Abstract
In 2010, the Accreditation Council for Graduate Medical Education released its resident duty hours restrictions, requiring that faculty monitor their residents’ patient handoffs to ensure that residents are competent in handoff communications. Although studies have reported the need to improve the effectiveness of the handoff and a variety of curricula have been suggested and implemented, a common method for teaching and evaluating handoff skills has not been developed. Also in 2010, engineers, informaticians, and physicians interested in patient handoffs attended a symposium in Savannah, Georgia, hosted by the Association for Computing Machinery, entitled Handovers and Handoffs: Collaborating in Turns. As a result of this symposium, a workgroup formed to develop practical and readily implementable educational materials for medical educators involved in teaching patient handoffs to residents. In this article, the result of that yearlong collaboration, the authors aim to provide clarity on the definition of the patient handoff, to review the barriers to performing effective handoffs in academic health centers, to identify available solutions to improve handoffs, and to provide a structured approach to educating residents on handoffs via a curricular blueprint. The authors’ blueprint was developed to guide educators in customizing handoff education programs to fit their specific, local needs. Hopefully, it also will provide a starting point for future research into improving the patient handoff. Increasingly complex patient care environments require both innovations in handoff education and improvements in patient care systems to improve continuity of care.
Although patient care has involved, for at least the last century, the input of multiple physicians, the traditional model of care includes one primary physician who assumes responsibility for each patient and others who consult in their areas of expertise. This established method provides continuity of care by minimizing patient transfers, often at the cost of prolonging an individual physician's workday.1,2 In the 21st century, the shift from this traditional model of inpatient medicine to a team-based model and the advent of resident duty hours restrictions have called attention to the patient handoff. In its 2006 National Patient Safety Goals, the Joint Commission recommended standardizing patient handoff procedures and using “read-back” and “repeat-back” practices during transitions of care.3 In 2010, the Joint Commission then incorporated the patient handoff into its Accreditation Standards,3 and the Accreditation Council for Graduate Medical Education (ACGME) released its resident duty hours restrictions, which went into effect in July 2011, requiring faculty to monitor their residents’ patient handoffs to ensure that residents are competent in handoff communications.4
Educating residents to perform patient handoffs effectively offers several benefits, including promoting patient safety, maintaining continuity of care, and enhancing and maintaining professionalism through teamwork.5 Although a variety of curricular methods have been suggested and implemented at academic health centers (AHCs) in the United States, no one has developed a comprehensive approach to teaching and assessing residents’ competence in patient handoffs. Our increasing reliance on electronic health records (EHRs) and other such technologies also necessitates that we consider the complex, tightly structured, highly interdependent, and technology-driven clinical organization of AHCs in designing curricula to teach patient handoffs to residents.
Designing a Curriculum Blueprint for Teaching Patient Handoff Skills to Residents
Computer-supported cooperative work (CSCW) addresses how computer technologies help people work together. Those involved in CSCW have developed workflow systems that help teams to communicate and to coordinate their actions.6 In health care, engineers, informaticians, and computer scientists have been working with physicians to support their clinical work for over two decades through the development of computerized physician order entry and electronic medical records.7–9
Given these collaborations and the increasing use of technology in patient handoffs, the CSCW 2010 conference committee issued a call for papers describing common themes and distinctive features of handoffs. This call led to a symposium entitled Handovers and Handoffs: Collaborating in Turns at the Association for Computing Machinery's 22nd annual CSCW conference held in Savannah, Georgia, in February 2010. This conference offered a venue for researchers and educators from the United States, Canada, and South America to discuss the state of patient handoffs. As a result of these discussions, a smaller workgroup, of which we were a part, formed to develop practical and readily implementable educational materials for program directors and other educators involved in teaching handoffs to residents. In this article, the product of our yearlong collaboration, we aim to provide clarity on the definition of the patient handoff, to review the barriers to performing effective handoffs in AHCs, to identify available solutions to improve handoffs, and to provide a structured approach to educating residents on handoffs via a curriculum blueprint.
Defining the Patient Handoff
Patient handoffs are complex and multifaceted events that occur daily at AHCs.10 The purpose of the handoff is to ensure continuity of care and high-quality, safe care decisions in a specific physical and cultural environment. Typically, handoffs involve the communication of information among participants; however, they are more than the passive transfer of information. The cornerstone of the handoff is the transfer of responsibility between the participants.11 Consequently, handoffs require a bidirectional conversation including active involvement of the sender and the receiver.12,13
Residents participating in patient handoffs may not interact regularly with each other, may be located in different parts of the AHC, may have different skill and experience levels, or may come from different clinical backgrounds. Despite these potential obstacles, residents need to transmit efficiently all of the relevant information about a group of patients and the responsibility for their care to the incoming physicians. At a minimum, residents should provide patient identification, diagnostic summary, the patient's current condition and trajectory, a plan of care, a prioritized to-do list, and a plan for anticipated events.14 Patients, physicians, and the public expect this brief exchange to result in a shared understanding of the patient among those responsible for his or her care. In particular, the receiving physician should be able to understand all likely contingencies and changes in the patient's condition.15–17 Effective handoffs include a meaningful dialogue that creates an opportunity to identify and correct errors in real time. These brief conversations then must establish meaning between the participants,18 resulting in a shared understanding of the patient, the care goals and tasks, and the possible scenarios that may pose a threat to the patient during the care process.
