Abstract
Background:
It is well documented that pressure-controlled ventilation (PCV) improves oxygenation and ventilation compared to volume-controlled ventilation and reduces peak airway pressure in gynecological laparoscopy. PCV with moderately inversed inspiratory–expiratory (I: E) ratio can successfully recruit collapsed alveoli and has been proved to be beneficial in intensive care. We tested the hypothesis that altering the I: E ratio to 1.5:1 in PCV improves ventilation during gynecological laparoscopy using laryngeal mask airway (LMA).
Objective:
To study pressure-controlled inverse ratio ventilation (PCIRV) with I: E ratio 1.5:1 as against PCV with I: E ratio 1:2 in gynecological laparoscopy with LMA using noninvasive parameters.
Materials and Methods:
Intraoperative hemodynamics and side-stream spirometry recordings were noted in 20 consecutive patients undergoing major gynecological laparoscopy with LMA. Flexible LMA or LMA supreme were used depending on normal body mass index (BMI) or high BMI, respectively.
Results:
Reversing the I: E ratio to 1.5:1 increased the tidal volume, mean airway pressures, and dynamic lung compliance significantly, all indicating better oxygenation at comparable peak airway pressures as against PCV with I: E ratio 1:2. There was no change in the end-tidal carbon dioxide. There was no auto-positive end expiratory pressure (PEEP) or change in the hemodynamics.
Conclusion:
Reversal of I: E ratio with PCV can be beneficially used with LMA in laparoscopy.
Keywords: Gynecological laparoscopy, inverse ratio ventilation, laryngeal mask airway, pressure-controlled ventilation
Introduction
Laparoscopy is associated with decreased functional residual capacity and increase in the peak airway pressure. Gynecological laparoscopy usually requires lithotomy and Trendelenburg position demanding additional ventilatory adjustments to maintain oxygenation and normocarbia.[1,2]
Laryngeal mask airway (LMA) has been used in gynecological laparoscopy.[2] It reduces intubation and extubation response, gives better oxygen saturations at extubation, and reduces postoperative morbidity and analgesia requirement. LMA supreme, because of its better sealing pressure, is used in patients where ventilatory pressures are expected to be higher than normal.[3] Use of pressure-controlled ventilation (PCV) with LMA has proved to be beneficial in adult as well as pediatric surgeries.[4,5] It reduces peak airway pressure and delivers a better tidal volume at comparable airway pressures.[5] The improvement in ventilation during PCV is thought to be due to altered flow pattern that improves alveolar gas distribution and not merely due to reduction of air leaks.[6] Inverse ratio ventilation (IRV) has been extensively used in intensive care units, postoperative cardiac surgeries,[7,8] and there are also reports of it being used in lower abdominal surgeries.[9] Longer inspiratory times improve the gas flow to the alveoli of slow time constants, thereby improving oxygenation in Acute Respiratory Distress Syndrome patients.[10]
Increase in the mean airway pressure, a typical feature of IRV that recruits collapsed alveoli, could thus improve ventilation during laparoscopy. We tested this hypothesis in this study.
Materials and Methods
20 consecutive patients between 18 and 60 years, American Society of Anesthesiologists class 1–3, scheduled for elective major gynecological laparoscopy with expected duration of surgery more than 45 min, were included in the study after written informed consent and ethic committee approval. Exclusion criteria were patients with history of gastroesophageal reflux disease, known allergy to any of the drugs used during the study, and patients with predicted difficult airway. Patients were premedicated with ranitidine 150 mg, metoclopramide 10 mg, and clonidine 100 mcg orally 1 h prior to surgery. After preoxygenation, anesthesia was induced with 1 mg midazolam, fentanyl 3 mcg/kg, and propofol 2–2.5 mg/kg intravenous (IV). Neuromuscular blockade was achieved with atracurium 0.6 mg/kg IV as a bolus and maintained intraoperatively with 0.12 mg/kg IV top-ups. Size 4 flexible LMAs were used for patients with a body mass index (BMI) less than 30 (18), while LMA supreme size 3 was used for patients with BMI more than 30 (2). The cuff was inflated with air until effective seal was obtained to the maximum 30 cc when there was no audible or palpable leak. Volume-controlled ventilation (VCV) was initiated with tidal volume 8 ml/kg body weight (Aestiva, GE/Datex-Ohmeda). Respiratory rate was adjusted (8–10) to maintain end-tidal carbon dioxide (EtCO2) between 34 and 37 mmHg. inspiratory–expiratory (I: E) ratio was kept 1:2. Maintenance of anesthesia was with 50% nitrous oxide with isoflurane 1%–1.5% in oxygen. Intraoperative monitoring included side-stream spirometry, noninvasive blood pressure, pulse oximetry, end-tidal carbon dioxide, 5-lead EKG, gas monitoring, and entropy. Anesthesia was supplemented by IV propofol infusion 2 mg/kg/h to stabilize entropy between 35 and 50. After pneumoperitoneum ventilation was changed to PCV with positive end expiratory pressure (PEEP) of 5 cm of H2O with I:E ratio 1:2. After 30 min readings were recorded. I: E ratio was now changed to 1.5:1 on the mode PCV (with IRV) [PCIRV] and PEEP of 5 cm of H2O continued. Readings were taken after 10 min of PCIRV.
