Abstract
Background:
Breastfeeding is one of the most important determinants of child survival, birth spacing, and the prevention of childhood infections. The beneficial effects of breastfeeding depend on its initiation, duration, and the age at which the breastfed child is weaned. Breastfeeding practices vary among different regions and communities.
Objectives:
To assess the pattern of infant feeding and its relation to certain practices of maternity and newborn care, and to assess the knowledge of mothers on the advantages of exclusive breastfeeding.
Materials and Methods:
The cross-sectional study was carried out in randomly selected villages of the Bhojipura Block of Bareilly district, Uttar Pradesh. A total of 123 women who had delivered within the last year were interviewed in a house-to-house survey. A study instrument was used to collect data. Chi- square test and regression analysis were used to analyze the data.
Results:
Most of the mothers were aged less than 30 years (78.04%) and were Hindus (73.9%). Most were illiterate (69.9%) and belonged to the lower socioeconomic class (97.5%). The majority were housewives (99.1%) and multiparous (68.2%). Most had initiated breastfeeding (78.8%) within 24 hours of delivery. About 15.4% of the infants did not receive colostrum and 22.8% of the infants were not exclusively breastfed. Ghutti (water mixed with honey and herbs), boiled water, tea, and animal milk were commonly used pre-lacteal feeds. About 47.2% of the respondents were not aware of the benefits of exclusive breastfeeding. About one quarter of the mothers started complementary feeding before the child was six months old. About half the deliveries had taken place at home and only a quarter of the females had had three or more antenatal visits during pregnancy. The birth weight of the majority (78%) of newborns was not measured. A majority (69.9%) of the mothers did not receive advice on child feeding. Multivariate logistic regression analysis showed that maternity and newborn care variables had no significant association with exclusive breastfeeding.
Conclusions:
Despite higher rates of early initiation of breastfeeding and exclusive breastfeeding, awareness of the benefits of exclusive breastfeeding was low. This indicates the need to promote awareness of the correct method of infant feeding and care of the newborn. Creating an awareness of the advantages of exclusive breastfeeding will further strengthen and support this common practice in rural communities and avoid an early introduction to complementary foods for sociocultural reasons.
Keywords: Birth weight, infant feeding practices, rural India
INTRODUCTION
Breastfeeding is one of the most important determinants of child survival, birth spacing, and prevention of childhood infections.[1,2] The importance of exclusive breastfeeding and immunological and nutritional values of breast milk have been well-demonstrated.[3,4] The beneficial effects of breastfeeding depend on the initiation of breastfeeding, its duration, and the age at which the breastfed child is weaned.[5] All infants should be fed exclusively on breast milk from birth to six months of age, and thereafter, while receiving appropriate and adequate complementary foods, breastfeeding should continue for up to two years of age or beyond.[6,7] Breastfeeding practices vary among different regions and communities. The Third National Family Health Survey (NFHS-3) of India reported that overall 21.5% of children aged under three years were breastfed within one hour of birth, 48.3% of the children aged zero to five months were exclusively breastfed, and 53.8% of the children aged six to nine months received solid or semi-solid food and breast milk.[8] The practice of breastfeeding among Indian mothers is almost universal, but initiation of breastfeeding is quite late and the colostrum is usually discarded. Breastfeeding practices in rural communities are shaped by their beliefs, which are influenced by social, cultural, and economic factors.[9] Continuous vigilance over infant feeding practices in the community is necessary for timely interventions, to ensure optimal growth and development. This information will be useful to policy makers for the formulation of interventional programs in the future. Therefore, the present study was carried out to assess the pattern of infant feeding and its relation to certain care practices of maternity and the newborn, and to assess the knowledge of mothers, who had delivered in the last one year, in the Bhojipura Block of Bareilly district, of the advantages of exclusive breastfeeding.
MATERIALS AND METHODS
The cross-sectional study was carried out in six randomly selected villages of the Bhojipura Block of Bareilly district, Uttar Pradesh. These six villages were selected by convenience out of 100 villages in the Bhojipura Block. Demographically, the villages of the Bhojipura block are populated by people with different religions, socioeconomic status, and other different characteristics. The study participants were mothers with infants aged between 0 and 11 months, who were interviewed in a house-to-house survey. Informed consent was taken from the mothers and the purpose of the study was explained to them. A total of 123 mothers who had delivered in the previous year were studied. The response rate was 100%.
