Abstract
Background:
The prevalence of vitamin D deficiency has recently been recognized in different parts of the world, even affecting healthy populations. The deficiency of vitamin D can lead to rickets in children and osteomalacia in adults. Few studies have been done to evaluate the status of vitamin D in the medical community. The objective of this study was to evaluate the prevalence of low levels of vitamin D in healthy Saudi medical students.
Materials and Methods:
A cross-sectional study was carried out in November 2009 on male and female students in the preclerkship years of medical school at the King Faisal University, Dammam. Data on age, consumption of dairy products and seafood, and exposure to sunlight were collected. The body mass index was calculated. Approximately, 15 ml of blood was extracted for the measurement of serum calcium, serum albumin, serum phosphorus, alkaline phosphatase, fasting parathyroid hormone, and vitamin D levels. Vitamin D deficiency was defined as serum 25-hydroxy vitamin D < 50 nmol/l. Comparison between groups was done for statistical significance using an unpaired t-test. Significance was set at P < 0.05 using 95% CI for all comparisons.
Results:
The data from 95 male and 103 female students were analyzed. The mean age for all students was 19.54 years. In 100% of the students, the vitamin D level was low. The prevalence of vitamin D deficiency in all students was 96.0% (92.64% in males and 99.03% in females), while the remaining 4% had vitamin D insufficiency. The mean 25-hydroxy vitamin D level was 26.83 ± 12.60 nmol/l in males and 16.03 ± 8.28 nmol/l in females (P-value = 0.0001). Males had a statistically significant higher body mass index as well as consumption of dairy products, while the consumption of seafood was significantly higher in females. There was no difference between the two groups in terms of exposure to the sun.
Conclusion:
Vitamin D deficiency was highly prevalent among medical students included in this study. An urgent action has to be taken in order to prevent adverse consequences of low vitamin D in the young, otherwise healthy populations.
Keywords: Insufficiency, medical students, Saudi, vitamin D deficiency
INTRODUCTION
The two main forms of vitamin D are vitamin D2 or ergocalciferol, obtained from the consumption of yeasts and plants, and vitamin D3 or cholecalciferol, mainly formed in the skin after exposure to ultraviolet B radiation, but also present in foods such as fish and cod liver oil. In both children and adults, the primary source of vitamin D is exposure to the sun while the content of vitamin D in food is low.[1] Vitamin D is important for the absorption of calcium, and bone formation and maintenance. The deficiency of vitamin D can lead to rickets in children and osteomalacia in adults.[2] In addition, low vitamin D levels in adults induce hyperparathyroidism, leading to decreased bone mass in the form of osteopenia and osteoporosis with its consequent fragility fractures.[3]
It is generally agreed that the evaluation of the status of vitamin D should be performed through the measurement of 25-hydroxy vitamin D (25OHD) levels, though what constitutes a normal level of vitamin D remains controversial.[4] In the past few years, a consensus has developed among the experts in the field that the normal 25OHD level is >75 nmol/l (>30 ng/ml), while a level between 52 and 72 nmol/l (21–29 ng/ml) is defined as a state of insufficiency and a level of <50 nmol/l (<20 ng/ml) is consistent with deficiency.[5] With the prevalence of food-fortifying programs, it was thought that vitamin D deficiency had been eradicated, but deficiency remains unexpectedly endemic in many parts of the world, and its prevalence appears to be increasing.[6] The deficiency is prevalent not only in females or the elderly but also in free-living healthy young male adults.[7] In fact, 30–50% of children and adults in the United Arab Emirates, Australia, Turkey, India, and Lebanon have been found to have vitamin D deficiency.[8] Although Saudi Arabia is one of the sunniest countries, vitamin D deficiency has long been reported as prevalent in the Saudi population.[9–11] A few studies performed over the last few years to evaluate the status of vitamin D in Saudi nationals have shown a high prevalence for its deficiency.[12–14]
After becoming aware of the high prevalence of vitamin D deficiency in the community, several medical students with low levels of vitamin D were seen at our endocrinology clinic. This study was carried out with an objective of evaluating the prevalence of low vitamin D levels (insufficiency and deficiency) in male and female medical students in the preclerkship years at King Faisal University-Dammam (KFU-D).
