Abstract
The main objective of the medical curriculum is to provide medical students with knowledge, skills and attitudes required for their practice. A decade ago, the UK Medical Council issued a report called “Tomorrow's Doctors”1 which called for the reduction in the factual content of the medical course with the promotion of problem-based and self-dedicated learning. This report was the basis for a move toward an extensive reform of the medical and nursing curricula. The new reformed curricula enhanced the integrated medical teaching and emphasized the teaching and learning of clinical skills. However, there were still concerns about the standards and appropriateness of the skills of new medical graduates.2
The changes in the teaching and learning methods, the radical changes in the health care delivery and the rapid growth of technology challenged the traditional way of clinical skills development and led to the emergence of clinical skills laboratories (CSLs) in the medical education of many medical and nursing schools. With the proliferation of the CSLs, it is important to evaluate and introduce the reader to their applications, bearing in mind the paucity of information on this subject particularly over the last couple of years. This article is based on literature review.
Keywords: Clinical, Skills, Laboratories, Centers, Units
INTRODUCTION
Clinical skills laboratories are educational facilities that have the potential benefit for undergraduate and postgraduate medical students and medical staff. They provide a safe and protected environment in which the learner can practise clinical skills before using them in real clinical settings. These skills laboratories help to ensure that all students acquire the necessary techniques and are properly assessed before practising on real patients. In addition, they support the acquisition, maintenance and enhancement of the clinical skills of students in the healthcare profession. The term ‘clinical skills’ involves history-taking, physical examination, clinical investigations, using diagnostic reasoning, procedural perfection, effective communication, team work and professionalism.3–5
Medical schools and postgraduate centers have gone to considerable lengths to create educational facilities dedicated to the teaching of clinical skills. The first CSL was established in Maastrich, The Netherlands Limburg University 1976.6 Since then many medical schools and educational institutions have integrated CSLs into their curricula. Currently, CSLs are established in several innovative medical schools including the University of Leeds, Dundee, Dublin, Southampton, Liverpool, and the Imperial College.3,7–9 In the Arab world, the United Arab Emirates University was the first to establish CSL in 1988.10 At present, there are many universities in the region using CSLs as a teaching tool.
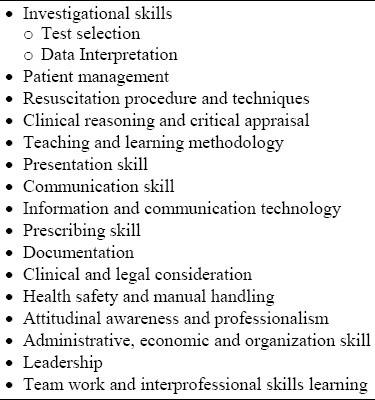
Most CSLs have core clinical skills that can be taught and learned. These include history taking with communication skills, physical examination and some technical and practical procedures. In general, the exact nature of the skill taught is usually determined by the local logistical and educational requirements. With advances in technology and the changes in teaching methodology, the list of skills that can be taught and learned in the CSLs has grown longer (Table 1).4 Because of the variety of these skills, it is important to define them and determine the level of competence required at each institution. For that reason, many CSLs involve curriculum development committees, undergraduate and postgraduate faculty members in the planning process.
Table 1.
Skills that can be taught and learned in the CSLs
SETTING
In setting up a clinical skill facility, it is important to follow the modern educational theory in the development and delivery of the program. The development of communication skills is a crucial area of focus for CSLs. In fact, a better name for those laboratories would be clinical and communication skills centers or units, because the proper application of clinical skills requires the integration of technical clinical skills and those of communication.11
Educational strategies that can be adapted in CSLs include student-centered, integrated, problem-based and self-directed learning as well as multi-profession, community-oriented or outcome-based education.12 Moreover, a small group, a large group, real, standardized and simulated patients or role play may be part of the method of learning. Audio and video recording is important particularly in the development of communication skills.4
Clinical skills laboratories vary in location, shape and site depending on the availability of space and resources. Most CSLs are located in hospitals or medical schools. However, Dacre J, et al (1996) has suggested the use of satellite centers where the skills and communication centers can be linked to peripheral facilities and teaching situations in the primary care clinics, lecture theatres or even the community through information technology.13 Many centers have placed computers and information technology in or near the clinical skills facility.
