 |
|---|---|---|---|
| n= | 6 | 6 | 6 |
| IVSd (mm) | 1.04±0.05 | 0.93±0.07 | 0.98±0.07 |
| LVIDd (mm) | 2.97±0.19 | 2.91±0.16 | 3.06±0.13 |
| LVPWd (mm) | 1.04±0.14 | 1.08±0.10 | 1.09±0.07 |
| IVSs (mm) | 1.74±0.05 | 1.54±0.04 | 1.66±0.12 |
| LVIDs (mm) | 1.38±0.06 | 1.33±0.08 | 1.49±0.10 |
| LVPWs (mm) | 1.53±0.18 | 1.72±0.14 | 1.68±0.09 |
| %FS | 53.5±3.7 | 55.0±1.2 | 51.6±3.1 |
| HR (bpm) | 517±26 | 559±18 | 569±22 |
| TAC 2wks | Control | AAV.LacZ | AAV.CXCR4 |
| n= | 5 | 7 | 7 |
| IVSd (mm) | 1.54±0.13 | 1.36±0.17 | 1.00±0.08*** |
| LVIDd (mm) | 2.66±0.36 | 3.13±0.67 | 3.31±0.35* |
| LVPWd (mm) | 1.66±0.17 | 1.33±0.19 | 1.14±0.16* |
| IVSs (mm) | 2.26±0.22 | 1.42±0.27 | 1.75±0.17 |
| LVIDs (mm) | 1.24±0.36 | 1.29±0.66 | 1.66±0.29* |
| LVPWs (mm) | 2.21±0.27 | 2.55±0.29 | 1.82±0.21* |
| %FS | 54.6±7.7 | 51.9±3.4 | 52.5±1.5 |
| HR (bpm) | 522±39 | 570±24 | 540±38 |
| TAC 8wks | Control | AAV.LacZ | AAV.CXCR4 |
| n= | 6 | 5 | 7 |
| IVSd (mm) | 1.12±0.24 | 0.77±0.27 | 1.23±0.16 |
| LVIDd (mm) | 4.28±0.69 | 4.48±0.33 | 3.23±0.43** |
| LVPWd (mm) | 1.27±0.33 | 1.09±0.08 | 1.34±0.15 |
| IVSs (mm) | 1.49±0.32 | 1.36±0.14 | 1.80±0.23 |
| LVIDs (mm) | 3.32±0.12 | 3.51±0.68 | 1.78±0.42*** |
| LVPWs (mm) | 1.73±0.47 | 1.55±0.20 | 1.85±0.21 |
| %FS | 24.5±9.7 | 22.8±8.1 | 45.3±5.9*** |
| HR (bpm) | 532±32 | 547±27 | 550±37 |
Table 2.
In vivo hemodynamics
| Sham | Control | AAV.LacZ | AAV.CXCR4 |
|---|---|---|---|
| n= | 6 | 5 | 5 |
| Pes (mmHg) | 91.1±0.05 | 96.5±2.5 | 95.6±4.1 |
| Ped (mmHg) | 4.3±2.62 | 5.1±3.7 | 3.2±1.1 |
| dP/dtmax (mmHg/sec) | 5291±671 | 5726±1002 | 6187±655 |
| dP/dtmin (mmHg/sec) | −4433±633 | −4475±782 | −5237±746 |
| Tau (ms) | 3.8±0.2 | 4.3±1.3 | 3.9±0.6 |
| EDV (uL) | 44.5±5.32 | 46.1±4.4 | 45.1±5.5 |
| ESV (uL) | 12.1±4.4 | 12.8±2.2 | 15.6±7.3 |
| SV (uL) | 41.3±4.81 | 42.0±5.4 | 39.4±7.3 |
| CO (uL/min) | 16199±1840 | 19065±3001 | 19332±3242 |
| EF (%) | 75.6±5.07 | 82.5±7.9 | 79.7±7.3 |
| SW (mmHg*uL) | 2958±258 | 3319±735 | 3146±558 |
| Ea (mmHg/uL) | 3.07±0.17 | 2.7±0.5 | 2.6±0.6 |
| ESPVR | 5.05±2.3 | 4.4±2.1 | 4.7±1.9 |
| EDPVR | 0.10±0.01 | 0.07±0.03 | 0.08±0.2 |
| PRSW | 81.69±10.5 | 98.1±25 | 89.2±13.2 |
| HR (bpm) | 518±15 | 494±39 | 484±36 |
| TAC 2wks | Control | AAV.LacZ | AAV.CXCR4 |
| n= | 6 | 4 | 6 |
| Pes (mmHg) | 129.3±1.2 | 138±10.1 | 131±6.5 |
| Ped (mmHg) | 7.1±1.5 | 4.2±3.9 | 7.5±3.0 |
| dP/dtmax (mmHg/sec) | 6599±671 | 6726±999 | 6787±506 |
| dP/dtmin (mmHg/sec) | −4433±633 | −5498±332 | −5237±746 |
| Tau (ms) | 4.2±0.3 | 3.9±2.0 | 4.1±0.5 |
| EDV (uL) | 27.5±3.0 | 31.6±7.4 | 49.5±7.5*, |
| ESV (uL) | 3.2±0.9 | 8.8±4.0 | 16.9±4.4 |
| SV (uL) | 24.3±3.2 | 26.8±4.8 | 35.2±4.5 |
| CO (uL/min) | 11155±1420 | 13199±2976 | 15223±1574* |
| EF (%) | 88.8±3.7 | 86.6±6.0 | 70.1±5.3*,# |
| SW (mmHg*uL) | 2378±207 | 2600±936 | 3546±430 |
| Ea (mmHg/uL) | 5.0±0.91 | 4.4±1.0 | 4.2±0.6 |
| ESPVR | 20.4±4.1 | 16.8±3.2 | 8.1±2.1*,## |
| EDPVR | 0.26±0.03 | 0.23±0.08 | 0.18±0.07 |
| PRSW | 176.5±19.5 | 158.4±30 | 142.2±23.2 |
| HR (bpm) | 483±33 | 504±44 | 474±26 |
| TAC 8wks | Control | AAV.LacZ | AAV.CXCR4 |
| n= | 5 | 5 | 5 |
| Pes (mmHg) | 103.3±2.6 | 104.8±4.5 | 123.81±3.9* |
| Ped (mmHg) | 12.5±1.1 | 14.0±1.0 | 7.7±1.1* |
| dP/dtmax (mmHg/sec) | 4238±168 | 4227±275 | 5409±300** |
| dP/dtmin (mmHg/sec) | −3185±196 | −3687±286 | −5033±382** |
| Tau (ms) | 5.4±0.2 | 5.7±0.2 | 4.9±0.3 |
| EDV (uL) | 118±5.9 | 130.7±9.8 | 60.7±3.6*** |
| ESV (uL) | 89.5±2.4 | 93.9±8.5 | 22.6±2.4*** |
| SV (uL) | 25.0±2.1 | 27.1±3.4 | 38.9±3.2* |
