Abstract
Objective:
To assess the influence of proseal laryngeal mask airway (PLMA) insertion on intraocular pressure (IOP).
Aim:
We compared the effects of PLMA insertion and laryngoscopic intubation on IOP and hemodynamic response in pediatric patients.
Background:
Previous studies have shown that there is no hemodynamic response to PLMA insertion similar to classic LMA insertion, but there is no published report about the influence of PLMA insertion on IOP. Conventional laryngoscopic tracheal intubation evokes a rise in IOP and cardiovascular response and has been traditionally used to secure the airway in pediatric patients undergoing ophthalmic surgery.
Materials and Methods:
59 patients, less than 14 years of age, scheduled for elective ophthalmic surgery were randomly divided into two groups, group P, in which the patient's airway was secured with PLMA (using introducer tool technique), and group T, in which the airway was secured with laryngoscopy-guided endotracheal intubation. Heart rate, blood pressure, and IOP were measured just before insertion of the airway device and subsequently three times at intervals of 1 min after insertion of the airway device.
Results:
In group T, there was a significant rise in IOP as well as hemodynamic parameters recorded. In group P, there was no significant rise in hemodynamic parameters, but a significant rise in IOP was found though the rise was less than in group T.
Conclusion:
We conclude that the PLMA use is associated with lesser cardiovascular response and rise in IOP as compared to tracheal intubation.
Keywords: Endotracheal intubation, intraocular pressure, proseal laryngeal mask airway
Introduction
Pediatric ocular surgery conventionally requires general anesthesia and tracheal intubation may have deleterious effects on cardiovascular function[1] and intraocular pressure (IOP).[2] Classic laryngeal mask airway (LMA) has been found to be superior to tracheal intubation in terms of maintaining stable IOP,[3] but positive pressure ventilation could become a challenge in certain cases. Proseal laryngeal mask airway (PLMA) offers the advantage of providing a better seal in the oropharynx to allow ventilation at much higher pressure and a drain tube to protect the lungs from aspiration and stomach from gastric insufflation.[4,5] Pressor response and changes in IOP to insertion of supraglottic devices such as classic LMA and i-gel[6] have been compared to tracheal intubation,[7] but changes in IOP to PLMA insertion have not been evaluated.
We undertook this study to compare the effects on IOP and cardiovascular response to PLMA insertion and laryngoscopic tracheal intubation in pediatric population.
Materials and Methods
Institutional ethical committee approval was taken and written informed guardians consent was obtained from 59 patients less than 14 years old scheduled to undergo elective ocular surgery under general anesthesia. All patients belonging to ASA grade I and II were randomly assigned to two groups using a closed envelope technique. In group P, patient's, airway was secured using PLMA (introducer tool technique) while in group T, with endotracheal tube following laryngoscopy. Glaucoma was ruled out by the ophthalmologist preoperatively. Grossly obese patients, those with known or apparent airway problems and those receiving any drug having an effect on IOP, were excluded from the study.
Monitoring included electrocardiography, heart rate, pulse oximetry, end tidal carbon-dioxide measurement, and noninvasive blood pressure. Eutectic mixture of local anesthetics was applied preoperatively to secure an intravenous (IV) access in operation room and all patients received pethidine 0.8 mg/kg IV followed by induction of anesthesia with thiopentone sodium titrated to loss of eyelash reflex. After ensuring adequacy of ventilation, vecuronium bromide 0.1 mg/ kg was given for neuromuscular (NM) blockade. Lungs were mask ventilated for 3 min with 66% nitrous oxide in oxygen with sevoflurane. NM block was monitored with peripheral nerve stimulator. When TOF count was zero, airway was secured using appropriately sized PLMA using introducer tool technique in group P, or endotracheal tube with Macintosh laryngoscope and the airway device was fixed using adhesive tapes to the skin over maxilla and mandible. Patients in whom more than one attempt was required for correct placement of either device were excluded from the study.
