Abstract
Asystole during posterior fossa neurosurgical procedures is not uncommon. Various causes have been implicated, especially when surgical manipulation is carried out in the vicinity of the brain stem. The trigemino-cardiac reflex has been attributed as one of the causes. Here, we report two cases who suffered asystole during the resection of posterior fossa tumors. The vago-glossopharyngeal reflex and the direct stimulation of the brainstem were hypothesized as the causes of asytole. These episodes resolved spontaneously following withdrawal of the surgical stimulus emphasizing the importance of anticipation and vigilance during critical moments of tumor dissection during posterior fossa surgery.
Keywords: Asystole, brainstem manipulation, posterior fossa surgery, trigemino-cardiac reflex, vago-glossopharyngeal reflex
Introduction
Neurosurgical conditions responsible for cardiac arrhythmias have been described in the literature.[1] The resultant arrhythmia may be sinus bradycardia, paroxysmal ventricular contraction, supraventricular tachycardia, ventricular fibrillation, or flutter.[2] Sudden bradycardia/asystole are not uncommon, especially when surgery is carried out in the vicinity of brain stem. Various causes have been described and most often, the trigemino-cardiac reflex is implicated. However, none attributed it to the vago-glossopharyngeal reflex during surgery in the posterior fossa. Here, two cases of asystole have been described during posterior fossa surgery. The vago-glossopharyngeal reflex andthe direct stimulation of brainstem are hypothesized as the causes.
Case Reports
Case 1
A 40-year-old male, weighing 65 kg, was admitted with complaints of headache, decreased hearing in the left ear and decreased vision in both eyes for one year. There was no history of any co-existing medical illness. He underwent a ventriculoperitoneal shunt insertion under general anesthesia six months back. All investigations were within normal limits. He was diagnosed with left acoustic neuroma [Figure 1]; hence, a retromastoid suboccipital craniotomy and excision of the tumor was planned. After induction of anesthesia, the patient was placed in the sitting position and surgery was commenced. During the dissection of tumor adjacent to the glossopharyngeal nerve, a transient episode of bradycardia occurred which resolvedspontaneously. Fifteen minutes later, bradycardia recurred which proceeded to asystole. The neurosurgeon was informed and atropine 0.3 mg was given, intravenously. The heart rate was reverted back to normal. The mean arterial pressure (MAP) showed a fall from 80 to 62 mmHg. A bolus of hydroxyethyl starch (100 ml) along with mephentermine 3 mg was administered. MAP increased to 74 mmHg; and the dissection of tumor was continued. Another episode of sudden asystole occurred four minutes later. The heart rate was improved after the stimulus was withdrawn. It was decided to stop the excision of tumor along the area of glossopharyngeal nerve. After completion of the procedure, the patient was shifted to intensive care unit for elective ventilation. The trachea was extubated uneventfully 12 hours later.
Figure 1.
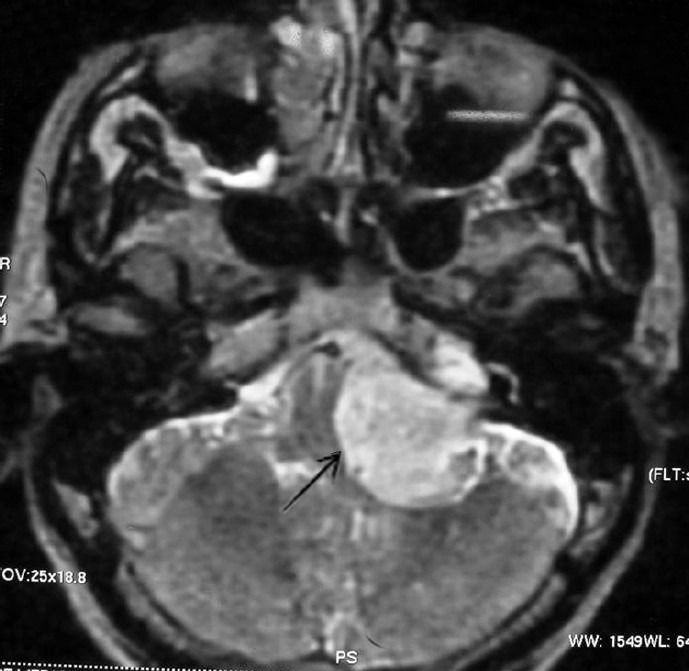
Magnetic resonance imaging of brain showing left cerebellopontine angle mass lesion (arrow) compressing the brainstem
Case 2
A 25-year-old male weighing 80 kg, presented with history of occipital headache and vomiting lasting for seven months.Magnetic resonance imaging of brain showed a dermoid cyst in the cisterna magna displacing the fourth ventricle. The midline suboccipital craniotomy and excision of the dermoid cyst were planned in prone position. The past history of any medical/surgical illness was unremarkable. The pre-operative investigations were all within normal limits. In the operating room, after induction ofanesthesia, the patient was positioned prone. After 160 minutes of surgery, the patient developed a sudden flat line on electrocardiogram (ECG) [Figure 2]. The operating surgeon was informed immediately and 100% oxygen was started. The asystole continued for 10 seconds and then reverted back to normal sinus rhythm spontaneously without any intervention. The stoppage of surgery and termination of asystole occurred simultaneously, indicating that brain handling was the cause.After this event,the surgery continued for two more hours and was uneventful.The patient was electively ventilated in view of the intraoperative course and was successfully extubated on the first pre-operative day. One week later, the patient was discharged from the hospital without any further complaints.
Figure 2.