| CO (uL/min) | 11296±1295 | 12320±1436 | 17745±1632 |
| EF (%) | 20.9±3.2 | 19.4±4.3 | 64.9±2.8*** |
| SW (mmHg*uL) | 1586±543 | 1999±250 | 3392±244** |
| Ea (mmHg/uL) | 4.0±0.3 | 4.0±0.6 | 3.2±0.8 |
| ESPVR | 3.9±1.9 | 2.9±1.2 | 9.9±2.2** |
| EDPVR | 0.20±0.11 | 0.12±0.08 | 0.13±0.04 |
| PRSW | 80.9±12.0 | 64.2±21.3 | 125.7±19.6* |
| HR (bpm) | 494±27 | 492±26 | 476±19 |
TAC was performed to induce left ventricular pressure overload in AAV9.CXCR4 and AAV9.LacZ mice. At 2 weeks post-TAC, mice overexpressing CXCR4 were protected against hypertrophic remodeling as compared to AAV9.LacZ controls. Specifically, AAV9.CXCR4-treated animals showed reduced septal and posterior wall thickness, as revealed in the echocardiograms (Fig. 3A), and had reduced HW:BWs compared to no AAV9 and AAV9.LacZ controls. Importantly, in vivo hemodynamic measurements indicated that the pre-TAC stroke and end-diastolic volumes with elevated ventricular pressures were maintained and ESPVR was not elevated, indicating CXCR4 overexpression prevented ventricular remodeling in the setting of pressure overload (Fig. 3A–C). Maximal pressures were not significantly different between all study groups (Table 1 & 2).
At 8 weeks post-TAC, AAV9.LacZ controls exhibited a 2-fold increase in HW:BW and a significant decline in function with depressed percent fractional shortening (%FS) and ESPVR. In contrast, AAV9.CXCR4 protected the myocardium from systolic failure. Echocardiography and in vivo hemodynamics revealed maintenance of ventricular volumes and ESPVR with AAV9.CXCR4 (Figs. 3A–C). Collectively, these findings demonstrate the cardioprotective capabilities of CXCR4 on chronic hypertrophic and heart failure responses in the absence of overt, acute hypoxia.
VEGF together with CXCL12 has been shown to promote cardiac stem cell mobilization and myocardial repair in the infarcted heart [14]. Furthermore, the CXCR4/CXCL12 axis upregulates VEGF at both the mRNA and protein levels, and promotes VEGF-mediated tumor angiogenesis, suggesting a potential regulatory interaction between these two angiogenic factors [26]. Our results suggest CXCR4 overexpression maintains myocardial capillary density after TAC 8wk. Cardiac sections were stained with isolectin-488 to identify myocardial capillary density. There were no significant differences at baseline between capillary densities of 4- and 12-week post-AAV9 hearts. AAV9.LacZ post-TAC 8 weeks exhibited a significant reduction in capillary structures associated with the prominent decrease in contractile function (Fig. 4A). In contrast, the AAV9.CXCR4 post-TAC 8 weeks possibly contributed to a pro-angiogenic environment leading to increased capillary density and enhanced systolic function post-TAC (Fig. 4A). We found maintenance of VEGF mRNA and enhanced protein expression in hearts treated with AAV9.CXCR4 subjected to TAC 8wks as compared to TAC+AAV9.LacZ control group (Fig. 4B), suggesting potential VEGF upregulation via a CXCR4 dependent mechanism. VEGF mRNA expression is reduced and protein expression near basal levels in the TAC+vehicle only ( no AAV) and TAC+LacZ groups when compared to baseline hearts. VEGF is typically upregulated in the early stages of cardiac hypertrophy( TAC 2 wks) promoting concentric enlargement [27] . As pathological hypertrophy progresses into heart failure, VEGF expression declines leading to a reduction in capillary density, apoptosis, and myocardial contractile dysfunction. AAV9.CXCR4 overexpression prevents VEGF reduction in pressure overload induced heart failure.