A structured, pretested and predesigned questionnaire was used to collect information on the sociodemographic profile (age, religion, and caste, type of family, parent's education, occupation, and income, and birth order), details on the initiation and duration of breastfeeding, artificial feeding and weaning practices, delivery details (type and place of delivery), antenatal practices (number of antenatal visits), and newborn care practices (the birth weight was measured and explained to mother, child's weight was plotted on the growth chart, and advice on child feeding was given).
Modified Prasad's classification, based on per capita monthly income, was applied to measure the individual's socioeconomic status. The individuals were categorized into upper, upper-middle, middle, lower-middle, and lower classes.[10] Exclusive breastfeeding was defined as per the World Health Organization.[11] Place of delivery was categorized as institutional or home.
Data entry and statistical analysis were performed using the Microsoft Excel and SPSS windows version 14.0 software. Percentages and regression analysis were applied to find the results. Multiple logistic regression analysis was done using exclusive breastfeeding as the dependent variable and maternal age, religion, socioeconomic status, parent's education, birth order, type of family, place of delivery, number of antenatal visits, birth weight measured, and feeding advice given, as the independent variables. The Odds ratios with 95% confidence intervals were calculated, to assess the association between the independent variables and exclusive breastfeeding. P values < 0.05 were considered significant.
RESULTS
In our study, a majority of the mothers was of age less than 30 years (78.04%) and were Hindus (73.9%). Most of the mothers were illiterate (69.9%) and belonged to a lower socioeconomic class (97.5%). The majority were housewives (99.1%), multiparous (68.2%). About 68.2% of the mothers had birth order ≥ 2 [Table 1].
Table 1.
Sociodemographic profile of respondents

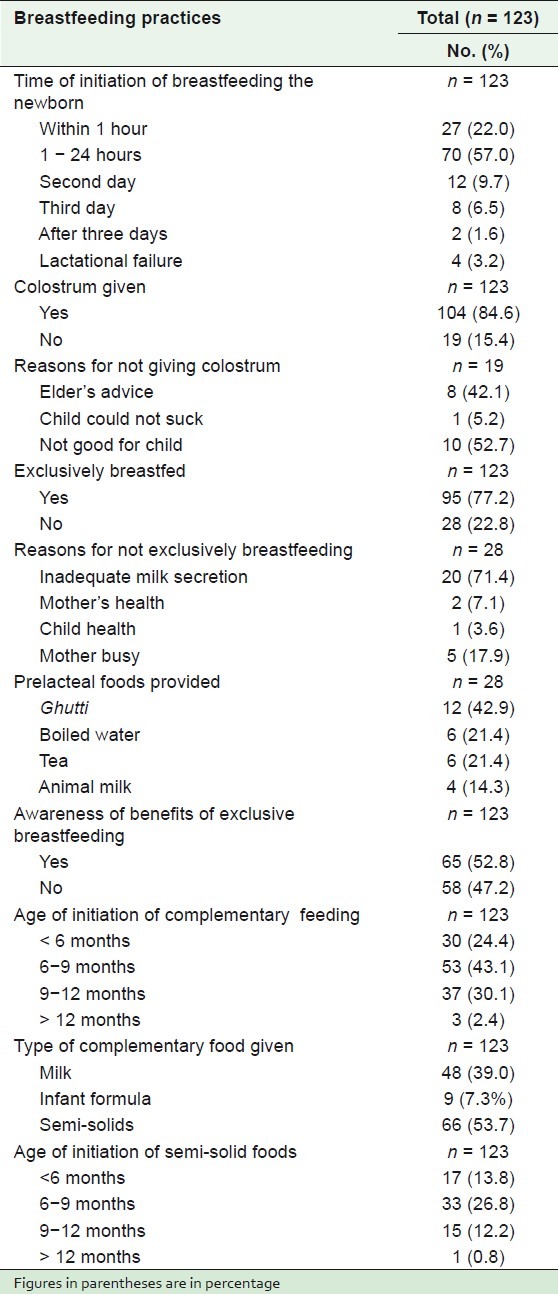
Most of the mothers had initiated breastfeeding (78.8%) within 24 hours of delivery. About 15.4% babies had not received colostrum. The most common reason stated by mothers for discarding colostrum was that they thought colostrum was not good for the child. About 22.8% of the infants were not exclusively breastfed. The most common reason for not doing so was inadequacy of milk secretion (71.4%). Ghutti, that is, water mixed with honey and herbs (42.9%), boiled water (21.4%), tea (21.4%), and animal milk (14.3%) were commonly used as pre-lacteal feeds. About 47.2% of the respondents were not aware of the benefits of exclusive breastfeeding. About one quarter of the respondents had started complementary feeding before the baby was six months old. The most common type of complementary food given was semi-solid (53.7%). About 13.8% of the mothers had started giving semi-solid foods before the baby was six months of age [Table 2].