Issues With Patient Handoffs
Although handoffs are common events in nearly all patient care settings, the literature to date highlights a few important issues. Poorly conducted handoffs result in the omission of care tasks, misunderstandings, errors, and adverse events.11,12,19–21 Discontinuity of care due to ineffective handoffs also has been associated with longer hospital stays and increased costs.12,22,23 Communication failures during handoffs frequently lead to uncertainty during subsequent patient care decisions, which can result in patient harm.11,12,19,20,23,24 As a result, regulatory agencies and accrediting organizations have increased their focus on handoffs as a key component of patient safety. Although handoffs have increased at AHCs under new resident duty hours restrictions,19 many residency programs provide only “on-the-job” instruction, without a formal curriculum. This paucity of formal curricula contributes to concerns about the effects of resident duty hours restrictions on inpatient continuity of care.2,25,26 Thus, despite evidence that communication plays a critical role in effective patient care,27 residents may be unable to conduct handoffs properly because of inexperience or their inability to synthesize information or to deal with inadequate staffing or patient emergencies. They also may be unwilling to conduct handoffs because of a desire to personally rather than collaboratively provide continuity of care, a sense of obligation to complete assigned tasks for their patients, or a fear that handoffs may not meet expectations.19,28 A particular problem with on-the-job instruction is that faculty, who were educated before the 80-hour workweek restrictions were enacted, may themselves lack training and a full appreciation of the importance of the transfer-of-care process, making them reluctant to incorporate teaching or supervision of the handoff into their clinical teaching and practice responsibilities.29
Technology and Tools for Improving Patient Handoffs
Research related to the design and improvement of handoffs in the fields of nursing and, to a lesser degree, medicine spans nearly 30 years and has emphasized continuity of patient care as a critical goal.24,30–32 Elements of handoff practices during end-of-shift transfers in high-risk industries, such as space shuttle in-flight management, nuclear power plants, and dispatch services, have been studied by human factors engineering researchers.17,33 Their approaches may offer guidance for medical handoffs, such as how to standardize the sequence of information items and ensure that the individual receiving the information has the opportunity to ask questions and to clarify responses.11 This research contributed to the Joint Commission's recommendation to standardize patient handoffs in medicine. However, implementing this recommendation has been challenging, in part because of a lack of guidance on how to interpret the term standardization given the significant range in the scope and content of handoffs across and within clinical units.11,34
Because the handoff is critical to patient safety, an important area for future work is the design of electronic handoff tools, either freestanding or as part of EHRs. Handoffs currently are not adequately supported by national EHR vendors. Historically, most physicians support the “off-the-record” status of the written sign-out, maintaining that it is not officially part of a patient's medical records; yet, recently, some physicians have tried to incorporate sign-out directly into the EHR.35 A key concern in this debate is increased liability for physicians due to the discoverability of sensitive communications.
Educational Approaches and Considerations for Improving Patient Handoffs
The 2010 ACGME standards for resident duty hours and the learning environment require that residents and practicing physicians receive formal training in patient handoff communication.36 A variety of methods for teaching handoff skills have been described in the literature, including live, Web, and video-based teaching modules,37–41 information frameworks designed or adapted to handoffs,42–44 the use of health information technology to support information exchange,5,45 and expanding the number of sources of information by including nurses and senior physicians in handoffs.12 Recent work also has focused on the use of objective skills-based examinations to allow residents to practice handoff skills in a simulated or an applied context.46,47 Despite this plethora of methods, educators are lacking a comprehensive system for teaching and assessing resident handoff skills that adheres to the new ACGME requirements.
Many of these methods to teach effective patient handoffs focus on residents’ ability to communicate and on systems that support their workflow, rather than on their development of the medical knowledge and clinical decision-making skills that ensure that the information they are communicating is appropriate and properly understood by the receiver.11,12 Even less attention is paid to professionalism, systems-based practice, and quality improvement. For other elements of clinical practice, such as taking a history, conducting a physical, making a differential diagnosis, or performing bedside procedures, there are formal curricula, systematic processes for teaching and evaluation, and graded autonomy as residents develop competence.48
To fill this gap, we set out to create a curriculum blueprint to assist educators in developing a similar method for teaching patient handoff skills. Our workgroup participated in monthly conference calls, with each participant bringing a unique perspective to the discussions, providing us with a comprehensive view of the field of patient handoffs. We generated a large list of tools and resources related to the topic and condensed it into our final curriculum blueprint, which then was reviewed internally and field tested at various AHCs across the country.
Our blueprint (see Table 1) introduces a set of initially validated tools for teaching and assessing handoff skills. It includes teaching and learning strategies and opportunities to apply and test what has been learned, suited to promote the progressive development of handoff competencies throughout residency. The structure of our blueprint is based on the six recognized and widely adopted ACGME competencies (patient care, medical knowledge, practice-based learning and improvement, interpersonal and communication skills, professionalism, and systems-based practice) that residents are required to cultivate during training.49 Our blueprint pairs activities for teaching handoffs with assessments that measure residents’ performance on the relevant competencies. This method extends the focus of curricula beyond the communication of information to medical knowledge, systems-based practice, and professionalism. Educators can adapt our blueprint to their program's specific needs, as customization is a necessary function of any tool to optimally teach and support handoffs within the given local context.
