Abstract
Objective:
Fibroadenoma is one of the commonest benign breast lesions in our outpatient clinics. Giant Juvenile fibroadenoma (GJF) characterized with their alarming rapid growth and gross disfigurement is less frequently identified.
Materials and Methods:
A 14-year review (1990-2004) of all fibroadenomas presented to the Outpatient Department was undertaken. Demographic data, duration of symptoms, size at presentation, the use of radiological, cytological and histo-pathological modalities, surgical excision and follow up were all noted. Eight-Hundred-Sixty-Four cases were diagnosed as fibroadenoma by both clinical and radiological examinations and confirmed by FNAC. Patients with fibroadenomas <2 cm in size were followed up regularly in the out patients department, while those >2 cm underwent surgical excision. GJF were defined as those with >5 cm in diameter.
Results:
The total number of excised fibroadenomas was 202 (23%), while the remaining662 (77%) fell into the follow up category. GJF were diagnosed in 9 patients accounting for 4.5% of all excised fibroadenomas. Age ranged between 14-23 years.
Conclusion:
However benign these lesions may appear, in view of the history of a sudden rapid breast enlargement as demonstrated in nearly all the clinical presentations, surgical excision remains the mainstay of treatment of such lesions in order to allow the previously compressed normal surrounding breast tissue to expand and retain its normal function and cosmetic appearance. The use of radiological modalities such as ultrasound and MRI may aid the diagnosis, limiting mammography to the older age group
Keywords: Juvenile fibroadenoma, breast
INTRODUCTION
Benign breast diseases fortunately comprise a large proportion of breast complaints presenting to our Outpatient Department. Fibroadenomas, commonly found by palpation or by radiological modalities, account for approximately 20% of open surgical breast excisions.1 They contain the same components as normal breast tissue, therefore, are expected to enlarge during pregnancy and regress at menopause in response to hormonal changes. The natural history of fibroadenoma is variable. Most stop growing at 2-3cm in diameter.1,2 Malignancy within fibroadenomas is rare. However, since it is possible, they should be sought and treated as malignant breast lesions arising independently.3
Giant juvenile fibroadenoma (GJF) are less frequently encountered, reported figures accounting for about 5% of all breast tumors. They are characterized by their predilection to young females in their teens or early 20s. Their rapid growth raises the suspicion of possible malignancy. Nonetheless, they do not become malignant, though often unsightly and disconcerting to the patient.2
MATERIAL AND METHODS
This 14-year study was undertaken at King Fahd Hospital of the University, Al Khobar, Eastern Province of Kingdom of Saudi Arabia from 1990 to 2004. All patients diagnosed with fibroadenomas who presented to the Outpatient Department were reviewed. Demographic data, duration of symptoms, size at presentation, the use of radiological and cytological modalities and operative records were included.
All patients underwent triple assessment in the form of clinical examination, radiological assessment using ultrasonography, unilateral single view mammography (in two patients) and MRI confirmed by FNAC.
Patients presenting with < 2cm lumps in diameter were given the option of regular follow up rather than excision. All patients presenting with lumps >2 cm in diameter were subjected to surgical excision. Lesions > 5cm in size were considered GJF and were totally excised through a circum-areolar or inframammary incisions. Cavities were not obliterated, no drains were used and meticulous care was taken to preserve the shape of the breast.
RESULTS
The total number of diagnosed fibroadenomas was 864. Of that number, those which underwent excision were 202(23%). GJF were reported in 9 (4.5%) of patients whose ages ranged between 19-23yrs. The common presenting symptom was a history of a rapidly growing painless breast mass within a duration of 4-9 months, characterized by marked breast asymmetry, stretched overlying skin and dilated superficial veins. The average size ranged between 8-14 cm in diameter.
Ultrasonography confirmed the diagnosis of the presence of a large hypoechoic mass surrounded by compressed breast parenchyma, yet failed to distinguish accurately between the lesion and the active breast tissue. A single view unilateral mammogram was used in two young teenage patients which confirmed the expectation that it was useless and ill recommended.
MRI accurately delineated the well encapsulated lesion, its characteristics and outline and also demonstrated the compressed breast tissue (Figures 1a and 1b). FNAC showed a hypercellular aspirate containing predominantly stromal cells with no atypia.
Figure 1a.