At the conclusion of surgery residual neuromuscular blockade was reversed with neostigmine 0.05 mg/kg and glycopyrrolate 0.008 mg/kg. Patient was allowed to breath spontaneously on the LMA and it was removed when entropy was beyond 80 with return of protective reflexes.
Any presence of oropharyngeal leak, hypotension, bradycardia, auto-PEEP was noted. Hemodynamic, spirometry, EtCO2, and pulse oximeter recordings were noted as per the following schedule:
-
a)
baseline VCV, prior to peritoneal insufflation with carbon dioxide,
-
b)
on VCV with PEEP of 5 cm of H2O after reaching the desired intra-abdominal pressure (15 mm of Hg) with patient in Trendelenburg and lithotomy position,
-
c)
After 30 min of PCV with I: E = 1:2,
-
d)
10 min after PCIRV with I: E = 1.5: 1
Choosing compliance loops not disturbed by surgical manipulation or intraperitoneal suction ensured the quality of the recordings. A trained technician blinded to the study protocol recorded the readings.
All the measurements were done using a side-stream spirometry device (D-lite™ flow sensor of S/5™ Anesthesia Monitor, Datex-Ohmeda), which continuously computes flow and pressure readings derived via a pressure sensor system, attached between the airway tube and the Y-piece. Spirometry readings included peak, plateau, mean airway pressures, airway compliance, PEEP, and airway resistance along with pressure-volume loop and flow–time graph. Hemodynamic monitoring included heart rate and noninvasive blood pressure. Stomach grading was done after the first trocar insertion and also just prior to deflation of pneumoperitoneum by the surgeon blinded to the ventilatory protocol. The reading was considered 0 when stomach was not visualized and 10 when it was obstructing surgical view.[11]
Statistical analysis was done using paired t-test and results were obtained at 95% confidence limit (SPSS version 15.0). Significance was defined at p ≤ 0.05. Data were presented as mean (SD). The main variable in the study, the mean airway pressure, was having a standard deviation of 1.2 from the pilot study done on 10 patients. A priori power analysis using two-sided analysis with an α error of 0.05 and a power of 0.8 showed that 20 patients were needed for the study.
Results
All 20 patients were adult females with an average age (39.3 years ± 7.87) and BMI (24.38 ± 4.42 kg/m2]) [Table 1]. The mean duration of surgery was 77 ± 32.6 min. The peak and plateau pressures after pneumoperitoneum during PCV were 26.5 ± 3.88 and 26.25 ± 3.8 cm of H2O, respectively) and during PCIRV 26.4 ± 3.66 and 26.2 ± 3.5 cm of H2O, respectively [Figure 1] and were statistically similar. However, the mean airway pressure (PAW) during PCV (12.1 ± 1.25 cm of H2O) was lower than PCIRV (17.3 ± 2.08 cm of H2O) (P = 0.000) [Figure 2]. Tidal volume on PCIRV (502 ± 47.19 ml) was significantly higher as compared to PCV (457 ± 39.35 ml) (P = 0.00) [Figure 3]. The dynamic compliance on PCIRV (23.7 ± 4.19 ml/cm H2O) was also significantly higher than PCV (21.45 ± 3.73 ml/cm H2O). There was no significant difference in the EtCO2 values during PCV and PCIRV (35.5 ± 1.8 and 34.85 ± 2.5, respectively). Mean oxygen saturation observed in this study though higher in PCIRV (99.10 ± 0.78) than in PCV (98.65 ± 1.08) (P = 0.009) was not statistically significant. The heart rate and mean arterial pressure in PCV and PCIRV were not significantly different from each other (P = 0.57 and P = 0.435, respectively). No oropharyngeal leak was observed and there was no change in the stomach grading.
