Abstract
A 2-year-old boy with heterotaxy syndrome with associated polysplenia, ventricular septal defect, and malrotation of gut with volvulus is presented. There was delay in diagnosis due to the unusual plain abdominal radiography findings. At laparotomy, the midgut was also found to be enclosed in a thin transparent cocoon.
KEY WORDS: Abdominal cocoon, heterotaxy, midgut volvulus, polysplenia
INTRODUCTION
Heterotaxy syndrome (HS) or situs ambiguous is defined as the abnormal arrangement of organs and vessels as opposed to the orderly arrangement typical of situs solitus and situs inversus.[1] We present an interesting case of malrotation with volvulus where the diagnosis was delayed because of the association with HS.
CASE REPORT
A 2-year-old boy presented with recurrent episodes of abdominal pain with distension, bilious vomiting and fever for 3 weeks. He weighed 8 kg and had a history of failure to thrive since early infancy. He was a known case of ventricular septal defect (VSD) and was on digoxin. He was dehydrated and lethargic with a pansystolic cardiac murmur. The abdomen was mildly distended with a nontender hepatomegaly. The chest radiograph was normal. The abdominal radiograph showed a prominent gas shadow in the upper half of the abdomen that was initially mistaken for a dilated colonic shadow by the treating physician. [Figure 1]. An ultrasonography suggested dilated large bowel loops that were peristalsing and moderate free fluid. He had a hemoglobin of 14.1 gm% and total leucocyte count of 9800/mm3 with blood urea 89 mg/dL and serum creatinine of 1.3 mg/dL. The 2D-echo revealed situs solitus with levocardia and a small 3 mm peri membranous VSD. The child was kept nil per oral and the fluid and electrolyte imbalance corrected. Due to persistent bilious aspirates, an upper gastrointestinal (GI) contrast study was performed that suggested malrotation with volvulus and situs inversus [Figure 2]. The abdomen was explored through an upper abdominal transverse incision. The stomach and duodenum were in mirror image position with gross distension up to the third part of the duodenum. There was a single 360° counterclockwise torsion at the base of the mesentery. The entire small bowel was healthy but enclosed in a thin transparent sac containing jelly-like material in the left half of the abdomen [Figure 3]. The ascending and transverse colon were posterior to the duodenum. The liver was slightly medially positioned. Multiple splenunculi (five in number) of variable sizes, were seen in the right upper quadrant related to the greater curvature of the stomach [Figure 4]. The bowel was derotated after excising thick Ladd's bands, sac excised and inversion appendectomy performed. The superior mesenteric vessels were seen to lie more toward the posterior aspect of the mesentery after the procedure. The child recovered uneventfully and was discharged on sixth postoperative day. At 2 years follow up, he is asymptomatic and thriving well.
Figure 1.

Prominent gas shadow in the upper half of the abdomen
Figure 2.
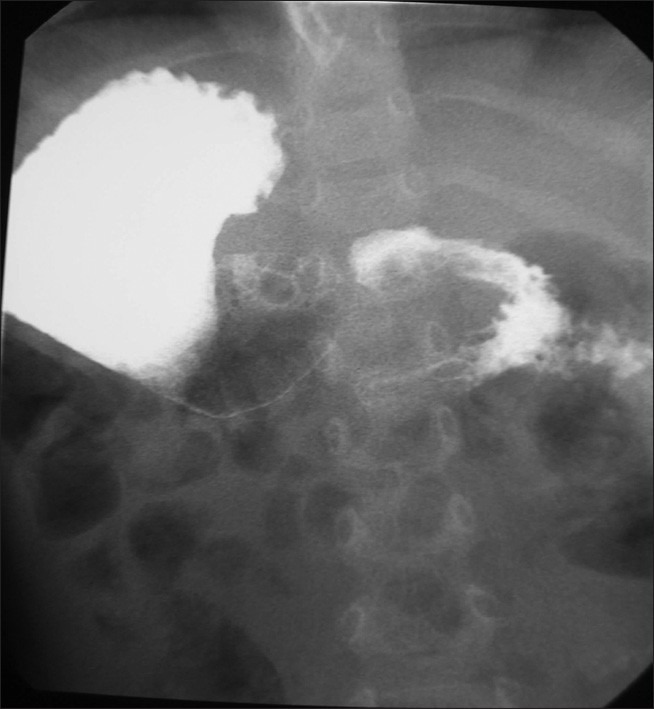
Upper gastrointestinal contrast study showing dilated stomach in the upper-right quadrant of the abdomen, duodenojejunal flexure to the left of the midline and cork screw appearance suggestive of volvulus
Figure 3.
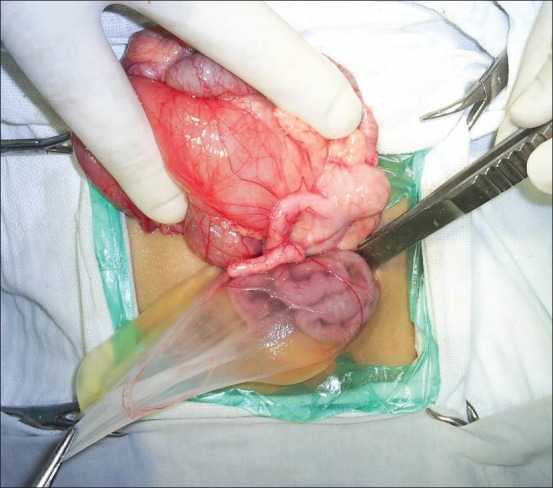
Laparotomy findings of distended duodenum, Ladd's bands and small bowel enclosed in a transparent cocoon
Figure 4.
