Abstract
Objective:
The objective of this study was to identify the patterns of prescribing for Acute respiratory infections in patients attending primary health care centers in the Aseer region, southwestern Saudi Arabia.
Materials & Methods:
This study was conducted at primary health care centers in the Aseer region during November 2003. A master sheet designed by the investigator was distributed to all the working physicians in the primary health care center in the Aseer region. The master sheet included the age, sex, complaints, signs, clinical diagnosis and the type of medications prescribed. Physicians were asked to include all patients attending on 17th November 2003, and send the master sheet to the Technical Supervision Unit at Primary Care Department, General Directorate of Health Affairs. Data of the master sheet was entered and analyzed by using SPSS.
Results:
The total number of patients attending with acute respiratory infections(ARIs) was 3000 which represented 25% of the patients attending primary health care centers that day. Children formed 60% of the total number of cases. Regarding symptoms and signs, it was found that 70% had a cough, 59% had a runny nose, and 43% had a sore throat . The common cold was the most common diagnosis (42%). Antipyretics, antihistamines, antibiotics and antitussives were prescribed for 78%, 48%, 45% and 25% respectively. Statistical analysis using logistic regression revealed that the higher the temperature, the more severe the throat congestion and the presence of exudates on pharynx, the higher the likelihood to prescribe antibiotics.
Conclusion:
In this study, it was found that the prescription of all drugs for ARIs was still high in spite of the fact that these conditions are self-limiting. To rationalize prescribing for ARI, implementation of the national protocol for diagnosis and treatment of ARIs is mandatory. Further studies to explore the physician's knowledge, attitudes and behavior concerning prescribing for ARI is strongly recommended.
Keywords: Prescribing, Acute Respiratory Infections, Primary health care centers
INTRODUCTION
Acute respiratory infections (ARIs) form one of the most common reasons for visits to the primary care physician.1 The causes for ARIs range from self limiting conditions such as the common cold to the more serious bacterial pneumonia.2 Whilst the majority of cases are viral, three-quarters of antibiotics consumed is for ARIs, which has contributed to the emergence of drug-resistant bacterial pathogens, serious side-effects and waste of health care resources.3 A large proportion of medications prescribed are unlikely to provide any clinical benefits to patients.4 However, there is tremendous pressure on doctors from patients and parents to prescribe medications regardless of diagnoses.5 Over-prescribing of antibiotics for ARIs is widespread globally, accross medical specialties and payment sources.4 The majority of antibiotics prescribed in ambulatory practice in the United States are for acute sinusitis, acute pharyngitis, and nonspecific upper respiratory tract infections (URI).6 In the United States, office visit for colds, URIs and bronchitis results in 40 million antibiotic prescriptions, accounting for 55% of all antibiotic prescriptions, at a cost of $ 726 million.7 In adults, the antibiotics prescribing rates for cold, URIs, and acute bronchitis are as high as 61%,63%, and 72%,respectively. While in children under 18 years, antibiotics were prescribed to 44% of the patients with common cold, 46% with URIs and 75% with bronchitis.8 In Canada, France, Germany, Italy, Spain and the UK, prescribing of antibiotics ranges from 32% to 74%.9
In Saudi Arabia, ARI was found to be the most common diagnostic label used in more than half of the prescriptions; antibiotics were prescribed for 53%, anti-cough for 43% and anti- histamine for 20% of patients with ARIs.10 In this context, optimizing therapy for ARIs is an appropriate area for action. Health care providers in Saudi Arabia have become aware of the problem of prescribing for ARIs and to solve this problem among children, “the national protocol for diagnosis and treatment of acute respiratory infections among children in health care centers and small hospitals” has been developed.11 However, to the best of our knowledge few studies exist on prescribing for ARIs in Saudi Arabia. The aim of this study is to describe the patterns of prescribing of antibiotics and other drugs in the treatment of ARIs by Primary Health Care Physicians in the Aseer Region, Saudi Arabia.
