Abstract
We present here a case of an uncommon complex uterine anomaly – Obstructed HemiVagina with Ipsilateral Renal Agenesis (OHVIRA), also known as Herlyn-Werner-Wunderlich syndrome in a 14-year-old girl along with sonographic (trans-abdominal and trans labial), and MRI findings. The patient underwent surgery wherein imaging findings were confirmed. An MRI has proved to be of great help in correct diagnosis avoiding surgical interventions/ laparoscopy, which were needed in past to diagnose this rare anomaly. We also discuss the development of this anomaly with the help of a relatively new theory of uro-genital development by Acien and review the literature.
KEY WORDS: Herlyn-Werner-Wunderlich syndrome, mullerian anomaly, obstructed vagina, OHVIRA syndrome
INTRODUCTION
By the end of the 20th century, embryology of female urogenital system was accepted to be a truly-settled issue. While the utero-cervical development was believed to be from paired paramesonephric ducts; sinovaginal bulb from urogenital sinus was thought to develop into lower vagina; the kidneys and ureters were believed to arise from wolffian pro/meso/metanephros. Aberration in vertical or horizontal fusion or arrest of paramesonephric ducts during course of development was understood to successfully explain various uterine anomalies. Some complex uterine anomalies such as OHVIRA syndrome (Obstructed Hemi Vagina with Ipsilateral Renal Agenesis) still defied the conventional theory of urogenital development until recently when theory of development of entire vagina from mesonephric ducts was postulated.
CASE REPORT
A 14-year-old girl presented with continuous pain in lower abdomen for the last 4 months. She had menarche at 13 years and a normal menstrual cycle of 5/28 days. Physical examination revealed normal external genitalia. Clinical abdominal examination was unremarkable. Hemogram and other biochemical parameters were within normal range.
Ultrasound examination done elsewhere was reported as ‘Endometriosis’, and patient was sent to us for confirmation of sonographic findings and evaluation.
Trans-abdominal ultrasound of the pelvis revealed 2 uterine horns. There was minimal endometrial fluid collection in both the horns. The right horn was seen to communicate caudally with a large, ovoid fluid collection with internal echoes [Figure 1a–c]. Both ovaries were normal. In addition, USG revealed absence of the right kidney while left kidney was normal. Translabial ultrasound revealed the lower limit of pelvic fluid collection, which was seen to end 1.5 cm above introitus [Figure 2]. The findings pointed towards vaginal location of the collection. However, in view of a normal menstrual cycle, further evaluation was done with MRI.
Figure 1.
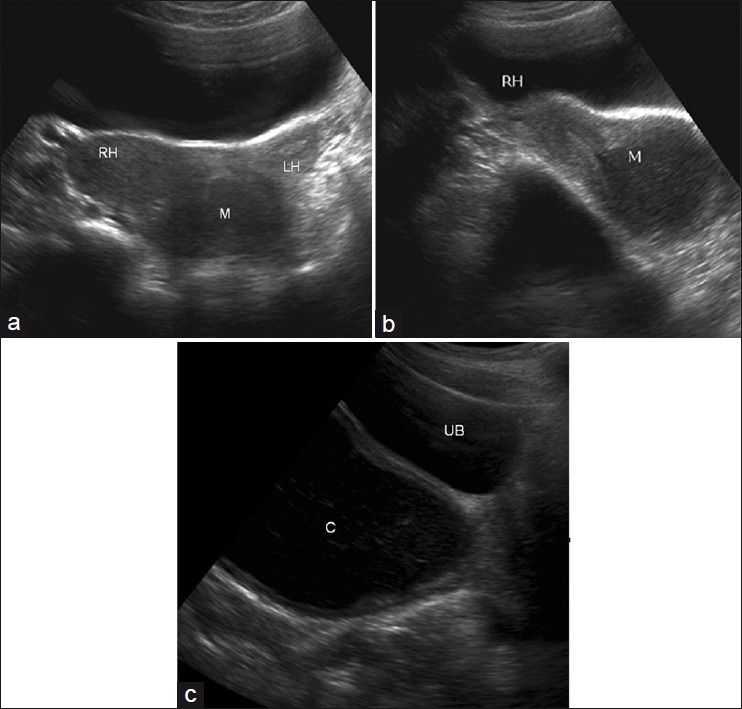
(a) Axial trans abdominal USG image showing right (RH) and left (LH) uterine horns. A hypoechoic lesion (M) is seen caudally (b) Sagittal trans abdominal USG image showing endometrial cavity of the right uterine horn (RH) communicating with the hypoechoic lesion (M) (c) Sagittal USG image directed further caudally shows the hypoechoic lesion to be an ovoid fluid collection with internal echoes, located posterior to the urinary bladder. It appears to end slightly above the introitus
Figure 2.