MATERIALS AND METHODS
This was a cross-sectional study conducted on 198 medical students. The study was approved by the Ethical and Research Committee of KFU-D. All medical students (227 males and 178 females) enrolled in the first and fourth preclerkship levels in the 2009–2010 academic year in the medical school of KFU-D in the Eastern Province of Saudi Arabia were invited to participate in the study. Informed consent was obtained from all participants. Students who refused to consent to the study were excluded. Students were also excluded if they had diseases that interfered with the metabolism of calcium and vitamin D, such as liver or renal diseases, or were using drugs that affected the level of vitamin D, such as vitamin D supplements, anticonvulsants, and steroids, or had a family history of inherited diseases of metabolism of vitamin D. One hundred and thirty-three students (58.6%) from the first year and 104 (58.4%) students from the fourth year responded. Twenty-one first-year students and 18 fourth-year students were excluded.
After consenting to the study, data regarding age, dairy product and seafood consumption, and exposure to sunlight were collected using a data collection sheet. Height and weight were measured, and the body mass index (BMI) was calculated. BMI was defined as the weight in kilograms divided by the square of the height in meters. Approximately 15 ml of blood was extracted from each student for the measurement of serum calcium, serum albumin, serum phosphorus, alkaline phosphatase, fasting parathyroid hormone, and vitamin D level. Blood was collected from students in the fasting state at the medical college during the month of November, 2009, between 8:00 and 10:00 AM. Following extraction, the blood was immediately centrifuged, and then stored at -20°C before being analyzed. All of the analyses were carried out at the laboratories of the King Fahd Hospital of the University-Al Khobar. Serum calcium, serum phosphorous, serum magnesium, serum albumin, and alkaline phosphatase were determined by a semi-auto-analyzer. Intact PTH was determined by a two-site binding immunoradiometric assay. The serum level of 25OHD was measured using the chemiluminescence immunoassay methodology. In this study, 25OHD was considered as normal if the level was >75 nmol/l, insufficient if the level was between 50 and 75 nmol/l, and deficient if the level was < 50 nmol/l.
The data were summarized either as percentages or means ± standard deviations (SD). A comparison of the means of the males and females or the first- and fourth-year groups was done for statistical significance using an unpaired t-test. Significance was set at P < 0.05 using 95% CI for all comparisons. The statistical analysis was performed using SPSS 17 software (SPSS, Chicago, IL, USA).
