Abstract
Background:
Three decades ago, Epidemiologists began to report a strong association between depression and cardiovascular disease - morbidity and mortality, and in the last decade, many large-scale studies have identified depression as an important risk factor for Coronary Artery Disease (CAD) and its morbidity and mortality.
Objectives:
To determine the frequency of clinical depression among patients admitted with Acute Coronary Syndrome (ACS) to the Coronary Care Unit (CCU) at King Fahd Hospital of the University (KFHU), and to find out if there is any relationship between depression and the traditional risk factors for CAD.
Methods:
One hundred and two patients admitted consecutively with ACS completed the self-rated Beck Depression Inventory (BDI) in their native language. The patients were classified into two groups: Group A comprising patients with no symptoms of depression and patients with subclinical or borderline depression, scored less than 21 points on BDI score scale; and Group B composed of those who scored 21 points and above. Various statistical tests were used whenever appropriate.
Results:
One hundred and two patients completed the BDI. Ninety-Two (90.2%) were males, with a mean age of 52.14±12.14 years. Of these, 37.3% were Saudis, 25.5% Non-Saudi Arabs, 31.4% from the Indian subcontinent and 5.9% were other Asians. Patients from the Indian Subcontinent were significantly younger than the Saudis (p<0.0001). The evidence of clinical depression was found in 20.6% of all patients, 13.2% of Saudi patients, 19.2% of Non-Saudi Arabs and 34.4% of those from the Indian subcontinent. There was a significant difference in the frequency of clinical depression between Saudi patients and the Indians (p=0.035). Smoking and dyslipidemia were the only strong predictors of clinical depression in our study.
Conclusion:
Depression is unquestionably associated with CAD. Its frequency in our patients with ACS was 20.6%, and the highest frequency was recorded among patients from the Indian subcontinent (34.4%). Smoking and dyslipidemia were the strongest independent risk factors for depression.
Keywords: Depression, Acute Coronary Syndrome, Coronary Artery Disease, Beck Depression Inventory
INTRODUCTION
The Cardiovascular System is the most important system in the human body. The functions of the brain and other body system organs are strongly dependent on proper cardiac performance. Our daily life appropriately emphasizes the strong connections between the heart, emotional reactions and social functions. Therefore, the appearance of normal emotional reactions such as shock, fear, anger, sadness, and grief in response to the development of heart disease is not unexpected.1 Three decades ago, epidemiologists began to report strong associations between depression and cardiovascular disease, morbidity and mortality; though, this association was the subject of a lot of criticism.2 During the last decade, many large-scale well-designed controlled studies have identified depression as an important risk factor for both first myocardial infarction (MI) and cardiovascular mortality.3–5 All clinical grades of depression even minor depression have been found to be associated with significantly increased risk of subsequent cardiovascular morbidity and mortality in patients with known Coronary Heart Disease (CHD).6–14 The prevalence of major depression disorder (MDD) is estimated to be between 15% and 23% among patients with known CHD,9,13,15 though it is frequently underdiagnosed and undertreated.16,17 Nevertheless, clinical depression has been recognized as an independent risk factor for the incidence of CHD for several decades (after the onset of clinical depression).18 The possible explanation of this association is the enhanced platelet activity in depressed patients. In the Sertraline Anti-Depressant Heart Attack Randomized Trial (SADHART) Platelet Substudy, the treatment with Sertraline (SSRI) was associated with substantial reduction of Platelet/Endothelial Activation, despite co-administration of widespread antiplatelet regimen including aspirin and Clopidogrel.19 In this study, our aim was to determine the frequency of clinical depression among patients who were admitted to Coronary Care Unit (CCU) with Acute Coronary Syndrome (ACS) in this part of the world with a different social and cultural environment.
OBJECTIVES
The objectives of this study were to: (1) determine the frequency of clinical depression among patients admitted with ACS to the CCU at King Fahd Hospital of the University; (2) find any association between depression and the traditional risk factors for coronary artery disease (CAD) such as age, sex, diabetes mellitus, hypertension, smoking, dyslipidemia, and strong family history of coronary artery disease.
METHODOLOGY
This was a prospective study conducted in King Fahd Hospital of the University (450-bed teaching hospital), Al Khobar, Eastern Province, Kingdom of Saudi Arabia (KSA), between July 2003 and February 2004.