IOP was measured in the nonoperated eye (previously prepared with lubricant eye drops) just before insertion of the device and subsequently three times at an interval of 1 min after insertion of the device using Schiotz tonometer (The Diagnostic Company: Riester, Germany). Hemodynamic parameters which included heart rate, mean, systolic and diastolic blood pressure were recorded simultaneously at the time of measuring IOP.
Anesthesia was maintained using nitrous oxide in oxygen with sevoflurane and vecuronium top ups for NM blockade. At the end of the surgery, the residual NM blockade was antagonized with neostigmine and glycopyrrolate in appropriate dosages.
Sample size was selected to detect a projected difference of 25% between the groups with respect to IOP for a type I error of 0.05 and a power of 0.9 and the power of analysis was based on a previous study of IOP measurement with LMA. Data are represented as mean ± SD. Between group comparisons were done using Student's “t” test and nonparametric Mann-Whitney test in case data did not follow normal distribution. Within group analysis was done using paired “t” test and nonparametric Wilcoxon Signet Rank test in case the data was not normally distributed. P value < 0.05 was considered significant. Nonparametric test were used to determine the correlation coefficient.
Results
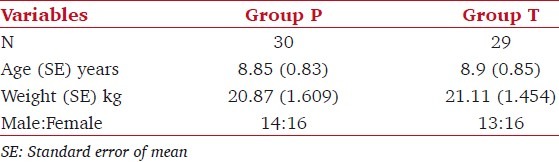
There was no significant difference in demographics between the two groups [Table 1]. Time taken for successful placement of the device in one attempt was similar in both the groups (group P 15 s and group T 18 s). Three patients in group P required more than one attempt for securing the airway and two patients required change in size of the PLMA. Two patients in group T also required a change in size of the endotracheal tube.
Table 1.
Demographic details of the patients
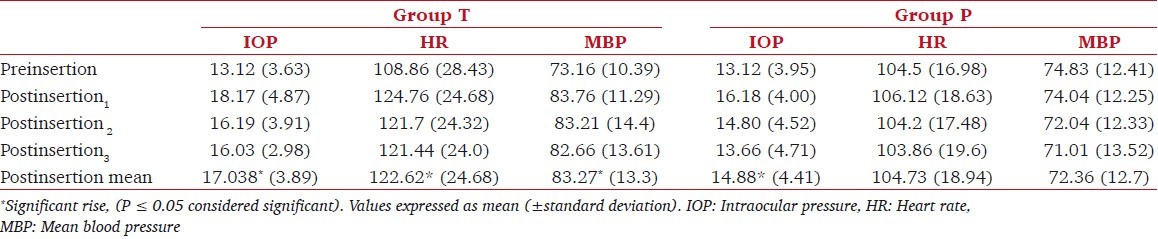
There was no significant difference in the heart rate (P = 0.476), mean blood pressure (P = 0.578), and IOP (P = 0.998) before insertion of the airway device between the two groups [Table 2]. Following insertion of endotracheal tube, there was a highly significant rise in heart rate (P = 0.000), mean blood pressure (P = 0.000), and IOP (P = 0.000). Though there was no significant rise in the heart rate (P = 0.921) and mean blood pressure (P = 0.327), there was a significant rise in IOP (P = 0.007) in group P [Table 2]. The percentage change in heart rate and mean blood pressure when compared between the two groups was found to be significant and highly significant, respectively. The mean IOP measured after insertion of PLMA was 14.8 mmHg in group P and 17.08 following laryngoscopy-guided intubation in group T and this difference was also statistically significant (P = 0.004). Unlike in group T, no significant positive correlation was found between hemodynamic response and rise in IOP in group P.
Table 2.