Fig. 4.
VEGF expression during pressure overload. (A) Cardiac sections were stained with isolectin-488 to identify myocardial capillary density. (B) Quantitative real time PCR data demonstrates an increase in VEGF transcription in TAC+AAV.CXCR4 group. (n=4 mice/group *= p<0.05) as compared to TAC+no AAV or TAC+Lacz groups. (C) VEGF protein expression was quantified using standard ELISA assay.
3.3. CXCL12 prevents β-adrenergic induced cardiac myocyte hypertrophy in vitro
The β-AR system is fundamental in the pathogenesis of heart failure. CXCR4 can counteract this β-AR-mediated action, specifically via an interaction with β2-AR [5]. In order to investigate chronic β-AR agonism in vitro, we exposed isolated adult rat cardiac myocytes to isoproterenol (500nM), for 24 hours, to induce cellular hypertrophy. We observed that isoproterenol increased cell size and H3-leucine uptake (enhanced protein sysnthesis) indicating cellular hypertrophy. Importantly, the hypertrophic response of cardiac myocytes significantly increased both CXCL12 and CXCR4 expression suggesting their involvement in myocyte hypertrophy (Fig. 5A). We then treated isolated cardiac myocytes with CXCL12 prior to isoproterenol stimulation. We found that CXCL12 prevented the cardiac myocyte hypertrophic response in vitro with a significant decrease in cell size and H3-leu uptake (Fig. 5B). Although the biological effects of CXCL12 are mainly initiated through CXCR4, recent evidence has indicated CXCR7 is also able to mediate CXCL12 signaling. Therefore, we used AMD3100, a specific CXCR4 inhibitor, to confirm that the CXCL12 anti-hypertrophic effect is directly mediated through CXCR4.
Fig. 5.
CXCL12/CXCR4 expression during cardiac myocyte hypertrophy in vitro. (A) Isolated adult rat cardiac myocytes were treated with isoproterenol (500nM) for 24 hours to induce cellular hypertrophy. Myocytes were immunostained for CXCR4 pre- and post-isoproterenol treatment. Additionally, RNA was harvested from the cell lysates and CXCL12/CXCR4 mRNA content was quantified. (n=4 independent experiments, * p<0.05, ** p<0.01). (B) Isolated adult rat cardiac myocytes were treated with CXC12 (100ng/mL) and isoproterenol (500nM) in the presence or absence of AMD3100 (10µM), CXCR4 antagonist. for 24 hours. When using the CXCR4 inhibitor AMD3100, the cells were pretreated for 45 minutes prior to CXCL12 treatment. Cell size was determined by outlining the myocyte perimeter and H3-leu uptake was measured to detect protein synthesis. (C) Isolated rat ventricular myocytes were treated with isoproterenol as previously described. Endogenous calcineurin acitivity was determined by a colorimetric free-phosphate assay using a calcineurin specific phospho-substrate. Nuclear and cytoplasmic fractions from cardiac myocytes treated with CXCL12 and isoproterenol were analyzed for NFATc3 content. GAPDH was used as a cytoplasmic loading control. RNA was isolated from cardiac myocytes treated with CXCL12 and isoproterenol. The NFAT target and calcineurin inhibitor, MCIP1.4, expression was determined by qPCR. (D) Overexpression of CXCR4 dramatically increases the tolerant threshold of cardiomyocyte to hypertrophic stimuli (isoproterenol at 500 nM) and reduces isoproterenol induced hypertrophy as compared to cells that are not infected. Isolated cardiac myocytes were infected with adenovirus encoding CXCR4 (MOI 100). 48 hours post-infection, cardiac myocytes were treated with isoproterenol as previously described. H3-leu uptake was measured to detect protein synthesis. (E) Whole ventricular tissue was minced, protein isolated and.endogenous calcineurin activity was determined in the lysates of ; no AAV, AAV9.lacZ and AAV9.CXCR4 at TAC 2weeks, and TAC 8weeks by a colorimetric free-phosphate assay using a calcineurin specific phosphosubstrate.