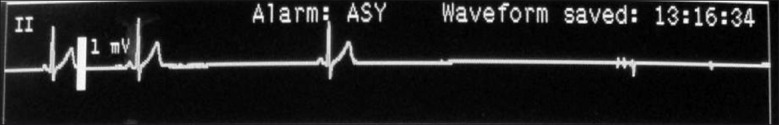
Flat line (asystole) in ECG lead II
Discussion
Cardiac pathology, hypoxia, light plane of anesthesia, use of agents like β-blockers, α2-agonists, potent narcotics, and other anesthetic drugs may all lead to bradycardia or asystole during an ongoing surgery. The asystole may also be produced through paradoxal cardiovascular reflexes.[3] Neurogenic bradycardia that may result in cardiac arrest is a rare, but well recognized complication during anesthesia. An acute increase in intracranial pressure and a subsequent secondary brainstem compression may be the reason. Sometimes, it may occur due to the vagal stimulation caused by any space occupying lesion in the medulla.[4] These reactions may be elicited by the activation of trigeminocardiac reflex due to the direct stimulation of the trigeminal nerve or its branches in the dura mater or the cerebellar tentorium.[5] The trigeminal nerve and the cardio-inhibitory vagus nerve constitute the afferent and efferent pathways of the reflex arc. Sudden asystolemay occur regardless of pressure on the brainstem during posterior fossa surgery.[6]
The impulses from the glossopharyngeal nerve travelvia the tractus solitarius of midbrain, and then to, the dorsal motor nucleus of vagus nerve. Activation of the reflex may, thereby, cause reflex bradycardia and sometimes asystole forming vago-glossopharyngeal reflex arc. The carotid sinus nerve (Hering's nerve), responsible for the conduction of impulses from the body and the carotid sinus, runs in the main trunk of the glossopharyngeal nerve and ends in the dorsal nucleus of the vagus nerve. It has been suggested that artificial synapses develop in the proximal portion of the glossopharyngeal nerve stimulating the carotid sinus via somatosensorial impulses.[7] It may also be due to the overflow of responses from the ninth cranial nerve into the vagal motor nucleus during handling of posterior fossa tumors. With the removal of the surgical stimulus, the bradycardia usually improves and pharmacological treatment is not required. Moreover, the drugs if given may mask the signs of brainstem handling and may permanently damage the cranial nerve nuclei.
Intraoperative cardiac arrest in patients placed in position other than supine poses a challenge in terms of resuscitation. Here, Case 1 was operated in sitting position,whereas Case 2 in lateral position. Repositioning these patients is difficult, as it not only needs manpower to safely turn the patient supine,but also delays cardiopulmonary resuscitation. Otherwise, resuscitation has to be carried out in unconventional positions.[8]
To conclude, the most possible explanation for asystole in the first case was due to the vago-glossopharyngeal reflex and in the second case, it was due to the direct handling of brainstem. The ability to predict the risk of asystole may better prepare clinicians to anticipate, identify, and manage an episode. It may also be suggested that in large posterior fossa tumors, specific history of symptoms related to glossopharyngeal neuralgia (paroxysmal neuralgic pain in the throat and neck precipitated by swallowing, chewing or coughing) should be taken. Transcutaneous pacing should be considered during the surgery in view of bradycardia and risk of asystole, especially in high risk patients. The importance of having the knowledge, vigilance, equipment, and skills to deal rapidly with such a case will be crucial for the patient's survival.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Talman WT. Cardiovascular regulation and lesions of the central nervous system. Ann Neurol. 1985;18:1–13. doi: 10.1002/ana.410180102. [DOI] [PubMed] [Google Scholar]
- 2.Rath GP, Chaturvedi A, Chouhan RS, Prabhakar H. Transient cardiac asystole in transsphenoidal pituitary surgery: A case report. J Neurosurg Anesthesiol. 2004;16:299–301. doi: 10.1097/00008506-200410000-00009. [DOI] [PubMed] [Google Scholar]
- 3.Kinsella SM, Tuckey JP. Perioperative bradycardia and asystole: Relationship to vasovagal syncope and the Bezold Jarisch reflex. Br J Anaesth. 2001;86:859–68. doi: 10.1093/bja/86.6.859. [DOI] [PubMed] [Google Scholar]
- 4.Kawasaki S, Ishii M, Kon S, Yoshida Y. A case of sporadic and transient bradyarrhythmias in a patient with a glioma in the medulla oblongata. Kokyu To Junkan. 1993;41:787–90. [PubMed] [Google Scholar]
- 5.Usami K, Kamada K, Kunii N, Tsujihara H, Yamada Y, Saito N. Transient asystole during surgery for posterior fossa meningioma caused by activation of the trigeminocardiac reflex: Three case reports. Clin Neurol Neurosurg. 2009;111:220. doi: 10.2176/nmc.50.339. [DOI] [PubMed] [Google Scholar]
- 6.Bilgin H, Bozkurt M, Yilmazlar H, Korfali G. Sudden asystole without any alerting signs during cerebellopontine angle surgery. J Clin Anesth. 2006;18:243–4. doi: 10.1016/j.jclinane.2005.12.014. [DOI] [PubMed] [Google Scholar]
- 7.Elias J, Kuniyoshi R, Valadao W, Carloni H, Borges MR, Peixoto CA, et al. Glossopharyngeal neuralgia associated with cardiac syncope. Arq Bra Cardiol. 2002;78:515–9. doi: 10.1590/s0066-782x2002000500008. [DOI] [PubMed] [Google Scholar]
- 8.Abraham M, Wadhawan M, Gupta V, Singh AK. Cardiopulmonary resuscitation in the lateral position: Is it feasible during pediatric intracranial surgery? Anesthesiology. 2009;110:1185–6. doi: 10.1097/ALN.0b013e31819f7b2b. [DOI] [PubMed] [Google Scholar]