MATERIALS AND METHODS
Aseer is one of the biggest administrative regions in Saudi Arabia, with a total population of 1.2 million. The health services are provided through 220 PHCCs and 16 hospitals. For smooth running of the health services, the Aseer region is divided into 16 health sectors. Each sector consists of a general hospital and numbers of PHCCs.
This cross-sectional study was conducted in November 2003 in Primary Health Care Centers in the Aseer region, southwestern Saudi Arabia. In order to achieve the study's objective, a master sheet was designed by the investigators. The master sheet included the age, sex, symptoms, signs, clinical diagnosis and prescribed medications for the patients (Appendix 1).
Appendix 1.
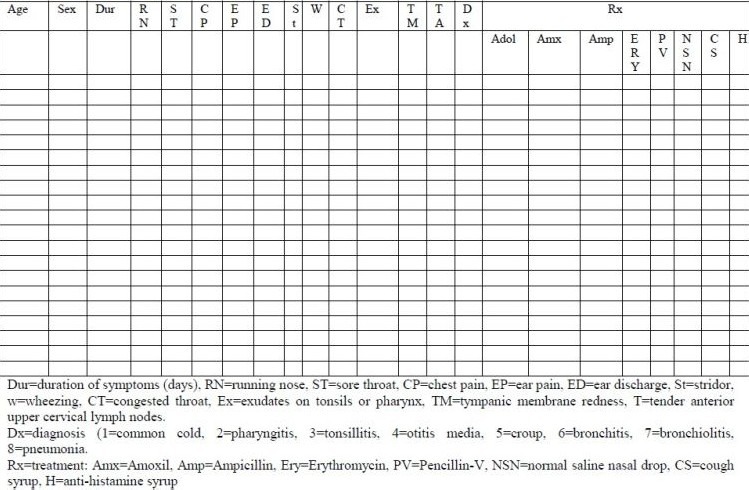
Master sheet for ARI management at PHCC level in Aseer region, KSA
The master sheet was formally sent by mail to all the technical supervisors (who are trained physicians responsible for supervising the activities of primary health care in the health sectors).They were instructed to explain and distribute the master sheets to the working physicians in all PHCC in each sector. Instructions were that any patient presenting with symptoms of acute respiratory infection on Monday, 17th November 2003 should be entered on this master sheet by the treating physicians. The next day, all the master sheets were collected and sent to the Technical Supervision Unit(TSU) in the Primary Care Department, General Directorate of Health Affairs.
Data of the master sheet was entered and analyzed using SPSS. Appropriate tests were used accordingly and P value was considered significant if it was < 0.05.
RESULTS
The total number of patients seen (Table 1) was 3000 patients which represented 25 % of the total population attending during that day. About 50% of children were under the age of 5 years, of whom were male 55%. The main complaints were cough (70%), runny nose (57%), and sore throat (43%). The main signs were congested throat (41%), fever (9%). Exudate on tonsils or throat (8%), and tender anterior cervical lymph nodes (7%). The main diagnoses were common cold (42%), pharyngitis (25%), and tonsillitis (17%).
Table 1.