Comparison of measured parameters between the two groups
Discussion
There is no published data about the influence of PLMA insertion on IOP, although previous studies have shown that there is no cardiovascular response to PLMA insertion.[7] Laryngoscopy-guided endotracheal intubation evokes rise in hemodynamic response and IOP.[1,2] We found stable hemodynamics to PLMA insertion (introducer tool technique). However, there was a significant rise in IOP with the use of PLMA though the rise was lesser than that with the use of an endotracheal tube.
Hemodynamic response to laryngoscopy and intubation are a reflection of an increase in sympathoadrenal activity due to oropharyngeal and laryngotracheal stimulation.[8] Major afferent source of the stimuli responsible for the adrenergic response may be the supraglottic structures distorted by laryngoscopy.[9]
The anatomic contact of the PLMA is more than that of classic LMA and it distorts the supraglottic structures more with the larger conical distal cuff filling the hypopharynx more completely and the wedge-shaped proximal cuff filling the proximal laryngopharynx more completely to form a better seal.[4] The presence of larger cuff possibly causes more distortion/compression and increased difficulty in insertion makes PLMA elicit a greater pressor response.
I-gel has a soft gel like anatomical cuff made of thermoplastic elastomer that does not require inflation after its placement in the airway tract. This may prevent stimulation of sympathoadrenal axis and thus rise in IOP. The hemodynamic and IOP response to insertion of classic LMA and I-gel was compared to that after endotracheal intubation. I-gel was found to be superior to the other two airway devices in maintaining stable hemodynamics and was not associated with a rise IOP under general anesthesia.[6]
Arterial pressure plays a role in control of IOP but has a relatively minor role if the arterial pressure is in the physiological range.[10,11] In patients with an initial IOP > 11 mmHg, no correlation with arterial pressure was found but a good correlation existed between the IOP and central venous pressure (CVP).[12] In our study, the baseline IOP in both the groups was more than 11 mmHg (approx. 13 mmHg) and no significant correlation was deduced between arterial pressure and IOP in the group P. A significant rise in IOP was found in group T, which could be a consequence of greater pressor response to laryngoscope-guided tracheal intubation. We did not study the correlation of IOP with CVP because invasive monitoring is unwarranted in an ophthalmic surgical procedure. A study can be performed in nonophthalmic surgical procedures requiring CVP monitoring wherein the relation between IOP and CVP can be studied.
Directly measured mucosal pressure with a PLMA in situ, rarely exceeds 34 cmH2O, implying that mucosal ischemic injury would be uncommon.[13] There is no published data about the influence of proseal LMA on carotid artery and internal jugular vein, but its larger cuff may cause more distortion/compression of the surrounding structures[4] and this may lead to more pressure on these great vessels which in turn may affect the IOP. We found that although the hemodynamics remained stable after PLMA insertion, there was a significant rise in IOP from the baseline values.
IOP is also known to increase after a rise in PaCO2 as a result of choroidal vasodilatation or elevation of CVP or possibly a combination of both the mechanisms.[11] We ensured normocapnia throughout the intraoperative period.
We use PLMA for securing the airway of almost all pediatric patients for ophthalmic surgery. Use of PLMA ensures smooth recovery essential for ophthalmic surgeries and avoids complications like postoperative sore throat commonly associated with endotracheal intubation. Applanation tonometry is the gold standard in measuring IOP and Schiotz tonometer is not very accurate. This was the limitation in our study, since for intraoperative measurements of IOP in our institute, ophthalmologists use the Schiotz tonometer.
We found a significant rise in IOP post PLMA insertion from the baseline values (mean IOP = 14.8 mmHg), with the maximum rise being 22.9 mmHg. The mean rise in IOP was within the normal range of 10–20 mmHg, which should not be deleterious to a normal eye but can be harmful for a patient with glaucoma or hypertension.