Clinical skills laboratories may consist of a large open space for seminars and several small side rooms for interviews. It may include a variety of clinical settings such as general practice consulting rooms, procedural skill rooms, accident and emergency cubicles, an Intensive Care Unit and a place for simulators. Storage areas and offices for teachers and support staff are important. It is also necessary that the available space is kept fluid for possible rearrangement to suit a particular lesson. In general, a clinical skills facility should provide a sense of a real clinical environment.
Simulation is an important component of the clinical and communication skill centers. Simulators can be classified into four types (Table 2).14
Table 2.
Simulator types
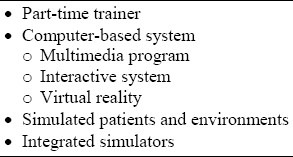
A part-time trainer: training model which represents part of the body or structure that can be used alone or can be attached to simulated patients for simultaneous technical and communication skills development.15
A computer-based system which can be in the form of: (a) multimedia program using audio and video systems; (b) interactive systems which provide the users with clinical variables that can be manipulated to provide feedback on the decisions and actions; (c) virtual reality that creates environments or objects such as computer-generated imaging that replicate kinaesthetic and tactile perception.
Simulated patients and environments: Simulated patients can be professional actors trained to present history and -sometimes mimic physical signs or can be trained patients. Both can be used as standardized patients.16 Creation of simulated environment is common in CSLs.
Integrated simulators. These simulators combine manikins with advanced computer controls that can be adjusted to provide various physiological parameter outputs.
Adequate staffing is important for the success of CSLs. Both teaching and support staff should be selected carefully. Teaching staff can be full time, part time, and seasonal or peripatetic clinical skill teachers. The support staff usually includes administrators, patient coordinators, a secretary and technicians.4 Finally, depending on its setting, CSLs can be used for teaching and learning at both undergraduate and postgraduate levels. They can be used by different professions including medical students, nursing students, dentistry and applied medical science students.
FACTORS THAT LED TO THE DEVELOPMENT OF CSLS
A number of factors have led to the reduction in the number of patients available for students’ training. They include: the recommended early student exposure to clinical skills, the growing number of students, the dramatic reduction of inpatient beds, shorter hospital stay and the shift of care to the ambulatory setting.1 Indications for hospital admission have changed, especially in urban areas as a result of advancement in the day care units. Consequently, patients admitted to hospitals are usually sicker and therefore, unsuitable for bedside clinical skills training. In addition, there is concern that bedside case presentation makes the patient uncomfortable.17 In fact, the estimated time allotted to bedside teaching as a component of medical training declined from 75% in the 1960s to 16% in 1978 and is even lower now.18,19
The above changes have raised concerns of inadequacy in the performance skills of students because of their altered clinical experience and the reduction in their opportunities for acquiring clinical skills.2,20
The increased demand and decreased number of the teaching staff resulting from financial constraints, the competing pressure, work load, administrative and research duties as well as an increase in the number of students and gender separation adopted by some medical schools in Muslim communities have urged the move towards the development of CSLs. The supervision of students and immediate feedback by the teaching staff have therefore become difficult. There is also the problem of legal action. Patients are now better informed, have greater expectations and will no longer accept the role of passive participants in bedside education. Patients reserve the right not to be involved with students.4 In addition to cultural issues, ethical issues are raised when genital, vaginal, rectal and breast examinations are to be done. These factors as well as the invasion of the medical field by computer technology has led to the increase in the number of CSLs and the use of simulation as an innovative teaching approach to medical education.
ADVANTAGES AND DISADVANTAGES OF CSLS
Clinical skills laboratories can be used for teamwork and multi-professional education.21 It provides the students with the access to learning opportunities in a safe and protected environment. Bridging the gap between the classroom and the clinical setting decreases students’ anxiety.