Table 2.
Breastfeeding practices among respondents
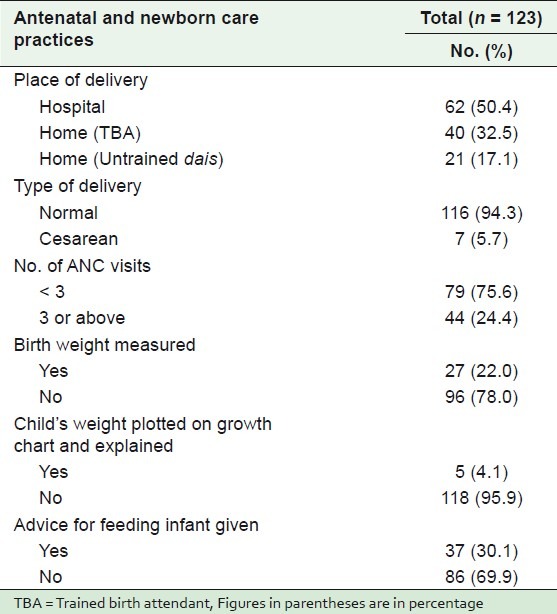
About half of deliveries had taken place at home and 17.1% of them were attended by untrained ‘dais’. The majority (94.3%) of the deliveries were normal. Only a quarter of the respondents had had three or more antenatal visits during pregnancy. Only 22% of the mothers reported that the birth weight of their children had been measured. Only 4.1% of the newborn's weight had been plotted on a growth chart and explained to their mothers. A majority of the mothers had had no advice on infant feeding [Table 3].
Table 3.
Maternity and newborn care practices in the study population
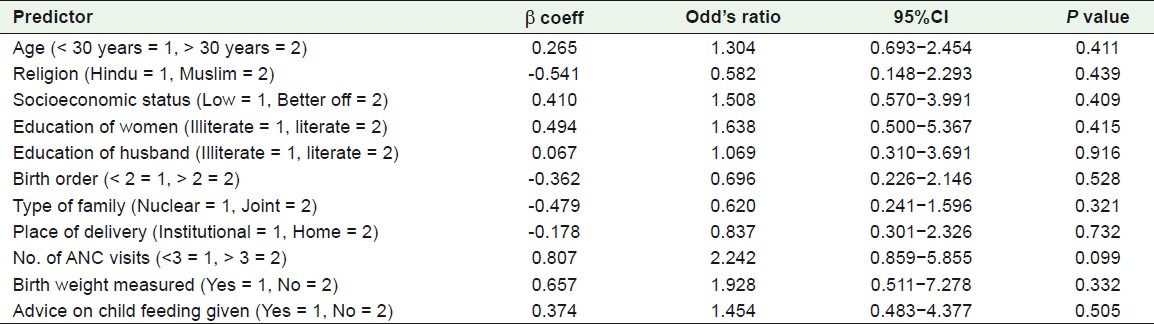
Multivariate analysis by logistic regression demonstrated no association between exclusive breastfeeding and maternal age, religion, socioeconomic status, parent's education, birth order, type of family, place of delivery, number of antenatal visits, whether the birth weight was measured, or feeding advice given [Table 4].
Table 4.