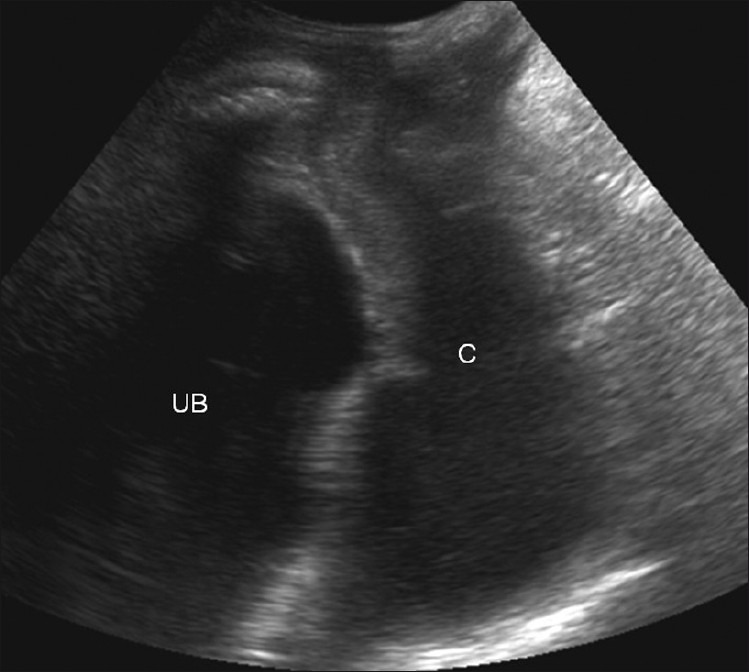
Trans labial sagittal USG image confirms that the collection (C) ends 1.5 cm above the introitus
An MRI, done the next day, confirmed the findings. In addition, it clearly demonstrated 2 vaginal cavities. The collapsed left hemivagina was seen to communicate with left cervix and corresponding uterine horn. The right hemivagina was markedly distended. Its lower end was convex and placed 1.5 cm above the introitus. The upper end communicated with the right uterine horn through the right cervix [Figure 3a and b]. Signal intensity of the contents of distended hemivagina was consistent with blood products, suggestive of a right hemato-hemicolpos [Figure 4a and b]. The MRI scored over sonography in very clear delineation of collapsed left hemivagina lumen and its continuity with ipsilateral uterine horn through left cervix. A diagrammatic representation of patient's anatomy makes it clearer [Figure 5]. A diagnosis of OHVIRA syndrome was made.
Figure 3.

(a) Coronal Single shot T2W image shows absence of the right kidney. The distended hemivagina (asterisk) is seen on the right side and the normal collapsed left hemivagina with minimal fluid is seen adjacent to it (black arrow). The distended hemivagina ends above the introitus and its contents are hypointense to fat. (b) Coronal Single shot T2W image shows right and left uterine horns (white arrows). The right uterine horn cavity is seen to communicate with the upper end of the fluid collection in right hemivagina (small black arrow)
Figure 4.