Table 1.
Spirometry and hemodynamics in pressure-controlled ventilation (PCV) and pressure-controlled inverse ratio ventilation (PCIRV), expressed as mean (SD)
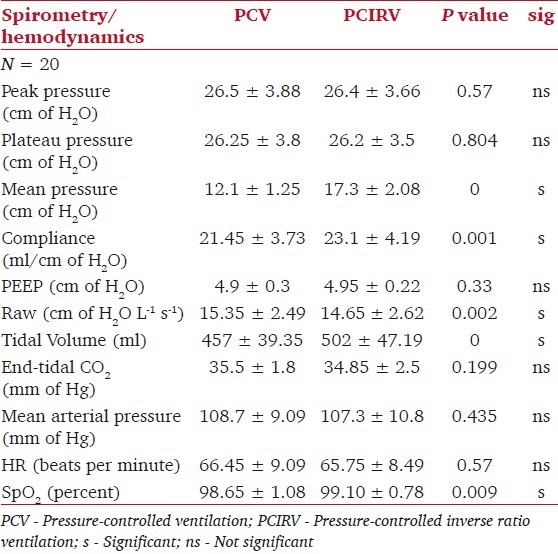
Figure 1.
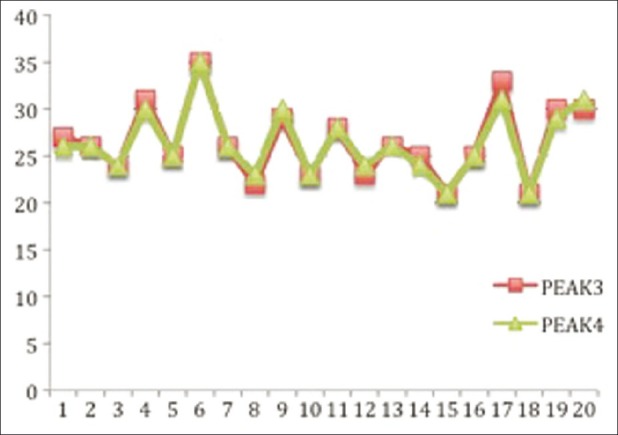
Comparison of Peak Airway Pressures during PCV (peak 3)and PCIRV(peak4) X axis- no. of patients, Y- axis- airway pressure in cm of H2O
Figure 2.
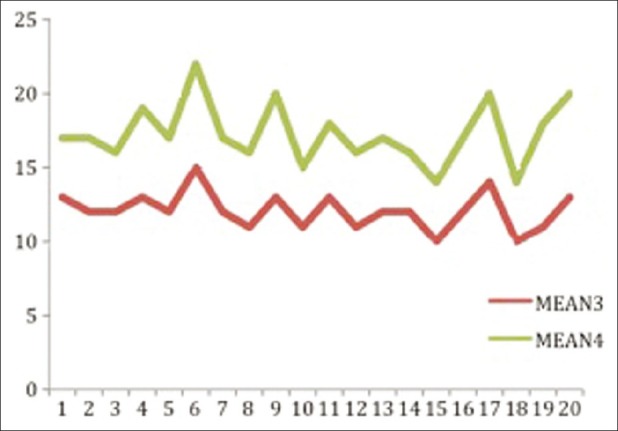
Comparison of Mean Airway Pressures during PCV(mean3) and PCIRV(mean4) X axis- no. of patients, Y axis- airway pressures in cm of H2O
Figure 3.