Inclusion Criteria
To qualify for inclusion, males and females were required to have a definite history of chest pain strongly suggestive of Unstable Angina (UA), Acute non-ST segment elevation myocardial infarction (NSTEMI) or ST segment elevation myocardial infarction (STEMI), the three components of acute coronary syndrome.
The diagnosis of unstable angina (UA) mainly depended on a convincing history of episodes of chest pain occurring at rest and lasting at least 10 minutes and leading to hospitalization, or a history of UA in a patient with a known coronary artery disease and a documented history of a prior myocardial infarction. The patient should have undergone a prior revascularization procedure, or had documented coronary artery stenosis greater than 75% in one of the major epicardial coronary arteries. The diagnosis of NSTEMI and STEMI depended mainly on a convincing prolonged chest pain lasting for more than 20 minutes, associated with electrocardiographic changes (ST segment depression, T waves inversion, ST segment elevation and Q waves), and specific cardiac enzymes elevation, e.g. creatine phosphokinase isoenzyme MB (CPK-MB), greater than the upper limit of normal and Troponin I or Troponin T more than two times the upper limit of normal.
Exclusion Criteria
The exclusion criteria included all of the following conditions: patients with an obvious language barrier, patients with abnormal cognitive functions, those with ACS of non-atherosclerotic etiology (e.g. anemia or cocaine use), Klipp Class III or IV status, those with persistent and clinically significant laboratory abnormalities such as severely impaired liver function test, thyroid function test and renal function test; patients with other significant non-cardiac disease such as chronic renal failure, chronic hepatic failure, and hypothyroidism, alcohol and substance abuse or dependence in the past six months, and finally a history of psychosis, bipolar disorder, Organic Brain Syndrome (OBS), or dementia.
The Study Sample
One hundred and two patients admitted consecutively to the CCU with Acute Coronary Syndrome (ACS) who met our inclusion criteria completed the self-rated Beck Depression Inventory (BDI) in their native language.24 The BDI which includes 21 multiple-choice questions (MCQs) was completed after the presenting symptoms were alleviated, 4 -7 days after the onset of ACS. BDI has been an internationally accepted practical questionnaire since 1961, and has been validated.21,22 The opinions of expertise in the fields of psychiatry, cardiology and community medicine were also obtained for the purpose of validation of BDI in KSA. The reliability of patient responses was calculated using Chronbach α = 0.82 which indicating high reliability. The study sample was divided according to patient ethnic background as follows: Saudi Arabs, Non-Saudi Arabs, patients from the Indian subcontinent (Indians, Pakistanis, Bangladeshi and Sri Lankans) and others mainly Asians. Arabic, Hindi, Urdu and English were initially used and the inventory was subsequently translated into English. Our patients were classified into two groups: Group A included those patients with subclinical depression or with no depression scoring 0-20 points on BDI score scale, and Group B for those scoring 21 points and above.
Statistical Analysis
The data were entered into a Personal Computer (PC) using Statistical Package for Social Science Version 10 (SPSS). Descriptive statistics for all variables were performed after scrutinizing the data.
T-test and Mann Whitney were used to compare between BDI total score and each of the different variables as appropriate. Analysis of variance (ANOVA) or Kruskal-Wallis were used appropriately to ascertain any differences among nationalities, age and BDI mean total score. The Levene test was used as the criteria for choosing between parametric and non-parametric tests. The Chi-square test was used to determine any association between risk factors and the total scores after categorizing them into two groups: sub-clinical and clinical depression. Logistic regression analysis was implemented to find the effect of different risk factors and BDI total score after clinical categorization. The level of significance was set at <0.05 throughout the study.
RESULTS
One hundred and two consecutive patients were able to complete BDI, 4-7 days after the onset of ACS. Table 1 describes the general characteristics of the study patients. Of this number, 92 were males (90.2%); and the remainder females, with a mean age of 52.14 ± 12.14 years; 51.43 ± 10.57 years for males, and 58.60 ± 21.71 years for females (p=0.076). Twenty-nine patients (28.43%) were admitted with unstable angina, 20 (19.61%) with Non-ST Segment Elevation Myocardial Infarction (NSTEMI), and 53 (51.96%) with ST Segment Elevation Myocardial Infarction (STEMI). There were 38 (37.3%) Saudis, 26 (25.5%) Non-Saudi Arabs, 32 (31.4%) from the Indian subcontinent and 6 (5.9%) other patients who were mainly Asians. The age difference between Saudi patients and those from the Indian subcontinent was statistically significant (p<0.0001). Fifty-one (50%) were diabetics, 51 (50%) hypertensive, 65 (63.72%) smokers, 51 (50%) dyslipidemic, 20 (19.61%) had a strong family history of coronary artery disease; 17 (16.66%) were obese (BMI 0f 30 kg/m2 and above according to the WHO classification ), and 16 (15.68%) had a previous history of heart failure.