The calcineurin/NFAT (Nuclear factor of activated T-cells) pathway plays a central role in mediating β-AR hypertrophy and heart failure [28]. NFAT is a key transcription factor that initiates the hypertrophic response in cardiac myocytes [29]. In its phosphorylated state, NFAT is cytoplasmic and the calcium dependent phosphatase, calcineurin (PP2B), dephosphorylates NFAT facilitating its translocation into the nucleus. Calcineurin associates with LTCCs and may be activated through microdomain fluctuations in calcium due to its close proximity to the LTCC [30]. CXCR4 has been reported to negatively regulate LTCC activity [4], however, the mechanism(s) underlying this inhibitory effect are not clear. Here, we assessed the role of CXCL12/CXCR4 axis on the regulation of calcineurin/NFAT pathway. To do so, isolated adult rat cardiac myocytes were treated with isoproterenol, in the presence or absence of CXCL12. We found isoproterenol alone significantly increased calcineurin phosphatase activity (54%±4%) whereas CXCL12 prevented isoproterenol induced calcineurin activation (Fig. 5C). Moreover, we observed functional downstream consequences of CXCL12-mediated blockage of calcineurin, including the inhibition of NFAT nuclear translocation and MCIP1.4 expression (modulatory calcineurin-interacting protein 1, exon 4 isoform) (Fig. 5C). We also investigated whether overexpression of CXCR4 increased the tolerant threshold of cardiomyocytes to hypertrophic stimuli in vitro. Isolated cardiac myocytes were infected with adenovirus encoding CXCR4 (MOI 100). 48 hours post-infection, cardiac myocytes were treated with isoproterenol as previously described. Overexpression of CXCR4 significantly reduced the hypertrophic response to isoproterenol, to a similar degree as the ligand, CXCL12, alone. There was an additive trend of CXCR4 overexpression and ligand together, however, this was not statistically significant. (Fig. 5D). Therefore to confirm our hypothesis of the anti-hypertrophic effects of the CXCL12/CXCR4 axis, endogenous calcineurin acitivity was determined in heart lysates of vehicle only, AAV9.lacZ and AAV9.CXCR4 at TAC 2weeks, and TAC 8weeks. We observed significant reduction in calcineurin activation at 2 weeks TAC as compared to AAV9.lacZ group (Fig. 5E). There is no significant difference in TAC 8wks as calcineurin activity is known to be a critical early stage regulator of pathological hypertrophy leading to heart failure [31]. These findings imply CXCR4 mediated attenuation of hypertrophic remodeling in the cardiac myocyte may occur via interruption of the calcineurin/NFAT pathway.
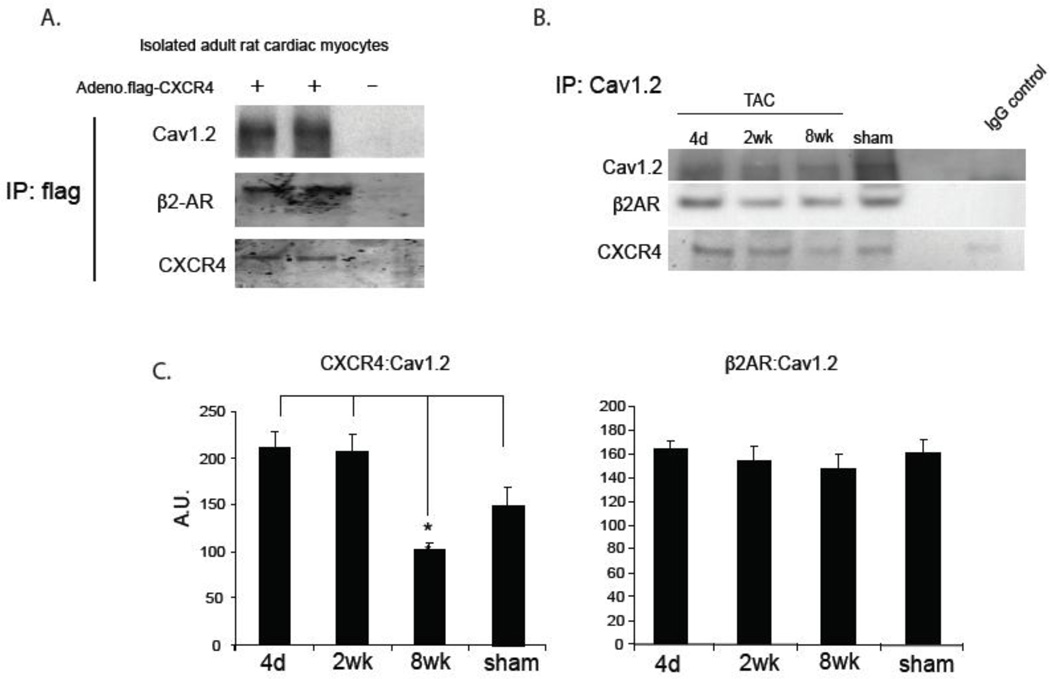
3.4. Cav1.2/β2AR/CXCR4 complex in the cardiac myocyte dissociates in heart failure
We have recently demonstrated a physical interaction between CXCR4 and β2-AR. The CXCR4-β2AR interaction leads to a decrease in β2-AR-induced PKA activity and PKA-dependent phosphorylation of down stream effectors [5]. β2-AR is known to associate with LTCC and regulate calcium channel activity. β2-ARs are enriched in the T-tubular region of myocytes producing focused signaling events and microdomain calcium modulation in the cell. We previously reported that activation of CXCR4 reduces diastolic [Ca+2] accumulation as a result of sustained isoproterenol activation of β-AR. The CXCL12/CXCR4 axis has also been shown to reduce isoproterenol-induced LTCC activity in the cardiac myocyte [4]. Extending these observations, we sought to determine whether CXCR4 is part of a larger complex involving the LTCC. If so, this may potentially explain CXCR4 regulation of calcium homeostasis and thus preventing cardiac myocyte hypertrophy and heart failure. Accordingly, isolated cardiac myocytes were infected with adenovirus encoding 3’ flag-CXCR4. Immunoprecipitation of flag-CXCR4 co-precipitated both Cav1.2 and β2-AR (Fig. 6A). This suggests CXCR4 participates in a large regulatory complex with LTCC. In addition, Cav1.2 also co-precipitated both β2-AR and CXCR4 in ventricular myocardial lysate in sham and animals exposed to pressure overload at 4 days, 2 weeks, and 8weeks. (Fig. 6B–C). Interestingly, the Cav1.2 macromolecular complex with CXCR4 dissociates in late-stage heart failure suggesting a potential role for CXCR4 in regulating β2-AR dependent LTCC function during heart failure.