Table 1.
Curricular Blueprint for Teaching and Assessing Resident Handoff Skills Based on the Accreditation Council for Graduate Medical Education (ACGME) Competencies*
| ACGME competency |
|||||||
|---|---|---|---|---|---|---|---|
| Recommended competencies and modes of assessment | Training level of targeted participants | Patient care | Medical knowledge | Interpersonal and communication skills | Professionalism | Practice-based learning and improvement | Systems-based practice |
| Educational lecture/Web tutoria1 with posttest38,39 | Intern | ✓ | ✓ | ✓ | ✓ | ||
| Video with formal debriefing and self-assessment37,40 | Intern | ✓ | ✓ | ✓ | |||
| “iSoBAR” checklist with formative feedback42 | Intern | ✓ | ✓ | ✓ | ✓ | ||
| Personalized instruction and formative feedback from senior residents or faculty | Intern | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Direct supervision and formative feedback from senior residents or faculty (until the handoff becomes an entrustable professional activity)65 | Intern | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Web simulation47 | Intern | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Observed simulated handoff experience (OSHE) with debriefing and formative feedback46 | Intern | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Summative assessment of regular handoffs and delegation as entrustable professional activity54,56 (from senior residents or faculty) | Intern | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Review of special circumstance handoffs (intensive care unit, emergency department, etc ) with formative feedback from senior residents or faculty | Junior/senior resident | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Summative assessment of special circumstance handoffs as entrustable professional activities46,47 (from senior residents or faculty) | Intern | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| OSHE (special circumstance handoffs) with debriefing and formative feedback65 | Junior resident | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Resident-led morning report with feedback66 | Junior/senior resident | ✓ | ✓ | ✓ | |||
| Train-the-trainer session for supervising intern handoffs | Junior/senior resident | ✓ | ✓ | ✓ | ✓ | ||
| Handoff case presentations with feedback | Junior/senior resident | ✓ | ✓ | ✓ | ✓ | ||
| Root-cause analysis of handoff errors (2–3 analyses)67 | Junior/senior resident | ✓ | ✓ | ||||
| Debriefing of overnight or night float residents to assess the adequacy of the handoff provided by the primary team (with feedback to the primary team)23 | Junior/senior resident | ✓ | ✓ | ||||
| Postcall/posttransfer interviews of residents to identify overnight/posttransfer events due to inadequate information exchange during handoff (with feedback from team that handed off) 19,23 | Junior/senior resident | ✓ | ✓ | ||||
| Posthandoff interviewing of oncoming resident/team for adequacy of information transfer (with feedback from team that handed off)57,68 | Junior/senior resident and faculty | ✓ | ✓ | ||||
| Quality audits and feedback of written or computerized handoff notes (with feedback) 58, 59 | Junior/senior resident and faculty | ✓ | ✓ | ||||
| Adaptation of handoff tools and forms to local settings using process69 | Junior/senior resident and faculty | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Development of local formative and summative evaluation tools, potentially using existing models41 | Junior/senior resident and faculty | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Development of the local protocol for entrustment decisions46,47 | Junior/senior resident and faculty | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
Developed by a computer-supported cooperative workgroup from the Handovers and Handoffs: Collaborating in Turns symposium in 2010.
In addition, our blueprint incorporates the formal progression from directly to more remotely supervised handoffs. This tradition of residents demonstrating increased responsibility over time dates back to Halsted's pioneering work in residency education,50 was expanded on by Kennedy and colleagues,51–53 and also was emphasized in the 2010 ACGME Common Program Requirements.36 Early in internship, curricula emphasize how to conduct effective basic handoffs. Over the course of residency, trainees learn to perform handoffs in more complex circumstances. Eventually, supervising residents and faculty entrust handoffs to trainees after formal assessments of their competence in the necessary skills.
In this approach, supervisors treat the handoff as an entrustable professional activity (EPA) or a discrete element of essential physician work that a supervisor can delegate or entrust to a resident, who will perform that task independently after the supervisor has determined that the resident has achieved a satisfactory level of competence.54–56 In our blueprint, a new intern handing off a sick patient for the first time warrants more supervision and guidance than a more experienced intern later in the academic year. In the senior years of residency, residents continue to build their handoff skills by collaborating on teams with faculty to tailor strategies and tools to best meet local needs and circumstances and to contribute to improved handoff practices within and across departments.