Profile of patients attended to PHCCs with acute respiratory infections, Aseer Region, KSA, 2003
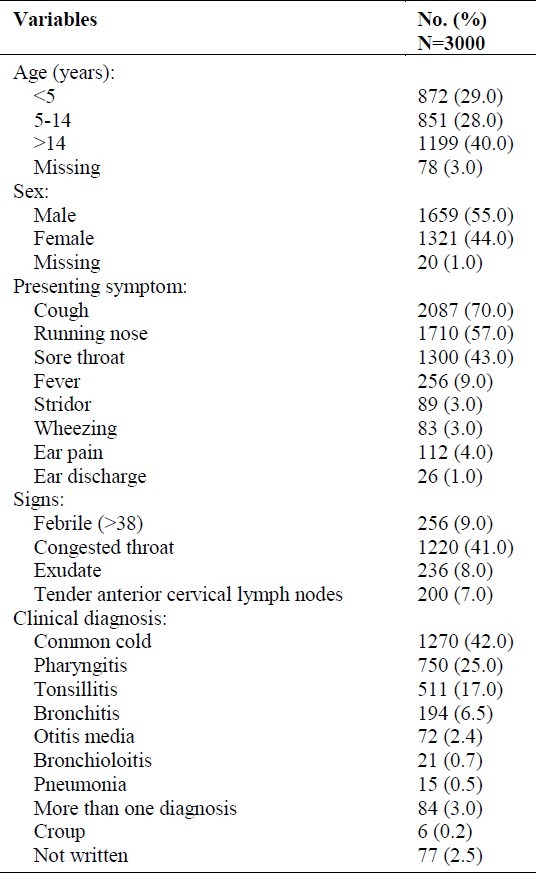
Table 2 shows the pattern of prescribing for acute respiratory infection. Paracetamol was the most common drug prescribed (78%) followed by Antihistamine (47%), antibiotics (45%), and cough syrups (24%) respectively.
Table 2.
Patterns of prescribing for ARI according to clinical diagnosis at PHCC, Aseer Region, KSA, 2003
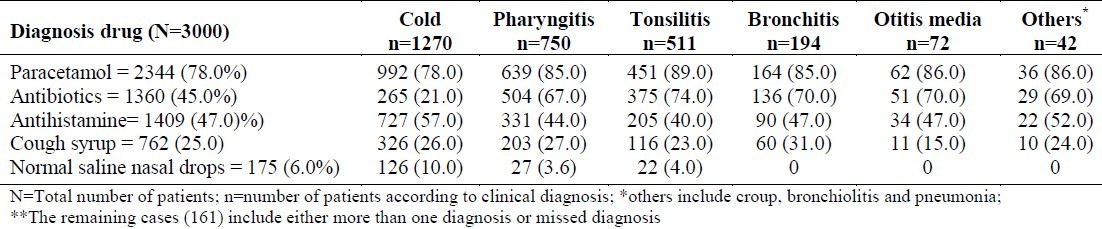
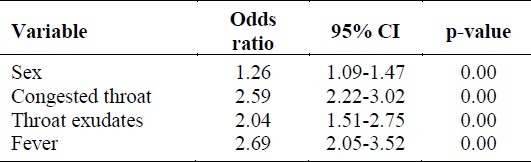
Table 3 shows the most common variables that determined the prescribing of antibiotics. The higher the fever the more likely there was of antibiotics prescribing. There was no significant difference of age. Females were prescribed antibiotics more than males. When using the logistic regression, antibiotic prescribing was the dependent variable with sex, fever, congested throat, exudation and anterior cervical lymph nodes enlargement as the independent variables. Fever, congested throat and exudates and sex were the significant predictors for antibiotics prescribing
Table 3.
Determinants of antiobiotic prescribing for sore throat among patients attended PHCC, Aseer region, KSA, 2003
DISCUSSION
This cross-sectional one day study may not represent the whole prescribing pattern of doctors for respiratory tract infections (RTI). However, the fact that 3000 prescriptions were issued by physicians in 220 PHCCs in the Aseer region provides a good picture of the prescribing pattern in this region.
The most commonly presenting group in this study was under 15-year-olds which seems natural, as this age group forms approximately 50% of Saudi population.12 Most of the infections in this age group were viral in origin. The proportion of females with ARIs in this study was only 55% (unlike other Saudi studies).13 However, a larger proportion of them were given antibiotics.
The most commonly presenting complaints in this study were cough and runny nose. It was shown in some studies that 20-30% of patients with rhinovirus infections would continue to cough for more than 2 weeks.5 A large proportion of patients had congested throat which is mainly a non-specific sign but in a minority of cases could indicate a bacterial cause.