Table 1.
General characteristics of the study patients
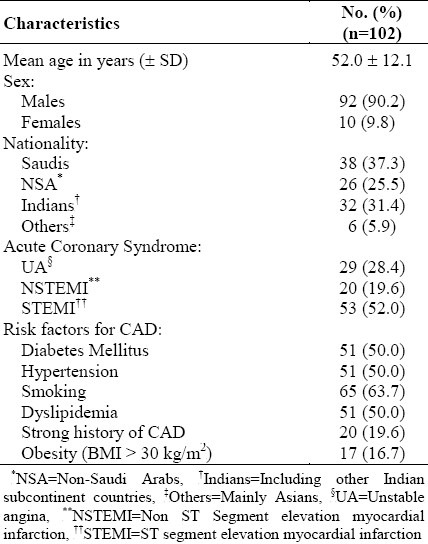
Table 2 shows that the highest mean BDI score was found among the patients from the Indian subcontinent, 16.81 ± 12.70 as compared to Saudis and Non-Saudi Arabs with a borderline significance (p=0.057). The mean BDI scores were not significantly different among patients presenting with the 3 different components of acute coronary syndrome (12.24 ± 7.50 for patients presenting with unstable angina, 14.50±8.42 for patients with NSTEMI and 12.66 ± 12.07 for patients with STEMI).
Table 2.
Mean BDI scores among different nationality subgroups with ACS
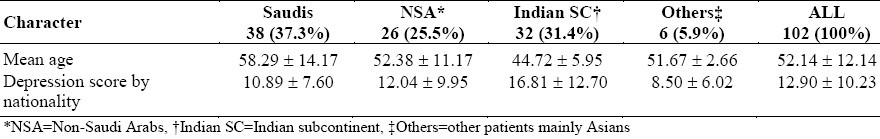
Table 3 shows that evidence of clinical depression was found in 20.6% of all patients, 13.2% of the Saudi patients, 19.2% of the Non-Saudi Arabs, 34.4% of the patients from the Indian subcontinent and none of the other patients. The difference between the Saudi patients and those from the Indian subcontinent was statistically significant (p=0.035).
Table 3.
Prevalence of clinical depressions among patients with ACS
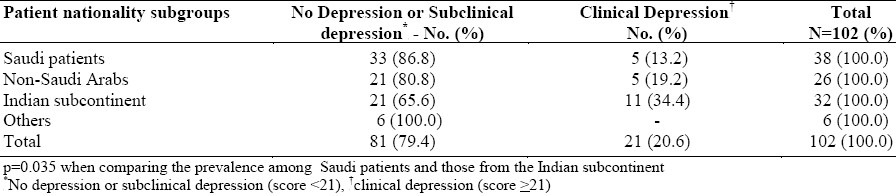
Table 4 illustrates the possible association between traditional risk factors for CAD and depression. Diabetes Mellitus was found to be associated with lower mean BDI score (p=0.018). The presence of hypertension, dyslipidemia, strong family history of coronary artery disease and obesity did not affect the BDI scores. However, smoking was the only risk factor associated with a significantly higher mean BDI score, 15.48 ± 10.85 as compared to 8.38 ± 7.17 in non-smoker (p=0.01). Patients with a previous history of CHF had a lower mean BDI score than patients without a previous history of CHF (p=0.043). Nevertheless, the frequency of clinical depression among smokers was significantly higher than in non-smokers, 26 out of 65 patients(40%) compared with 6 out of 37 patients(16.2%) respectively, p=0.02.
Table 4.
Risk factors as possible predictors of depression
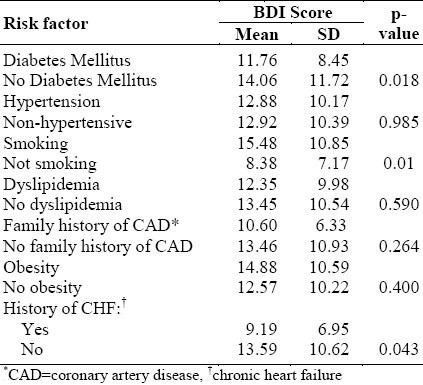
After controlling for the effect of other traditional risk factors (diabetes mellitus, hypertension, and strong family history of CAD) in a logistic regression model, smoking and dyslipidemia remained the most important significant predictors of clinical depression (p=0.0072 and p=0.00342, respectively).