Multivariate logistic regression analysis of predictors of exclusive breastfeeding in the total study sample
DISCUSSION
A primary health center (PHC) was situated at a distance of about 15 km from the six villages. There was also a sub-center in two of the six villages. The PHC and the sub-centers were accessible geographically and economically also, for the local community of the villages of the study region. The staff responsible for maternal and child health were regularly available at the PHC and the sub center, with facilities for antenatal care, delivery, birth weight measurement, and growth monitoring available. The percentage of mothers who had exclusively breastfed for six months was 77.2%, which was much higher than the 46% at national level.[8] The rate of exclusive breastfeeding for six months was only 28.33% in an urban slum of Kolkata.[12] Women in rural areas have a very positive attitude toward the initiation of breastfeeding.[13] Most of the mothers initiated breastfeeding (78.8%) within 24 hours of delivery, in our study. Our finding is much higher compared to the (37.1%) reported at the national level.[8] A total of 21.2% of the mothers in our study did not breastfeed even 24 hours after the delivery. Our findings are compatible with those (19.0%) reported by Madhu et al. (2009).[14] Breast milk should be initiated within 30 minutes of delivery.[15] The delay in initiation leads to a delay in the development of oxytocin reflexes, which are very important for the contraction of the uterus and the breast milk reflex. Studies show that the earlier breastfeeding begins the earlier and more effective the consolidation of the process, and therefore, a better impact on the after-birth period, which helps in the earlier initiation of the secretion of breast milk.[16] About 84.6% of mothers fed colostrum to their child, which is a good practice. Similar observations were reported by Deshpande Jayant et al. (2010), in their rural study.[17] Khan et al. (2009) also reported similar findings in their study conducted in the urban slum of Aligarh.[18] Colostrum is rich in vitamins, minerals, protein and immunoglobulins that protect the child from infections.[19] The most common reason stated by mothers for discarding colostrum was that they thought colostrum was not good for the child. Similar findings have been reported by Gupta et al. (2010) in their study conducted in an urban slum of Lucknow.[20] About 22.8% of the infants were not exclusively breastfed. The most common reason found for not doing so was inadequate milk secretion (16.2%). About one-quarter of the respondents admitted that they gave pre-lacteal feeding to their child. Ghutti, boiled water, tea, and animal milk were the commonly used pre-lacteal feeds. Similar findings (27%) were reported by Deshpande et al. (2010).[17] Honey and water was commonly used as a pre-lacteal feed in rural West Bengal as reported by Mandal et al. (2007).[21] Giving pre-lacteal feed is a deep-rooted custom in India, as is evident in a plethora of studies.[22–24] Pre-lacteal feeds are given because it is believed that they act as laxatives or as a means of clearing the meconium. Unfortunately, the mothers are not aware that the pre-lacteal feeds could be a source of contamination.[17] Honey, which is used as pre-lacteal food in infants is now not recommended to be given below the age of one, because of the risk of infection by Clostridium botulinum.
Although it is universally acknowledged that exclusive breastfeeding for the first six months could reduce infant mortality by 13%, the rates of exclusive breastfeeding remain low in rural and urban areas.[25] Even as exclusive breastfeeding was prevalent in more than three-quarters of the study population, nearly half of the mothers were unaware of its benefits. This can be attributed to the fact that the dominant characteristics of the study population were mothers of low socioeconomic class with a low level of literacy. Exclusive breastfeeding for the first six months, which is highly recommended, is often a necessity in poor communities that cannot afford formula or cow's milk. This could be the most likely reason for a high percentage of mothers in the study adopting exclusive breastfeeding. However, creating an awareness of its advantages will further strengthen and support this common practice in rural communities and avoid the early introduction of complementary foods for sociocultural reasons. Thus, no opportunity should be missed by doctors and health workers to educate the rural women on the benefits of breastfeeding. Mothers with inadequate milk supply could be taught methods of improving milk secretion and the value of lactagogues.
About one quarter of the respondents in our study started complementary feeding before six months. Similar trends were reported by Chudasama et al. (2009) in their study conducted in Gujarat.[26] Too early or late introduction of complementary feeds is common and is responsible for under nutrition between six and twenty-four months.[27] Growth faltering incipiently worsens from around six months of age and results in malnutrition in later months and years.
About 13.8% of the mothers started giving semi-solid foods before six months of age, while nearly 13% of the mothers gave semi-solid foods after nine months.
The current recommendations suggest six months as the best age for initiation of semi-solid foods. The health services in the study area were underutilized.