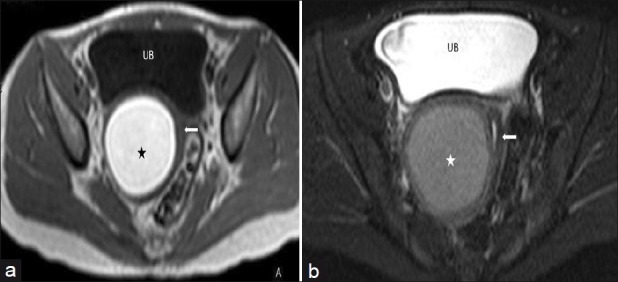
(a) Axial T1W image of the pelvis shows bright signal intensity of the right hemivaginal collection (asterisk). The collapsed left hemivagina is seen adjacent to it (arrow) (b) Axial fat saturated T2W image of the pelvis showing right hemivaginal collection (asterisk) and collapsed left hemivagina with minimal fluid (arrow)
Figure 5.
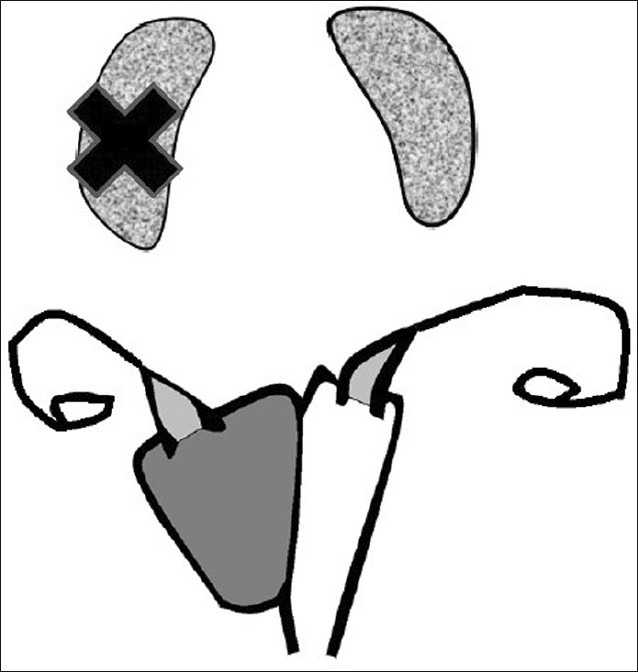
Diagrammatic representation of anatomy of patient showing OHVIRA syndrome
Local examination under anesthesia revealed a bulge in medial wall of the patent left hemivagina caused by the distended right hemivagina [Figure 6a].
Figure 6.
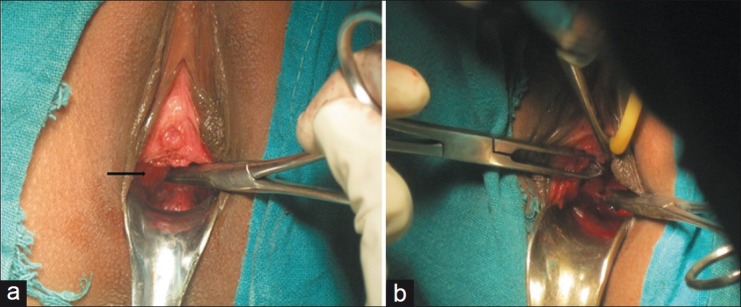
(a) Intraoperative photograph showing smooth bulge (black arrow) in medial wall of patent left hemivagina caused by right hematohemicolpos (b) Intraoperative photograph of septoplasty procedure showing drainage of altered blood
Patient was treated surgically by creating an opening in the septum between 2 hemivaginae and letting the collection in obstructed right hemivagina drain into patent left hemivagina. Patient was relieved of her symptoms [Figure 6b]. Post-operative follow up USG 1 month later revealed complete disappearance of hematocolpos and a collapsed hemivagina on right side. The cyclic dysmenorrhea disappeared. The surgical outcome was satisfactory with expectation of near normal fertility and normal sexual abilities.