RESULTS
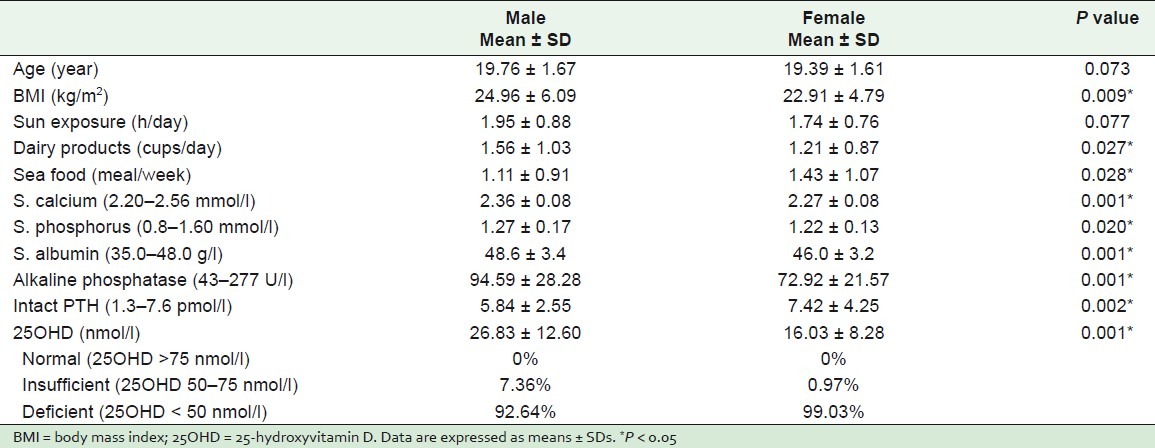
Data from 112 students from the first year and 86 students from the fourth year were analyzed. There were 95 male and 103 female students. The mean age for all the students was 19.54 years. Males had a significantly higher BMI (24.96 ± 6.09 vs. 22.91 ± 4.79, P-value = 0.009) and a higher consumption of dairy products (1.56 ± 1.03 vs. 1.21 ± 0.87 cups/day, P-value = 0.027), although the duration of their exposure to the sun was not significantly longer (1.95 ± 0.87 vs. 1.74 ± 0.76 h/day, P-value = 0.077). Females consumed significantly more seafood (1.43 ± 1.07 vs. 1.11 ± 0.9 serving/week, P-value = 0.028). In addition to significantly lower 25OHD levels, females had significantly lower calcium levels, albumin levels, phosphorus levels, and alkaline phosphatase with a higher mean level of PTH (7.42 ± 4.24 vs. 5.84 ± 2.54, P-value = 0.002) compared with males [Table 1]. Because the only information available on students who refused to participate was their gender and the year of the study (they did not fill the data collection sheet), it was not possible to study their baseline characteristics.
Table 1.
Clinical and biochemical data and vitamin D status for both male and female medical students
The comparison between first- and fourth-year students is shown in Table 2. The difference in the BMI between the first- and fourth-year students was statistically nonsignificant (P-value = 0.742). In addition, the difference in exposure to the sun was similar (1.75 ± 0.88 vs. 1.94 ± 0.73 h/day, P-value = 0.199). The intake of seafood was significantly lower (7.42 ± 4.24 vs. 5.84 ± 2.54 serving/week, P-value = 0.002) and the consumption of dairy products was nonsignificantly lower in the fourth-years compared to first-year students. The differences in 25OHD and PTH levels were also not statistically significant. Fourth-year students had significantly lower levels of serum calcium (2.29 ± 0.09 vs. 2.33 ± 0.09, P = 0.002) and alkaline phosphatase.
Table 2.
Clinical and biochemical data and vitamin D status for first-year and fourth-year medical students
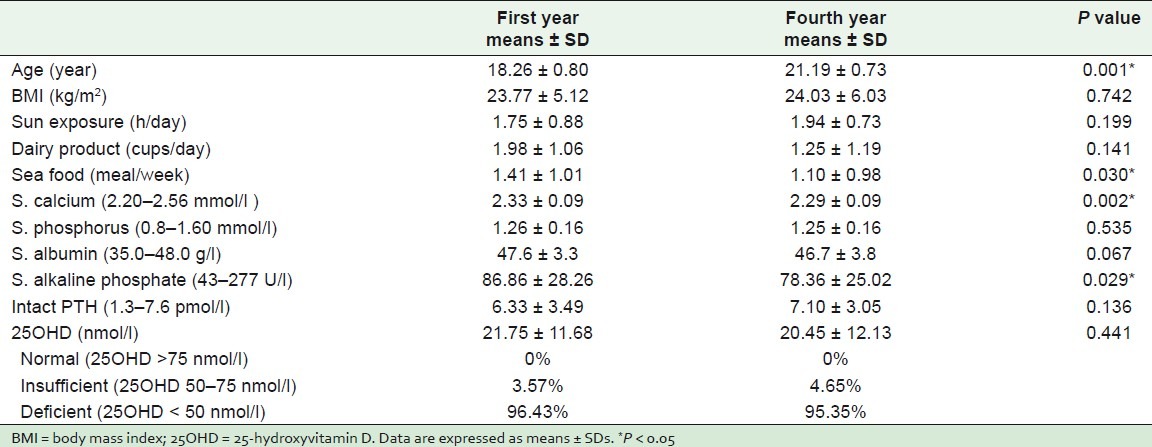
All students were diagnosed to have low levels of vitamin D. None of them had a level of >75 nmol/l. Vitamin D was insufficient in 7.36% of the male and in 1% of the female students, and it was deficient in 92.64% of the male students and 99.03% of the female students. The mean 25OHD level was 26.83 ± 12.60 nmol/l in males and 16.03 ± 8.28 nmol/l in females with a highly significant statistical difference (P-value = 0.001; Table 1). In a comparison of first- and fourth-year students, 96.43% of the first-year students and 95.35% of the fourth-year students had vitamin D deficiency [Table 2].