Fig. 6.
CXCR4 interacts with β2-AR and Cav1.2 in the cardiac myocyte in vitro and in vivo. (A) Isolated cardiac myocytes were infected with adenovirus encoding flag.CXCR4 (MOI 100). 48 hours post-infection, cardiac myocytes were harvested for protein. Protein was subjected to flag immunoprecipitation using anti-flag coated agarose beads followed by western blot. (B) CXCR4 associates with β2-AR and Cav1.2 in the heart in vivo. Whole ventricular tissue was minced and protein isolated. Anti-Cav1.2 antibody was used for immunoprecipitation and membrane was blotted for CXCR4 and β2-AR. (C) Densitometric analysis for CXCR4 and β2-AR is shown (n=5). *P , 0.05
4. Discussion
We have demonstrated a novel anti-remodeling role of the CXCL12/CXCR4 chemokine axis in the cardiac myocyte. The major findings of this study were: 1) CXCL12/CXCR4 is dynamically regulated during hypertrophy and heart failure progression; 2) elevated expression of CXCR4 via AAV9.CXCR4 treatment prevented heart failure induced by pressure overload and maintained capillary density; 3) CXCR4-mediated attenuation of hypertrophic remodeling in the cardiac myocyte may occur via inhibition of the calcineurin/NFAT pathway; 4) CXCR4 participates in a Cav1.2/β2-AR complex in the cardiac myocyte and this association breaks down in heart failure suggesting the cardioprotection elicited by CXCR4 may employ multiple mechanisms including regulation of LTCC function, calcium homeostasis and VEGF regulation.
Previously we reported CXCR4 prevents isoproterenol induced diastolic Ca2+ overload and influences downstream β-AR signaling in isolated cardiac myocytes [5]. Here we have shown that CXCR4 may potentially regulate hypertrophic responses in the heart. A transcriptional profile of sham operated mice compared to one day TAC up to 8 weeks TAC showed a significant and sustained increase of ANF. Importantly, HIF1α is a key regulator of angiogenesis and hypertrophy in response to pressure overload and has been determined to negatively regulate p53 expression [22, 32]. Downregulation of HIF1α leads to an increase in p53 and myocardial contractile dysfunction.
HIF1 α is a major transcription factor for the expression of CXCL12 and CXCR4, each containing hypoxia response elements in their respective promoters [32]. CXCL12/CXCR4 expression mirrors that of HIF1α in vivo, suggesting their possible involvement in myocardial hypertrophy and heart failure. We generated self-complementary (double-stranded) AAV9 vector containing either CXCR4 or LacZ control. AAV9.CXCR4 treatment prevented adverse ventricular remodeling and systolic failure in the mouse 8weeks post-TAC. Importantly, CXCR4 overexpression prevented the acute increase in ESPVR by TAC 2weeks in concordance with inhibition of ventricular hypertrophy. The regulated control of ESPVR under chronic pressure overload by the AAV9.CXCR4 group prevents the subsequent cardiac decompensation and reduction in ESPVR by TAC 8weeks. The cardioprotective effect of AAV9.CXCR4 in the heart correlated with maintenance of capillary density and elevated VEGF production compared to TAC 8 week control groups. The decline in VEGF is a critical mediator in the transition between hypertrophy and heart failure. Elevation of VEGF expression in heart failure by CXCR4 may represent a potential mechanism into the functional benefit observed in chronic pressure overload.
In order to identify downstream signaling consequences of CXCR4 overexpression implicated in cardiac failure, we assessed β-ARs signaling associated with hypertrophy and heart failure. CXCL12 treatment as well as CXCR4 overexpression inhibits isoproterenol induced cardiac myocyte hypertrophy. This inhibition significantly affects the central hypertrophic signaling node, the calcium-dependent calcineurin/NFAT pathway decreasing calcineurin activity, NFAT translocation and MCIP1.4 expression. There is growing evidence calcineurin is activated by subcellular/microdomain changes in calcium concentration operating within the background of massively fluctuating cytosolic calcium levels during myocyte contraction and relaxation [33]. Calcineurin located in T-tubular structures may detect microdoman calcium perturbuations via LTCCs, transient receptor potential channels and also by cytoskeletal disruption of the T-tubular structure causing genetic and metabolic disturbances in the cardiac myocyte. AAV9.CXCR4 treatment prevented calcineurin activity at TAC 2weeks further supporting the anti-hypertrophic capability of CXCR4. These data support the notion of CXCR4 impacting calcium dependent processes such as calcineurin activity and further establishes CXCR4 as a key regulator of calcium homeostasis in the cardiac myocyte undergoing chronic β-AR hypertrophic stresses.