In this study, the most common diagnosis was the common cold (42%). The predominance of this acute self-limiting diagnosis indicates a real need for the promotion of health education for patients on the modification of their behaviour to seek help. Self care and when to utilize the health care system should be emphasized as a part of the education.
Antipyretics (Paracetamol) was the most frequently prescribed medication (78%) in this study even though fever, sore throat and ear pain were found in only 55% of the patients. This pattern of prescribing could be due to the fact that doctors think that the patients may need paracetamol in the course of their illness in spite of the initial clinical features. Antihistamines was the second in rank; and the prescribing of cough syrups was also high. Prescribing of both antihistamines and cough syrups is not supported by the literature14 and their prescribing may even be harmful especially to patients under 5 years for whom paradoxically it is the most often prescribed. Antibiotics were prescribed in 45 % of patients with ARIs. There is evidence that the community, as well as patients would benefit if unnecessary use of antibiotics can be minimized. In Japan, the resistance of group A streptococcal isolates to erythromycin, which was 62% in 1974, fell to less than 2% in 1988 when macrolides use was reduced from 22% of all antibiotics prescribed to only 8%.15 Indiscriminate use of antibiotics should be discouraged and reserved for patients with group A streptococcal pharyngitis and for patients with identified bacterial complications such as otitis media, pneumonia or sinusitis.16
There have been many forms of interventions aimed at changing physicians’ prescribing behavior. These have included audit studies, group discussion and feedback, introduction of general practice drug formulary or hospital formulary,17 guidelines for antibiotics and Non-Steroidal Anti-inflammatory Drugs.18 Information of rational prescribing should be promoted and circulated at national and local medical meetings and the input from local practitioners should be considered. There is a need to increase doctors’ awareness of the lack of proven benefits and the definite high cost and side effects of many prescriptions for self-limiting illness.
Now, is the time to implement the Saudi national protocol for the diagnosis and treatment of ARIs to improve case-management, train staff and promote community awareness. Khoja et al11 have pointed out that the implementation of ARTI protocol has resulted in the reduction of prescribing different medications. The implementation of ARI control programs elsewhere, such as in Pakistan, has resulted in a significant reduction in the prescribing of antibiotics and in fatality rates of ARI cases in children.5
In conclusion, this study has clarified the prescribing pattern for ARI in a section of the Saudi population. Prescribing antibiotics and other medications for ARI is still high and needs rationalization. Training on and implementation of the Saudi national protocol for diagnosis and treatment of ARI in children is mandatory to improve the prescribing for ARI . Similar protocol for the management of ARI among adults is suggested. Further studies to explore the knowledge, skills and attitudes of primary health care physicians towards prescribing for ARI are needed.19
REFERENCES
- 1.Anonymous. Acute respiratory infections: the forgotten pandemic. Communiqué from the international Conference on Acute Respiratory Infections, Canerra, Australia 7-10 July, 1997. International Journal of Tuberculosis and Lung Disease. 1998;2:2–4. [PubMed] [Google Scholar]
- 2.Gonzales R, Steiner JF, Sande MA. Antibiotic prescribing for adults with colds, upper respiratory tract infections, and bronchitis by ambulatory care physicians. JAMA. 1997;5:79–83. [PubMed] [Google Scholar]