Because the information that is conveyed in the handoff is an abstract representation of clinical data based on the experience of one care team, a resident's ability to communicate (or to receive and recognize) the salient information about a patient also depends on his or her clinical experience. Thus, handoffs are complex clinical and communication tasks, and it is critical that residents acquire the specific skills to receive handoffs as well as to provide them. These skills include how to manage handoff dialogue through active listening, asking relevant questions, and collaborating to generate the optimal information exchange and shared understanding to guide care. The handoff communication skills of residents, particularly junior trainees, may also improve with greater supervision and coaching by more senior residents or faculty.13,18,22
Our blueprint does not include specific tools for formative or summative assessment of residents’ handoff skills, but we propose that such resources be developed or adapted locally, possibly from assessment tools found in the literature, such as the checklist for the Observed Simulated Hand-off Experience (OSHE). Our blueprint also includes competencies for senior residents, which rely on developing local assessment tools that precede a supervisor's decision to entrust a junior resident with the handoff. In addition, our blueprint contains a series of handoff-related quality improvement activities for senior residents and faculty, including interviewing outgoing and oncoming teams23,57,58 and auditing written and electronic handoff information.59
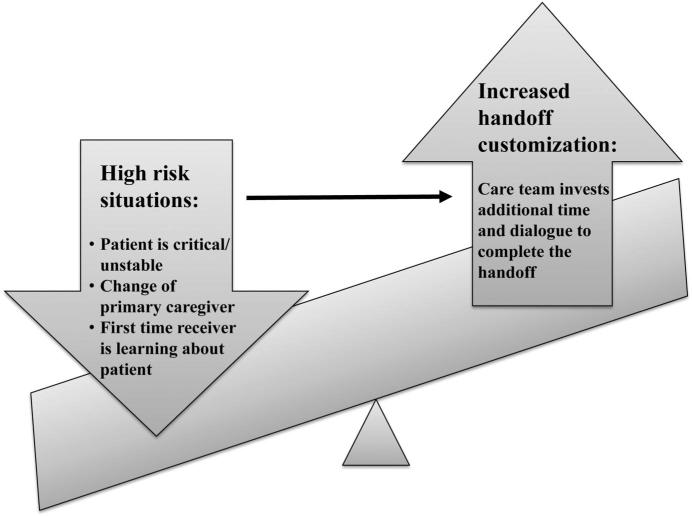
Another way for educators to customize the teaching and supervision of handoffs is to stratify them according both to the importance of the handoff and to the potential for communication breakdown (see Figure 1). Diagnostic complexity, patient vulnerability, uncertain disease trajectory, or incomplete medical history or test results, for example, are patient-related factors that increase the importance of the handoff in the overall care of a patient. Conversely, the handoff of a straightforward, stable, or well-characterized patient is less likely to lead to an adverse event even if the handoff is conducted ineffectively.
Figure 1.
Risk-stratifying handoffs. The emphasis that a resident places on the handoff should be appropriate to the situation. In high-risk situations (i.e., the patient requires an escalation of care), the care team invests additional time and dialogue to complete the handoff. Conversely, for a straightforward, stable, or well-characterized patient, a concise and efficient handoff is more appropriate than a lengthy report.
Risk factors that increase the probability of a communication breakdown occurring include the degree of familiarity of the sender or receiver with the patient, the type of handoff, and the level of experience of the clinicians involved. An illustrative example of the effects of these risk factors is the intern in July for whom the potential for a communication breakdown during the handoff increases substantially. Therefore, new residents handing off complex, sick patients should be supervised until they have learned to perform sign-out effectively and the consequent risk of missed information decreases.
There also may be benefits to continuing some level of supervision or senior resident presence during handoffs even after the task has been approved as an EPA for the resident. From the perspective of enhancing patient safety, recommendations to extend supervision have been adapted from high-reliability organizations that have focused on how redundancy (another set of eyes and ears) can reduce handoff errors and how feedback to the presenter contributes to enhanced accuracy and learning.17,33,60 This approach is congruent with the concept of resilience or a high-reliability organization's preoccupation with failure, which increases the ability of the system to detect the deterioration of patients, as well as information transfer errors and omissions.17
For individual residency programs, implementing our blueprint entails selecting the appropriate tools and approaches, initially educating all residents and faculty to promote a common understanding of the educational intervention and tools, and the subsequent work by senior residents and faculty to adapt the tools and approaches to the programs’ particular handoff situations and areas of risk. Specialists also conduct special circumstance handoffs, which have different needs for information exchange and dialogue. Examples of special circumstance handoffs include the anesthesiology team handing off a complex, postoperative patient to the surgical intensive care unit team, and the two handoffs to transfer a routine surgical patient from the operating room to the postanesthesia care unit and, subsequently, to the inpatient floor. Thus, rather than adopting a one-size-fits-all approach, educators seeking to improve residents’ handoff skills will benefit from a model of teaching like our blueprint that provides the essential information in a way that can be customized to local needs and includes supervised progressive experiences and self-correcting feedback opportunities to accelerate and enhance resident learning and the application of these tools.61 Used in this way, our blueprint is also relevant and adaptable to efforts to improve the handoff in nursing and other health professions.
Moving Forward
To ensure regulatory compliance and improve patient safety, educational strategies to teach handoff skills must be part of any effort to improve handoffs. In this article, we present a comprehensive, longitudinal blueprint that can be adapted to the time and financial resources available to residency programs and also tailored to meet specialty or local-level circumstances and needs. Our innovative approach62 to teaching handoff skills can be applied by all educators and program directors who face the common problem of how to teach and assess residents. By design, our blueprint focuses on delineating solutions, highlighting specific competencies and evidence where appropriate for the use of a specific solution. It also provides a useful starting point for future research into improving patient handoffs.