β-ARs are intimately involved in the pathogenesis of heart failure. β-AR signaling through G-protein cascades has evolved to include dimerization and biased signaling as cellular mechanisms to regulate β-AR mediated signals [34, 35]. β1-AR and β2-AR can homo- and heterodimerize leading to unique downstream signaling profiles associated with dimerization [36]. β-ARs regulate and also physically associate with calcium channels in the cardiac myocyte. β2-AR has been shown to regulate LTCCs through a physical association [37]. β1-AR and β2-AR have unique spatial organization in the cardiac myocyte leading to compartmentalization of their respective signals [17]. β1-AR has been shown to induce diffuse production of cAMP, while β2-AR is confined to cAMP production in the T-tubular region. These discrete calcium signaling units in the cardiac myocyte play important roles in regulating microdomain calcium concentrations which have significant impacts on calcium dependent signaling events. It is the breakdown of these units and t-tubule structures which can lead to dysregulated calcium homeostasis associated with heart failure.
We postulated CXCR4 may regulate cardioprotective signaling and possibly inhibit heart failure progression through a calcium regulatory complex involving Cav1.2 and β2-AR. Immunoprecipitation with anti-Cav1.2 antibodies not only identified β2-AR but also CXCR4 association in the hearts of sham operated animals suggesting a basal level of interaction between Cav1.2, β2-AR and CXCR4. Importantly, in four day TAC animals the association tends to increase, however, as pressure overload persists, significant dissociation in late stage heart failure is detected. We hypothesize the disruption of the CXCR4/β2-AR/Cav1.2 complex during heart failure progression leads to a diminished ability of the cardiac myocyte to regulate calcium which may affect downstream processes such as calcineurin activity. The participation of CXCR4 in cardiac myocyte hypertrophy and cardiac failure due to pressure overload further broadens CXCR4 as a target for the treatment of cardiovascular disease.
In this study, we demonstrated that cardiac overexpression of CXCR4 in mice exposed to pressure overload prevented ventricular remodeling and maintained cardiac function, possibly by interrupting the calcineurin/NFAT pathway. In addition, we identified a complex involving Cav1.2/β2-AR/CXCR4 in healthy cardiac myocytes and we found that the complex dissociated during heart failure. CXCR4 participation in a Cav1.2-β2-AR regulatory complex provides further mechanistic insight into how CXCR4 modulates calcium homeostasis and chronic pressure overload responses in the cardiac myocyte.
Highlights.
-
➢
AAV9.CXCR4 gene therapy treatment prevented heart failure induced by TAC.
-
➢
CXCR4 overexpression prevented ventricular remodeling.
-
➢
CXCL12 treatment prevented isoproterenol induced cardiomyocytes hypertrophy.
-
➢
CXCL12/CXCR4 axis inhibited the β-adrenergic-mediated calcineurin/NFAT signaling.
Acknowledgements
Sources of funding
This work was supported, in whole or in part, by the National Heart, Lung and Blood Institute Ruth L. Kirschstein National Research Service Award 1F30HL096344-01 (T.J.L.); Mount Sinai School of Medicine Medical Scientist Training Program GM007280 (T.J.L.), the American Heart Association (grant 10GRNT4180006 to S.T.T); and National Institutes of Health (grant 1K02HL102163-01 to S.T.T; grant R01 HL050000 to R.J.H),.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures. None of the authors have any conflict of interest to disclose.