The new learning methods and educational strategies discussed above are difficult to employ in the traditional method using bedside teaching and are, therefore, best used in the CSLs. Students’ communication skills and attitudes to their importance can be improved by integrating these skills into the overall clinical skills program.22 One of the most important advantages of CSLs is that by integrating them into the theoretical component of the curriculum, skills are learnt within their proper context.23 Computer assisted learning and information technology can be used to enhance the interaction between theory and practice.24
The use of simulators enable students to practise and make mistakes without the risk to the patients or themselves. Unlike patients, simulators have predictable behavior, experiences are reproducible and allow standardized experience. They are neither embarrassed or stressed, have no time restrictions and so can be used as required. They can be programmed to simulate selected findings, conditions, or complications and they can be used for training on the management of difficult situations.25 It has been shown that the single most important determinant of skills and knowledge retention is repeated practice,26 which is more feasible in CSLs. Studies have shown that students who graduated from innovative medical schools used more skills during clerkships than students who had followed traditional programs.7 Clinical skills laboratories encourage self-learning since both the medico-legal and ethical issues are not a concern and the use of manikins obviate institutional, individual, and cultural barriers. Students can practice genital, vaginal, rectal and breast examinations without embarassment. This gives them the practice they need and are, therefore, able to approach patients with greater confidence. Direct feedback on performance can be provided with the use of audio-visual aids,27 peer review and teachers’ assessment with opportunities for reflection, evaluation and enhancement or modifications for further action on the part of the learners. The innovative medical institutions require fewer teaching staff who are not required to be full-time teachers. This provides greater flexibility and opportunity for research and staff development. The use of simulators reduces the time spent by students and faculty looking for enough suitable patients for teaching or learning.
The CSLs provide the ideal environment for the assessment of skills acquisition. It has been shown that candidates successful at written examinations have variable practice experiences. In fact, skills cannot be assessed properly by written examinations and should not be tested in isolation. Objective structured clinical examination (OSCE), which can be carried out at the clinical skills learning facilities, is becoming a standard method of skills evaluation.
Video recording and frequent feedback from teachers can also help in both formative and summative assessment. Computer-based simulation allows meticulous assessment of performance including a detailed analysis of movement and behavior and can be used as a method of measuring procedural psychomotor skills.28
The use of CSLs has many advantages, but there are also drawbacks. Skills centers provide different contexts for learning, but cannot replicate reality. There is also the problem of the lack of expertise to maintain CSL centers. Since there are no medico-legal issues to be mindful of, students may ignore the learning of certain clinical skills. Furthermore, simulation instruments can be used to test a specific aspect of technical competence but may not provide a complete assessment of a holistic approach to the patient. The clinical skills facilities are costly. In one study, it was shown that the cost of setting up the main lab was $133,000, and had the mean annual budget of $11,000.29 Information technology resources and simulators need continuous maintenance and updates. The use of informatics resource in developing countries would be hampered by technical difficulties.
GUIDELINES FOR A SUCCESSFUL IMPLEMENTATION
For many medical schools, the high cost of the facility and equipment and the need for continuous update and maintenance is a major barrier to the incorporation of CSLs in their curriculum. Many teaching staff who are strong believers of bedside clinical teaching may resist the change.19 In addition, planning skills centers involves a variety of stakeholders and users, some of whom may not be enthusiastic for change. Since CSLs are costly, it is important to ensure that the outcome is justifiable so that investors can be persuaded. Clinical skills laboratories should be designed to support the intended learning outcome and to form an integral part of the overall curriculum. The development of clinical skills should be integrated into the communication skills program and other parts of the curricula, to avoid reverting to formal method of education. To be successful, clinical skill units need to be flexible in design and schedule. It needs to be within or near the medical schools. The environment and the clinical space should as far as possible mimic the conditions of real practice.30
In conclusion, with the recent changes in the medical education and the fast pace of technological development, CSLs have become an important educational environment for the acquisition of clinical skills. Many clinical skills can be learned and taught in CSLs which also provide ideal environment for assessment. However, they should not replace, but rather complement bedside teaching.