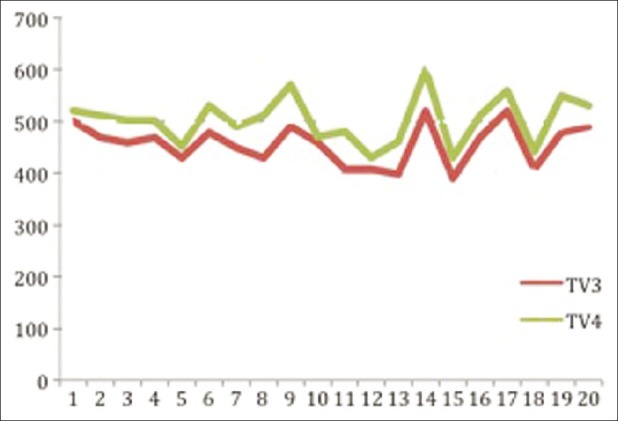
Comparison of Tidal volumes during PCV(TV3) and PCIRV(TV4). Xaxis- no of patients, Y-axis- tidal volume in ml
Discussion
Our study comparing PCV with I: E ratio 1:2 and PCIRV with I:E ratio 1.5:1. Higher PAW and tidal volume (TV) was observed in PCIRV as compared to PCV. These differences were seen despite peak and plateau pressures being similar in both types of ventilation. The higher tidal volume in PCIRV possibly resulted from the decelerating flow of PCV combined with optimally inversed I:E ratio which sustained the inspiratory pressure for a longer time. This facilitated ventilation of the slow recruiting alveoli. Increased alveolar oxygenation during PCV has been attributed to the increase in the PAW.[6] Higher PAW achieved by moderate prolongation of the I/E ratio with optimum extrinsic PEEP improves ventilation in the intensive care units and trauma patients.[10,12] Benefits of IRV, though well known to postoperative care units, have not been studied in laparoscopy so far. IRV increases dynamic lung compliance and also improves oxygen saturation. With increasing I:E ratios, one may encounter auto-PEEP, circulatory collapse, and barotrauma.[12,13] On the contrary, moderate reversal of I:E ratio to 1.5:1 not only improves the PAW, the key determinant of alveolar ventilation, but also allows sufficient time for expiration and avoids generation of auto-PEEP. This mode of ventilation does not find any mention in laparoscopy so far in literature.
Every 100 ml increase in the tidal volume reduces PaCO2 on average by 5.3 mm Hg in normal-weight patients and by 3.6 mmHg in morbidly obese patients.[14] In our study, the tidal volume in PCIRV (502 ± 47.19 ml) is significantly higher than that in PCV (457 ± 39.35 ml) (P = 0.00) but determining the exact fall in the PCO2 was beyond the scope of the study. Llorens et al. found that only changing the inspiratory pressures and the ratio of inspiratory time to total time without much changing the minute ventilation was enough to compensate the changing lung mechanics during gynecological laparoscopy.[15]
We found no evidence of intrinsic PEEP. Vasopressors were not needed and grading of stomach view did not change. Achieving best tidal volume at a given oropharyngeal leak pressure can be challenging at times for the anesthetists who are using LMA for gynecological laparoscopy. Changing the I: E ratio to 1.5:1 proves beneficial in such situations.
The limitation of our study is that it is the study of limited data from 20 female patients; invasive monitoring with arterial blood gas sampling was not performed and it is a single blinded study. The mean duration of surgery in our study was 77 ± 32.6 min. Since this type of ventilation has not been tested before using LMA, we limited its usage to 10 min. We found no contraindication for using the LMA for longer durations.
