Abstract
We report a case of hemoptysis occurring after subclavian vein puncture for pacemaker implantation. Hemoptysis related to injury of lung parenchyma is a rare complication of subclavian vein access and is usually self limited, but can affect prognosis in critically ill patients. Venogram-guided or even better wire-guided venous puncture allow safe access to the subclavian vein in difficult cases. A review of the pertinent literature is also presented.
Keywords: hemoptysis, guidewire, subclavian
Introduction
Subclavian vein puncture is a relatively fast and safe technique to access the right heart for placement of pacemaker leads, it has been described since the beginning of the era of endocavitary pacemaker leads placement1 and has often been the preferred access technique for many operators.2 Complications like alveolar hemorrhage, hemothorax and hemoptysis are rare (<0.1%) in this setting,3 and even though the course of these complications is usually benign and self limited, there may be a severely adverse outcome in critically ill patients.4 We present a case of hemoptysis occurring after difficult subclavian vein puncture, also we recommend the use of wire-guided puncture in cases of difficult subclavian vein access.
Case Presentation
An 80-year-old patient presented with repetitive syncope due to paroxysmal second degree mobitz 2 AV block, the patient had no relevant past medical history. The patient had serum hemoglobin at 14.5 g/dL, normal platelets and red blood cells count, also he had normal prothrombin and partial thromboplastin time, the patient was not taking any anticoagulant or antiplatelet therapy.
A decision to implant a VDD pacemaker was taken, we used the left subclavian vein puncture which is our preferred technique for venous access. The operator had almost 10 years experience in cardiac pacing with an annual workflow of around 100 devices. He used the clavicle and the sternal notch as landmarks and with intermittent fluoroscopic guidance, the needle gauge was 18 (inner diameter 0.838 mm, outer diameter 1.270 mm, length 7 cm), the tear-away introducer sheath had 9 F (Intradyn™) and the guidewire had 46 cm length with a J shaped soft tip. Venous access was difficult, multiple punctures trajectories and sites were attempted to finally have access to the subclavian vein, there was no evidence of arterial puncture, also there was no needle-air reflux suggesting parenchymal puncture.
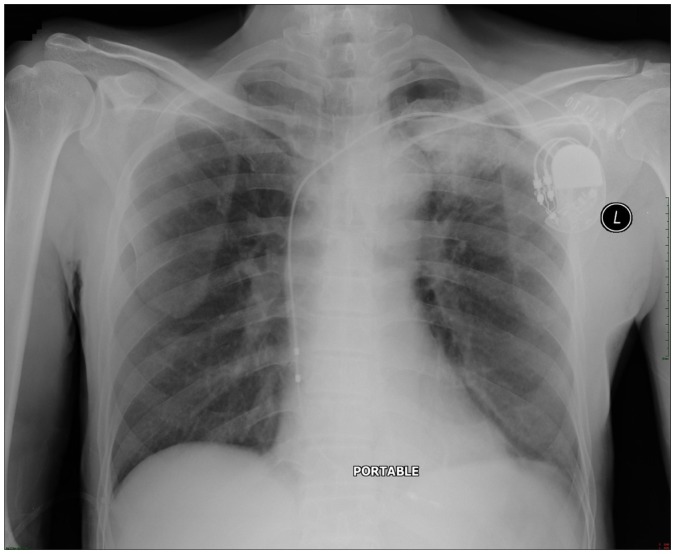
The patient was mildly sedated and he had no complaints during the procedure, he had normal oximetry, peri-operative electrical parameters were adequate, the pacing system consisted of VDD generator (Verity, Saint Jude Medical) connected to a VDD lead (tined tip, same manufacturer). The procedure ended without remarkable incident. Almost one hour after the procedure, the patient started to have hemoptysis, it was of minimal amount (estimated to approximately 50 cc/24 hours), oxygen saturation stayed above 95% and there was no chest pain. Post-operative chest X rays (Fig. 1) showed left upper lobe infiltrates suggesting alveolar hemorrhage. Pulmonary consultation suggested only supportive measures (oxygen supply, regular check of vital signs and hematocrit ) and no bronchoscopy was suggested. Hemoptysis persisted for 48 hours and decreased gradually to stop after 72 hours, the pre-discharge chest X rays (Fig. 2) realized 3 days after the procedure showed a nearly complete disappearance of the infiltrates.
Figure 1.
Post operative chest X ray showing left upper lobe alveolar hemorrhage.
Figure 2.
Nearly total clearance of the infiltrates 72 hours after the procedure.