DISCUSSION
Although the true incidence of mullerian defects is about 1.1 - 3.5%,[1] it is believed to be much higher (around 25%) in women with recurrent miscarriages and subfertility.[2] Review of literature in 15 reported studies consisting of 1771 patients during 1965 - 1996 period revealed mean incidence of uterus didelphys to be 11.1%.[2] A strong association of renal agenesis with uterus didelphys (81%)[3] has also been suggested.
The incidence of OHVIRA syndrome is very small and only isolated case reports have been published. Many of these present in an early infancy because of collection of secretions in the obstructed vagina under influence of maternal hormones; others are picked up within 1 - 2 years of onset of menarche due to development of hematocolpos, hematometra, or even hematosalpinx. These patients present with cyclical dysmenorrhea, which later evolves into persistent pelvic pain. Nearly all of them are initially misdiagnosed clinically as in our case which was thought to be endometriosis/tubercular collection on clinical grounds.
To understand the pathogenesis of mullerian anomalies and their association with renal anomalies, the embryology of utero-vaginal development needs to be reviewed. [Figure 7a]. Vaginal embryonic development has become a topic of hot debate consequent to propounding of new theory of vaginal origin by Acien.[4]
Figure 7.
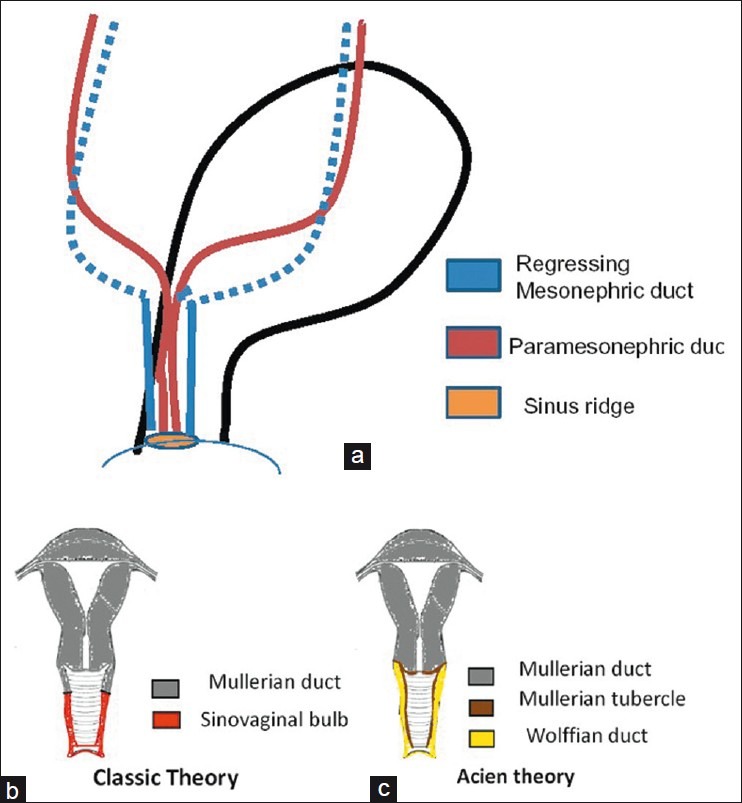
(a) Embryological development of the female urogenital system (b) Classic theory of development of uterus and vagina (c) Acien theory of development of uterus and vagina
The classic theory of vaginal development says that upper part of vagina develops from mullein (paramesonephric) duct and the lower part from sinovaginal bulbs derived from urogenital sinus. The fusion of 2 sinovaginal bulbs form vaginal plate, which canalize later to form vaginal lumen[5] [Figure 7b].
The classic theory was found inadequate in explaining complex mullerian malformations like OHVIRA and their coexistence with renal anomalies. Acien proposed that while uterus and cervix were derived from fused-paired paramesonephric ducts (2nd part) and divergent distal paramesonephric ducts (3rd part), the vagina was completely of mesonephric (wolffian) origin although its lining did reveal mullerian cells derived from mullerian tubercle. Hence, paramesonephric ducts do not contribute to formation of the vagina although mullerian tubercle does, such that the vagina is lined by cells from mullerian tubercle. [Figure 7c] This theory has been further reinforced by data published by Sánchez[6] in his experiments with female rats using histoimmunochemistry techniques.