MRI of a 15 year-old female, using a T1 weighted image demonstrating a mixed iso-intense/low signal of a large mass occupying the upper half of the breast with well demarcated outline and compressed normal intermediate signal breast tissue.
Figure 1b.

MRI using a T2 weighted image demonstrating the mass with high signal intensity occupying the anterior part of the breast surrounded by compressed breast tissue. Left breast appeared normal. (same patient)
At excision, the gross appearance showed a well encapsulated thin-walled lobulated mass 8×9 cm in diameter (Figure 2). Histopathology confirmed the diagnosis by its characteristic appearance of the intracanilicular and pericanilicular growth patterns, dilated spaces, leaf-like projections, epithelial hyperplasia and lack of stromal condensation (Figures 3a and 3b). There was no reported recurrence in any of the patients after six years of follow-up.
Figure 2.

The excised 8×11cm lobulated, thin capsule, soft mass.
Figure 3a.
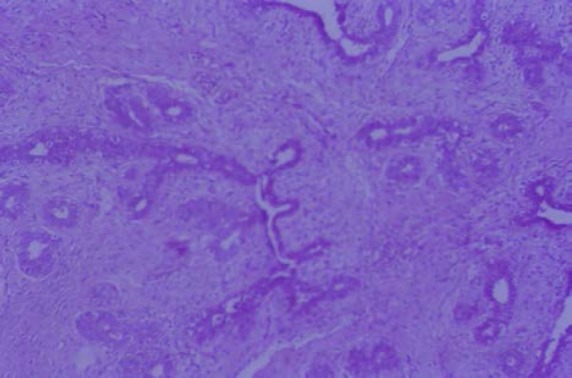
Sections of the previously shown breast mass demonstrating proliferating glands and stroma with intracanalicular and pericanalicular patterns of growth, dilated spaces and leaf like projection. Glands show focal apocrine metaplasia and mild focal epithelial hyperplasia.
Figure 3b.
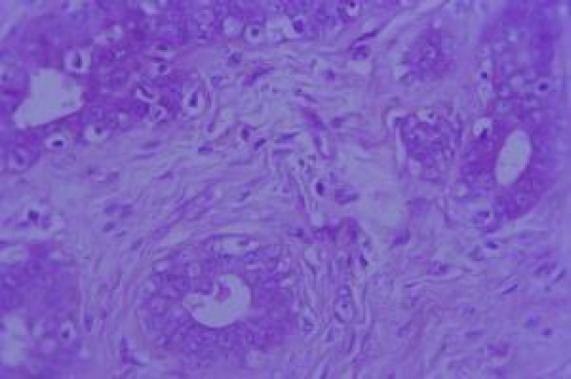
High power demonstrating the above findings
DISCUSSION
Fibroadenomas are considered an abnormality of normal development and involution which under certain circumstances can be observed without surgical intervention. However, excision may be required if the mass enlarges to more than 2cm in size, since it leads to cause anxiety or compromise cosmetic appearance.1
GJF are less frequently identified, with reported figures around 5% of all breast tumors. These lesions are typically solitary and by definition are larger than 5 cm in size or weigh 500 grams.4 They are characterized by their predilection to young females in their teens or early 20s. Their rapid growth raises the suspicion of the possibility of malignancy. Nonetheless, they do not become malignant, though often unsightly and disconcerting to the patient.2 Occasionally, due to their rapid enlargement they can cause the skin to ulcerate, although the skin is not adherent to the tumor.5
Cystosarcoma phyllodes is one of the differential diagnoses of Giant juvenile fibroadenoma. Phyllodes tumor generally mimics fibroadenoma in both its clinical presentation and cytological diagnosis. It has been reported to occur in ectopic breast tissue commonly in the axillary region and more rarely, the vulva and the inguinal regions.6
Preoperative diagnosis can be difficult, and in some instances almost impossible to diagnose on the frozen section. Occasionally, even on permanent sections, the two conditions may be difficult to differentiate. The diagnosis of Cystosarcoma phyllodes can be mainly based on increased stromal cellularity, pleomorphisim, and the presence of mitotic figures.7 Occasionally, Phyllodes tumors present with bloody nipple discharge which is attributed to extensive areas of hemorrhagic necrosis.7,8 Juvenile gigantomastia can be another differential diagnosis of juvenile fibroadenoma. This is characterized by estrogen receptor positive and its hypersensitivity to estrogen.9
In contrast, a variety of benign breast lesions can occur in prepubertal female children. In a reported series of thirty seven cases of benign breast lesions, with ages ranging between 7.5-11.5years, fibroadenoma was the commonest, accounting for 22 (59.5%), juvenile fibaroadenoma 9 (24.2%) virginal hypertrophy 3 (8.1%) and one case of cystosarcoma phyllodes 1(2.7%), duct papilloma 1 (2.7%) and tuberculosis 1 (2.7%).10