REFERENCES
- 1.Recommendations on Undergraduate Medical Education. London, UK: General Medical Council; 1993. Education Committee of the General Medical Council. Tomorrow’ Doctors. [Google Scholar]
- 2.Remmen R, Scherpbier AJ, Derese A, Denekens J, Hermann I, van der Vleufen CPM, et al. Unsatisfactory basic skills performance by students in traditional medical curricula. Med Teach. 1998;20:579–582. [Google Scholar]
- 3.Boulay CD, Medway C. The clinical skills resource: a review of current practice. Medical Education. 1999;33:185–191. doi: 10.1046/j.1365-2923.1999.00384.x. [DOI] [PubMed] [Google Scholar]
- 4.Bradley P, Postlethwaite K. Setting up a clinical skills learning facility. Medical Education. 2003;37(Suppl 1):6–13. doi: 10.1046/j.1365-2923.37.s1.11.x. [DOI] [PubMed] [Google Scholar]
- 5.Sebiany AM. New trends in medical education: The clinical skills laboratories. Saudi Med J. 2003;24(10):1043–1047. [PubMed] [Google Scholar]
- 6.Al-Yousuf NH. The clinical skills laboratory as a learning tool for medical students and health professionals. Saudi Med J. 2004;25(5):549–551. [PubMed] [Google Scholar]
- 7.Bligh J, Bradley P. One year's experience with a clinical skills resource centre. Medical Education. 1999;33:114–20. doi: 10.1046/j.1365-2923.1999.00351.x. [DOI] [PubMed] [Google Scholar]
- 8.Remmen R, Scherpbier A, Vleuten CV, Denekens J, Derese A, Hermann I, et al. Effectiveness of basic clinical skills training programmes: a cross-sectional comparison of four medical schools. Medical Education. 2001;35:121–128. doi: 10.1046/j.1365-2923.2001.00835.x. [DOI] [PubMed] [Google Scholar]
- 9.Morgan R. Using clinical skills laboratories to promote theory-practice integration during first practice placement: an Irish perspective. Journal of Clinical Nursing. 2006;15:155–161. doi: 10.1111/j.1365-2702.2006.01237.x. [DOI] [PubMed] [Google Scholar]
- 10.Das M, Townsend A, Hasan MY. The views of senior students and young doctors of their training in a skills laboratory. Medical Education. 1998;32(2):143. doi: 10.1046/j.1365-2923.1998.00182.x. [DOI] [PubMed] [Google Scholar]
- 11.Kneebone R, Kidd J, Nestel D, Asvall S, Paraskeva P, Darzi A. An innovative model for teaching and learning clinical procedures. Medical Education. 2002;36:628–634. doi: 10.1046/j.1365-2923.2002.01261.x. [DOI] [PubMed] [Google Scholar]
- 12.Dent JA, Ker JS, Angell-Preece HM, Preece PE. Twelve tips for setting up an ambulatory care (outpatient) teaching centre. Med Teach. 2001;23(4):345–350. doi: 10.1080/01421590120057012. [DOI] [PubMed] [Google Scholar]
- 13.Dacre J, Nicol M, Holroyed D, Ingram D. The development of a clinical skills centre. J. R. Coll. Physicians Lond. 1996;30(4):318–324. [PMC free article] [PubMed] [Google Scholar]
- 14.Bradley P. The history of simulation in medical education and possible future directions. Medical Education. 2006;40:254–262. doi: 10.1111/j.1365-2929.2006.02394.x. [DOI] [PubMed] [Google Scholar]
- 15.Kneebone R, Nestel D. Learning clinical skills – the place of simulation and feedback. Clinical Teacher. 2005;2(2):86. [Google Scholar]
- 16.McGraw RC, O’Connor HM. Standardized patients in the early acquisition of clinical skills. Medical Education. 1999;33:572–578. doi: 10.1046/j.1365-2923.1999.00381.x. [DOI] [PubMed] [Google Scholar]