Discussion
Hemoptysis is a rare complication of subclavian vein puncture in the setting of pacemaker implantation3,4 and to the best of our knowledge, only few cases of hemoptysis have been reported in the literature in this setting.5 Even though the course is usually benign, it can be critical in special conditions like coagulation disturbances and chronic lung diseases. The course is usually short and self limited when the mechanism is punctual injury of lung parenchyma, it is more critical when it is related to subclavian artery laceration along with parenchymal injury with potential formation of a track or fistula that maintain blood leak and hemoptysis.5
Subclavian vein access can be challenging especially in patients with difficult anatomy, this could be Hemoptysis after pacemaker implantation due to atypical subclavian vessels trajectory, atypical clavicular bone anatomy and/or atypical structure of the lungs (ie, emphysema); Also, in hypotensive or hypoxemic patients, arterial puncture may be mistaken for venous puncture. Accordingly, we estimate that puncture-related complications are higher when dealing with difficult anatomy and the operator experience plays an important role in these settings. When subclavian venous access is difficult and when the cephalic vein is not accessible (ie, rudimentary), contrast venography6 may facilitate axillary or subclavian vein puncture, but this venogram-guided method gives only transient guiding landmark and can be limited in case of renal failure or intolerance to the contrast product.
Accordingly, we suggest the use of wire-guided puncture for difficult cases of subclavian puncture; after introducing a guidewire with adapted physical properties through a superficial brachial vein (basilic or cephalic vein), the wire is pushed into the subclavian vein, and so subclavian puncture under fluoroscopy is made easier and safer. Even though this technique has been previously described for venous cutdown,7 we hypothesize that it is rarely used for subclavian venous puncture; therefore we suggest the use of this technique in difficult cases and in high risk patients like very thin or very obese patients, elderly patients, patients with difficult anatomy, patients with severe lung disease, patients with coagulation disorders).
Conclusion
Alveolar hemorrhage is a rare complication of subclavian vein puncture, and the course is usually benign but can be critical in patients with chronic lung disease or with coagulation disorders. If cephalic vein access is not possible and in cases when subclavian vein access is difficult, we suggest the use of wire-guided venous access as a safe and efficient method to implement especially in patients at high risk of puncture related complications.
Footnotes
Author Contributions
Conceived and designed the experiments: AK. Analysed the data: AK, NN, PE. Wrote the first draft of the manuscript: AK, NN, PE. Contributed to the writing of the manuscript: AK, NN, PE. Agree with manuscript results and conclusions: AK, NN, PE. Jointly developed the structure and arguments for the paper: AK, NN, PE. Made critical revisions and approved final version: AK, NN, PE. All authors reviewed and approved of the final manuscript. AK, NN, PE.
Competing Interests
Author(s) disclose no potential conflicts of interest.
Disclosures and Ethics
As a requirement of publication author(s) have provided to the publisher signed confirmation of compliance with legal and ethical obligations including but not limited to the following: authorship and contributorship, conflicts of interest, privacy and confidentiality and (where applicable) protection of human and animal research subjects. The authors have read and confirmed their agreement with the ICMJE authorship and conflict of interest criteria. The authors have also confirmed that this article is unique and not under consideration or published in any other publication, and that they have permission from rights holders to reproduce any copyrighted material. Any disclosures are made in this section. The external blind peer reviewers report no conflicts of interest.
Funding
Author(s) disclose no funding sources.
References
- 1.Solomon N, Escher DJ. A rapid method for insertion of the pacemaker catheter electrode. Am Heart J. 1963;66:717–8. doi: 10.1016/0002-8703(63)90330-2. [DOI] [PubMed] [Google Scholar]
- 2.McNeill GP, Taylor NC. Use of subclavian vein for permanent cardiac pacing. Br Heart J. 1978;40:114–6. doi: 10.1136/hrt.40.2.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kirk AJ, Turner MA. Surgical aspects of permanent cardiac pacemakers. Life Support Syst. 1987;5:223–31. [PubMed] [Google Scholar]
- 4.García-Anguiano Duque F, Marchena Gómez J, Servent Pedescoll R. Hemoptysis, a rare complication of punction-catheterization of the subclavian vein. Rev Clin Esp. 1994;194:202. [PubMed] [Google Scholar]
- 5.Goldberg A, Inna Rosenfeld I, Marmor A. Hemoptysis—a rare complication of pacemaker implantation. Indian Pacing Electrophysiol J. 2008;8:75–6. [PMC free article] [PubMed] [Google Scholar]
- 6.Dora SK, Kumar VK, Bhat A, Tharakan JA. Venogram-guided extrathoracic subclavian vein puncture. Indian Heart J. 2003;55:637–40. [PubMed] [Google Scholar]
- 7.Shockley LW, Butzier DJ. A modified wire-guided technique for venous cut-down access. Ann Emerg Med. 1990;19:393–5. doi: 10.1016/s0196-0644(05)82344-3. [DOI] [PubMed] [Google Scholar]