DISCUSSION
Vitamin D deficiency continues to be an unrecognized epidemic in many populations around the world.[15] It has been reported in healthy children, young adults, middle-aged adults, and the elderly, and is common among both males and females.[16] Moreover, it is common even in the populations of the sunniest countries. In this study, we found vitamin D deficiency to be highly prevalent in healthy Saudi medical students in the preclerkship years of a medical school in the Eastern Province of Saudi Arabia. In fact, none of the students evaluated had normal levels of vitamin D, defined as 25OHD > 75 nmol/l,[5] and the majority of male and female students at the start and at the end of the preclerkship period had 25OHD levels consistent with the definition of vitamin D deficiency. A similar high prevalence of low vitamin D was reported recently among patients from Eastern Province of Saudi Arabia.[12,13] Also Ardawi et al.[14] reported an approximately 80% prevalence of hypovitaminosis D in 1172 Saudi women from the western region of Saudi Arabia, while Sadat-Ali et al.[17] found a 28% and 37% prevalence of hypovitaminosis in male patients aged 25–35 years and ≥50 years, respectively. The above reported variation in prevalence can be partially explained by the difference in the populations studied, the time of the year when the blood samples were collected and, possibly, the different laboratory methodologies used.[18] This study was conducted during the month of November using the chemiluminescence immunoassay methodology. This may have contributed to the high prevalence of low vitamin D.
Recently, González-Padilla et al.[19] reported a high prevalence of hypovitaminosis D in medical students from Spain, and Multani et al.[20] found that 87.5% of resident doctors from India had low vitamin D levels. However, in a study that was conducted in a hospital in the Boston area of USA, only 36% of the healthy students, residents, and physicians aged 18–29 years were found to be vitamin D deficient.[7] The markedly higher prevalence of low vitamin D in medical students in Saudi Arabia and Spain and the resident doctors from India as compared to individuals from the Boston area of USA , in spite of the abundance of sunlight found in the former areas may be related to the difference in dietary habits and food fortification[21] in addition to racial and genetic factors. The results of this study, which showed that 100% of young educated students in the medical field have low vitamin D, raise a great concern about the future skeletal health of these young students. The 25OHD concentration was found recently to be an independent determinant of peak bone mass.[22] Importantly, Lips et al.[23] and Heaney[24] concluded that adequate vitamin D levels can prevent osteoporosis-related hip fractures.
In general, hypovitaminosis D has been reported in the literature as being more prevalent in women.[25,26] Several factors were postulated for the low vitamin D level in females, including dietary habits, exposure to the sun, pregnancy and lactation. There is also controversy regarding the contribution of the wearing of a veil to lower vitamin D levels in Muslim women.[27,28] Our female students had significantly lower consumption of dairy products. Also almost all of our female medical students were veiled. However, the lower 25OHD levels in the femle students included in this study may not be explained by the difference in sunlight exposure since there was no statistical significant difference between male and female students with regard to exposure to sunlight. The lower vitamin D levels in female students involved in this study also cannot be explained by difference in BMI since they had significantly lower BMI than the male students. Obesity is considered as one of the risk factors for low vitamin D levels; this low level of vitamin D in obese patients p ossibly resulting from the sequestrating effect of a high quantity of subcutaneous fat on circulating vitamin D.[29–31] As expected, owing to lower vitamin D levels, females were found to have significantly lower serum calcium and higher mean PTH levels, possibly as part of an early secondary hyperparathyroidism leading to significantly lower serum phosphorus.[32] The lower level of alkaline phosphatase in females is possibly related to the use of oral contraceptive pills.[33]
After spending more than 3 years in college , fourth-year medical students were consuming less dairy products and seafood than the first-year students, and their low vitamin D levels persisted. The lower serum calcium and the higher PTH levels compared to first year students is another indicator of the poor dietary habits of this group of medical students. Al-Gelban[34] found that students of a Saudi Teachers’ Training College had unhealthy lifestyles and dietary habits, while Nisar et al.[35] reported unhealthy lifestyles and dietary habits in students of a private medical university in Karachi.