Breast carcinoma is quite rare under the age of 20 years. Invasive ductal carcinoma, secretory carcinomas, and invasive lobular-type carcinoma have sporadically been reported.4,11 Like breast cancer, fibroadenomas have both progesterone and estrogen receptors and are therefore, expected to at least rely partly on these hormones to grow. Exogenous estrogen therapy has also been incriminated in the development of fibroadenomas as described in a case of a complete androgen insensitivity syndrome XY karotype (CAIS) who received exogenous estrogen as replacement therapy to after orchidectomy.2 Multiple Juvenile fibroadenomas require careful management because of the risk of recurrence after local excision.12 Some authors are of the opinion that a security zone of mammary parenchyma is mandatory.13
Mammograms are generally not helpful and are not recommended for this age group. Ultrasound evaluation usually shows diffuse glandular process that may or may not be distinct from the surrounding breast tissue. Thus radiographically, these modalities cannot distinguish juvenile fibroadenoma from cystosarcoma phyllodes.14 MRI is currently playing a major role in accurately delineating additional lesions not demonstrated by conventional modalities.15 though in our cases it played an important role in accurately delineating the lesion.
Many non-surgical excisions have been attempted by invasive radiologist. The use of cryoablation for cytologically proven fibroadenomas have played a role in size reduction or total elimination of lesions with minimal scarring and patient satisfaction.1 However, this method is slow (3-12 months) and tedious for the anxious patient. Recently, the FDA approved treatment of fibroadenomas with ultrasonic guided vacuum-assisted biopsy has added a new option for the non-surgical approach. It has been suggested for lesions of <2cm in diameter. However, it has not been completely successful in the total excision of lesions >2cm in diameter. Consequently, some patients have had to undergo conventional surgical excision.16
With the advent of minimally invasive surgery, endoscopic resection of benign breast tumors and axillary dissection have gained some popularity in recent years. Both methods of using the anterior adipose tissue or retromammary space have been equally reported. This approach provides superior cosmetic results with high levels of patient satisfaction. However, the mean duration of the surgery is 79 minutes with a mean hospital stay of 3.5 days as compared the conventional day- surgery procedure of the classical excision.17,18
This current study has shown that in all these teenage patients, clinical features suggested a benign breast lesion, despite the speed of the growing mass. Ultrasonography confirmed the diagnosis of the presence of a large hypoechoic mass surrounded by compressed breast parenchyma but failed to show details of the margins. Mammography performed in two patients was not helpful in aiding the diagnosis owing to the natural increased density of the young breasts and so is not recommended for this age group. MRI on the other hand, was more accurate in delineating the features and the extent of the lesions. FNAC and histopathology confirmed the diagnosis of GJF.
Since Giant juvenile fibroadenoma is a condition of young females, surgical excision remains as the main treatment. Therefore, meticulous care must be taken to attain the best cosmetic results without compromising the breast function or management outcome. The surgical approach should be determined by the surgeons’ preference and skills.