- 3.Stone S, Gonzales R, Maselli J, Lowenstein SR. Antibiotics prescribing for patients with colds, upper respiratory infections, and bronchitis: A national study of hospital – based emergency departments. Ann Emerg Med. 2000;36:320–7. doi: 10.1067/mem.2000.109341. [DOI] [PubMed] [Google Scholar]
- 4.Campbell H. Acute respiratory infections: a global challenge .Arch Dis. Child. 1995;73:281–3. doi: 10.1136/adc.73.4.281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Orr PH, Scherer K, MacDonald A, et al. Randomized placebo-controlled trials of antibiotics for acute bronchitis: A critical review of the literature. J Fam Pract. 1993;36:507. [PubMed] [Google Scholar]
- 6.Gonzales R, Bartlett JG, Besser RE, Cooper RJ, Hicker JM, Hffman JR, Sande MA. Principles of Appropriate Antibiotics Use for Treatment of Acute Respiratory Tract Infections in Adults: Background, Specific Aims, and Methods. Ann Intern Med. 2001;134:479–86. doi: 10.7326/0003-4819-134-6-200103200-00013. [DOI] [PubMed] [Google Scholar]
- 7.Gonzales R, Malone DC, Maselli JH, Sande MA. Excessive antibiotic use for acute respiratory infections in the United States. Clin Infect Dis. 2001;33:757–62. doi: 10.1086/322627. [DOI] [PubMed] [Google Scholar]
- 8.Mainous AG, 3rd, Hueston WJ, Davis MP, Pearson WS. Trends in antimicrobial prescribing and upper respiratory infections among adults and children. Am J Public Health. 2003;93:1910–4. doi: 10.2105/ajph.93.11.1910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Huchon GJ, Gialdroni-Grassi G, Leophonte P, Manresa F, Schaberg T, Woodhead M. Initial antibiotics therapy for lower respiratory tract infection in the community: a European survey. Eur Respir J. 1996;9:1590–5. doi: 10.1183/09031936.96.09081590. [DOI] [PubMed] [Google Scholar]
- 10.Al-Khaldi YM, Al-Sharif AI, Al-Gelban KS, Al –Hammami QM, Al-Jaser AO. Impact of National Protocol on Management of Acute Respiratory Infections in Children. Saudi Med J. 2001;22:780–3. [PubMed] [Google Scholar]
- 11.Khoja TA, Ahmed K, AL-Hawas M, Al–Korashi M. National Protocol for Diagnosis and Treatment of acute Respiratory Infections Among Children in Health Centers and small Hospitals. 1st edition. Riyadh: Ministry of Health, Saudi Arabia; 1997. [Google Scholar]
- 12.Khoja TA, Farid SM. Saudi Arabia Family health Survey 1996: Principal Report. Riyadh: Ministry of Health 2000; 2000. [Google Scholar]
- 13.Bawazir S. Prescribing patterns of ambulatory care physicians in Saudi Arabia. Ann Saudi Med. 1993;13:172–7. doi: 10.5144/0256-4947.1993.172. [DOI] [PubMed] [Google Scholar]
- 14.Benenson AS, editor. Control of communicable diseases manual. An official report of the American Public Health Association. 16th ed. Washington DC: American Public Health Association; 1995. pp. 395–400. [Google Scholar]
- 15.Harding J, Modell M, Freudenbury S, et al. Prescribing: the power to set limits. BMJ. 1985;290:450–3. doi: 10.1136/bmj.290.6466.450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Turner RB, Sperber SJ, Sorrentino JV, et al. Effectiveness of clemastine fumarate for treatment of rhinorrhea and sneezing associated with the common cold. Clin Infect Dis. 1997;25:824–30. doi: 10.1086/515546. [DOI] [PubMed] [Google Scholar]
- 17.Beardon PHG, Brown SV, Mowat DAE, et al. Introducing a drug formulary to general practice - effects on practice prescribing cost. J R Coll Gen Pract. 1987;37:305–7. [PMC free article] [PubMed] [Google Scholar]
- 18.Feely J, Chan R, Cooman L, et al. Hospital formularies: need for continuous intervention. BMJ. 1990;300:28–9. doi: 10.1136/bmj.300.6716.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Orr PH, Scherer K, Macdonald A, Moffatt MEK. Randomized placebo-controlled trials of antibiotics for acute bronchitis: a critical review of the literature. J Fam Pract. 1993;36:507–12. [PubMed] [Google Scholar]