The present study is one of the few studies carried out to evaluate the status of vitamin D in the medical community. The limitations of our study are that, being cross-sectional rather than longitudinal, comparisons between first-year and fourth-year students became suboptimal. Also, the use of the chemiluminescence immunoassay is not the gold standard method for the measurement of 25OHD levels. Besides, information on the consumption of dairy products and seafood, and exposure to sunlight was collected by means of a data collection sheet rather than a validated questionnaire.
CONCLUSION
In 100% of the medical students studied, there were low vitamin D levels found. An urgent action through the modification of lifestyle and dietary habits, along with improved food fortification and treatment of this deficiency, must be undertaken in order to prevent any future untoward consequences of hypovitaminosis D in these young healthy populations.
ACKNOWLEDGMENTS
The author thanks the Deanship of the Scientific Research, KFU, for the support, without which this study could not have been carried out. The author also sincerely thanks the following medical students and interns: Amal Sadiq Al-Saad, Sanaa Sadiq Al-Saad, Mariam Abduljaleel Al-Khalifah, Hawra Sameer Al-Khalifah, Ayat Ali Al-Ali, Layla Nasser Al-Nasser, Ahmad Sameer Al-Khalifah, and Fahad Omar Arafat, who contributed to subject recruitment and blood sample collection.
Footnotes
Source of Support: Nil
Conflict of Interest: Nil
REFERENCES
- 1.Lips P. Vitamin D physiology. Prog Biophys Mol Biol. 2006;92:4–8. doi: 10.1016/j.pbiomolbio.2006.02.016. [DOI] [PubMed] [Google Scholar]
- 2.Cashman KD. Vitamin D in children and adolescence. Postgrad Med J. 2007;83:230–5. doi: 10.1136/pgmj.2006.052787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Holick MF. The Vitamin D Epidemic and its Health Consequences. J Nutr. 2005;135:2739S–48S. doi: 10.1093/jn/135.11.2739S. [DOI] [PubMed] [Google Scholar]
- 4.Holick MF. Vitamin D status: Measurement, interpretation, and clinical application. Ann Epidemiol. 2009;19:73–8. doi: 10.1016/j.annepidem.2007.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jones G, Horst R, Carter G, Makin HL. Contemporary diagnosis and treatment of vitamin D-related disorders. J Bone Miner Res. 2007;11(Suppl 2):V11–5. doi: 10.1359/jbmr.07s219. [DOI] [PubMed] [Google Scholar]
- 6.Lowdon J. Low vitamin D status: On the increase? J Fam Health Care. 2008;18:55–7. [PubMed] [Google Scholar]
- 7.Tangpricha V, Pearce EN, Chen TC, Holick MF. Vitamin D Insufficiency among Free-Living Healthy young Adults. Am J Med. 2002;12:659–62. doi: 10.1016/s0002-9343(02)01091-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Holick MF. Vitamin D Deficiency. N Engl J Med. 2007;357:266–81. doi: 10.1056/NEJMra070553. [DOI] [PubMed] [Google Scholar]
- 9.Sedrani SH, Elidrissy AW, El Arabi KM. Sunlight and vitamin D status in normal Saudi subjects. Am J Clin Nutr. 1983;38:129–32. doi: 10.1093/ajcn/38.1.129. [DOI] [PubMed] [Google Scholar]