We conclude that PLMA has an advantage over laryngoscopy-guided tracheal intubation in minimizing the rise in IOP and hemodynamic response in patients with normal baseline IOPs. However, caution should be exercised when using PLMA in patients with glaucoma or hypertension in who even a minimal rise in IOP may prove harmful for the eye. Further studies are required to substantiate our results in patients with glaucoma and hypertension.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Bishop MJ, Bedford RF, Kil HK. Physiologic and Pathophysiologic Responses to Intubation. In: Benumof Jl., editor. Airway Management Principles and Practice. 1st ed. Mosby: Saunders, Philadelphia; 1996. pp. 102–17. [Google Scholar]
- 2.Wynands JF, Cromwell DF. Intraoccular tension in association with succinylcholine and endotracheal intubation: a preliminary report. Can Anaesth Soc J. 1960;7:39–43. doi: 10.1007/BF03013681. [DOI] [PubMed] [Google Scholar]
- 3.Lamb K, James MF, Janicki PK. The laryngeal mask airway for intraocular surgery: effects on intraocular pressure and stress responses. Br J Anaesth. 1992;69:143–7. doi: 10.1093/bja/69.2.143. [DOI] [PubMed] [Google Scholar]
- 4.Brimacombe JR. ProSeal LMA for ventilation and airway protection. In: Brimacombe JR, editor. Laryngeal Mask Airway Principles and Practice. 2nd ed. Philadelphia, USA: WB Saunders; 2005. pp. 503–537. [Google Scholar]
- 5.Keller C, Brimacombe J. Mucosal Pressure and oropharyngeal leak pressure with the Proseal verses the classic laryngeal mask airway. Br J Anaesth. 2002;85:262–6. doi: 10.1093/bja/85.2.262. [DOI] [PubMed] [Google Scholar]
- 6.Brimacombe J, Keller C, Fullekrug B, Agro F, Rosenblatt W, Dierdorf SF, et al. A multicenter study comparing the Proseal with the Classic laryngeal mask airway in anesthetized, nonparalyzed patients. Anesthesiology. 2002;96:289–95. doi: 10.1097/00000542-200202000-00011. [DOI] [PubMed] [Google Scholar]
- 7.Ismail SA, Bisher NA, Kandil HW, Mowafi HA, Atawia HA. Intraocular pressure and haemodynamic responses to insertion of the i-gel, laryngeal mask airway or endotracheal tube. Eur J Anaesthesiol. 2011;28:443–8. doi: 10.1097/EJA.0b013e328345a413. [DOI] [PubMed] [Google Scholar]
- 8.Derbyshire DR, Chmielewski A, Fell D, Vater M, Achola KJ, Smith G. Plasma catecholamine response to tracheal intubation. Br J Anaesth. 1983;55:855–60. doi: 10.1093/bja/55.9.855. [DOI] [PubMed] [Google Scholar]
- 9.Shribman AJ, Smith G, Achola KJ. Cardiovascular and catecholamine responses to laryngoscopy with and without tracheal intubation. Br J Anaesth. 1987;59:295–9. doi: 10.1093/bja/59.3.295. [DOI] [PubMed] [Google Scholar]
- 10.Macri FJ. Vascular pressure relationships and the intraocular pressure. Arch Opthalmol. 1961;65:571–4. doi: 10.1001/archopht.1961.01840020573021. [DOI] [PubMed] [Google Scholar]
- 11.Murphy DF. Anesthesia and intraocular pressure. Anesth Analg. 1985;64:520–30. [PubMed] [Google Scholar]
- 12.Tsamparlakis J, Casey TA, Howell W, Edridge E. Dependence of intraocular pressure on induced hypotension and posture during surgical anaesthesia. Trans Ophthalmol Soc U K. 1980;100:521–6. [PubMed] [Google Scholar]
- 13.Shimbori H, Ono K, Miwa T, Morimura N, Noguchi M, Hiroki K. Comparison of the LMA-ProSeal and LMA-Classic in children. Br J Anaesth. 2004;93:528–31. doi: 10.1093/bja/aeh238. [DOI] [PubMed] [Google Scholar]