An early failure of metanephric diverticulum to develop (around 5 weeks) from mesonephric duct results in agenesis of ureteric bud, which leads to agenesis of ipsilateral ureter and kidney.
Mesonephros is responsible for development and positioning of paired paramesonephric duct in close proximity. At around 9 weeks gestation, the paramesonephric duct is positioned in such a manner that it is lateral to mesonephric duct in first part, crosses it anteriorly and lies medial to it in converging portion. Due to failed positioning of paired paramesonephric duct, the two hemiuteri and hemicervices fail to unite, resulting in uterus didelphys. In OHVIRA syndrome, developmental arrest of ipsilateral mesonephric duct results in failure of distal hemivagina to develop, thereby resulting in obstructed hemivagina. The OHVIRA syndrome consists of uterus didelphys, unilateral low vaginal obstruction, and ipsilateral renal agenesis, all 3 components being secondary to mesonephric duct-induced müllerian anomalies.
Treatment invariably requires surgical intervention in the form of excision of vaginal septum to relieve obstruction. In addition to relief of pain due to obstruction, surgery also reduces chances of pelvic endometriosis due to retrograde menstrual seeding. Patients are able to have normal sexual life. Some are even able to conceive and carry pregnancy to term. In fact, hemihystrectomy, done in earlier times, is no more preferred now as the reported incidence of pregnancy in both horns is almost equal. Altchek and Paciuc have reported pregnancy occurring twice in a previously-obstructed didelphys uterus after surgical correction.[7] The surgeon must, therefore, make every effort to preserve the obstructed uterus.
In conclusion, OHVIRA syndrome is an uncommon congenital anomaly with clinical significance and simple surgical management. Imaging, particularly an MRI plays a major role in diagnosis, which is often missed clinically. Appropriate surgery is a single stage procedure to either excise or completely divide the obstructing septum. The complex mullerian anomalies have been difficult to diagnose correctly without help of imaging. An MRI has been particularly helpful. An early correct diagnosis is the goal to relieve the symptoms and prevent complications, caused by retrograde menstruation which may result in endometriosis and, also, preserve sexual and conception abilities.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Strassmann EO. Fertility and unification of double uterus. Fertil Steril. 1966;17:165–76. doi: 10.1016/s0015-0282(16)35882-4. [DOI] [PubMed] [Google Scholar]
- 2.Acien P. Incidence of Müllerian defects in fertile and infertile women. Hum Reprod. 1997;12:1372–6. doi: 10.1093/oxfordjournals.humrep.a019588. [DOI] [PubMed] [Google Scholar]
- 3.Li S, Qayyum A, Coakley FV, Hricak H. Association of renal agenesis and mullerian duct anomalies. J Comput Assist Tomogr. 2000;24:829–34. doi: 10.1097/00004728-200011000-00001. [DOI] [PubMed] [Google Scholar]
- 4.Acién P. Embryological observations on the female genital tract. Hum Reprod. 1992;7:437–45. doi: 10.1093/oxfordjournals.humrep.a137666. [DOI] [PubMed] [Google Scholar]
- 5.Koff AK. Development of the vagina in the human fetus. Contrib Embryol. 1933;24:59–91. [PubMed] [Google Scholar]
- 6.Sánchez-Ferrer ML, Acién MI, Sánchez del Campo F, Mayol-Belda MJ, Acién P. Experimental contributions to the study of the embryology of the vagina. Hum Reprod. 2006;21:1623–8. doi: 10.1093/humrep/del031. [DOI] [PubMed] [Google Scholar]
- 7.Altchek A, Paciuc J. Successful pregnancy following surgery in the obstructed uterus in a uterus didelphys with unilateral distal vaginal agenesis and ipsilateral renal agenesis: Case report and literature review. J Pediatr Adolesc Gynecol. 2009;22:e159–62. doi: 10.1016/j.jpag.2009.02.001. [DOI] [PubMed] [Google Scholar]