- 10.Woodhouse NY, Norton WL. Low vitamin D level in Saudi Arabians. King Faisal Spec Hosp Med J. 1982;2:127–31. [Google Scholar]
- 11.Fonseca V, Tongia R, El-Hazmi M. Exposure to sunlight and vitamin D deficiency in Saudi Arabian women. Postgrad Med J. 1984;60:589–91. doi: 10.1136/pgmj.60.707.589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Eledrisi M, Alamodi R, Alhaj B, Rehmani R. Vitamin D: Deficiency or no deficiency. South Med J. 2007;100:543–4. doi: 10.1097/SMJ.0b013e31802f81db. [DOI] [PubMed] [Google Scholar]
- 13.Elsammak MY, Al-Wosaibi AA, Al-Howeish A, Alsaeed Vitamin d deficiency in Saudi Arabs. J Horm Metab Res. 2010;42:364–8. doi: 10.1055/s-0030-1248296. [DOI] [PubMed] [Google Scholar]
- 14.Ardawi MS, Qari MH, Rouzi AA, Maimani AA, Raddadi RM. Vitamin D status in relation to obesity, bone mineral density, bone turnover markers and vitamin D receptor genotypes in healthy Saudi pre- and postmenopausal women. Osteoporos Int. 2011;22:463–75. doi: 10.1007/s00198-010-1249-7. [DOI] [PubMed] [Google Scholar]
- 15.Holick MF, Chen TC. Vitamin D deficiency: A worldwide problem with health consequences. Am J Clin Nutr. 2008;87:1080s–6s. doi: 10.1093/ajcn/87.4.1080S. [DOI] [PubMed] [Google Scholar]
- 16.Holick MF. High Prevalence of Vitamin D Inadequacy and Implications for Health. Mayo Clin Proc. 2006;81:353–73. doi: 10.4065/81.3.353. [DOI] [PubMed] [Google Scholar]
- 17.Sadat-Ali M, Al-Elq A, Al-Turki H, Al-Mulhim F, Al-Ali AK. Vitamin D levels in healthy men in eastern Saudi Arabia. Ann Saudi Med. 2009;29:378–82. doi: 10.4103/0256-4947.55168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lai JK, Lucas RM, Banks E, Ponsonby AL Ausimmune Investigator Group. Variability in vitamin D assays impairs clinical assessment of vitamin D status. Intern Med J. 2012;42:43–50. doi: 10.1111/j.1445-5994.2011.02471.x. [DOI] [PubMed] [Google Scholar]
- 19.González-Padilla E, Soria López A, González-Rodríguez E, García-Santana S, Mirallave-Pescador A, Groba Marco Mdel V, et al. High prevalence of hypovitaminosis D in medical students in Gran Canaria, Canary Islands (Spain)] Endocrinol Nutr. 2011;58:267–73. doi: 10.1016/j.endonu.2011.03.002. [DOI] [PubMed] [Google Scholar]
- 20.Multani SK, Sarathi V, Shivane V, Bandgar TR, Menon PS, Shah NS. Study of bone mineral density in resident doctors working at a teaching hospital. J Postgrad Med. 2010;56:65–70. doi: 10.4103/0022-3859.65272. [DOI] [PubMed] [Google Scholar]
- 21.Crowe FL, Steur M, Allen NE, Appleby PN, Travis RC, Key TJ. Plasma concentrations of 25-hydroxyvitamin D in meat eaters, fish eaters, vegetarians and vegans: Results from the EPIC-Oxford study. Public Health Nutr. 2011;14:340–6. doi: 10.1017/S1368980010002454. [DOI] [PubMed] [Google Scholar]
- 22.Välimäki VV, Alfthan H, Lehmuskallio E, Löyttyniemi E, Sahi T, Stenman UH, et al. Vitamin D status as a determinant of peak bone mass in young Finnish men. J Clin Endocrinol Metab. 2004;89:76–80. doi: 10.1210/jc.2003-030817. [DOI] [PubMed] [Google Scholar]