- 17.White LL. Preparing for clinical just in time. Nurse Educator. 2006;31(2):57–60. doi: 10.1097/00006223-200603000-00005. [DOI] [PubMed] [Google Scholar]
- 18.Gale CP, Gale RP. Is bedside teaching in cardiology necessary for the undergraduate education of medical students? Medical Education. 2006;40:11–13. doi: 10.1111/j.1365-2929.2005.02357.x. [DOI] [PubMed] [Google Scholar]
- 19.MEL-Bagir KA. What is happening to bedside clinical teaching? Medical Education. 2002;36:1185–1188. doi: 10.1046/j.1365-2923.2002.01372.x. [DOI] [PubMed] [Google Scholar]
- 20.Carter R, Aitchison M, Mufti GR, Scott R. Catheterisation: your urethra in their hands. BMJ. 1990;301(6757):905. doi: 10.1136/bmj.301.6757.905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tucker K, Wakefield A, Boggis C, Lawson M, Roberts T, Gooch J. Learning together: clinical skills teaching for medical and nursing students. Medical Education. 2003;37:630–637. doi: 10.1046/j.1365-2923.2003.01558.x. [DOI] [PubMed] [Google Scholar]
- 22.Willis SC, Jones A, O’Neill PA. Can undergraduate education have an effect on the ways in which pre-registration house officers conceptualize communication? Med Educ. 2003;37:603–8. doi: 10.1046/j.1365-2923.2003.01555.x. [DOI] [PubMed] [Google Scholar]
- 23.O’Connor HM. Training undergraduate medical students in procedural skills. Emergency Medicine. 2002;14:131–135. doi: 10.1046/j.1442-2026.2002.00333.x. [DOI] [PubMed] [Google Scholar]
- 24.Schittek M, Mattheos N, Lyon HC, Attstrom R. Computer assisted learning: A review. Eur J Dent Educ. 2001;5:93–100. doi: 10.1034/j.1600-0579.2001.050301.x. [DOI] [PubMed] [Google Scholar]
- 25.Issenberg SB, McGaghie WC, Hart IR, Mayer JW, Felner JM, Petrusa ER, Waugh RA, et al. Simulation technology for health care professional skills training and assessment. JAMA. 1999;282(9):861–866. doi: 10.1001/jama.282.9.861. [DOI] [PubMed] [Google Scholar]
- 26.Kneebone RL, Scott W, Darzi A, Horrocks M. Simulation and clinical practice: strengthening the relationship. Medical Education. 2004;38:1095–1102. doi: 10.1111/j.1365-2929.2004.01959.x. [DOI] [PubMed] [Google Scholar]
- 27.Paul S, Dawson KP, Lanphear JH, Cheema MY. Video recording feedback: a feasible and effective approach to teaching history-taking and physical examination skills in undergraduate paediatric medicine. Medical Education. 1998;32:332–336. doi: 10.1046/j.1365-2923.1998.00197.x. [DOI] [PubMed] [Google Scholar]
- 28.Datta V, Mandalia M, Mackay S, Chang A, Cheshire N, Darzi A. Relationship between skill and outcome in the laboratory-based model. Surgery. 2002;131:318–23. doi: 10.1067/msy.2002.120235. [DOI] [PubMed] [Google Scholar]
- 29.Korndorffer JR, Jr, Stefanidis D, Scott DJ. Laparoscopic skills laboratories: current assessment and a call for resident training standards. The American Journal of Surgery. 2006;191:17–22. doi: 10.1016/j.amjsurg.2005.05.048. [DOI] [PubMed] [Google Scholar]
- 30.Kneebone RL, Kidd J, Nestel D, Barnet A, Lo B, King R, et al. Blurring the boundaries: scenario-based simulation in a clinical setting. Medical Education. 2005;39:580–587. doi: 10.1111/j.1365-2929.2005.02110.x. [DOI] [PubMed] [Google Scholar]