DISCUSSION
After reviewing the literature, it appeared that depression is unquestionably associated with CAD and it is hard not to think of this association in terms of depression as a cause of CAD.2 It appeared also that depression is an independent risk factor for CAD, even several decades after the first episode,3,4,18 and is an independent risk factor for increased post ACS morbidity and mortality.2,6,9,10,14,23 It is important to remember, however, that what has been demonstrated is an association and not causality.2 Unfortunately, post-myocardial infarction depression often goes unrecognized.17 In our study, approximately one in five patients admitted with ACS (20.6%) suffered from symptoms of moderate to severe clinical depression. This agreed quite strongly with other studies (15-23%).2,10,17 The frequency of clinical depression among patients from the Indian subcontinent was significantly higher than in Saudis and non-Saudi Arabs. Furthermore, though patients from the Indian subcontinent had a significantly lower mean age compared to Saudi patients, they had a high frequency rate of clinical depression. Patients from the Indian subcontinent were three and half times more prone to developing clinical depression as compared to Saudi patients. The probable factors responsible for this high frequency are: the lack of family and social support, the relatively low socio-economic status, unsatisfactory accommodation and living conditions, work pressures, and the significant differences in the cultural and social backgrounds.7,15
There is a large body of evidence to suggest that depression may be associated with several pathophysiologic mechanisms including hypothalamic-pituitary axis hyperactivity, autonomic nervous system dysfunction, and increased platelet activity which may explain the increased risk of CAD in a depressed population.20,24 Those pathophysiologic mechanisms, especially increased platelet/ endothelial activity, may be considered as active players in the pathogenesis of coronary atherosclerosis and the early occurrence of CAD in immigrant workers from the Indian subcontinent. However, this hypothesis needs confirmation in a well designed prospective study focusing on immigrant patients from the Indian subcontinent suffering from ACS. Smoking was the only risk factor for CAD which was strongly associated with depression in our study (p=0.01). This finding was similar to those reported by Carney et al, and Glassman et al.10,25 After controlling for the effect of other traditional risk factors, such as diabetes mellitus, hypertension, and strong family history of CAD in a logistic regression model, smoking and dyslipidemia remained the most important significant predictors of depression (p=0.0072 and p=0.0342, respectively). Our findings are supported by those of Kaplan et al26 who reported that the effect of smoking on the degree of carotid atherosclerosis in 1100 middle-aged men was 3.4 times greater in depressed than in non-depressed men; and the effect of LDL cholesterol level on atherosclerosis was nearly doubled. However, the studies which focused on the association between traditional risk factors and depression failed to document such an association.27 Nevertheless, in those studies in which a significant association has been found, depression remained an independent predictor of cardiac morbidity and mortality after controlling those risk factors.3 Our findings may suggest that clinical depression, smoking and dyslipidemia represent a potentially serious confounding cause for CAD, and the post-ACS higher morbidity and mortality.2 However, we are still far short of proof that depression has a causal role in the etiology and pathogenesis of CAD. There remain some unsolved questions concerning the biological mechanisms relating depression to CAD, the causes and the nature of depression preceding the first or recurrent cardiac events and the power of anti-depressive therapeutic programs to reduce the morbidity and mortality of CAD in depressed patients.28 The SADHART Trial opened the door to the hope that treating depression with Selective Serotonin Reuptake Inhibitors may effectively reduce morbidity and mortality in depressed post-ACS patients.19
CONCLUSION
Depression is unquestionably associated with CAD, and is an independent risk factor for post-ACS morbidity and mortality. This is a preliminary prospective study intended to determine the frequency of clinical depression among patients suffering from ACS. The frequency of clinical depression among our patients was 20.6% and was very high among patients from the Indian subcontinent (34.4%). Smoking and dyslipidemia were the only significant predictors of depression in our study. Therefore, we are in accord with the opinion that depression, smoking and dyslipidemia may together be serious confounders of CAD. However, the causative relationship between depression and CAD was beyond the scope of this study. Thus, further controlled studies are needed to elucidate this important problem in this part of the world.