REFERENCES
- 1.Kaufman CS, Bachman B, lttrup PJ, White M, Carolin KA, Freman-Gibb L, et al. Office based ultrasound-guided cryoablation of the breast fibroadenomas. Am J Surg. 2002;184:394–400. doi: 10.1016/s0002-9610(02)01010-3. [DOI] [PubMed] [Google Scholar]
- 2.Davis SE, Wallace AM. A 19-year-old with complete androgen insensitivity syndrome and Juvenile fibroadenoma of the breast. Breast J. 2001;7(6):430–3. doi: 10.1046/j.1524-4741.2001.07610.x. [DOI] [PubMed] [Google Scholar]
- 3.Stafyla V, Kotsifopulos N, Grigoriades K, Kassaras G, Sakorafas G. Lobular carcinoma in situ of the breast within a fibroadenoma, case report. Gynecol Oncol. 2004;94(2):572–4. doi: 10.1016/j.ygyno.2004.04.031. [DOI] [PubMed] [Google Scholar]
- 4.Musio F, Mozingo D, Otchy DP. Multiple giant fibroadenoma. Am Surg. 1991;57:438–4. [PubMed] [Google Scholar]
- 5.Namiar R, Kutty K. Giant Fibroadenoma (cystosarcoma phyllodes) in adolescent females- a clinicopathological study. Br J Surg. 1974;61:261–9. doi: 10.1002/bjs.1800610210. [DOI] [PubMed] [Google Scholar]
- 6.Oshida K, Miyauchi M, Yamamoto N, Takeuchi T, Suzuki M, Nagashima T, et al. Pyllodes tumor arising in ectopic breast tissue of the axilla. Breast Cancer. 2003;10(1):8284. doi: 10.1007/BF02967630. [DOI] [PubMed] [Google Scholar]
- 7.Briggs RM, Walters M, Rosenthal D. Cystosarcoma phyllodes in adolescent female patients. Am J Surg. 1983;146:712–4. doi: 10.1016/0002-9610(83)90324-0. [DOI] [PubMed] [Google Scholar]
- 8.Tagaya N, Kogure H, Shmizu K. A case of Phyllodes tumor with bloody nipple discharge in Juvenile patient. Breast Cancer. 1999;6(3):207–10. doi: 10.1007/BF02967169. [DOI] [PubMed] [Google Scholar]
- 9.Morimoto T, Komaki K, Mori T, Sasa M, Miki H, Inoue H, et al. Juvenile gigantomastia: report of a case. Surg Today. 1993;23(3):260–4. doi: 10.1007/BF00309238. [DOI] [PubMed] [Google Scholar]
- 10.Inder M, Vaishnav K, Mathur DR. Benign breast lesions in prepubertal female children – A study of 20 years. J Indian Med Assoc. 2001;99(11):619–20. [PubMed] [Google Scholar]
- 11.Rivera-hueto F, Hevia-Vazquez A, Utrilla-Alcolea JC, Galera-Davidson H. Long term prognosis of teenagers with breast cancer. Int J Surg Pathol. 2002;10(4):273–9. doi: 10.1177/106689690201000405. [DOI] [PubMed] [Google Scholar]
- 12.Dike AM, Oberman HA. Juvenile (cellular) adenofibromas. A clinicopathological study. Am J Pathol. 1985;9:730–6. doi: 10.1097/00000478-198510000-00004. [DOI] [PubMed] [Google Scholar]
- 13.Remadi S, Ismail A, Karpuz V, Zacharie S, Vassilakos P. Cellular (juvenile) Fibroadenoma of the breast. A clinico-pathologic and immunohistochemical study of 7 cases. Ann Pathol. 1994;14(6):392–7. [PubMed] [Google Scholar]
- 14.Simmons R, Cance W, Lacicca M. A giant juvenile fibroadenoma in a 12-year-old girl: A case report for breast conservation. The Breast Journal. 2000;6(6):418–20. doi: 10.1046/j.1524-4741.2000.98049.x. [DOI] [PubMed] [Google Scholar]
- 15.Diekmann F, Diekmann S, Beljavskaja M, Bick U, Taupitz M, Blohmer JU, et al. Preoperative MRT of the breast in invasive lobular carcinoma comparison with invasive ductal carcinoma. Rofo. 2004;176(4):544–49. doi: 10.1055/s-2004-813011. [DOI] [PubMed] [Google Scholar]
- 16.Sperber F, Blank A, Metser U, Flusser G, Klausner JM, Lev-chlouche D. Diagnosis and treatment of breast fibroadenoma by ultrosongraphic guided vacuum-assisted biopsy. Arch Surg. 2003;38(7):796–800. doi: 10.1001/archsurg.138.7.796. [DOI] [PubMed] [Google Scholar]
- 17.Kitamura K, Hashizume M, Kataoka A, et al. Trans axillary approach for endoscopic extirpation of benign brest tumors. Surg Laparosc Endosc. 1998;8:277–9. [PubMed] [Google Scholar]
- 18.Takayuki O, Zenro N, Wataru I, Kenichi S. Endoscopic resection of benign breast tumors. Retromammary space approach. Surg Laprosc Endosc. 2002;12:100–3. doi: 10.1097/00129689-200204000-00005. [DOI] [PubMed] [Google Scholar]


