Abstract
Candida infection of gastrointestinal tract is frequent in immunocompromised patients and rare in an otherwise healthy person in whom no permissive factor is present. Herein is a case report on 25-year-old woman, 2 months postpartum, with fungal gastric ulcer with invasion leading to fungemia. She developed fever and anemia. Gastric biopsy and blood culture both showed growth of Candida albicans. The patient responded well to parenteral amphotericin B. This supports the hypothesis of invasion of Candida from gastric ulcer into blood.
Keywords: Extraesophageal candidiasis, fungal gastric ulcer, gastric candidiasis, gastric ulcer
Candida infection of gastrointestinal (GI) tract is frequent in an immunocompromised patient and rare in an otherwise healthy person. In the GI tract, it frequently involves the esophagus and rarely involves the stomach and small bowel.[1–3] There are only few reports of Candida involving stomach and small bowel.[4] Candida infection of the stomach can occur in persons who ingest corrosive chemicals, such as concentrated sulfuric acid and thiocyanates.[5] Esophageal candidiasis invariably appears as plaque on endoscopy.[6,7] Whereas in stomach, Candida infection is associated with gastric ulcer that tends to be larger or may appear as a mass.[3,5,8]
Our case is unique as this giant fungal gastric ulcer occurred in an immunocompetent female and involved the stomach rather than the esophagus.
CASE REPORT
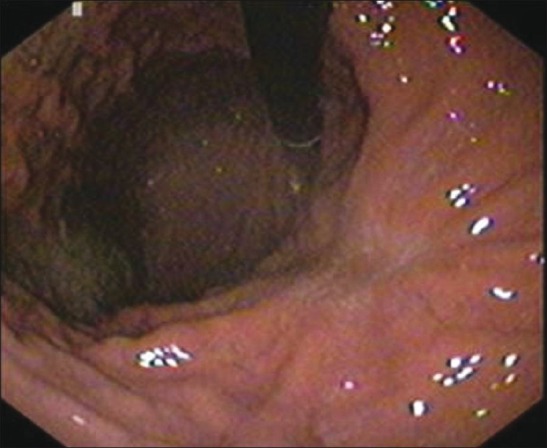
A 25-year-old woman, nondiabetic, 2 months postpartum presented in December 2009 with upper abdominal pain of 2 months, dry cough and fever of 2 weeks duration. She lost 8 kg weight in the last 2 months. There was no history of obvious GI bleed, prolonged acid suppressant use, non-steroidal anti-inflammatory drugs usage, alcohol intake or corrosive intake in the past. On examination the patient had only tachycardia. Investigations revealed hemoglobin (Hb) 76 g/L (microcytic hypochromic), total leukocyte count (TLC) 14.9 × 109/L (polymorphonuclear leukocytes 40%, lymphocytes 20%, eosinophils 36%, monocytes 4%), platelets 340 × 109/L and prothrombin time 12.8 s (control 10.9 s). Liver function tests showed serum bilirubin 0.35 mg/ dL, alanine and aspartate aminotransferase 30 and 47 U/L, respectively, alkaline phosphatase 147 U/L, and total protein and albumin 63 and 33 g/L, respectively. Serum creatinine was 0.8 mg/dL, postprandial blood sugar was 78 mg/dL, potassium was 4.0 mEq/L, and sodium was 136 mEq/L. Stool guaiac test for occult blood was positive. Chest radiography and abdominal ultrasonography were normal. Enzyme-linked immunosorbent assay for human immunodeficiency virus was negative. Upper GI endoscopy showed a large oval to circular 10 × 6 cm ulcer with slough at base, smooth and irregular margin in lesser curvature of stomach [Figure 1]. Initially ulcer was considered to be malignant. Contrast-enhanced computed tomography (CT) abdomen revealed mild thickening of stomach wall along the lesser curvature and a few small retroperitoneal lymph nodes. CT thorax showed normal study. Sputum tested for Mycobacterium tuberculosis for 3 consecutive days was negative. Endoscopic biopsy from ulcer showed fibrocollagenous tissue infiltrated with moderate inflammatory infiltrate along with bits of granulation tissue, with no evidence of malignancy. Antral biopsy revealed Helicobacter pylori-associated gastritis. The patient was initially treated with parenteral antibiotics and a combination of omeprazole, amoxicillin, and clarithromycin for 14 days for H. pylori. However, fever did not respond even after 2 weeks of treatment. Repeat endoscopic biopsies were taken from antrum and from the ulcer edge and base. Histology demonstrated granulation tissue, numerous yeast, and pseudohyphal fungal forms on Periodic acid-Schiff stain consistent with Candida albicans [Figure 2], whereas antral biopsy was negative for H. pylori. There was no evidence of malignancy. Blood culture also showed growth of C. albicans. Intravenous amphotericin B was started along with proton pump inhibitor. Fever and cough subsided. Total leucocyte count normalized. Serum electrophoresis showed the following: IgA 208 mg/dL (normal 100–490 mg/dL), IgM 337 mg/dL (normal 50–320 mg/dL), and IgG 2280 mg/dL (normal 800–1700 mg/dL). Intravenous amphotericin was continued for initial 3 weeks followed by oral fluconazole. Repeat endoscopy at 3 weeks showed reduction in size of ulcer. The patient was followedup for the next 1 year in our gastroenterology outpatient department. Endoscopy at 3 months showed complete healing of ulcer and antral biopsy was negative for H. pylori [Figure 3]. The patient was off any form of treatment for the next 9 months and she is now asymptomatic. Repeat endoscopy at 9 months revealed normal study.