The interventions that we included in our blueprint either have undergone initial testing and validation or, like the OSHE, are based on earlier tools, such as the objective structured clinical examination, which have been extensively validated.63,64 Still, larger-scale tests are needed to study the effectiveness of these resources in enhancing residents’ competence in handoff skills. Use of our blueprint by a number of groups has the potential to produce enough data to allow full validation of the included tools and to generate a robust database of methods to teach handoff skills that groups can customize for different specialties and local circumstances. Whether efforts to teach and support handoffs will translate into improved patient outcomes remains to be seen. Research to assess the impact of improved handoffs on patient outcomes is difficult to conduct because multiple factors and potential confounds exist in the complex clinical environment of the AHC. However, a starting point to system-wide handoff improvement is a shared vision and approach to augmenting the skills of residents who are engaged in more handoffs than ever with the advent of duty hours restrictions.
Acknowledgments
The authors thank Nikhil Sharma, Michael Cohen, and Brian Hilligoss, from the School of Information at the University of Michigan, and Emily Patterson, then from Health Information Management and Systems at the Ohio State University School of Allied Medical Professions, for organizing the symposium Handovers & Handoffs: Collaborating in Turns; the symposium participants, as well as the ACGME, without whom this project would not have been possible; and Dr. Erik Van Eaton, Dr. Karen Horvath, and the University of Washington School of Medicine Department of Surgery, for their innovations in computerized rounding and sign-out.
Funding/Support: Dr. Horwitz and Dr. Arora receive funding from the Agency for Healthcare Research and Quality (R03HS018278-01). Dr. Horwitz also receives support from the National Institute on Aging (K08 AG038336), the American Federation for Aging Research through the Paul B. Beeson Career Development Award Program, and the Claude D. Pepper Older Americans Independence Center at Yale University School of Medicine (#P30AG21342 NIH/NIA). These organizations had no role in the study design; in the collection, analysis, and interpretation of data; in the writing of the final article; or in the decision to submit the article for publication.
Footnotes
Other disclosures: Dr. Philibert is an employee of the ACGME, and Dr. Arora has received funding from the ACGME, which established the standards and restrictions discussed in this article. Dr. Arora also chaired the Society of Hospital Medicine's handoff task force.
Ethical approval: Not applicable.
Disclaimer: The opinions expressed in this article are solely those of the authors and do not necessarily represent the official views of the National Institute on Aging, the National Institutes of Health, or the American Federation for Aging Research.
References
- 1.Philibert I, Leach DC. Re-framing continuity of care for this century. Qual Saf Health Care. 2005;14:394–396. doi: 10.1136/qshc.2005.016170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nakayama DK, Thompson WM, Wynne JL, Dalton ML, Bozeman AT, Innes BJ. The effect of ACGME duty hour restrictions on operative continuity of care. Am Surg. 2009;75:1234–1237. [PubMed] [Google Scholar]
- 3.The Joint Commission . Accreditation Standards. The Joint Commission; Oakbrook, Ill: 2010. [Google Scholar]
- 4.Nasca TJ, Day SH, Amis ES, Jr, ACGME Duty Hour Task Force The new recommendations on duty hours from the ACGME Task Force. N Engl J Med. 2010;363:e3. doi: 10.1056/NEJMsb1005800. [DOI] [PubMed] [Google Scholar]
- 5.Van Eaton EG, Horvath KD, Lober WB, Rossini AJ, Pellegrini CA. A randomized, controlled trial evaluating the impact of a computerized rounding and sign-out system on continuity of care and resident work hours. J Am Coll Surg. 2005;200:538–545. doi: 10.1016/j.jamcollsurg.2004.11.009. [DOI] [PubMed] [Google Scholar]
- 6.Scandurra I, Hägglund M, Koch S. From user needs to system specifications: Multi-disciplinary thematic seminars as a collaborative design method for development of health information systems. J Biomed Inform. 2008;41:557–569. doi: 10.1016/j.jbi.2008.01.012. [DOI] [PubMed] [Google Scholar]
- 7.Timpka T, Nyce JM. Dilemmas at a primary health care center: A baseline study for computer-supported cooperative health care work. Methods Inf Med. 1992;31:204–209. [PubMed] [Google Scholar]
- 8.Committee on Quality of Health Care in America, Institute of Medicine . Crossing the Quality Chasm: A New Health System for the 21st Century. National Academy Press; Washington, DC: 2001. [Google Scholar]
- 9.Leatt P, Shea C, Studer M, Wang V. IT solutions for patient safety—Best practices for successful implementation in healthcare. Healthc Q. 2006;9:94. [PubMed] [Google Scholar]
- 10.Horwitz LI, Krumholz HM, Green ML, Huot SJ. Transfers of patient care between house staff on internal medicine wards: A national survey. Arch Intern Med. 2006;166:1173–1177. doi: 10.1001/archinte.166.11.1173. [DOI] [PubMed] [Google Scholar]
- 11.Cohen MD, Hilligoss PB. The published literature on handoffs in hospitals: Deficiencies identified in an extensive review. Qual Saf Health Care. 2010;19:493–497. doi: 10.1136/qshc.2009.033480. [DOI] [PubMed] [Google Scholar]