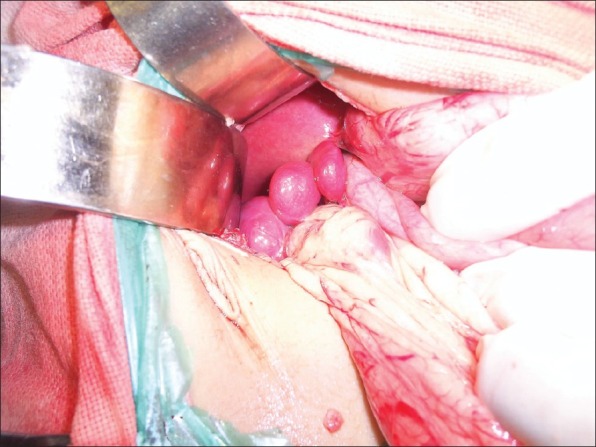
Polysplenia located in the upper-right quadrant along the greater curvature of the stomach
DISCUSSION
Heterotaxy syndrome (HS) is associated with an abnormal arrangement of organs and vessels. Based on the spleen, it has three major subtypes: (a) asplenia; (b) polysplenia, that is, cluster of small splenunculi, a multilobed spleen or a large spleen accompanied with several smaller splenules; and (c) normal spleen located in the right upper quadrant of the abdomen. (1) HS with asplenia (right atrial isomerism) is characterized by bilateral right-sidedness including bilateral “right” lungs with epiarterial bronchi, bilateral “right” atria and a symmetrical horizontal liver and no spleen.
HS with polysplenia also called as left atrial isomerism is characterized by a tendency toward bilateral left sidedness that may include bilateral “left” (bilobed) lungs with hyparterial bronchi, bilateral “left” atria and multiple spleens.[2] This is a rare complex disorder with an incidence of approximately 4 per 1 million live births. There is no age or sex predisposition. The etiology is unknown and believed to be multifactorial. Familial cases have also been reported. Apart from congenital cardiac anomalies (50–90%), HS is also associated with abnormal symmetry of liver (50–67%), preduodenal portal vein (17–50%), biliary atresia with hypoplasia of portal vein, abnormally “short” or truncated pancreas (50%), interruption of inferior vena cava with continuation via a dilated azygos or hemiazygos vein into superior vena cava (58–100%) and malrotation (70–100%) with or without midgut volvulus.[1] Congenital heart disease is the major cause of mortality. Our patient presented with polysplenia but no obvious lung anomalies and a small VSD.
Patients with heterotaxy may have different degrees of intestinal rotation varying from classic malrotation predisposing to volvulus to nonrotation, where due to a broader mesentery such a risk is reduced.[2] Due to this variability, there is some controversy regarding surgical intervention in all cases. Symptomatic patients, as in our case, with suspicion of midgut volvulus should undergo exploratory laparotomy promptly. As barium studies may not predict that patients will be at risk for midgut volvulus, the Ladd's procedure should perhaps be performed in all patients with malrotation.[3] Moreover, elective intervention is always better tolerated than an emergency surgery.[4,5] With continuing advances in cardiovascular care, there is improved survival beyond infancy and therefore the presence of an associated cardiac anomaly should not be a contraindication for surgical management of malrotation in children with heterotaxy. In our patient who had only a small VSD, the failure to thrive was most likely due to recurrent attacks of volvulus which had been neglected until then.
The presence of a thin transparent membranous sac enclosing the small bowel was also unusual in this case and has not been reported in the literature before. The sac could very well represent the amniotic membrane during physiological hernia in utero and gives us a likely embryological period at which the defects occurred. An appropriate contrast study should be performed in patients with unusual abdominal radiograph findings to avoid delay in diagnosis.
CONCLUSION
Diagnosis of malrotation volvulus in a child with heterotaxy is a challenge both for the clinician and radiologist. An elective Ladd's procedure is recommended in all these patients.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Kuvuturu S, Roper W, Stawicki SP. Acute pancreatitis in a patient with situs inversus/polysplenia syndrome: A case report and review of literature. OPUS 12 Scientist. 2008;2:10–2. [Google Scholar]
- 2.Ditchfield MR, Hutson JM. Intestinal rotational abnormalities in polysplenia and asplenia syndromes. Pediatr Radiol. 1998;28:303–6. doi: 10.1007/s002470050358. [DOI] [PubMed] [Google Scholar]
- 3.Powell DM, Othersen HB, Smith CD. Malrotation of the intestines in children: The effect of age on presentation and therapy. J Pediatr Surg. 1989;24:777–80. doi: 10.1016/s0022-3468(89)80535-4. [DOI] [PubMed] [Google Scholar]
- 4.Choi M, Borenstein SH, Hornberger L, Langer JC. Heterotaxia syndrome: The role of screening for intestinal rotation abnormalities. Arch Dis Child. 2005;90:813–5. doi: 10.1136/adc.2004.067504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yu DC, Thiagarajan RR, Laussen PC, Laussen JP, Jaksic T, Weldon CB. Outcomes after Ladd procedure in patients with Heterotaxy syndrome, congenital heart disease, and intestinal malrotation. J Pediatr Surg. 2009;44:1089–95. doi: 10.1016/j.jpedsurg.2009.02.015. [DOI] [PubMed] [Google Scholar]