Figure 1.

Endoscopy showing large ulcer with slough at base in lesser curvature of stomach
Figure 2.
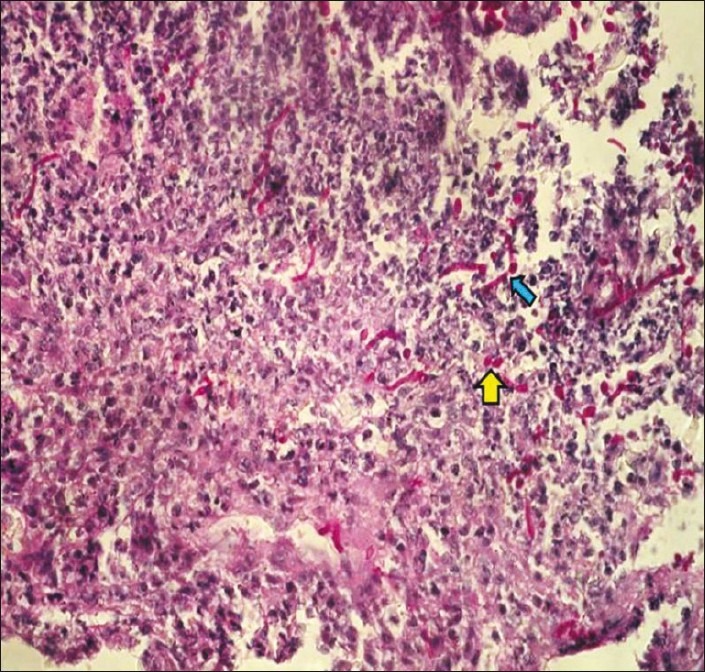
Photomicrograph showing granulation tissue, numerous yeast (yellow arrow), and pseudohyphal fungal forms (block blue arrow) on Periodic acid-Schiff stain consistent with Candida albicans
Figure 3.
Endoscopy showing a healed ulcer
DISCUSSION
There is limited literature on Candida infection of the GI tract outside of the esophagus. Fungal colonization of the stomach may be seen in patients with underlying malignancy and/or who had undergone surgery for peptic ulcer disease or in an immunosuppressed state, but infrequent in immunocompetent individuals.
In evaluation of 2537 outpatients, Knoke and Bernhardt found gastric Candida in only 6; each of those patients had a previous gastric or esophageal resection. On endoscopy, lesion appeared as whitish plaques.[3] However, in a study on the presence of Candida as a stomach opportunistic germ in 149 patients consecutively undergoing gastroscopy, Candida was isolated in 23 patients (15.4%).[9] Appearance of extraesophageal invasive candidiasis with ulceration or mass is even rarer; only single case reports were available.[4,8] However, our patient had large gastric ulcer and ulcer appeared to be malignant, as previously reported by Maryam et al.[5,8] Virtually all described patients with extraesophageal invasive candidiasis were immunosuppressed or had gastric resection.[4,8] In contrast, our patient was not on immunosuppression agents, acid lowering agents or didn’t have underlying gastric resection or immunosuppressive conditions.
In another retrospective study, Loffeld et al showed fungal colonization in 19% of gastric ulcers, however none of them had tissue invasion.[5] The author concluded that fungus in gastric ulcer is probably a secondary phenomenon.[5,10] Gastric ulcer may be colonized with fungus, but invasion is rare.[5] Invasive extraesophageal candidiasis patients may present with abdominal pain, nausea, vomiting, diarrhea and fever.[4,8] Our patient was symptomatic with fever from invasive candidiasis. Invasive Candida infection was evident from positive blood culture for C. albicans and good response to systemic antifungal therapy. No other focus of fever was found. The urine examination was normal and the vaginal swab examination showed no evidence of Candida. She possibly initially had H. pylori-associated gastric ulcer, later colonized by Candida leading to invasive disease. There is scanty literature on combined H. pylori and fungal gastric ulcer, especially in the postpartum period. Our patient was also treated with anti-H. pylori drugs.