- 12.Philibert I. Use of strategies from high-reliability organisations to the patient hand-off by resident physicians: Practical implications. Qual Saf Health Care. 2009;18:261–266. doi: 10.1136/qshc.2008.031609. [DOI] [PubMed] [Google Scholar]
- 13.Gibson SC, Ham JJ, Apker J, Mallak LA, Johnson NA. Communication, communication, communication: The art of the handoff. Ann Emerg Med. 2010;55:181–183. doi: 10.1016/j.annemergmed.2009.10.009. [DOI] [PubMed] [Google Scholar]
- 14.Borowitz SM, Waggoner-Fountain LA, Bass EJ, Sledd RM. Adequacy of information transferred at resident sign-out (in-hospital handover of care): A prospective survey. Qual Saf Health Care. 2008;17:6–10. doi: 10.1136/qshc.2006.019273. [DOI] [PubMed] [Google Scholar]
- 15.Paine LA, Millman A. Sealing the cracks, not falling through: Using handoffs to improve patient care. Front Health Serv Manage. 2009;25:33–38. [PubMed] [Google Scholar]
- 16.Parker J, Coiera E. Improving clinical communication: A view from psychology. J Am Med Inform Assoc. 2000;7:453–461. doi: 10.1136/jamia.2000.0070453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Patterson ES, Roth EM, Woods DD, Chow R, Gomes JO. Handoff strategies in settings with high consequences for failure: Lessons for health care operations. Int J Qual Health Care. 2004;16:125–132. doi: 10.1093/intqhc/mzh026. [DOI] [PubMed] [Google Scholar]
- 18.DeVito JA. The Interpersonal Communication Book. 10th ed. Pearson Education, Inc.; Boston, Mass: 2004. [Google Scholar]
- 19.Arora V, Johnson J, Lovinger D, Humphrey HJ, Meltzer DO. Communication failures in patient sign-out and suggestions for improvement: A critical incident analysis. Qual Saf Health Care. 2005;14:401–407. doi: 10.1136/qshc.2005.015107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gandhi TK. Fumbled handoffs: One dropped ball after another. Ann Intern Med. 2005;142:352–358. doi: 10.7326/0003-4819-142-5-200503010-00010. [DOI] [PubMed] [Google Scholar]
- 21.Kitch BT, Cooper JB, Zapol WM, et al. Handoffs causing patient harm: A survey of medical and surgical house staff. Jt Comm J Qual Patient Saf. 2008;34:563–570. doi: 10.1016/s1553-7250(08)34071-9. [DOI] [PubMed] [Google Scholar]
- 22.Horwitz LI, Moin T, Krumholz HM, Wang L, Bradley EH. What are covering doctors told about their patients? Analysis of sign-out among internal medicine housestaff. Qual Saf Health Care. 2009;18:248–255. doi: 10.1136/qshc.2008.028654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Horwitz LI, Moin T, Krumholz HM, Wang L, Bradley EH. Consequences of inadequate sign-out for patient care. Arch Intern Med. 2008;168:1755–1760. doi: 10.1001/archinte.168.16.1755. [DOI] [PubMed] [Google Scholar]
- 24.Petersen L, Brennan T, O'Neil A, et al. Does housestaff discontinuity of care increase the risk for preventable adverse events? Ann Intern Med. 1994;121:866–872. doi: 10.7326/0003-4819-121-11-199412010-00008. [DOI] [PubMed] [Google Scholar]
- 25.Tabrizian P, Rajhbeharrysingh U, Khaitov S, Divino CM. Persistent noncompliance with the work-hour regulation. Arch Surg. 2011;146:175–178. doi: 10.1001/archsurg.2010.337. [DOI] [PubMed] [Google Scholar]
- 26.Antiel RM, Thompson SM, Hafferty FW, et al. Duty hour recommendations and implications for meeting the ACGME core competencies: Views of residency directors. Mayo Clin Proc. 2011;86:185–191. doi: 10.4065/mcp.2010.0635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sutcliffe KM, Lewton E, Rosenthal MM. Communication failures: An insidious contributor to medical mishaps. Acad Med. 2004;79:186–194. doi: 10.1097/00001888-200402000-00019. [DOI] [PubMed] [Google Scholar]
- 28.Arora V, Dunphy C, Chang VY, Ahmad F, Humphrey HJ, Meltzer D. The effects of on-duty napping on intern sleep time and fatigue. Ann Intern Med. 2006;144:792–798. doi: 10.7326/0003-4819-144-11-200606060-00005. [DOI] [PubMed] [Google Scholar]
- 29.Helms AS, Perez TE, Baltz J, et al. Use of an appreciative inquiry approach to improve resident sign-out in an era of multiple shift changes. J Gen Intern Med. doi: 10.1007/s11606-011-1885-4. [published online ahead of print October 14, 2011] doi: 10.1007/s11606-011-1885-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wolf Z. Learning the professional jargon of nursing during change of shift report. Holist Nurs Pract. 1989;4:78–83. doi: 10.1097/00004650-198911000-00014. [DOI] [PubMed] [Google Scholar]
- 31.Strange F. Handover: An ethnographic study of ritual in nursing practice. Intensive Crit Care Nurs. 1996;12:106–112. doi: 10.1016/s0964-3397(96)81074-3. [DOI] [PubMed] [Google Scholar]
- 32.Reiley P, Stengrevics S. Change of shift report: Put it in writing! Nurs Manag (Harrow) 1989;20:54–56. [PubMed] [Google Scholar]
- 33.Patterson ES, Woods DD. Shift changes, updates, and the on-call architecture in space shuttle mission control. Comput Support Coop Work. 2001;10:317–346. doi: 10.1023/a:1012705926828. [DOI] [PubMed] [Google Scholar]
- 34.Patterson ES. Structuring flexibility: The potential good, bad and ugly in standardisation of handovers. Qual Saf Health Care. 2008;17:4–5. doi: 10.1136/qshc.2007.022772. [DOI] [PubMed] [Google Scholar]
- 35.Stein DM, Stetson PD. Commentary: Time to sign off on sign-out. Acad Med. 2011;86:804–806. doi: 10.1097/ACM.0b013e31821d8409. [DOI] [PubMed] [Google Scholar]
- 36.Accreditation Council for Graduate Medical Education [December 6, 2011];Common Program Requirements. www.acgme.org/acWebsite/dutyHours/dh_dutyhoursCommonPR07012007.pdf.