About half of deliveries in our study took place at home and 17.1% of them were attended by untrained ‘dais’. Our figures are better than those reported by NFHS-3 for rural India (71.1%).[8] Only a quarter of the respondents had more than three antenatal visits during pregnancy. According to NFHS-3,[8] about 42.8% of the rural mothers had at least three antenatal care visits for their last birth. Only 22% of the mothers in the current study reported that the birth weight of their children had been measured. Birth weight was not recorded in 38.2% of the newborns in a study conducted in rural West Bengal.[21] In another study conducted in rural Gujarat the birth weight of 22.7% children was not measured.[28] Thus, our study reveals that there was lack of awareness among mothers regarding the measurement of the birth weight of their infants, emphasizing the need for education on infant health and nutrition during the antenatal period and delivery. For 96% of the children, weight was not plotted on a growth chart and explained to the mothers. This practice should be strictly adopted and advice on infant feeding given. The majority of the mothers in our study did not get advice on child feeding. Most of the mothers in the study conducted by Madhu et al.,[14] were given information on breastfeeding practices by their doctors. Factors such as maternal age, religion, socioeconomic status, parent's education, birth order, type of family, place of delivery, number of antenatal visits, measured birth weight with explanation, and feeding advice were analyzed for multivariate analysis, but none were found to be statistically significant for exclusive breastfeeding. In another study conducted by Chandrashekhar et al. (2006) in Nepal, friends’ feeding practices, type of delivery, and baby's first feed were the factors that influenced the exclusive breastfeeding practice of the mothers.[29]
One potential limitation of this study could be the small localized population. Hence, the findings in this study cannot be generalized to cover the state or India as a whole. Only a quarter of the respondents had three or more antenatal visits during pregnancy. This indicates underutilization of the maternal and child healthcare facilities in the region. Despite the higher rates of early initiation of breastfeeding and exclusive breastfeeding, there was low awareness of the benefits of exclusive breastfeeding . About one quarter of the respondents started complementary feeding before six months. The birth weight of a majority of newborns was also not measured. Advice for child feeding was not given to two-thirds of the mothers. This indicates the need for promoting awareness of correct practices for infant feeding and the care of the newborn. Creating an awareness of the advantages of exclusive breastfeeding will further strengthen and support this common practice in rural communities and avoid early introduction of complementary foods for sociocultural reasons.
Footnotes
Source of Support: Nil
Conflict of Interest: Nil
REFERENCES
- 1.Iskandar MB, Costello C, Nasution Y. Initiation and duration of breast feeding in Indonesia. Asia Pac Popul J. 1990;5:89–112. [PubMed] [Google Scholar]
- 2.Bautista LE. Factors associated with initiation of breast feeding in the domician Republic. Rev Panam Salud Publica. 1997;1:200–7. [PubMed] [Google Scholar]
- 3.Arifeen S, Black RE, Antelman G, Baqui A, Caulfield L, Becker S. Exclusive breast-feeding reduces acute respiratory infection and diarrhea deaths among infants in Dhaka slums. Pediatrics. 2001;108:E67. doi: 10.1542/peds.108.4.e67. [DOI] [PubMed] [Google Scholar]
- 4.Dewey KG, Cohen RJ, Brown KH, Rivera LL. Effects of exclusive breast-feeding for four versus six months on maternal nutritional status and infant motor development: Results of two randomized trials in Honduras. J Nutr. 2001;131:262–7. doi: 10.1093/jn/131.2.262. [DOI] [PubMed] [Google Scholar]
- 5.Victora CG, Smith PG, Vaughan JP, Nobre LC, Lombardi C, Teixeira AM, et al. Evidence for protection against infant deaths from infectious diseases in Brazil. Lancet. 1987;2:319–22. doi: 10.1016/s0140-6736(87)90902-0. [DOI] [PubMed] [Google Scholar]
- 6.Britton C, McCormick FM, Renfrew MJ, Wade A, King SE. Support for breast feeding mothers. Cochrane Database Syst Rev. 2007;1:CD001141. doi: 10.1002/14651858.CD001141.pub3. [DOI] [PubMed] [Google Scholar]
- 7.Innocenti Declaration on the Protection, Promotion and Support of Breastfeeding, Florence, Italy, 1 August 1990. New York: UNICEF; 1990. WHO/UNICEF meeting on Breastfeeding in the 1990s; a global initiative. [Google Scholar]
- 8.Ministry of Health and Family Welfare: National Family Health Survey 3, India. [Last cited in 2007]. Available from: http://mohfw.nic.in/nfhs3/CD.htm .