In general, peptic ulcer disease during pregnancy is relatively rare. This lower frequency of peptic ulcer in pregnancy may be secondary to lower gastric acid output and increased protective mucus production associated with elevated progesterone levels.[11]
It is still not clear whether fungal colonization or invasion of gastric ulcer has any effect on healing of ulcer. Literature showed mixed results. Wu and colleagues reported that presence of fungus in gastric ulcer did not affect healing.[12] In contrast, another study showed that fungal colonization of gastric ulcers impairs the course of ulcer healing as well as persistence of symptoms.[13] A study on experimental rat demonstrated delay in healing of duodenal ulcer infected with Candida.[14] The authors implicated low expression of vascular endothelial growth factor-A (VEGF-A) and proliferating cell nuclear antigen (PCNA) as underlying pathogenic mechanism.[14]
In this report, we have described an immunocompetent patient in the early postpartum period presenting with extraesophageal candidiasis, as manifested by a large gastric ulcer, in the absence of predisposing factors.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Badarinarayanan G, Gowriskankar R, Muthulakshmi K. Esophageal candidiasis in non-immune suppressed patients in a semi-urban town, southern India. Mycopathologia. 2000;149:1–4. doi: 10.1023/a:1007245919761. [DOI] [PubMed] [Google Scholar]
- 2.Kodsi BE, Wickremesinghe PC, Kozinn PJ, Iswara K, Goldberg PK. Candida esophagitis. a prospective study of 27 cases. Gastroenterology. 1976;71:715–9. [PubMed] [Google Scholar]
- 3.Knoke M, Bernhardt H. Endoscopic aspects of mycosis in the upper digestive tract. Endoscopy. 1980;12:295–8. doi: 10.1055/s-2007-1021763. [DOI] [PubMed] [Google Scholar]
- 4.Joshi SN, Garvin PJ, Sunwoo YC. Candidiasis of the duodenum and jejunum. Gastroenterology. 1981;80:829–33. [PubMed] [Google Scholar]
- 5.Loffeld RJ, Loffeld BC, Arends JW, Flendrig JA, van Spreeuwel JP. Fungal colonization of gastric ulcers. Am J Gastroenterol. 1988;83:730–3. [PubMed] [Google Scholar]
- 6.Scott BB, Jenkins D. Gastro-oesophageal candidiasis. Gut. 1982;23:137–9. doi: 10.1136/gut.23.2.137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wilcox CM, Schwartz DA. Endoscopic-pathologic correlates of Candida esophagitis in acquired immunodeficiency syndrome. Dig Dis Sci. 1996;41:1337–45. doi: 10.1007/BF02088557. [DOI] [PubMed] [Google Scholar]
- 8.Rajablou M, Ganz RA, Batts KP. Candida infection presenting as multiple ulcerated masses. Gastrointest Endosc. 2007;65:164–6. doi: 10.1016/j.gie.2006.05.024. [DOI] [PubMed] [Google Scholar]
- 9.Minoli G, Terruzzi V, Butti GC, Benvenuti C, Rossini T, Rossini A. A prospective study on Candida as a gastric opportunistic germ. Digestion. 1982;25:230–5. doi: 10.1159/000198837. [DOI] [PubMed] [Google Scholar]
- 10.Zwolinska-Wcisto M, Budak A, Bogdal J, Trojanowska D, Stachura J. Fungal colonization of gastric mucosa and its clinical relevance. Med Sci Monit. 2001;7:982–8. [PubMed] [Google Scholar]
- 11.Michaletz-Onody PA. Peptic ulcer disease in pregnancy. Gastroenterol Clin North Am. 1992;21:817–26. [PubMed] [Google Scholar]
- 12.Wu CS, Wu SS, Chen PC. A prospective study of fungal infection of gastric ulcers: Clinical significance and correlation with medical treatment. Gastrointest Endosc. 1995;42:56–8. doi: 10.1016/s0016-5107(95)70244-x. [DOI] [PubMed] [Google Scholar]
- 13.Zwolińska-Wcisło M, Budak A, Bogdał J, Trojanowska D, Stachura J. Effect of fungal colonization of gastric mucosa on the course of gastric ulcers healing. Med Sci Monit. 2001;7:266–75. [PubMed] [Google Scholar]
- 14.Jin L, Yoshida M, Nakamura T, Ishikawa H, Wakabayashi G, Tanabe M, et al. Candida albicans infection delays duodenal ulcer healing in cysteamine-induced duodenal ulcers in rats. Dig Dis Sci. 2008;53:2878–85. doi: 10.1007/s10620-008-0385-9. [DOI] [PubMed] [Google Scholar]