- 37.Arora V, Farnan J, Paro J, Vidyarthi A, Johnson J. Teaching video: “Handoffs: A typical day on the wards. ”. [December 6, 2011];MedEdPORTAL. 2011 Feb 17; http://services.aamc.org/30/mededportal/servlet/s/segment/mededportal/?subid=8331.
- 38.Horwitz LI, Moin T, Green ML. Development and implementation of an oral sign-out skills curriculum. J Gen Intern Med. 2007;22:1470–1474. doi: 10.1007/s11606-007-0331-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chu ES, Reid M, Schulz T, et al. A structured handoff program for interns. Acad Med. 2009;84:347–352. doi: 10.1097/ACM.0b013e3181970829. [DOI] [PubMed] [Google Scholar]
- 40.Telem DA, Buch KE, Ellis S, Coakley B, Divino CM. Integration of a formalized handoff system into the surgical curriculum: Resident perspectives and early results. Arch Surg. 2011;146:89–93. doi: 10.1001/archsurg.2010.294. [DOI] [PubMed] [Google Scholar]
- 41.DeVoge JM, Bass EJ, Atia M, Bond M, Waggoner-Fountain L, Borowitz SM. The development of a Web-based resident sign-out training program.. Paper presented at: 2009 IEEE International Conference on Systems, Man, and Cybernetics; San Antonio, Tex. October 11–14, 2009; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Porteous JM, Stewart-Wynne EG, Connolly M, Crommelin PF. iSoBAR—A concept and handover checklist: The National Clinical Handover Initiative. Med J Aust. 2009;190(11 suppl):S152–S156. doi: 10.5694/j.1326-5377.2009.tb02625.x. [DOI] [PubMed] [Google Scholar]
- 43.Amato-Vealey EJ, Barba MP, Vealey RJ. Hand-off communication: A requisite for perioperative patient safety. AORN J. 2008;88:763–770. doi: 10.1016/j.aorn.2008.07.022. [DOI] [PubMed] [Google Scholar]
- 44.DeVoge JM, Bass EJ, Sledd R, Borowitz S, Waggoner-Fountain L. Collaborating with physicians to redesign a sign-out tool: An iterative, multifaceted approach with users—even busy ones—can yield a satisfying and efficient product. Ergon Des. 2009:20–28. doi: 10.1518/106480409X415170. Winter. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Petersen LA, Orav EJ, Teich JM, O'Neil AC, Brennan TA. Using a computerized sign-out program to improve continuity of inpatient care and prevent adverse events. Jt Comm J Qual Improv. 1998;24:77–87. doi: 10.1016/s1070-3241(16)30363-7. [DOI] [PubMed] [Google Scholar]
- 46.Farnan JM, Paro JA, Rodriguez RM, et al. Hand-off education and evaluation: Piloting the observed simulated hand-off experience (OSHE). J Gen Intern Med. 2010;25:129–134. doi: 10.1007/s11606-009-1170-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Filichia L, Halan S, Blackwelder E, et al. Description of Web-enhanced virtual character simulation system to standardize patient hand-offs. J Surg Res. 2011;166:176–181. doi: 10.1016/j.jss.2010.04.052. [DOI] [PubMed] [Google Scholar]
- 48.Amis S, Philibert I, editors. The ACGME 2010 Duty Hour Standards: Enhancing Quality of Care, Supervision and Resident Professional Development. Vol. 2011. Accreditation Council for Graduate Medical Education; Chicago, Ill: [February 2, 2012]. ACGME Task Force on Quality Care and Professionalism. New Supervision Standards: Discussion and Justification. pp. 57–60. http://www.acgme-2010standards.org/pdf/monographs/jgme-11-00-39-45.pdf. [Google Scholar]
- 49.Swing SR, Clyman SG, Holmboe ES, Williams RG. Advancing resident assessment in graduate medical education. J Grad Med Educ. 2009;1:278–286. doi: 10.4300/JGME-D-09-00010.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Harvey AM. The influence of William Stewart Halsted's concepts of surgical training. Johns Hopkins Med J. 1981;148:215–236. [PubMed] [Google Scholar]
- 51.Kennedy TJ, Lingard L, Baker GR, Kitchen L, Regehr G. Clinical oversight: Conceptualizing the relationship between supervision and safety. J Gen Intern Med. 2007;22:1080–1085. doi: 10.1007/s11606-007-0179-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kennedy TJ, Regehr G, Baker GR, Lingard L. Point-of-care assessment of medical trainee competence for independent clinical work. Acad Med. 2008;83(10 suppl):S89–S92. doi: 10.1097/ACM.0b013e318183c8b7. [DOI] [PubMed] [Google Scholar]