- 9.Khan ME. Breast feeding and weaning practices in India. Asia Pac Popul J. 1990;5:71–88. [PubMed] [Google Scholar]
- 10.Agarwal AK. Social classification: The need to update in the present scenario. Indian J Community Med. 2008;33:50–1. doi: 10.4103/0970-0218.39245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Report of the expert consultation on the optimal duration of exclusive breastfeeding: Conclusions and recommendations. Geneva: WHO; 2001. World Health Organization. [Google Scholar]
- 12.Roy S, Dasgupta A, Pal B. Feeding practices of children in an urban slum of Kolkata. Indian J Community Med. 2009;34:362–3. doi: 10.4103/0970-0218.58402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chandrashekar S, Chakladar BK, Rao RS. Infant feeding-- knowledge and attitudes in a rural area of Karnataka. Indian J Pediatr. 1995;62:707–12. doi: 10.1007/BF02825124. [DOI] [PubMed] [Google Scholar]
- 14.Madhu K, Chowdary S, Masthi R. Breast feeding practices and newborn care in rural areas: A descriptive cross-sectional study. Indian J Community Med. 2009;34:243–6. doi: 10.4103/0970-0218.55292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.UNICEF, Ten steps to promote successful breastfeeding Mother and Child Health Division. Geneva: World Health Organisation; 1989. World Health Organisation. [Google Scholar]
- 16.Iarukov A, Nin’o A, Iarukova N, Doicheva E, Kolev D. The early breast feeding of newborn infants. Akush Ginekol (Sofiia) 1992;31:13–5. [PubMed] [Google Scholar]
- 17.Deshpande JD, Giri PA, Phalke DB, Phalke VD, Kalakoti P, Syed MM. Socio-cultural practices in relation to breastfeeding, weaning and child rearing among Indian mothers and assessment of nutritional status of children under five in rural India. AMJ. 2010;3:618–24. [Google Scholar]
- 18.Khan Z, Mehnaz S, Khalique N, Ansari MA, Siddiqui AR. Poor perinatal care practices in urban slums: Possible role of social mobilization networks. Indian J Community Med. 2009;34:102–7. doi: 10.4103/0970-0218.51229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Davies MC, Arinolan G, Sanusin R, Osotimehin B. Immunoglobulin classes and nutritional factors in plasma and breast milk of lactating mothers in Nigeria. Iran J Immunol. 2006;3:181–6. [PubMed] [Google Scholar]
- 20.Gupta P, Srivastava VK, Kumar V, Jain S, Masood J, Ahmad N, et al. Newborn care practices in urban slums of Lucknow, UP. Indian J Community Med. 2010;35:82–5. doi: 10.4103/0970-0218.62570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mandal PK, Sardar JC, Chatterjee C, Lahiri SK, Ghosh PK. A study on breast feeding practices among infants in a rural area of west Bengal. Indian J Prev Soc Med. 2007;38:28–31. [Google Scholar]
- 22.Chaturvedi M, Nandan D, Gupta SC. Rapid assessment of infant-feeding practices in Agra district. Indian J Community Med. 2007;32:227. [PubMed] [Google Scholar]
- 23.Sharma D, Sharma S. Bottlenecks to breastfeeding in Rural Rajasthan. Indian J Community Med. 2005;30:155–6. [Google Scholar]
- 24.Pathi S, Das BC. Breast feeding practices in a rural ICDS block of Khallikote, South Orissa. Indian J Community Med. 2005;30:154. [Google Scholar]
- 25.Lal V, Rai SK. The culture of bottle feeding. Indian J Community Med. 2009;34:247–8. doi: 10.4103/0970-0218.55293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chudasama RK, Patel PC, Kavishwar AB. Determinants of Exclusive breast feeding in South Gujarat of India. J Clin Med Res. 2009;1:102–8. doi: 10.4021/jocmr2009.06.1242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ramachandran P. Breastfeeding practices in South Asia. Indian J Med Res. 2004;119:13–5. [PubMed] [Google Scholar]
- 28.Bhanderi DJ, Mukherjee SM, Gohel MK, Christian DS. An evaluation of the utilization of reproductive and child health services provided by government to the rural community of Anand district, Gujrat. Indian J Public Health. 2009;53:250–2. [PubMed] [Google Scholar]
- 29.Chandrashekhar TS, Joshi HS, Binu VS, Shankar PR, Rana MS, Ramachandran U. Breast-feeding initiation and determinants of exclusive breast-feeding - a questionnaire survey in an urban population of western Nepal. Public Health Nutr. 2006;10:192–7. doi: 10.1017/S1368980007248475. [DOI] [PubMed] [Google Scholar]