References
- 1.Ghadge SK, Muhlstedt S, Ozcelik C, Bader M. SDF-1alpha as a therapeutic stem cell homing factor in myocardial infarction. Pharmacol Ther. 2010;129(1):97–108. doi: 10.1016/j.pharmthera.2010.09.011. [DOI] [PubMed] [Google Scholar]
- 2.Penn MS. SDF-1:CXCR4 axis is fundamental for tissue preservation and repair. Am J Pathol. 2010;177(5):2166–2168. doi: 10.2353/ajpath.2010.100803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yu J, Li M, Qu Z, Yan D, Li D, Ruan Q. SDF-1/CXCR4-mediated migration of transplanted bone marrow stromal cells toward areas of heart myocardial infarction through activation of PI3K/Akt. J Cardiovasc Pharmacol. 2010;55(5):496–505. doi: 10.1097/FJC.0b013e3181d7a384. [DOI] [PubMed] [Google Scholar]
- 4.Pyo RT, Sui J, Dhume A, Palomeque J, Blaxall BC, Diaz G, et al. CXCR4 modulates contractility in adult cardiac myocytes. J Mol Cell Cardiol. 2006 Nov;41(5):834–844. doi: 10.1016/j.yjmcc.2006.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Larocca TJ, Schwarzkopf M, Altman P, Zhang S, Gupta A, Gomes I, et al. beta2-Adrenergic Receptor Signaling in the Cardiac Myocyte is Modulated by Interactions with CXCR4. J Cardiovasc Pharmacol. 2010;56(5):548–559. doi: 10.1097/FJC.0b013e3181f713fe. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jo DY, Rafii S, Hamada T, Moore MA. Chemotaxis of primitive hematopoietic cells in response to stromal cell-derived factor-1. J Clin Invest. 2000;105(1):101–111. doi: 10.1172/JCI7954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hughes S. Cardiac stem cells. The Journal of pathology. 2002;197(4):468–478. doi: 10.1002/path.1159. [DOI] [PubMed] [Google Scholar]
- 8.Moore MA, Hattori K, Heissig B, Shieh JH, Dias S, Crystal RG, et al. Mobilization of endothelial and hematopoietic stem and progenitor cells by adenovector-mediated elevation of serum levels of SDF-1, VEGF, and angiopoietin-1. Annals of the New York Academy of Sciences. 2001;938:36–45. doi: 10.1111/j.1749-6632.2001.tb03572.x. [DOI] [PubMed] [Google Scholar]
- 9.Hiasa K, Ishibashi M, Ohtani K, Inoue S, Zhao Q, Kitamoto S, et al. Gene transfer of stromal cell-derived factor-1alpha enhances ischemic vasculogenesis and angiogenesis via vascular endothelial growth factor/endothelial nitric oxide synthase-related pathway: next-generation chemokine therapy for therapeutic neovascularization. Circulation. 2004;109(20):2454–2461. doi: 10.1161/01.CIR.0000128213.96779.61. [DOI] [PubMed] [Google Scholar]
- 10.Abbott JD, Huang Y, Liu D, Hickey R, Krause DS, Giordano FJ. Stromal cell-derived factor-1alpha plays a critical role in stem cell recruitment to the heart after myocardial infarction but is not sufficient to induce homing in the absence of injury. Circulation. 2004;110(21):3300–3305. doi: 10.1161/01.CIR.0000147780.30124.CF. [DOI] [PubMed] [Google Scholar]
- 11.Saxena A, Fish JE, White MD, Yu S, Smyth JW, Shaw RM, et al. Stromal cell-derived factor-1alpha is cardioprotective after myocardial infarction. Circulation. 2008;117(17):2224–2231. doi: 10.1161/CIRCULATIONAHA.107.694992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chen J, Chemaly E, Liang L, Kho C, Lee A, Park J, et al. Effects of CXCR4 gene transfer on cardiac function after ischemia-reperfusion injury. Am J Pathol. 2010;176(4):1705–1715. doi: 10.2353/ajpath.2010.090451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhang F, Cheng J, Lam G, Jin DK, Vincent L, Hackett NR, et al. Adenovirus vector E4 gene regulates connexin 40 and 43 expression in endothelial cells via PKA and PI3K signal pathways. Circ Res. 2005;96(9):950–957. doi: 10.1161/01.RES.0000165867.95291.7b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tang JM, Wang JN, Zhang L, Zheng F, Yang JY, Kong X, et al. VEGF/SDF-1 promotes cardiac stem cell mobilization and myocardial repair in the infarcted heart. Cardiovasc Res. 2011;91(3):402–411. doi: 10.1093/cvr/cvr053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Liehn EA, Tuchscheerer N, Kanzler I, Drechsler M, Fraemohs L, Schuh A, et al. Double-Edged Role of the CXCL12/CXCR4 Axis in Experimental Myocardial Infarction. J Am Coll Cardiol. 2011;58(23):2415–2423. doi: 10.1016/j.jacc.2011.08.033. [DOI] [PubMed] [Google Scholar]
- 16.Vlahakis SR, Villasis-Keever A, Gomez T, Vanegas M, Vlahakis N, Paya CV. G protein-coupled chemokine receptors induce both survival and apoptotic signaling pathways. J Immunol. 2002;169(10):5546–5554. doi: 10.4049/jimmunol.169.10.5546. [DOI] [PubMed] [Google Scholar]
- 17.Nikolaev VO, Moshkov A, Lyon AR, Miragoli M, Novak P, Paur H, et al. Beta2-adrenergic receptor redistribution in heart failure changes cAMP compartmentation. Science. 2010;327(5973):1653–1657. doi: 10.1126/science.1185988. [DOI] [PubMed] [Google Scholar]
- 18.Zheng M, Zhu W, Han Q, Xiao RP. Emerging concepts and therapeutic implications of beta-adrenergic receptor subtype signaling. Pharmacol Ther. 2005;108(3):257–268. doi: 10.1016/j.pharmthera.2005.04.006. [DOI] [PubMed] [Google Scholar]