- 53.Kennedy TJ. Towards a tighter link between supervision and trainee ability. Med Educ. 2009;43:1126–1128. doi: 10.1111/j.1365-2923.2009.03543.x. [DOI] [PubMed] [Google Scholar]
- 54.ten Cate O, Snell L, Carraccio C. Medical competence: The interplay between individual ability and the health care environment. Med Teach. 2010;32:669–675. doi: 10.3109/0142159X.2010.500897. [DOI] [PubMed] [Google Scholar]
- 55.ten Cate O, Scheele F. Competency-based postgraduate training: Can we bridge the gap between theory and clinical practice? Acad Med. 2007;82:542–547. doi: 10.1097/ACM.0b013e31805559c7. [DOI] [PubMed] [Google Scholar]
- 56.Sterkenburg A, Barach P, Kalkman C, Gielen M, ten Cate O. When do supervising physicians decide to entrust residents with unsupervised tasks? Acad Med. 2010;85:1408–1417. doi: 10.1097/ACM.0b013e3181eab0ec. [DOI] [PubMed] [Google Scholar]
- 57.Pickering BW, Hurley K, Marsh B. Identification of patient information corruption in the intensive care unit: Using a scoring tool to direct quality improvements in handover. Crit Care Med. 2009;37:2905–2912. doi: 10.1097/CCM.0b013e3181a96267. [DOI] [PubMed] [Google Scholar]
- 58.Bump GM, Jovin F, Destafano L, et al. Resident sign-out and patient hand-offs: Opportunities for improvement. Teach Learn Med. 2011;23:105–111. doi: 10.1080/10401334.2011.561190. [DOI] [PubMed] [Google Scholar]
- 59.Flanagan ME, Patterson ES, Frankel RM, Doebbeling BN. Evaluation of a physician informatics tool to improve patient handoffs. J Am Med Inform Assoc. 2009;16:509–515. doi: 10.1197/jamia.M2892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Patterson ES, Wears RL. Patient handoffs: Standardized and reliable measurement tools remain elusive. Jt Comm J Qual Patient Saf. 2010;36:52–61. doi: 10.1016/s1553-7250(10)36011-9. [DOI] [PubMed] [Google Scholar]
- 61.Johnson JK, Arora VM. Improving clinical handovers: Creating local solutions for a global problem. Qual Saf Health Care. 2009;18:244–245. doi: 10.1136/qshc.2009.032946. [DOI] [PubMed] [Google Scholar]
- 62.Kanter SL. Toward better descriptions of innovations. Acad Med. 2008;83:703–704. doi: 10.1097/ACM.0b013e3181838a2c. [DOI] [PubMed] [Google Scholar]
- 63.Harden RM, Stevenson M, Downie WW, Wilson GM. Assessment of clinical competence using objective structured examination. BMJ. 1975;1:447–451. doi: 10.1136/bmj.1.5955.447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Newble D. Techniques for measuring clinical competence: Objective structured clinical examination. Med Educ. 2004;38:199–203. doi: 10.1111/j.1365-2923.2004.01755.x. [DOI] [PubMed] [Google Scholar]
- 65.Gakhar B, Spencer AL. Using direct observation, formal evaluation, and an interactive curriculum to improve the sign-out practices of internal medicine interns. Acad Med. 2010;85:1182–1188. doi: 10.1097/ACM.0b013e3181da8370. [DOI] [PubMed] [Google Scholar]
- 66.Sanfey H, Stiles B, Hedrick T, Sawyer RG. Morning report: Combining education with patient handover. Surgeon. 2008;6:94–100. doi: 10.1016/s1479-666x(08)80072-8. [DOI] [PubMed] [Google Scholar]
- 67.Vorley G. Mini Guide to Root Cause Analysis. Quality Management and Training; Guildford, UK: 2008. [December 6, 2011]. http://www.root-cause-analysis.co.uk/images/Green%20RCA%20mini%20guide%20v5%20small.pdf. [Google Scholar]
- 68.Chang VY, Arora VM, Lev-Ari S, D'Arcy M, Keysar B. Interns overestimate the effectiveness of their hand-off communication. Pediatrics. 2010;125:491–496. doi: 10.1542/peds.2009-0351. [DOI] [PubMed] [Google Scholar]
- 69.Arora V, Johnson J. A model for building a standardized hand-off protocol. Jt Comm J Qual Patient Saf. 2006;32:646–655. doi: 10.1016/s1553-7250(06)32084-3. [DOI] [PubMed] [Google Scholar]