ACKNOWLEDGMENT
I sincerely thank Dr. Ahmed Bahnassy, Associate Professor of Family and Community Medicine, for his valuable help in the statistical analysis; Prof. Hassan B. Abdelhafeiz, Professor of Psychiatry, King Faisal University and King Fahd Hospital of the University (KFHU), for reviewing this manuscript, the nursing staff of Coronary Care Unit, KFHU, especially Ms. Mariamma and Ms. Julia for their support and cooperation; and Mrs. Wilhelmina M. Salalac, Medical Secretary, for her secretarial support.
REFERENCES
- 1.Sadek A. Mind.-Heart Relationship, Handbook. Cairo: Pfizer Middle East (MER); 2002. pp. 11–2. [Google Scholar]
- 2.Glassman AH, Shapiro PA. Depression and the course of coronary artery disease. Am J Psychiatry. 1998;155:4–11. doi: 10.1176/ajp.155.1.4. [DOI] [PubMed] [Google Scholar]
- 3.Anda R, Williamson D, Jones D, Macera C, Eaker E, Glassman A, Marks J. Depressed affect, hopelessness, and the risk of ischemic heart disease in a cohort of US adults. Epidemiology. 1993;4:285–94. doi: 10.1097/00001648-199307000-00003. [DOI] [PubMed] [Google Scholar]
- 4.Ferketich AK, Schwartzbaum JA, Frid DJ, Moeschberger ML the National Health and Nutrition Examination Survey. Depression as an antecedent to heart disease among women and men in the NHANES I study. Arch Intern Med. 2000;160:1261–8. doi: 10.1001/archinte.160.9.1261. [DOI] [PubMed] [Google Scholar]
- 5.Schulz R, Beach SR, Ives DG, Martire LM, Ariyo AA, Kop WJ. Association between depression and mortality in older adults: the Cardiovascular Health Study. Arch Intern Med. 2000;160:1761–8. doi: 10.1001/archinte.160.12.1761. [DOI] [PubMed] [Google Scholar]
- 6.Barefoot JC, Schroll M. Symptoms of depression, acute myocardial infarction, and total mortality in a community sample. Circulation. 1996;93:1976–80. doi: 10.1161/01.cir.93.11.1976. [DOI] [PubMed] [Google Scholar]
- 7.Everson SA, Goldberg DE, Kaplan GA, Cohen RD, Pukkala E, Toumilehto J, Salonen JT. Hopelessness and risk of mortality and incidence of myocardial infarction and cancer. Psychosom Med. 1996;58:113–21. doi: 10.1097/00006842-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 8.Ford DE, Mead LA, Chang PP, Cooper-Patric L, Wang NY, Klag MJ. Depression is a risk factor for coronary artery disease in men: the precursors study. Arch Intern Med. 1998;158:1422–6. doi: 10.1001/archinte.158.13.1422. [DOI] [PubMed] [Google Scholar]
- 9.Carney RM, Rich MW, Freedland KE, Saini J, Tevelde A, Simeone C, Clark K. Major depressive disorder predicts cardiac events in patients with coronary artery disease. Psychosom Med. 1988;50:627–33. doi: 10.1097/00006842-198811000-00009. [DOI] [PubMed] [Google Scholar]
- 10.Carney RM, Freedland KE, Rich MW, Jaffe AS. Depression as a risk factor for cardiac events in established coronary heart disease, a review of possible mechanisms. Am Behav Med. 1995;17:142–9. doi: 10.1007/BF02895063. [DOI] [PubMed] [Google Scholar]
- 11.Frasure-Smith N, Lesperance F, Talajic M. Depression and 18-month prognosis after myocardial infarction. Circulation. 1995;91:999–1005. doi: 10.1161/01.cir.91.4.999. [DOI] [PubMed] [Google Scholar]
- 12.Ladwig KH, Kieser M, Konig J, Breithardt G, Borgrefe M. Affective disorders and survival after acute myocardial infarction: results from the post infarction late potential study. Eur Heart J. 1991;12:959–64. [PubMed] [Google Scholar]
- 13.Lesperance F, Frasure-Smith N, Juneau M, Theroux P. Depression and 1-year prognosis in unstable angina. Arch Intern Med. 2000;160:1354–60. doi: 10.1001/archinte.160.9.1354. [DOI] [PubMed] [Google Scholar]