Conclusion
PCIRV with I: E ratio 1.5:1 can be an effective mode of ventilation in major gynecological laparoscopy using LMA. It is an unconventional mode of ventilation in laparoscopy and can be used when conventional methods seem inadequate to achieve the set tidal volume at a given peak airway pressure, like in the case of moderately obese patients. It delivers better tidal volume compared to either PCV or VCV with I: E ratio 1:2. It is associated with the rise in the PAW, oxygen saturation, and dynamic lung compliance, which are the indicators of better alveolar ventilation.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Nguyen NT, Anderson JT, Budd M, Fleming NW, Ho HS, Jahr J, Stevens CM, et al. Effects of pneumoperitoneum on intraoperative pulmonary mechanics and gas exchange– during laparoscopic gastric bypass. Surg Endosc. 2004;18:64–71. doi: 10.1007/s00464-002-8786-x. [DOI] [PubMed] [Google Scholar]
- 2.Natalini G, Facchetti P, Decembrini MA, Lanza G, Rosano A, Bernardini A, et al. Pressure controlled versus volume controlled ventilation with laryngeal mask airway. J Clin Anesth. 2001;13:436–9. doi: 10.1016/s0952-8180(01)00297-5. [DOI] [PubMed] [Google Scholar]
- 3.Carron M, Freo U, Ori C. Usefulness of spirometry in air leak evaluation during laparoscopic surgery in an obese patient with laryngeal mask airway Supreme™. Br J Anaesth. 2010;105:387–89. doi: 10.1093/bja/aeq223. [DOI] [PubMed] [Google Scholar]
- 4.Goldmann K, Roettger C, Wulf H. Use of the ProSeal laryngeal mask airway for pressure-controlled ventilation with and without positive end- expiratory pressure in paediatric patients: a randomized, controlled study. Br J Anaesth. 2005;95:831–4. doi: 10.1093/bja/aei246. [DOI] [PubMed] [Google Scholar]
- 5.Jeon WJ, Cho SY, Rang Bang M, Ko SY. Comparison of Volume-controlled and pressure-controlled ventilation using a laryngeal mask airway during gynecological laparoscopy. Korean J Anesthesiol. 2011;60:167–72. doi: 10.4097/kjae.2011.60.3.167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Baker AB, Babington PC, Colliss JE, Cowie RW. Effects of varying inspiratory flow waveform and time in intermittent positive pressure ventilation I: Introduction and methods. Br J Anaesth. 1977;49:1207–20. doi: 10.1093/bja/49.12.1207. [DOI] [PubMed] [Google Scholar]
- 7.Shu-Hui W, Ta-Sen W. The outcome of early pressure controlled inverse ratio ventilation on patients with severe acute respiratory distress syndrome in surgical intensive care unit. Am J Surg. 2002;183:151–5. doi: 10.1016/s0002-9610(01)00870-4. [DOI] [PubMed] [Google Scholar]
- 8.Smith RP, Fletcher R. Pressure controlled inverse ratio ventilation after cardiac surgery. Eur J Anaesthesiol. 2001;18:401–6. doi: 10.1046/j.0265-0215.2001.00864.x. [DOI] [PubMed] [Google Scholar]
- 9.Tweed WA, Tan PL. Presssure controlled –inverse ratio ventilation and pulmonary gas exchange during lower abdominal surgery. Can J Anaesth. 1992;39:1036–40. doi: 10.1007/BF03008371. [DOI] [PubMed] [Google Scholar]
- 10.Yanos J, Watling SM, Verhey J. The Physiologic Effects of Inverse Ratio Ventilation. Chest. 1998;114:834–8. doi: 10.1378/chest.114.3.834. [DOI] [PubMed] [Google Scholar]
- 11.Maltby JR, Beriault MT, Watson NC, Fick GH. Gastric distension and ventilation during laparoscopic cholecystectomy: LMA-Classic vs.tracheal intubation. Can J Anaesth. 2000;47:622–6. doi: 10.1007/BF03018993. [DOI] [PubMed] [Google Scholar]
- 12.Gore DC, Dennis C. Haemodynamic and ventilatory effects associated with increasing inspiratory-expiratory ventilation. J Trauma. 1998;45:268–72. doi: 10.1097/00005373-199808000-00011. [DOI] [PubMed] [Google Scholar]
- 13.Connery LE, Deignan MJ, Gujer MW, Richardson MG. Acute respiratory distress syndrome, mechanical ventilation, and right ventricular function. Br J Anaesth. 1999;83:493–5. doi: 10.1093/bja/83.3.493. [DOI] [PubMed] [Google Scholar]
- 14.Sprung J, Whalley DG, Falcone T, Warner DO, Hubmayr RD, Hammel J. The impact of Morbid Obesity, Pneumoperitoneum and Posture on Respiratory System Mechanics and Oxygenation during Laparoscopy. Anesth Analg. 2002;94:1345–50. doi: 10.1097/00000539-200205000-00056. [DOI] [PubMed] [Google Scholar]
- 15.Llorens J, Ballester M, Tusman G, Blasco L, Garcia-Fernandez J, Jover J, et al. adaptive support ventilation for gynaecological laparoscopic surgery in Trendelenburg position: Bringing ICU modes of mechanical ventilation to the operating room. Eur J Anaesthesiol. 2009;26:135–9. doi: 10.1097/EJA.0b013e32831aed42. [DOI] [PubMed] [Google Scholar]