- 19.Pacher P, Nagayama T, Mukhopadhyay P, Batkai S, Kass DA. Measurement of cardiac function using pressure-volume conductance catheter technique in mice and rats. Nat Protoc. 2008;3(9):1422–1434. doi: 10.1038/nprot.2008.138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tarzami ST, Calderon TM, Deguzman A, Lopez L, Kitsis RN, Berman JW. MCP-1/CCL2 protects cardiac myocytes from hypoxia-induced apoptosis by a G(alphai)-independent pathway. Biochem Biophys Res Commun. 2005;335(4):1008–1016. doi: 10.1016/j.bbrc.2005.07.168. [DOI] [PubMed] [Google Scholar]
- 21.Drazner MH. The progression of hypertensive heart disease. Circulation. 2011;123(3):327–334. doi: 10.1161/CIRCULATIONAHA.108.845792. [DOI] [PubMed] [Google Scholar]
- 22.Sano M, Minamino T, Toko H, Miyauchi H, Orimo M, Qin Y, et al. p53-induced inhibition of Hif-1 causes cardiac dysfunction during pressure overload. Nature. 2007;446(7134):444–448. doi: 10.1038/nature05602. [DOI] [PubMed] [Google Scholar]
- 23.Liu YL, Yu JM, Song XR, Wang XW, Xing LG, Gao BB. Regulation of the chemokine receptor CXCR4 and metastasis by hypoxia-inducible factor in non small cell lung cancer cell lines. Cancer Biol Ther. 2006;5(10):1320–1326. doi: 10.4161/cbt.5.10.3162. [DOI] [PubMed] [Google Scholar]
- 24.Zhang M, Mal N, Kiedrowski M, Chacko M, Askari AT, Popovic ZB, et al. SDF-1 expression by mesenchymal stem cells results in trophic support of cardiac myocytes after myocardial infarction. FASEB J. 2007;21(12):3197–3207. doi: 10.1096/fj.06-6558com. [DOI] [PubMed] [Google Scholar]
- 25.Suckau L, Fechner H, Chemaly E, Krohn S, Hadri L, Kockskamper J, et al. Long-term cardiac-targeted RNA interference for the treatment of heart failure restores cardiac function and reduces pathological hypertrophy. Circulation. 2009;119(9):1241–1252. doi: 10.1161/CIRCULATIONAHA.108.783852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Liang Z, Brooks J, Willard M, Liang K, Yoon Y, Kang S, et al. CXCR4/CXCL12 axispromotes VEGF-mediated tumor angiogenesis through Akt signaling pathway. Biochem Biophys Res Commun. 2007;359(3):716–722. doi: 10.1016/j.bbrc.2007.05.182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sano M, Minamino T, Toko H, Miyauchi H, Orimo M, Qin Y, et al. p53-induced inhibition of Hif-1 causes cardiac dysfunction during pressure overload. Nature. 2007;446(7134):444–448. doi: 10.1038/nature05602. [DOI] [PubMed] [Google Scholar]
- 28.Vega RB, Bassel-Duby R, Olson EN. Control of cardiac growth and function by calcineurin signaling. J Biol Chem. 2003;278(39):36981–36984. doi: 10.1074/jbc.R300023200. [DOI] [PubMed] [Google Scholar]
- 29.Passier R, Zeng H, Frey N, Naya FJ, Nicol RL, McKinsey TA, et al. CaM kinase signaling induces cardiac hypertrophy and activates the MEF2 transcription factor in vivo. J Clin Invest. 2000;105(10):1395–1406. doi: 10.1172/JCI8551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chen X, Nakayama H, Zhang X, Ai X, Harris DM, Tang M, et al. Calcium influx through Cav1.2 is a proximal signal for pathological cardiomyocyte hypertrophy. J Mol Cell Cardiol. 2010;50(3):460–470. doi: 10.1016/j.yjmcc.2010.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Molkentin JD. Calcineurin and beyond: cardiac hypertrophic signaling. Circ Res. 2000;87(9):731–738. doi: 10.1161/01.res.87.9.731. [DOI] [PubMed] [Google Scholar]
- 32.Wenger RH, Stiehl DP, Camenisch G. Integration of oxygen signaling at the consensus HRE. Sci STKE. 2005;2005(306):re12. doi: 10.1126/stke.3062005re12. [DOI] [PubMed] [Google Scholar]
- 33.Heineke J, Ritter O. Cardiomyocyte calcineurin signaling in subcellular domains: from the sarcolemma to the nucleus and beyond. J Mol Cell Cardiol. 2012;52(1):62–73. doi: 10.1016/j.yjmcc.2011.10.018. [DOI] [PubMed] [Google Scholar]
- 34.Gomes I, Ijzerman AP, Ye K, Maillet EL, Devi LA. G protein-coupled receptor heteromerization: a role in allosteric modulation of ligand binding. Mol Pharmacol. 2011;79(6):1044–1052. doi: 10.1124/mol.110.070847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Whalen EJ, Rajagopal S, Lefkowitz RJ. Therapeutic potential of beta-arrestin- and G protein-biased agonists. Trends Mol Med. 2010;17(3):126–139. doi: 10.1016/j.molmed.2010.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zhu WZ, Chakir K, Zhang S, Yang D, Lavoie C, Bouvier M, et al. Heterodimerization of beta1- and beta2-adrenergic receptor subtypes optimizes beta-adrenergic modulation of cardiac contractility. Circ Res. 2005;97(3):244–251. doi: 10.1161/01.RES.0000176764.38934.86. [DOI] [PubMed] [Google Scholar]
- 37.Davare MA, Avdonin V, Hall DD, Peden EM, Burette A, Weinberg RJ, et al. A beta2 adrenergic receptor signaling complex assembled with the Ca2+ channel Cav1.2. Science. 2001;293(5527):98–101. doi: 10.1126/science.293.5527.98. [DOI] [PubMed] [Google Scholar]