- 14.Bush DE, Ziegelstein RC, Tayback M, Richter D, Stevens S, Zahalsky H, Fauerbach JA. Even minimal symptoms of depression increase mortality risk after acute myocardial infarction. AM J Cardiol. 2001;88:337–41. doi: 10.1016/s0002-9149(01)01675-7. [DOI] [PubMed] [Google Scholar]
- 15.Welin C, Lappas G, Wilhelmsen L. Independent importance of psychosocial factors for prognosis after myocardial infarction. J Intern Med. 2000;247:629–39. doi: 10.1046/j.1365-2796.2000.00694.x. [DOI] [PubMed] [Google Scholar]
- 16.Musselman DL, Evans DL, Nemeroff CB. The relationship of depression to cardiovascular disease: epidemiology, biology and treatment. Arch Gen Psychiatry. 1998;55(7):580–92. doi: 10.1001/archpsyc.55.7.580. [DOI] [PubMed] [Google Scholar]
- 17.Strik JMH, Honig A, Maes M. Depression and Myocardial Infarction: relationship between heart and mind. Progress in Neuro-Psychopharmacology and Biological Psychiatry. 2001;25(4):879–89. doi: 10.1016/s0278-5846(01)00150-6. [DOI] [PubMed] [Google Scholar]
- 18.Ford DE, Mead LA, Chang PP, Cooper-Patrick L, Wang NY, Klag MJ. Depression is a risk factor for coronary artery disease in men: the Precursor Study. Arch Intern Med. 1998;158(13):1422–6. doi: 10.1001/archinte.158.13.1422. [DOI] [PubMed] [Google Scholar]
- 19.Glassman AH, O’Connor CM, Califf RM, Swedberg K, Schwartz P, Bigger T, et al. Sertraline Treatment of Major Depression in Patients With Acute MI or Unstable Angina. Sertraline AntiDepressant Heart Attack Randomized Trial (SADHART) JAMA. 2002;288:701–9. doi: 10.1001/jama.288.6.701. [DOI] [PubMed] [Google Scholar]
- 20.Serebuary VL, Glassman AH, Malinin AL, Nemroff CB, Musselman DI, van Zyl LT, et al. Platelet/endothelial biomarkers in depressed patients treated with selective Serotonin Reuptake Inhibitor Sertraline after acute coronary event: the Sertraline Anti-Depressant heart Attack Randomized Trial (SADHART) Platelet Substudy. Circulation. 2003;108(8):939–44. doi: 10.1161/01.CIR.0000085163.21752.0A. [DOI] [PubMed] [Google Scholar]
- 21.Beck AT, Steer R, Garbin MG. Psychometric properties of the Beck Depression Inventory: twenty-five years later. Clin Psychol Rev. 1988;8:77–100. [Google Scholar]
- 22.Gatewood-Colwell G, Kaczmarek M, Ames MH. Reliability and Validity of the Beck Depression Inventory for a white and Mexican-American gerontic population. Psychol Rep. 1989;65(3 Pt 2):1163–3. doi: 10.2466/pr0.1989.65.3f.1163. [DOI] [PubMed] [Google Scholar]
- 23.Zeiglstein RC. Depression after myocardial infarction. Cardiol Rev. 2001;9(1):45–51. doi: 10.1097/00045415-200101000-00009. [DOI] [PubMed] [Google Scholar]
- 24.Malhotra S, Tesar GE, Franco K. The relationship between depression and cardiovascular disorders. Curr Psychiatry Rep. 2000;2(3):241–6. doi: 10.1007/s11920-996-0017-z. [DOI] [PubMed] [Google Scholar]
- 25.Glassman Ah, Hezler JE, Covey LS, Cottler LB, Stetner F, Tipp JE, Johnson J. Smoking, smoking cessation, and major depression. JAMA. 1999;264:1546–9. [PubMed] [Google Scholar]
- 26.Kaplan GA, Cohen RD, Wilson TW, Kauhanen J, Salonen R. 32nd Annual Conference on Cardiovascular Epidemiology, American Heart Association. Dallas (TX): American Heart Association Press; 1992. Mar 19-21, Depression amplifies the association between carotid atherosclerosis and age, hypertension, low density lipoprotein, and platelet aggregability. [Google Scholar]
- 27.Frasure-Smith N, Lesperance F, Talajic M. Depression Following Myocardial Infarction: impact on 6 month survival. JAMA. 1993;270:1819–25. [PubMed] [Google Scholar]
- 28.Appels A. Depression and coronary artery disease: Observations and Questions. J Psychosm Res. 1997;43(5):443–52. doi: 10.1016/s0022-3999(97)00158-x. [DOI] [PubMed] [Google Scholar]