- 23.Lips P, Hosking D, Lippuner K, Norquist JM, Wehren L, Maalouf G, et al. The prevalence of vitamin D inadequacy amongst women with osteoporosis: An international epidemiological investigation. J Intern Med. 2006;260:245–54. doi: 10.1111/j.1365-2796.2006.01685.x. [DOI] [PubMed] [Google Scholar]
- 24.Heaney RP. Nutritional factors in osteoporosis. Annu Rev Nutr. 1993;13:287–316. doi: 10.1146/annurev.nu.13.070193.001443. [DOI] [PubMed] [Google Scholar]
- 25.Gannage-Yared M, Chemali R, Yaacoub N, Halaby G. Hypovitaminosis D in sunny Country: Relation to Lifestyle and Bone Markers. J Bone Miner Res. 2000;15:1856–62. doi: 10.1359/jbmr.2000.15.9.1856. [DOI] [PubMed] [Google Scholar]
- 26.Sherman SS, Hollis BW, Tobin JD. Vitamin D status and related parameters in a healthy population: The effect of age, sex, and season. J Clin Endocrinol Metab. 1990;71:405–13. doi: 10.1210/jcem-71-2-405. [DOI] [PubMed] [Google Scholar]
- 27.Guzel R, Kozanoglu E, Guler-Uysal F, Soyupak S, Sarpel T. Vitamin D status and bone mineral density of veiled and unveiled Turkish women. J Womens Health Gend Based Med. 2001;10:765–70. doi: 10.1089/15246090152636523. [DOI] [PubMed] [Google Scholar]
- 28.Islam MZ, Akhtaruzzaman M, Lamberg-Allardt C. Hypovitaminosis D is common in both Veiled and nonveiled Bangladeshi women. Asia Pac J Clin Nutr. 2006;15:81–7. [PubMed] [Google Scholar]
- 29.Arunabh S, Pollack S, Yeh J, Aloia JF. Body fat content and 25- hydroxyl vitamin D levels in healthy women. J Clin Endocrinol Metab. 2003;88:157–61. doi: 10.1210/jc.2002-020978. [DOI] [PubMed] [Google Scholar]
- 30.Goldner WS, Stoner JA, Thompson J, Taylor K, Larson L, Erickson J, et al. Prevalence of vitamin D insufficiency and deficiency in morbidly obese patients: A comparison with non-obese controls. Obes Surg. 2008;18:145–50. doi: 10.1007/s11695-007-9315-8. [DOI] [PubMed] [Google Scholar]
- 31.Al-Elq A, Sadat-Ali M, Al-Turki H, Al-Mulhim F, Al-Ali AK. Is there is a relationship between body mass index and vitamin D levels? Saudi Med J. 2009;12:1542–6. [PubMed] [Google Scholar]
- 32.Giusti A, Barone A, Razzano M, Pizzonia M, Oliveri M, Palummeri E, et al. High prevalence of secondary hyperparathyroidism due to hypovitaminosis D in hospitalized elderly with and without hip fracture. J Endocrinol Investig. 2006;29:809–13. doi: 10.1007/BF03347375. [DOI] [PubMed] [Google Scholar]
- 33.Crofton PM, Evans N, Bath LE, Warner P, Whitehead TJ, Critchley HO, et al. Physiological versus standard sex steroid replacement in young women with premature ovarian failure: Effects on bone mass acquisition and turnover. Clin Endocrinol (Oxf) 2010;73:707–14. doi: 10.1111/j.1365-2265.2010.03868.x. [DOI] [PubMed] [Google Scholar]
- 34.Al-Gelban KS. Dietary habits and exercise practice among the students of a Saudi Teachers, Training College. Saudi Med J. 2008;29:754–9. [PubMed] [Google Scholar]
- 35.Nisar N, Qadri MH, Fatima K, Perveen S. Dietary and life style among the students of a private medical university in Karachi. J Pak Med Assoc. 2008;58:687–90. [PubMed] [Google Scholar]


